Abstract
There is significant disagreement about how to support trans-identified or gender-dysphoric young people. Different experts and expert bodies make strikingly different recommendations based upon the same (limited) evidence. The US-originating “gender-affirmative” model emphasizes social transition and medical intervention, while some other countries, in response to evidence reviews of medical intervention outcomes, have adopted psychological interventions as the first line of treatment. A proposed model of gender-affirming care, comprising only medical intervention for “eligible” youth, is described in Rosenthal (Citation2021). Determining eligibility for these medical interventions is challenging and engenders considerable disagreement among experts, neither of which is mentioned. The review also claims without support that medical interventions have been shown to clearly benefit mental health, and leaves out significant risks and less invasive alternatives. The unreliability of outcome studies and the corresponding uncertainties as to how gender dysphoria develops and responds to treatment are also unreported.
Background
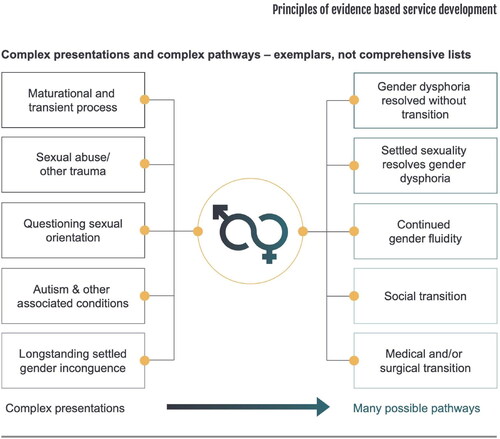
There has been a rapid rise in reported cases of gender dysphoria and trans-identified youth in the last few years (de Graaf, Giovanardi, Zitz, & Carmichael, Citation2018; Cass, Citation2021; American College Health Association, Citation2021). Gender dysphoria (GD) is a distressing condition that requires compassionate care (American Psychiatric Association, Citation2020), but neither gender dysphoria itself nor what constitutes best care are well understood. Gender dysphoria appears to have many different etiological influences, with biological, cultural, social, and psychological factors, and a variety of pathways to resolution (several presentations and pathways are shown in , reproduced from the Cass Interim Report [Cass Review, Citation2022a, page 57]). It has been suggested that many forms of gender dysphoria exist, including childhood onset which typically resolves and is associated with adult homosexual orientation (Ristori & Steensma, Citation2016; Singh, Bradley, & Zucker, Citation2021), a condition (paraphilia) observed in older men (Blanchard, Citation1989; Bailey & Blanchard, Citation2017), and other less-understood presentations that appear to be associated with comorbid mental illness, autism spectrum disorders, trauma, or other mental health issues (Bockting, Knudson, & Goldberg, Citation2006; Churcher-Clarke & Spiliadis, Citation2019; Evans & Evans, Citation2021; Evans, Citation2022; Lemma, Citation2018; Parkinson, Citation2014; Withers, Citation2020).
Figure 1. Examples of some different presentations and pathways for gender dysphoria, reproduced from the UK National Health Services commissioned Cass Interim Report (Cass Review, Citation2022a, page 57).
Several interventions for gender dysphoria have been attempted with varying degrees of success, ranging from puberty blockers, hormones and surgery (Coleman et al., Citation2012; Citation2022; Hembree et al., Citation2017; Rafferty et al., Citation2018) to noninvasive holistic developmentally-informed care and treatment of co-occurring mental health conditions (Ayad et al., Citation2022; Churcher-Clarke & Spiliadis, Citation2019; Evans & Evans, Citation2021; Evans, Citation2022; Parkinson, Citation2014; Schwartz, Citation2021; Withers, Citation2020). Simple progression of time, absent any intervention, has also been noted to lead to a resolution of gender dysphoria in many with childhood onset (Ristori & Steensma, Citation2016; Singh et al., Citation2021).
It is currently not possible to reliably estimate how any given individual case of gender dysphoria might proceed, with or without any specific intervention (Levine, Abbruzzese, & Mason, Citation2022). Even for the better studied childhood onset cases, there is no clinical test to reliably estimate the likelihood of persistence (Singh et al., Citation2021). For the quickly rising adolescent onset cohort (Kaltiala-Heino, Bergman, Työläjärvi, & Frisén, Citation2018, p. 31): “virtually nothing is known regarding adolescent onset GD, its progression and factors that influence the completion of the developmental tasks of adolescence among young people with GD and/or transgender identity.” As a result of these uncertainties, what constitutes the best possible care for gender dysphoria is poorly understood and the subject of intense disagreement among professionals (Vrouenraets, Fredriks, Hannema, Cohen-Kettenis, & de Vries, Citation2015).
