ABSTRACT
Gay, bisexual, and other men who have sex with men (gbMSM) are disproportionately affected by HIV. While pre-exposure prophylaxis (PrEP) is highly effective at preventing HIV acquisition, uptake of PrEP among gbMSM is low, which may in part be due to stigma associated with PrEP use. This systematic review aimed to explore experiences of PrEP stigma and to identify factors associated with this. Four databases were searched for papers including terms relating to (i) gbMSM, (ii) PrEP, and (iii) stigma, with narrative synthesis used to analyze results. After screening, 70 studies were included in the final analysis. Experiences of PrEP stigma were found to be characterized by a number of stereotypes and came from a range of sources. Five categories of factors were associated with stigma: (i) healthcare-related factors, (ii) cultural and contextual factors, (iii) sociodemographic factors, (iv) peer-discussion, and (v) psychosocial factors. These findings suggest that stigma can be a common experience for gbMSM. However, some are more at risk than others. Interventions aimed at reducing PrEP stigma may be useful in increasing uptake.
Main text introduction
Since the beginning of the HIV epidemic, gay, bisexual, and other men who have sex with men (gbMSM) have been disproportionately affected by HIV (Mayer et al., Citation2021; Health Protection Surveillance Centre, Citation2023). Rapid advancements in HIV prevention include pre-exposure prophylaxis (PrEP) – a highly effective medication taken by those who do not have HIV to decrease their chances of acquiring HIV (Centres for Disease Control and Prevention, Citation2023; Grant et al., Citation2014; Liu et al., Citation2016). Despite this, the uptake of PrEP has been slow (Eaton et al., Citation2017; Parsons et al., Citation2017). One reason for this may be the stigma surrounding PrEP and those who take it (Golub, Citation2018). Goffman describes stigma as the negative classification and rejection of an individual based on possessing an attribute that is considered discrediting (Goffman, Citation1963). In this case, PrEP use may be viewed as a discrediting attribute.
While extensive research has been conducted on PrEP effectiveness and acceptability, it is only recently that stigma has begun to be explored in more detail. In a narrative review, Golub noted that PrEP stigma is a significant barrier to uptake, and often disproportionately affects marginalized groups (Golub, Citation2018). However, to date no systematic reviews have been conducted on this topic. Identifying associates of stigma may offer insights into ways in which PrEP uptake can be increased and pave the way for interventions to reduce stigma. This systematic review aimed to explore gbMSM’s experiences of stigma related to PrEP, and to establish the factors associated with experiences of PrEP stigma.
Materials and methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., Citation2021) and was registered on PROSPERO (ID: CRD42022327834). The research questions were identified by patient and public involvement (PPI) from a sample of seven gbMSM.
Study selection
Four databases (PubMed, Web of Science, EMBASE, PsycInfo) were searched in May 2022 using terms relating to (i) gbMSM (ii) PrEP, and (iii) stigma (see supplementary appendix for full search terms). A comprehensive search strategy was developed based on previous literature (Murchu et al., Citation2021; Nguyen et al., Citation2019; Virendrakumar et al., Citation2021). Only studies published in English in peer-reviewed journals between 2012-May 2022 that collected primary data from adult gbMSM were considered for inclusion. Studies must have included measures of self-reported anticipated or experienced stigma related to PrEP.
Data screening and extraction
Search results were exported to the web app Rayyan (Ouzzani et al., Citation2016), which was used to screen and tag articles, and to categorize these as included or excluded. Following the removal of duplicates, two researchers independently screened titles and abstracts, with full text of studies not excluded at this stage subsequently screened. Conflicts were resolved through discussion. The extracted data included author names, publication year, location, sample size and characteristics, study design, aim, stigma measures, and main findings.
Quality appraisal
Two researchers independently assessed study quality using the Mixed Methods Appraisal Tool, which consists of two screening questions, followed by five specific questions depending on the study designs (Hong et al., Citation2018). Conflicting appraisals were resolved through discussion, with a third reviewer consulted in cases where the conflict could not be resolved.
Analysis
Due to the wide range of measures used across studies, a meta-analysis was considered inappropriate. Instead, narrative synthesis was used to thematically analyze the data according to (i) the nature of PrEP stigma (ii) sources of stigma, and (iii) factors associated with stigma. This process involved coding extracted data, and subsequently creating themes based on these codes. Some themes were apparent from the original texts (e.g. in cases where authors had explicitly referred to items as stereotypes), while others were inferred by the authors of this review (e.g. coding items as stereotypes based on quotes from participants).
Results
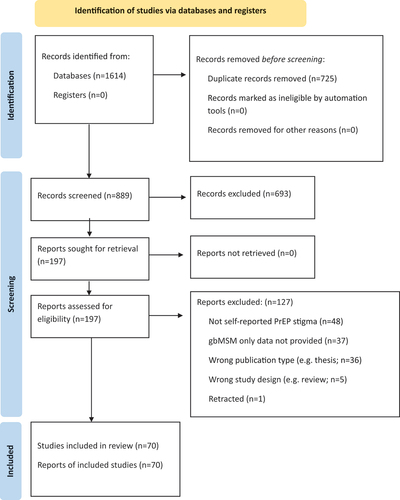
The database search yielded a total of 1614 articles. After duplicates were removed, the titles and abstracts of 889 articles were screened. Of these, 196 articles appeared to meet the inclusion criteria.
Following full-text screening, a total of 70 articles were included in the final analysis (see ).
Quality appraisal
The majority of included studies (n = 62) met all five MMAT criteria and were conducted using the appropriate methods and providing adequate data to substantiate their claims. The remaining were judged to be of medium quality, with none considered low quality (see ).
Table 1. Study characteristics.
Study characteristics
presents an overview of the included studies. The majority of these (n = 52) employed qualitative methods, but quantitative descriptive (n = 13) and mixed methods (n = 5) studies were also reviewed. Of these, 15 were cross-sectional, and 3 were longitudinal. Most studies (n = 41) were based in the USA, however a further 19 different countries were represented.
Sample sizes ranged from 12 to 750 participants, with a total of 6,537 gbMSM participants included overall.
Narrative synthesis
Just two studies explicitly reported prevalence of PrEP stigma, with quite different estimates of 10% (Rogers et al., Citation2019) and 45.2% (Quinn et al., Citation2020) of gbMSM samples. A further two studies noted that the majority of their samples were aware of stigmatizing attitudes and behaviors toward PrEP and PrEP users (Franks et al., Citation2018; Virendrakumar et al., Citation2021).
PrEP stigma was characterized by several stereotypes (see ), including assumptions that (i) PrEP users are more likely to engage in behaviors deemed “higher risk” (n = 32), (ii) PrEP users are HIV positive (n = 29), (iii) PrEP users are more promiscuous than non-PrEP users (n = 28), and (iv) PrEP is only for gbMSM (n = 15).
Table 2. Overview of PrEP user stereotypes reported.
Six sources of experienced and anticipated stigma related to PrEP were identified. From most to least commonly reported, these were (i) healthcare professionals (HCPs; n = 25), (ii) partners (n = 18), (iii) other gbMSM (n = 16), (iv) friends and acquaintances (n = 14), (v) family (n = 14), and (vi) self-stigma (n = 7) (see ).
Table 3. Sources of PrEP stigma.
The stigma associated with PrEP use was reported to affect various aspects of gbMSM’s lives. Most commonly, stigma was reported to affect relationships (n = 17), the decision to disclose PrEP use (n = 15), health behaviors (n = 10), and mental health (n = 6; see ).
Table 4. Implications of PrEP stigma.