One approach is the “affirmative model,” which routinely offers rapid social transition and medical intervention, i.e., puberty blockers, hormones and surgery (Rafferty et al., 2018, Table 2). This approach has become the prevailing model in the United States, where it originated (Cass Review, Citation2022a, p. 78), and was formally endorsed by the American Academy of Pediatrics (AAP) in 2018 (Rafferty et al., 2018). The AAP guidelines explain that gender affirmation “was formerly referred to as ‘transitioning’” (Rafferty et al., 2018, p. 5), and, in practice, hormones or puberty blockers can even be prescribed at the first clinic visit (Terhune, Respaut, & Conlin, Citation2022). In contrast, on the heels of rigorous evidence reviews of medical intervention outcomes, detailed later, Finland (Council for Choices in Healthcare Finland (COHERE Finland), Citation2020), Sweden (Swedish National Board of Health & Welfare, Citation2022), the UK in their proposed guidelines (NHS England, Citation2022), and Florida in its proposed regulations (Ghorayshi, Citation2022) have turned to prioritizing mental health interventions instead, only recommending medical intervention for those under 18 after extensive evaluation, if at all. For example, the central UK pediatric gender clinic is now slated to be shut down due to safety and viability concerns, with the Cass Interim Report describing that staff felt “under pressure to adopt an unquestioning affirmative approach and that this is at odds with the standard process of clinical assessment and diagnosis that they have been trained to undertake in all other clinical encounters” (Cass Review, Citation2022a, p. 17). A more holistic approach is now to be adopted (the Cass Review, [Citation2022b] noted in follow-up that many they spoke with had different interpretations of terms related to gender affirming and exploratory therapeutic care). The French National Academy of Medicine (Citation2022) has similarly advised caution and encouraged psychotherapy.
The striking difference between the two approaches to treating gender-distressed youth (“affirmation” featuring puberty blockers, hormones and surgeries versus noninvasive psychotherapy as the first line of treatment) and the seriousness of the medical interventions involved invites further scrutiny. In this paper, the available research evidence is compared to Rosenthal (Citation2021), a recent review which “highlights key advances in our understanding of transgender and gender-diverse youth, the challenges of providing gender-affirming care, gaps in knowledge and priorities for research” (p. 581). His review is a suitable representative of the approach emphasizing medical intervention not only because of its breadth, prominence as a Nature review and wide impact (e.g., its role in legal proceedings [Amicus Brief of Medical Groups, 2022]), but also because Rosenthal coauthored both the Endocrine Society guidelines (Hembree et al., Citation2017) and one of the foundational papers outlining the gender-affirmative model (Hidalgo et al., Citation2013). Non-specialists and even specialist clinicians may lack sufficient time or expertise to disentangle the current expert disagreements; the aim of this evidence comparison is to help clinicians and others better navigate current research and inform their practice, as well as to educate patients directly.
Rosenthal (Citation2021) presents a narrative for the development and treatment of trans-identification and gender dysphoria which rests on five key points, common in approaches emphasizing medical intervention. The first point presents the framing in terms of gender identity. The rest are stated as or implied to be facts, but are insufficiently supported by the evidence Rosenthal (Citation2021) provides, and in some cases even in conflict with it or the evidence more broadly.
Gender identity underlies gender dysphoria and is a fundamental personal characteristic, suggested to be biologically “ingrained.”
The current sharp rise of youth presenting with gender dysphoria does not correspond to an intrinsic rise in cases.
Care is medical intervention, with agreed upon eligibility criteria well supported by evidence.
Medical interventions have been demonstrated to be effective and safe.
Detransition does not represent medical harm and is rare.
These points are now elaborated in turn.
1. Gender identity underlies gender dysphoria and is a fundamental personal characteristic, suggested to be biologically “ingrained.”
Rosenthal’s (Citation2021) assumptions regarding gender identity provide context for all five points listed above. He assumes gender dysphoria and trans-identification are due to a conflict between a person’s gender identity and their body, with gender identity defined as “a person’s fundamental, inner sense of self as male or female” which “is not always binary” (p. 582). He assumes this fundamental gender identity “can only be assumed and not known until an individual reaches a particular level of psychological development and self-awareness” (p. 582).