Various factors were found to be associated with PrEP-related stigma. These factors were organized under five general categories, which were as follows: healthcare factors (n = 25), culture and context (n = 24), sociodemographics (n = 22), peer discussion (n = 12), and psychosocial factors (n = 12). An overview of the studies reporting these factors can be seen in , with more information about each factor provided below.
Table 5. Factors associated with PrEP stigma.
Healthcare factors
Experienced and anticipated stigma varied based on where PrEP was accessible. gbMSM reported mixed views on publicly funded clinics, with some pleased that PrEP was available through these, and others hesitant to seek PrEP from these clinics due to previous experiences of stigma (Kimani et al., Citation2021; S. Lee et al., Citation2019). Those considering seeking PrEP anticipated that they would be stigmatized if they accessed this through designated PrEP services, STI clinics, or HIV services (Grace et al., Citation2018; Kimani et al., Citation2021; Puppo et al., Citation2020). Some gbMSM suggested making PrEP available through drop-in centers and in less busy areas to reduce concerns about stigma (Kimani et al., Citation2021; Maloney et al., Citation2017).
Differences between HCPs were commonly reported as factors affecting stigma. For example, primary care providers (PCPs) were perceived as less competent at providing PrEP than specialists in two studies (Mpunga et al., Citation2021; Refugio et al., Citation2019). Interactions with HCPs who were gay themselves, or who were considered “gay-friendly” were frequently reported to be less stigmatizing than interactions with other HCPs (Bistoquet et al., Citation2021; Grace et al., Citation2018; S. Lee et al., Citation2019; Meyers et al., Citation2021; Mpunga et al., Citation2021; Ouzzani et al., Citation2016; Refugio et al., Citation2019; Reyniers et al., Citation2021; Williamson et al., Citation2019). Gay HCPs were perceived as more understanding, with patients reporting that it was easier to talk to and be honest with them (Bistoquet et al., Citation2021; Meyers et al., Citation2021). Some specifically switched to gay-friendly HCPs (Mpunga et al., Citation2021; Reyniers et al., Citation2021), and 52.63% of one sample reported that they would only attend gay-friendly HCPs due to previous experiences of stigma (Reyniers et al., Citation2021).
Some sexual health behaviors were found to be associated with stigma in the studies reviewed. Most commonly, PrEP users who did not use condoms reported facing additional stigma (Bourne et al., Citation2017; Brooks, Landrian, et al., Citation2019; Meyers et al., Citation2021; C. J. Sun et al., Citation2019). Similarly, non-PrEP users who did not use condoms anticipated that they would face stigma for this if they sought PrEP (Alt et al., Citation2022; Jackson et al., Citation2012). Less commonly, those who used condoms in combination with PrEP reported negative reactions due to this (Owens et al., Citation2020).
Awareness of, and experience with PrEP was examined in a small number of studies, with those who had used PrEP reporting significantly less concerns about discussing sexual activity with HCPs (Huang et al., Citation2019), as well as lower scores on the adapted PrEP User Stereotypes Scale (Magno et al., Citation2019). Meanwhile, those unaware of PrEP scored higher on a measure of perceived healthcare discrimination (J. J. Lee et al., Citation2022). However, due to the small number of papers exploring these issues, as well as the cross-sectional nature of the studies in question, these findings cannot be generalized, and directionality cannot be assumed. It may be the case that those reporting less concerns about discussing sexual activity with HCPs are more likely to use PrEP, regardless of PrEP stigma scores. Separately, a single study explored awareness of, and behaviors related to HIV, and how this relates to PrEP stigma. Surprisingly, in this study, those reporting greater knowledge of HIV were less likely to have recently discussed PrEP with a partner and to feel that their partner would support them if they used PrEP (Rice et al., Citation2019). However, those reporting a higher perceived risk of HIV acquisition and those reporting having tested for HIV within the past 3 months were more likely to report recently discussing PrEP with a partner and feeling that their partner would support them if they used PrEP (Rice et al., Citation2019). Despite this, those with a higher perceived risk of HIV acquisition were also less likely to report comfort around discussing PrEP with their partners (Rice et al., Citation2019). Again, as these findings were specific to one paper, further research on this topic is needed before they can be generalized.
Culture and context
Stigma appeared to vary between countries and culture, as well as over time. While the majority of the included studies focused on gbMSM from the USA, 19 other countries were included. However, as many of these countries were represented by only one or two studies, it is not possible to make definite statements about how stigma may differ across these contexts. In addition, these findings are likely biased due to the fact that only studies published in English were included. Further reviews of research published in other languages may reveal differences in PrEP stigma across different cultural contexts.
One major difference found between countries in the studies reviewed was that sex between men was criminalized in some countries, adding an additional layer of stigma around seeking PrEP as a gbMSM (Baruch et al., Citation2020; Vaccher et al., Citation2018). While gbMSM from certain cultures in South Asian and Central American countries noted that stigma was higher within these cultures, these statements came from a handful of individuals and may not reflect the wider experiences of gbMSM within these cultures (Bartels et al., Citation2021; Jaspal & Daramilas Citation2016; J. J. Lee et al., Citation2022)
Variations in stigma were also reported within countries. While higher levels of stigma were reported in certain cities such as New York in one study (Franks et al., Citation2018), the southern USA was reported as an area in which stigma was higher in a number of studies. Specifically, gbMSM from the Southern USA reported that the religious culture of this area amplified stigma related to PrEP (Devarajan et al., Citation2020; Hong et al., Citation2018; Refugio et al., Citation2019; Thomann et al., Citation2018). The idea of HIV as a “punishment from God” was discussed in both Central American countries (Alcantar Heredia & Goldklank, Citation2021; Klein & Washington, Citation2020), as well as within the southern USA (Hong et al., Citation2018) often leading to PrEP stigma, due to the association with HIV.
Some living in the southern USA also cited living in a rural area as a contributor to stigma, noting that there are less HCPs in these locations than in bigger cities, and that the HCPs in rural areas were perceived as less accepting of PrEP and gbMSM (Devarajan et al., Citation2020; Grace et al., Citation2018; Mpunga et al., Citation2021). Often, gbMSM reported either having to stay with these HCPs- in some cases attempting to educate them (Reyniers et al., Citation2021) or having to travel long distances to access care from less stigmatizing HCPs (Bistoquet et al., Citation2021; Grace et al., Citation2018; Mpunga et al., Citation2021; Williamson et al., Citation2019). Additionally, privacy was cited as an issue within smaller, rural towns, with gbMSM reporting concern about rumors being spread about PrEP users in these towns (Lin et al., Citation2022; Mpunga et al., Citation2021; Remy et al., Citation2020).
As well as differences by location, time also appeared to affect experiences of PrEP stigma, with some studies reporting many felt that PrEP stigma had decreased over time, and would continue to decrease (Alt et al., Citation2022; Owens et al., Citation2020; Pantalone et al., Citation2020; Quinn et al., Citation2020; C. J. Sun et al., Citation2019). Similarly, some PrEP users reported feeling less affected by stigma the longer they had been on PrEP. In two studies, gbMSM anticipated increased stigma around PrEP as awareness grew (Alcantar Heredia & Goldklank, Citation2021; Klein & Washington, Citation2020).
Sociodemographic factors
Stigma was associated with a range of sociodemographic factors in the studies reviewed, suggesting that experiences differ for different groups of gbMSM. One group that appeared to face additional stigma was “closeted” men- those who are not openly gay or bisexual. This cohort reported concern that if others knew that they took PrEP, they would also know that they are gbMSM and stigmatize them (Alcantar Heredia & Goldklank, Citation2021; Bourne et al., Citation2017; S. Lee et al., Citation2019; Sarita et al., Citation2017). This concern was especially prevalent among bisexual men (Alcantar Heredia & Goldklank, Citation2021), while gbMSM identifying as “exclusively homosexual” reported significantly less concern about being asked why they take PrEP (Huang et al., Citation2019).
Experiences of stigma also differed by race and ethnicity in the studies reviewed, with most studies here finding that non-White gbMSM experienced more stigma than their White counterparts, as well as additional barriers to PrEP (Bartels et al., Citation2021; Devarajan et al., Citation2020; Hubach et al., Citation2017; Nguyen et al., Citation2021; Refugio et al., Citation2019; Remy et al., Citation2020). This was particularly common for Black gbMSM (Devarajan et al., Citation2020; Hubach et al., Citation2017; Nguyen et al., Citation2021; Refugio et al., Citation2019; Remy et al., Citation2020) but was also an issue for Hispanic gbMSM (Bartels et al., Citation2021).
For example, in one study, Black gbMSM reported feeling stereotyped by PrEP campaigns targeted at them, perceiving these as suggesting that HIV only affected Black gbMSM, or blaming them for HIV (Remy et al., Citation2020). Another study found that Black men often associated being HIV+ with being gay, and treated those seeking PrEP “differently” due to the misconception that PrEP users are HIV positive (Nguyen et al., Citation2021).
The type of stigma discussed also varied by race in two studies (Franks et al., Citation2018; Huang et al., Citation2019), with one finding that Black and Latino gbMSM were significantly more likely than White gbMSM to discuss HIV-related stereotypes, but significantly less likely to discuss promiscuity stereotypes (Franks et al., Citation2018).
Age was associated with stigma in some of the papers reviewed, with older individuals- particularly older gbMSM- reported as a source of PrEP stigma in three studies (Collins et al., Citation2017; García et al., Citation2017; Williamson et al., Citation2019), while younger gbMSM were perceived to be less stigmatizing toward PrEP use (Collins et al., Citation2017; García et al., Citation2017). Separately, younger gbMSM reportied significantly higher perceived PrEP stigma scores in one study (Karuga et al., Citation2016), indicating that, while this cohort may be more accepting of PrEP and those who use it, they may experience higher instances of stigma. As this is a single study, these findings may not be generalizable; further studies exploring differences in perceived PrEP stigma by age ranges would be merited.
gbMSM of various ages speculated that generational differences may be partially related to the fact that many older people had directly experienced the height of the AIDS crisis, often losing loved ones and possibly being more fearful of HIV as a result (Bourne et al., Citation2017; Collins et al., Citation2017; García et al., Citation2017; Williamson et al., Citation2019). The contrast between HIV prevention methods between now and then was suggested as another reason for resistance to PrEP among older gbMSM (Bourne et al., Citation2017; Collins et al., Citation2017; García et al., Citation2017). Age was related to the type of stigma gbMSM reported concern about, with one study finding that those aged 50 or older were more likely to mention HIV-related stereotypes (Franks et al., Citation2018), while another found that younger PrEP users were more likely to report concern about assumptions that they had multiple partners, engaged in “strange” sex, did not use condoms, or were “bottoms,” as well as concerns that health insurance premiums would increase (Karuga et al., Citation2016).
A handful of studies explored socio-economic factors, with one finding that those earning over $15,000 per year reported less concern about PrEP stigma (Huang et al., Citation2019). However, the authors also found that concern about certain items specifically increased by income. These were as follows: others assuming that PrEP users are HIV positive, others questioning why one is taking PrEP, and discussing sex life with HCPs (Huang et al., Citation2019). In another study, those earning over $20,000 per year were more likely to discuss PrEP stigma related to promiscuity (Franks et al., Citation2018). Meanwhile, those with higher levels of education were more likely to report concern about promiscuity stereotypes (Elopre et al., Citation2018; Franks et al., Citation2018), while those with lower education levels were more likely to mention HIV-based stereotypes (Franks et al., Citation2018).
Much like the findings relating to cultural differences, these findings should be interpreted with caution, as in some cases- particularly relating to socio-economic differences, a limited number of studies examined this factor. Further research on PrEP stigma and its associates should aim to recruit diverse samples and compare stigma levels across a range of sociodemographic factors.
Peer discussion
Some of the studies reviewed suggest that one way to address PrEP stigma could be through informal discussions between PrEP users and non-PrEP users. Often, these conversations took place in social settings, with influential figures within communities acting as role models by sharing their experiences, addressing misconceptions, and encouraging others to consider PrEP (García et al., Citation2017; Pantalone et al., Citation2020). Those who had not had these conversations reported that they would fear stigma less if they knew someone taking PrEP (Mimiaga et al., Citation2014).
Psychosocial factors
Just under one-quarter of the included studies examined the relationship between psychosocial factors and PrEP stigma. Those exploring relationship factors primarily compared differing relationship dynamics. For example, while in one study, being in a non-monogamous relationship was found to be a source of stigma, (Bosco et al., Citation2021), three other studies found that discussing PrEP within monogamous relationships was reported to be especially challenging (Bartels et al., Citation2021; Mimiaga et al., Citation2014; C. J. Sun et al., Citation2019). Similarly, those with more partners were more likely to report comfort with discussing PrEP with a partner and perceiving that their partners would support their PrEP use (Rice et al., Citation2019). However, those in non-monogamous relationships also faced unique challenges, with some choosing not to disclose their PrEP use in order to avoid revealing that their relationships are non-monogamous, due to anticipated stigma related to this (Garcia & Saw, Citation2019; Virendrakumar et al., Citation2021; Williamson et al., Citation2019). One study comparing relationships in which individuals had either (i) agreed on a monogamous relationship, (ii) agreed on a non-monogamous relationship, or (iii) had not discussed or agreed upon the relationship dynamic, found that those in the first two groups were significantly more likely to report feeling comfortable to discussing PrEP with a partner and perceiving that their partner would support them if they used PrEP use (Rice et al., Citation2019).
gbMSM in relationships with differing HIV statuses were more likely than those in relationships in which partners had the same HIV status to report that their partner would support them if they took PrEP, although they also reported significantly lower levels of comfort about discussing PrEP with a partner (Rice et al., Citation2019). In some cases, PrEP users with partners who were HIV positive chose not to be open about their PrEP use in order to avoid revealing their partner’s status and potentially exposing them to HIV stigma (Alcantar Heredia & Goldklank, Citation2021).
One study assessing psychological measures and substance abuse within relationships found that participants were less likely to report feeling comfortable discussing PrEP with a partner if they reported recent binge drinking, substance use, internalized homophobia (Stephenson et al., Citation2022) Additionally, participants were less likely to report that their partner would support them using PrEP if they reported higher recent depressive symptoms, or if their partners reported recent substance use or higher internalized homophobia (Stephenson et al., Citation2022).
Psychological measures were also explored on an individual level in a handful of studies, with one study finding that those reporting higher levels of internalized homophobia were significantly more likely to start PrEP (Magno et al., Citation2019). Another study (Chemnasiri et al., Citation2020) found significant positive relationships between avoidance of femininity and anticipated PrEP stigma, as well as between heterosexual self-preservation and PrEP stigma. This study also found that heterosexual self-preservation was associated with increased interest in PrEP, while those reporting higher levels of avoidance of feminity reported lower interest in PrEP (Chemnasiri et al., Citation2020). In both cases, these relationships were qualified by an interaction with anticipated PrEP stigma, suggesting that these associations are also dependent on levels of PrEP stigma (Chemnasiri et al., Citation2020). Given the lack of attention paid to these issues in the literature, further studies should explore how PrEP stigma may indirectly affect other psychological factors, and subsequently PrEP uptake.
Few studies touched on the role of social support, although one study found that PrEP users usually disclosed their PrEP use to those they had a strong connection to, and those who did not report close relationships were less likely to disclose their PrEP use to their friends and family (Alcantar Heredia & Goldklank, Citation2021). Those who were not open about their gbMSM identities or PrEP use often reported lacking a supportive community (Devarajan et al., Citation2020).
While the findings of a small number of studies suggest that psychosocial factors may be linked to PrEP stigma, it should be acknowledged that less than 20% of the included studies examined these factors. Additionally, the majority of the findings regarding relationship factors came from a single study (Rice et al., Citation2019). It is evident that a more thorough investigation into the relationship between psychosocial factors and PrEP stigma is needed.
Discussion
This review provides a valuable insight into the sources of PrEP stigma, as well as the factors associated with increased and decreased levels of stigma in gbMSM. Additionally, findings suggest that stigma associated with PrEP use is complex and shaped by various stereotypes. Identifying ways in which these stereotypes can be tackled is an important consideration when designing interventions to reduce PrEP stigma, thereby increasing the uptake of PrEP.
Consistent with the wider literature, PrEP stigma permeates various aspects of gbMSM’s lives, having negative effects on their relationships, health behaviors, decision to disclose PrEP use, and mental wellbeing, highlighting the importance of developing interventions to decrease PrEP stigma (Witzel et al., Citation2019; Wong et al., Citation2019).
However, it is notable that less than 10% of the studies explored the impact of PrEP stigma on mental health. One reason for this may be because many psychological measures are quantitative, while the majority of studies included in this review were qualitative in nature. Given that stigma has been shown to be strongly associated with negative mental health outcomes in people living with HIV (Katz & Nevid, Citation2005; Vanable et al., Citation2006), the role of psychological factors in stigma merits an in-depth investigation.
While stigma emerged from multiple sources, the most frequently reported source of perceived and enacted stigma was HCPs, suggesting a clear need for HCPs to create a supportive and non-judgmental environment for PrEP users and those seeking PrEP. Similarly, over one-third of studies reported that healthcare factors- such as the clinic PrEP was available in, as well as HCP characteristics- were associated with PrEP stigma. Often, attending STI clinics to access PrEP led to anticipated stigma, in addition to acting as a barrier to many gbMSM. As Calabrese suggests, it may be beneficial to make PrEP available in wider settings such as primary care centers in order to reduce anticipated stigma and increase uptake (Calabrese, Citation2020). It is clear that HCPs could also benefit from training to familiarize themselves with PrEP and caring for gbMSM patients.
Interestingly, this review found no interventions specifically targeted at reducing PrEP stigma, however our findings suggest this should be an important consideration for future research. The importance of developing interventions to address PrEP stigma is apparent when considering the impacts discussed above. By addressing the stigma surrounding PrEP, barriers to seeking health care could be mitigated in order to increase positive health behaviors, including PrEP uptake and adherence among gbMSM, which is especially important given that this cohort is disproportionately affected by HIV.
A key factor to take into account when designing interventions is the finding that education about PrEP frequently came from informal, peer-discussions between PrEP users and non-PrEP users. These conversations were reported to challenge stigma by dispelling myths and offering a space to ask questions. It may be beneficial for stakeholders to collaborate with key community figures when attempting to promote PrEP.
A strength of the review was that the studies came from 20 different countries, spanning five continents. Experiences of stigma varied by location, with over a quarter of studies reporting geographical and cultural differences in stigma. The results suggest that when attempting to reduce PrEP stigma, it is important to acknowledge the cultural context, and consider that interventions developed in one country may not be applicable globally. In addition, stigma varied based on a range of sociodemographic factors, suggesting that certain groups of gbMSM are more at risk of facing stigma when taking or seeking PrEP compared to others.
This review also highlights a key gap in the literature, which is the lack of research into the role of psychological factors on experiences of PrEP stigma. Only five studies explored this topic, and other research in this area is limited (Hammack et al., Citation2018; Rosengren et al., Citation2021). Further research should investigate this in more depth by analyzing relationships between psychosocial measures and experiences of PrEP stigma. As well as continued research on gbMSM’s experiences of PrEP stigma, this should also be investigated in other populations, as findings may not be generalizable to all PrEP users.
Limitations
Despite covering a range of countries, over half of the studies reviewed came from the USA. In addition, only studies published in English were included, meaning that findings are biased toward a Western-centric sample and may not be generalizable to other contexts. While several studies exploring the experience of stigma were reviewed, most did not use validated measures of this, partly because validated scales specifically measuring PrEP stigma were only recently developed (Klein & Washington, Citation2019). Additionally, most studies were also cross-sectional, meaning that the directionality of relationships between stigma and its associates cannot be known. Similarly for certain factors, the number of studies investigating the impact of these was limited which limits the generalizability of certain findings.
Conclusion
Our findings offer a deeper understanding of the nature and consequences of PrEP stigma in gbMSM. We also note several gaps in the literature to be addressed by further research. Importantly, the findings highlight the need for stigma to be addressed in order to improve PrEP uptake and overall health seeking behaviors among gbMSM, which will ultimately reduce likelihood of HIV acquisition. By understanding the factors associated with PrEP stigma, those involved in providing care can begin to identify ways of reducing such stigma and barriers to care.
Supplemental Material
Download MS Word (18.9 KB)Acknowledgments
The authors wish to thank the members of the patient and public involvement panel for sharing their feedback and ideas about the research topic and design. The authors also wish to thank the journal reviewers for their feedback on the initial draft of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/00918369.2024.2326891.
Additional information
Funding
References
- Alcantar Heredia, J. L., & Goldklank, S. (2021, December). The relevance of pre-exposure prophylaxis in gay men’s lives and their motivations to use it: A qualitative study. BMC Public Health, 21(1), 1829. https://doi.org/10.1186/s12889-021-11863-w
- Alt, M., Rotert, P., Conover, K., Dashwood, S., & Schramm, A. T. (2022, February). Qualitative investigation of factors impacting pre‐exposure prophylaxis initiation and adherence in sexual minority men. Health Expectations, 25(1), 313–321. https://doi.org/10.1111/hex.13382
- Arnold, T., Brinkley-Rubinstein, L., Chan, P. A., Perez-Brumer, A., Bologna, E. S., Beauchamps, L., Johnson, K., Mena, L., & Nunn, A. (2017, February 21). Social, structural, behavioral and clinical factors influencing retention in pre-exposure prophylaxis (PrEP) care in Mississippi. Public Library of Science One, 12(2), e0172354. Caylà JA, editor. https://doi.org/10.1371/journal.pone.0172354
- Bartels, S., Castillo, I., Davis, D. A., Hightow-Weidman, L. B., Muessig, K. E., Galindo, C., & Barrington, C. (2021, December). PrEP disclosure experiences of gay and bisexual men in guatemala. AIDS and Behavior, 25(12), 4115–4124. https://doi.org/10.1007/s10461-021-03276-y
- Baruch, R., Cuadra, S. M., Arellano, J., Sánchez, D., Ortega, D. V., & Arredondo, A. (2020). Pre-exposure prophylaxis and its implications in Mexico: Notions of men who have sex with men. Sexual Health, 17(1), 22. https://doi.org/10.1071/SH18193
- Bistoquet, M., Makinson, A., Tribout, V., Perrollaz, C., Bourrel, G., Reynes, J., & Oude Engberink, A. (2021, December). Pre-exposure prophylaxis makes it possible to better live one’s sexuality and guide men who have sex with men towards a responsible approach to their health: A phenomenological qualitative study about primary motivations for PrEP. AIDS Research and Therapy, 18(1), 2. https://doi.org/10.1186/s12981-020-00327-7
- Bosco, S. C., Pawson, M., Parsons, J. T., & Starks, T. J. (2021, July 3). Biomedical HIV prevention among gay male couples: A qualitative study of motivations and concerns. Journal of Homosexuality, 68(8), 1353–1370. https://doi.org/10.1080/00918369.2019.1696105
- Bourne, A., Cassolato, M., Thuan Wei, C. K., Wang, B., Pang, J., Lim, S. H., Azwa, I., Yee, I., & Mburu, G. (2017, January). Willingness to use pre‐exposure prophylaxis (PrEP) for HIV prevention among men who have sex with men (MSM) in Malaysia: Findings from a qualitative study. Journal of the International AIDS Society, 20(1), 21899. https://doi.org/10.7448/IAS.20.1.21899
- Brooks, R. A., Landrian, A., Nieto, O., & Fehrenbacher, A. (2019, July). Experiences of anticipated and enacted pre-exposure prophylaxis (PrEP) stigma among latino MSM in Los Angeles. AIDS and Behavior, 23(7), 1964–1973. https://doi.org/10.1007/s10461-019-02397-9
- Brooks, R. A., Nieto, O., Landrian, A., & Donohoe, T. J. (2019, April 3). Persistent stigmatizing and negative perceptions of pre-exposure prophylaxis (PrEP) users: Implications for PrEP adoption among latino men who have sex with men. Aids Care-Psychological & Socio-Medical Aspects of Aids/hiv, 31(4), 427–435. https://doi.org/10.1080/09540121.2018.1499864
- Brooks, R. A., Nieto, O., Landrian, A., Fehrenbacher, A., & Cabral, A. (2020, October). Experiences of pre-exposure prophylaxis (PrEP)–related stigma among black MSM PrEP users in Los Angeles. Journal of Urban Health-Bulletin of the New York Academy of Medicine, 97(5), 679–691. https://doi.org/10.1007/s11524-019-00371-3
- Calabrese, S. K. (2020, December). Understanding, contextualizing, and addressing PrEP stigma to enhance PrEP implementation. Current HIV/AIDS Reports, 17(6), 579–588. https://doi.org/10.1007/s11904-020-00533-y
- Centres for Disease Control and Prevention [Internet]. (2023). Pre-exposure prophylaxis (PrEP). Retrieved October 21, 2023, from https://www.cdc.gov/hiv/risk/prep/index.html
- Chakrapani, V., Newman, P. A., Shunmugam, M., Mengle, S., Varghese, J., Nelson, R., & Bharat, S. (2015, October). Acceptability of HIV pre-exposure prophylaxis (PrEP) and implementation challenges among men who have sex with men in India: A qualitative investigation. AIDS Patient Care and STDs, 29(10), 569–577. https://doi.org/10.1089/apc.2015.0143
- Chemnasiri, T., Varangrat, A., Amico, K. R., Chitwarakorn, A., Dye, B. J., Grant, R. M., & Holtz, T. H. (2020, February 1). Facilitators and barriers affecting PrEP adherence among Thai men who have sex with men (MSM) in the HPTN 067/ADAPT study. Aids Care-Psychological & Socio-Medical Aspects of Aids/hiv, 32(2), 249–254. https://doi.org/10.1080/09540121.2019.1623374
- Collins, S. P., VM, M., & Stekler, J. D. (2017, January 2). The impact of HIV pre-exposure prophylaxis (PrEP) use on the sexual health of men who have sex with men: A qualitative study in Seattle, WA. International Journal of Sexual Health, 29(1), 55–68. https://doi.org/10.1080/19317611.2016.1206051
- Devarajan, S., Sales, J. M., Hunt, M., & Comeau, D. L. (2020, March 3). PrEP and sexual well-being: A qualitative study on PrEP, sexuality of MSM, and patient-provider relationships. Aids Care-Psychological & Socio-Medical Aspects of Aids/hiv, 32(3), 386–393. https://doi.org/10.1080/09540121.2019.1695734
- Driver, R., Allen, A. M., Finneran, S., Maksut, J. L., Eaton, L. A., & Kalichman, S. C. (2021, December). Masculine ideology and black men who have sex with men’s interest in HIV pre-exposure prophylaxis (PrEP). Journal of Health Psychology, 26(14), 2908–2920. https://doi.org/10.1177/1359105320941236
- Dubov, A., Galbo, P., Altice, F. L., & Fraenkel, L. (2018, November). Stigma and shame experiences by MSM who take PrEP for HIV prevention: A qualitative study. American Journal of Men’s Health, 12(6), 1843–1854. https://doi.org/10.1177/1557988318797437
- Eaton, L. A., Kalichman, S. C., Price, D., Finneran, S., Allen, A., & Maksut, J. (2017, May). Stigma and conspiracy beliefs related to pre-exposure prophylaxis (PrEP) and interest in using PrEP among black and white men and transgender women who have sex with men. AIDS and Behavior, 21(5), 1236–1246. https://doi.org/10.1007/s10461-017-1690-0
- Elopre, L., McDavid, C., Brown, A., Shurbaji, S., Mugavero, M. J., & Turan, J. M. (2018, December). Perceptions of HIV pre-exposure prophylaxis among young, black men who have sex with men. AIDS Patient Care and STDs, 32(12), 511–518. https://doi.org/10.1089/apc.2018.0121
- Franks, J., Hirsch-Moverman, Y., Loquere, A. S., Amico, K. R., Grant, R. M., Dye, B. J., Rivera, Y., Gamboa, R., & Mannheimer, S. B. (2018, April). Sex, PrEP, and stigma: Experiences with HIV pre-exposure prophylaxis among New York City MSM participating in the HPTN 067/ADAPT study. AIDS and Behavior, 22(4), 1139–1149. https://doi.org/10.1007/s10461-017-1964-6
- García, M., Harris, A. L., & Clark, J. L. (2017 September, 27). PrEP awareness and decision-making for latino MSM in San Antonio, Texas. Public Library of Science One, 12(9), e0184014. Clark JL, editor. https://doi.org/10.1371/journal.pone.0184014
- Garcia, M., & Saw, G. (2019, April 3). Socioeconomic disparities associated with awareness, access, and usage of pre-exposure prophylaxis among latino MSM ages 21–30 in San Antonio, TX. J Journal of HIV/AIDS & Social Services, 18(2), 206–211. https://doi.org/10.1080/15381501.2019.1607795
- Goffman, E. (1963). Stigma: Notes on the Management of Spoiled Identity. Touchstone.
- Golub, S. A. (2018, April). PrEP Stigma: Implicit and explicit drivers of disparity. Current HIV/AIDS Reports, 15(2), 190–197. https://doi.org/10.1007/s11904-018-0385-0
- Golub, S. A., Gamarel, K. E., & Surace, A. (2017, May). Demographic differences in PrEP-related stereotypes: Implications for implementation. AIDS and Behavior, 21(5), 1229–1235. https://doi.org/10.1007/s10461-015-1129-4
- Gómez, W., Holloway, I. W., Pantalone, D. W., & Grov, C. (2022 February, 1). PrEP uptake as a social movement among gay and bisexual men. Culture, Health & Sexuality, 24(2), 241–253. https://doi.org/10.1080/13691058.2020.1831075
- Grace, D., Jollimore, J., MacPherson, P., Strang, M. J. P., & Tan, D. H. S. (2018, January). The pre-exposure prophylaxis-stigma paradox: Learning from Canada’s first wave of PrEP users. AIDS Patient Care and STDs, 32(1), 24–30. https://doi.org/10.1089/apc.2017.0153
- Grant, R. M., Anderson, P. L., McMahan, V., Liu, A., Amico, K. R., Mehrotra, M., Hosek, S., Mosquera, C., Casapia, M., Montoya, O., Buchbinder, S., Veloso, V. G., Mayer, K., Chariyalertsak, S., Bekker, L.-G., Kallas, E. G., Schechter, M., Guanira, J., Bushman, L., Burns, D. N., & Rooney, J. F. (2014, September). Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: A cohort study. The Lancet Infectious Diseases, 14(9), 820–829. https://doi.org/10.1016/S1473-3099(14)70847-3
- Hammack, P. L., Meyer, I. H., Krueger, E. A., Lightfoot, M., Frost, D. M., & Costa, A. B. (2018, September 7). HIV testing and pre-exposure prophylaxis (PrEP) use, familiarity, and attitudes among gay and bisexual men in the United States: A national probability sample of three birth cohorts. Public Library of Science One, 13(9), e0202806. Costa AB, editor. https://doi.org/10.1371/journal.pone.0202806
- Harkness, A., Satyanarayana, S., Mayo, D., Smith-Alvarez, R., Rogers, B. G., Prado, G., & Safren, S. A. (2021, May 1). Scaling up and out HIV prevention and behavioral health services to latino sexual minority men in South Florida: Multi-level implementation barriers, facilitators, and strategies. AIDS Patient Care and STDs, 35(5), 167–179. https://doi.org/10.1089/apc.2021.0018
- Health Protection Surveillance Centre. (2023). Update on epidemiology of HIV in Ireland, to the end of 2022.
- Hong, Q. N., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., Gagnon, M.-P., Griffiths, F., Nicolau, B., O’Cathain, A., Rousseau, M.-C., Vedel, I., & Pluye, P. (2018, December 18). The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Education for Information, 34(4), 285–291. https://doi.org/10.3233/EFI-180221
- Huang, P., Wu, H. J., Strong, C., Jan, F. M., Mao, L. W., Ko, N. Y., Li, C.-W., Cheng, C.-Y., & Ku, S. W. W. (2019, November 2). Unspeakable PrEP: A qualitative study of sexual communication, problematic integration, and uncertainty management among men who have sex with men in Taiwan. Journal of Applied Communication Research: JACR, 47(6), 611–627. https://doi.org/10.1080/00909882.2019.1693608
- Hubach, R. D., Currin, J. M., Sanders, C. A., Durham, A. R., Kavanaugh, K. E., Wheeler, D. L., & Croff, J. M. (2017, August). Barriers to access and adoption of pre-exposure prophylaxis for the prevention of HIV among men who have sex with men (MSM) in a relatively rural state. AIDS Education and Prevention, 29(4), 315–329. https://doi.org/10.1521/aeap.2017.29.4.315
- Jackson, T., Huang, A., Chen, H., Gao, X., Zhong, X., & Zhang, Y. (2012, October). Cognitive, psychosocial, and sociodemographic predictors of willingness to use HIV pre-exposure prophylaxis among chinese men who have sex with men. AIDS and Behavior, 16(7), 1853–1861. https://doi.org/10.1007/s10461-012-0188-z
- Jaiswal, J., Griffin, M., Singer, S. N., Greene, R. E., Acosta, I. L. Z., Kaudeyr, S. K., Kapadia, F., & Halkitis, P. N. (2018, October 16). Structural barriers to pre-exposure prophylaxis use among young sexual minority men: The P18 cohort study. Current HIV Research, 16(3), 237–249. https://doi.org/10.2174/1570162X16666180730144455
- Jaramillo, J., Pagkas-Bather, J., Waters, K., Shackelford, L. B., Campbell, R. D., Henry, J., Grandberry, V., Ramirez, L. F., Cervantes, L., Stekler, J., Andrasik, M. P., & Graham, S. M. (2022, September). Perceptions of sexual risk, PrEP services, and peer navigation support among HIV-Negative latinx and black men who have sex with men (MSM) residing in Western Washington. Sexuality Research & Social Policy, 19(3), 1058–1068. https://doi.org/10.1007/s13178-021-00595-6
- Jaspal, R., Daramilas, C. (2016, December 31). Perceptions of pre-exposure prophylaxis (PrEP) among HIV-negative and HIV-positive men who have sex with men (MSM). Cogent Medicine, 3(1), 1256850. Lee A, editor. https://doi.org/10.1080/2331205X.2016.1256850
- Karuga, R. N., Njenga, S. N., Mulwa, R., Kilonzo, N., Bahati, P., O’reilley, K., Gelmon, L., Mbaabu, S., Wachihi, C., Githuka, G., & Kiragu, M. (2016, April 13). “How I wish this thing was initiated 100 Years ago!” Willingness to take daily oral pre-exposure prophylaxis among men who have sex with men in Kenya. Public Library of Science One, 11(4), e0151716. Kumar A, editor. https://doi.org/10.1371/journal.pone.0151716
- Katz, S., & Nevid, J. S. (2005, February). Risk factors associated with posttraumatic stress disorder symptomatology in HIV-Infected women. AIDS Patient Care and STDs, 19(2), 110–120. https://doi.org/10.1089/apc.2005.19.110
- Kimani, M., Van Der Elst, E. M., Chirro, O., Wahome, E., Ibrahim, F., Mukuria, N., de Wit, T. F. R., Graham, S. M., Operario, D., & Sanders, E. J. (2021 January, 19). “I wish to remain HIV negative”: Pre-exposure prophylaxis adherence and persistence in transgender women and men who have sex with men in coastal Kenya. Public Library of Science One, 16(1), e0244226. Morgan E, editor. https://doi.org/10.1371/journal.pone.0244226
- Klassen, B. J., Lachowsky, N. J., Lin, S. Y., Edward, J. B., Chown, S. A., Hogg, R. S., Moore, D. M., & Roth, E. A. (2017, October). Gay men’s understanding and education of new HIV prevention technologies in Vancouver, Canada. Qualitative Health Research, 27(12), 1775–1791. https://doi.org/10.1177/1049732317716419
- Klein, H., & Washington, T. A. (2019). The Pre-Exposure Prophylaxis (PrEP) Stigma Scale: Preliminary findings from a pilot study. International Public Health Journal, 11(2), 185–195.
- Klein, H., & Washington, T. A. (2020). Older versus younger men who have sex with men: Awareness of and potential barriers to the use of pre-exposure prophylaxis (PrEP) medication to prevent the transmission of HIV. J Journal of AIDS and HIV Treatment, 2(2), 42–50.
- Lau, J. Y. C., Wong, N. S., Lee, K. C. K., Kwan, T. H., Lui, G. C. Y., Chan, D. P. C., & Lee, S.-S. (2022, March). What makes an optimal delivery for PrEP against HIV: A qualitative study in MSM. International Journal of STD & AIDS, 33(4), 322–329. https://doi.org/10.1177/09564624211060824
- Lee, J. J., Aguirre, J., Munguia, L., Robles, G., Ramirez Hernandez, K., Ramirez, J. I., Leyva Vera, C. A., & Duran, M. C. (2022, October 3). Engagement of latino immigrant men who have sex with men for HIV prevention through eHealth: Preferences across social media platforms. Ethnicity & Health, 27(7), 1684–1697. https://doi.org/10.1080/13557858.2021.1943322
- Lee, S., Kwan, T., Wong, N., Lee, K. C., Chan, D. P., Lam, T. T., & Lui, G. C. (2019., October 16) Piloting a partially self-financed mode of human immunodeficiency virus pre-exposure prophylaxis delivery for men who have sex with men in Hong Kong. Hong Kong Medical Journal [Internet]. https://www.hkmj.org/earlyrelease/hkmj198030.htm.
- Lin, C., Li, L., Liu, J., Fu, X., Chen, J., Cao, W., & Li, Y. (2022 March, 4). HIV PrEP services for MSM in China: A mixed-methods study. Aids Care-Psychological & Socio-Medical Aspects of AIDS/HIV, 34(3), 310–314. https://doi.org/10.1080/09540121.2021.1896661
- Liu, A. Y., Cohen, S. E., Vittinghoff, E., Anderson, P. L., Doblecki-Lewis, S., Bacon, O., Chege, W., Postle, B. S., Matheson, T., Amico, K. R., Liegler, T., Rawlings, M. K., Trainor, N., Blue, R. W., Estrada, Y., Coleman, M. E., Cardenas, G., Feaster, D. J., Grant, R., Philip, S. S., & Buchbinder, S. (2016, January 1). Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Internal Medicine, 176(1), 75. https://doi.org/10.1001/jamainternmed.2015.4683
- Magno, L., Dourado, I., Sutten Coats, C., Wilhite, D., Da Silva, L. A. V., Oni-Orisan, O., Brown, J., Soares, F., Kerr, L., Ransome, Y., Chan, P. A., & Nunn, A. (2019 August, 3). Knowledge and willingness to use pre-exposure prophylaxis among men who have sex with men in Northeastern Brazil. Global Public Health, 14(8), 1098–1111. https://doi.org/10.1080/17441692.2019.1571090
- Maksut, J. L., Eaton, L. A., Siembida, E. J., Fabius, C. D., & Bradley, A. M. (2018, November). Health care discrimination, sex behavior disclosure, and awareness of pre-exposure prophylaxis among black men who have sex with men. Stigma and Health, 3(4), 330–337. https://doi.org/10.1037/sah0000102
- Maloney, K. M., Krakower, D. S., Ziobro, D., Rosenberger, J. G., Novak, D., & Mayer, K. H. (2017, August). Culturally competent sexual healthcare as a prerequisite for obtaining preexposure prophylaxis: Findings from a qualitative study. LGBT Health, 4(4), 310–314. https://doi.org/10.1089/lgbt.2016.0068
- Mayer, K. H., Nelson, L., Hightow-Weidman, L., Mimiaga, M. J., Mena, L., Reisner, S., Daskalakis, D., Safren, S. A., Beyrer, C. & Sullivan, P. S. (2021, March). The persistent and evolving HIV epidemic in American men who have sex with men. Lancet, 397(10279), 1116–1126. https://doi.org/10.1016/S0140-6736(21)00321-4
- Meyers, K., Wu, Y., Shin, K. Y., Hou, J., Hu, Q., Duan, J., Li, Y., & He, X. (2021, June 1). Salient constructs for the development of shared decision-making tools for HIV pre-exposure prophylaxis uptake and regimen choice: Behaviors, behavioral skills, and beliefs. AIDS Patient Care and STDs, 35(6), 195–203. https://doi.org/10.1089/apc.2021.0066
- Mimiaga, M. J., Closson, E. F., Kothary, V., & Mitty, J. A. (2014, January). Sexual partnerships and considerations for HIV antiretroviral pre-exposure prophylaxis utilization among high-risk substance using men who have sex with men. Archives of Sexual Behavior, 43(1), 99–106. https://doi.org/10.1007/s10508-013-0208-8
- Mpunga, E., Persaud, N., Akolo, C., Boyee, D., Kamanga, G., Trapence, G., Chilongozi, D., Ruberintwari, M., & Masankha Banda, L. (2021, October 27). Readiness for use of HIV preexposure prophylaxis among men who have sex with men in Malawi: Qualitative focus group and interview study. JMIR Public Health Surveillance, 7(10), e26177. https://doi.org/10.2196/26177
- Murchu, E. O., Marshall, L., Hayes, C., Harrington, P., Moran, P., Teljeur, C., & Ryan, M. (2021, September). Oral pre-exposure prophylaxis (PrEP) to prevent HIV: A systematic review and meta-analysis of clinical effectiveness, safety, adherence and risk compensation in all populations. HIV/AIDS. Retrieved January 17, 2024. Internet. 10.1101/2021.09.24.21264095
- Newman, P. A., Guta, A., Lacombe-Duncan, A., & Tepjan, S. (2018). Clinical exigencies, psychosocial realities: Negotiating HIV pre-exposure prophylaxis beyond the cascade among gay, bisexual and other men who have sex with men in Canada. Journal of the International AIDS Society, 21(11), e25211. https://doi.org/10.1002/jia2.25211
- Nguyen, L. H., Nguyen, H. L. T., Tran, B. X., Larsson, M., Rocha, L. E. C., Thorson, A., & Strömdahl, S. (2021, December). A qualitative assessment in acceptability and barriers to use pre-exposure prophylaxis (PrEP) among men who have sex with men: Implications for service delivery in Vietnam. BMC Infectious Diseases, 21(1), 472. https://doi.org/10.1186/s12879-021-06178-5
- Nguyen, L. H., Tran, B. X., Rocha, L. E. C., Nguyen, H. L. T., Yang, C., Latkin, C. A., Thorson, A., & Strömdahl, S. (2019, September). A systematic review of ehealth interventions addressing HIV/STI prevention among men who have sex with men. AIDS and Behavior, 23(9), 2253–2272. https://doi.org/10.1007/s10461-019-02626-1
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016, December). Rayyan—a web and mobile app for systematic reviews. Systematic Review, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4
- Owens, C., Hubach, R. D., Williams, D., Lester, J., Reece, M., & Dodge, B. (2020, February). Exploring the pre-exposure prophylaxis (PrEP) health care experiences among men who have sex with men (MSM) who live in rural areas of the Midwest. AIDS Education and Prevention, 32(1), 51–66. https://doi.org/10.1521/aeap.2020.32.1.51
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., McGuinness, L. A., & Whiting, P. (2021, April). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, 105906. https://doi.org/10.1016/j.ijsu.2021.105906
- Pantalone, D. W., Holloway, I. W., Goldblatt, A. E. A., Gorman, K. R., Herbitter, C., & Grov, C. (2020, January). The impact of pre-exposure prophylaxis on sexual communication and sexual behavior of urban Gay and bisexual men. Archives of Sexual Behavior, 49(1), 147–160. https://doi.org/10.1007/s10508-019-01478-z
- Parsons, J. T., Rendina, H. J., Lassiter, J. M., Whitfield, T. H. F., Starks, T. J., & Grov, C. (2017, March 1). Uptake of HIV pre-exposure prophylaxis (PrEP) in a National cohort of Gay and bisexual men in the United States. JAIDS Journal of Acquired Immune Deficiency Syndromes, 74(3), 285–292. https://doi.org/10.1097/QAI.0000000000001251
- Philbin, M. M., Parker, C. M., Parker, R. G., Wilson, P. A., Garcia, J., & Hirsch, J. S. (2016, June). The promise of pre-exposure prophylaxis for black men who have sex with men: An ecological approach to attitudes, beliefs, and barriers. AIDS Patient Care and STDs, 30(6), 282–290. https://doi.org/10.1089/apc.2016.0037
- Puppo, C., Spire, B., Morel, S., Génin, M., Béniguel, L., Costagliola, D., Ghosn, J., Mabire, X., Molina, J. M., Rojas Castro, D., & Préau, M. (2020, May 13). How PrEP users constitute a community in the MSM population through their specific experience and management of stigmatization. The example of the French ANRS-PREVENIR study. Aids Care-Psychological & Socio-Medical Aspects of Aids/hiv, 32(sup2), 32–39. https://doi.org/10.1080/09540121.2020.1742863
- Quinn, K. G., Christenson, E., Spector, A., Amirkhanian, Y., & Kelly, J. A. (2020, August). The influence of peers on PrEP perceptions and use among young black Gay, bisexual, and other men who have sex with men: A qualitative examination. Archives of Sexual Behavior, 49(6), 2129–2143. https://doi.org/10.1007/s10508-019-01593-x
- Refugio, O. N., Kimble, M. M., Silva, C. L., Lykens, J. E., Bannister, C., & Klausner, J. D. (2019). PrEPTECH: A telehealth-based initiation program for human immunodeficiency virus pre-exposure prophylaxis in young men of color who have sex with men. A pilot study of feasibility. Journal of Acquired Immune Deficiency Syndromes (1999), 80(1), 40–45. January 1, 2019 https://doi.org/10.1097/QAI.0000000000001873
- Remy, L. M., Majee, W., Teti, M., & Enriquez, M. (2020 October, 1). Perceptions of black men who have sex with men about accessing and taking PrEP: A qualitative study. J Journal of HIV/AIDS & Social Services, 19(4), 263–282. https://doi.org/10.1080/15381501.2020.1824843
- Reyniers, T., Zimmermann, H. M. L., Davidovich, U., Vuylsteke, B., Laga, M., Hoornenborg, E., Prins, M., De Vries, H. J. C., & Nöstlinger, C. (2021, July). The social meanings of PrEP use – a mixed‐method study of PrEP use disclosure in Antwerp and Amsterdam. Sociology of Health & Illness, 43(6), 1311–1327. https://doi.org/10.1111/1467-9566.13283
- Rice, W. S., Stringer, K. L., Sohail, M., Crockett, K. B., Atkins, G. C., Kudroff, K., Batey, D. S., Hicks, J., Turan, J. M., Mugavero, M. J., & Turan, B. (2019, November). Accessing pre-exposure prophylaxis (PrEP): Perceptions of Current and potential PrEP users in Birmingham, Alabama. AIDS and Behavior, 23(11), 2966–2979. https://doi.org/10.1007/s10461-019-02591-9
- Rogers, B. G., Whiteley, L., Haubrick, K. K., Mena, L. A., & Brown, L. K. (2019 November, 1). Intervention messaging about pre-exposure prophylaxis use among young, black sexual minority men. AIDS Patient Care and STDs, 33(11), 473–481. https://doi.org/10.1089/apc.2019.0139
- Rosengren, A. L., Lelutiu-Weinberger, C., Woodhouse, E. W., Sandanapitchai, P., & Hightow-Weidman, L. B. (2021, July). A scoping review of HIV pre-exposure prophylaxis stigma and implications for stigma-reduction interventions for men and transwomen who have sex with men. AIDS and Behavior, 25(7), 2054–2070. https://doi.org/10.1007/s10461-020-03135-2
- Schwartz, J., & Grimm, J. (2019, January 2). Stigma communication surrounding PrEP: The experiences of a sample of men who have sex with men. Health Communication, 34(1), 84–90. https://doi.org/10.1080/10410236.2017.1384430
- Stephenson, R., Chavanduka, T. M. D., Sullivan, S., & Mitchell, J. W. (2022, July). Partner support and communication for pre-exposure prophylaxis (PrEP) use among male couples. Archives of Sexual Behavior, 51(5), 2549–2562. https://doi.org/10.1007/s10508-021-02118-1
- Storholm, E. D., Volk, J. E., Marcus, J. L., Silverberg, M. J., & Risk Perception, S. D. (2017, August). Sexual behaviors, and PrEP adherence among substance-using men who have sex with men: A qualitative study. Prevention Science, 18(6), 737–747. https://doi.org/10.1007/s11121-017-0799-8
- Sullivan, M. C., & Eaton, L. A. (2021, June). Intersecting barriers to PrEP awareness and uptake in black men who have sex with men in Atlanta, GA: A syndemic perspective. International Journal of Behavioral Medicine, 28(3), 349–359. https://doi.org/10.1007/s12529-020-09925-1
- Sun, C. J., Anderson, K. M., Toevs, K., Morrison, D., Wells, C., & Nicolaidis, C. (2019, February). “Little tablets of gold”: An examination of the psychological and social dimensions of PrEP among LGBTQ communities. AIDS Education and Prevention, 31(1), 51–62. https://doi.org/10.1521/aeap.2019.31.1.51
- Sun, S., Yang, C., Zaller, N., Zhang, Z., Zhang, H., & Operario, D. (2021, November). PrEP willingness and adherence self-efficacy among men who have sex with men with recent condomless anal sex in Urban China. AIDS and Behavior, 25(11), 3482–3493. https://doi.org/10.1007/s10461-021-03274-0
- Tangmunkongvorakul, A., Chariyalertsak, S., Amico, K. R., Saokhieo, P., Wannalak, V., Sangangamsakun, T., Goicochea, P., Grant, R. (2013, August 1). Facilitators and barriers to medication adherence in an HIV prevention study among men who have sex with men in the iPrex study in Chiang Mai, Thailand. Aids Care-Psychological & Socio-Medical Aspects of Aids/hiv, 25(8), 961–967. https://doi.org/10.1080/09540121.2012.748871
- Thomann, M., Grosso, A., Zapata, R., & Chiasson, M. A. (2018, July 3). ‘WTF is PrEP?’: Attitudes towards pre-exposure prophylaxis among men who have sex with men and transgender women in New York City. Culture, Health & Sexuality, 20(7), 772–786. https://doi.org/10.1080/13691058.2017.1380230
- Vaccher, S. J., Kaldor, J. M., Callander, D., Zablotska, I. B., & Haire, B. G. (2018, December). Qualitative insights into adherence to HIV pre-exposure prophylaxis (PrEP) among Australian gay and bisexual men. AIDS Patient Care and STDs, 32(12), 519–528. https://doi.org/10.1089/apc.2018.0106
- Vanable, P. A., Carey, M. P., Blair, D. C., & Littlewood, R. A. (2006, September). Impact of HIV-Related stigma on health behaviors and psychological adjustment among HIV-Positive men and women. AIDS and Behavior, 10(5), 473–482. https://doi.org/10.1007/s10461-006-9099-1
- Virendrakumar, B., Stephen, C., Jolley, E., Schmidt, E. (2021, May) Disability-related stigma and discrimination in sub-saharan Africa and south Asia: A systematic literature review [Internet]. Sightsavers. p. 78. Retrieved January 17, 2024 from https://research.sightsavers.org/wp-content/uploads/2021/08/Sightsavers-systematic-review-into-stigma-and-disability-FINAL-UPDATED.pdf
- Williamson, I., Papaloukas, P., Jaspal, R., & Lond, B. (2019, October 20). ‘There’s this glorious pill’: Gay and bisexual men in the English midlands navigate risk responsibility and pre-exposure prophylaxis. Critical Public Health, 29(5), 560–571. https://doi.org/10.1080/09581596.2018.1497143
- Witzel, T. C., Nutland, W., & Bourne, A. (2019, June). What are the motivations and barriers to pre-exposure prophylaxis (PrEP) use among black men who have sex with men aged 18–45 in London? Results from a qualitative study. Sexually Transmitted Infections, 95(4), 262–266. https://doi.org/10.1136/sextrans-2018-053773
- Wong, C. S., Kumar, P. A., Wong, C. M., Choong, B. C. H., Lim, O. Z., Chan, Y. Y., Ibrahim, M. A. B., Chio, M. T., Tan, R. K. J., & Chen, M. I. (2019, April). Acceptability of HIV pre-exposure prophylaxis (PrEP) and opinions on PrEP service delivery among men who have sex with men in Singapore: A qualitative study. AIDS Education and Prevention, 31(2), 152–162. https://doi.org/10.1521/aeap.2019.31.2.152
- Zapata, J. P., Petroll, A., St, D., Aubin, E., & Quinn, K. (2022, January 28). Perspectives on social support and stigma in PrEP-related care among gay and bisexual men: A qualitative investigation. Journal of Homosexuality, 69(2), 254–276. https://doi.org/10.1080/00918369.2020.1819709