As would support a fundamental gender identity, Rosenthal (Citation2021, p. 581) states there is “compelling evidence that biology contributes to gender identity development [3–16] (with the correlate that gender identity, like sexual orientation, is ingrained and not a ‘choice’).”
(The [3–16] refers to numbered references in Rosenthal, [Citation2021] itself.) In support of a biological ingrained gender identity, Rosenthal (Citation2021) provides genetic and neurological studies of people with gender dysphoria or trans-identification compared to people in the general population; however, these studies fall short. Some are confounded by including children (whose gender dysphoria is likely to abate [Ristori & Steensma, Citation2016; Singh et al., Citation2021]), not controlling for homosexuality (which does have some biological indicators), or having unusual and stereotypical definitions of gender (e.g., defining male gender as masculinity which is then taken to correspond to “aggressive, dominant, and independent” [Polderman et al., Citation2018, p. 102]). The others have too small samples (Marek et al., Citation2022), find nothing conclusive, or detect no signal. Rosenthal (Citation2021) also presents endocrinological studies of disorders of sexual development (DSD), an entirely different condition with a well defined genetic or hormonal etiology, unlike gender dysphoria. As the vast majority of trans-identified people have no DSD, reliance on DSD studies and the endocrine differences in that population in order to claim an endocrine component to gender dysphoria is misleading. In sum, there is no currently available test (brain, DNA, or otherwise) that can reliably differentiate between a trans-identified and a non-trans identified person, which Rosenthal (Citation2021) acknowledges: “(n)o currently available laboratory test can identify an individual’s gender identity” (p. 581). Neither Rosenthal (Citation2021) nor anyone else (see for instance, Frigerio, Ballerini, & Valdés Hernández, [Citation2021]) has established the existence of a biologically “ingrained” gender identity.
If Rosenthal (Citation2021) had shown his assumed fundamental gender identity to be biologically “ingrained,” this might imply that gender identity, and thus trans-identification, was unalterable in general (unlike, say, a gender dysphoria case with a possible biological contribution). The well-known frequent resolution of childhood onset gender dysphoria (Ristori & Steensma, Citation2016; Singh et al., Citation2021) could be interpreted as an example where Rosenthal’s (Citation2021) assumed fundamental gender identity only becomes correctly known with maturity, so it is not necessarily in conflict with an unalterable fundamental gender identity. In contrast, other experts have suggested gender identity itself might change (Zucker, Citation2017). Even a reference Rosenthal (Citation2021) cites for gender identity (Coleman et al., 2012) relies on another which claims “People vary in the intensity of their gender identification and in the permanence and completeness of this feeling. One’s feelings of being a man and/or woman may fluctuate…” (Bockting, Citation1999, p. 3).
A biologically “ingrained” gender identity would appear to be in direct conflict with observations where gender dysphoria has resolved, either spontaneously, or with help of psychotherapy, at a variety of ages (Churcher-Clarke & Spiliadis, Citation2019; D’Angelo, Citation2018; Evans & Evans, Citation2021; Levine, Citation2018; Parkinson, Citation2014; Withers, Citation2020). More generally, these cases of transient gender dysphoria seem difficult to fit within Rosenthal’s assumptions regarding gender identity and gender dysphoria.
2. The current sharp rise of youth presenting with gender dysphoria does not correspond to an intrinsic rise in cases
The “epidemic-like” rise (French National Academy of Medicine, Citation2022) of gender dysphoria in youth is viewed as an open puzzle (Cass, Citation2021; Swedish National Board of Health & Welfare, Citation2022), with questions being raised about possible relations to social contagion (Anderson, Citation2022a; Citation2022b; Littman, Citation2018; Marchiano, Citation2017). These suggested psychosocial influences do not appear to connect easily to the assumption of a fundamental (biologically “ingrained”) gender identity.
In response to a psychosocial hypothesis that might help explain the rise, Rosenthal (Citation2021) is dismissive. He refers to the hypothesis, that psychosocial factors can cause or contribute to the development of gender dysphoria in some individuals (Littman, Citation2018; Citation2021), as “a putative phenomenon” (p. 588). He repeats criticisms of the study (Littman, Citation2018) that generated this hypothesis, but not the rebuttals (Littman, Citation2020) of the criticisms. He then misleadingly states “(t)he above-noted methodological concerns prompted publication of a correction by the original author” (Rosenthal, Citation2021, p. 589) without mentioning that for the correction: “Other than the addition of a few missing values in Table 13, the Results section is unchanged in the updated version of the article” (Littman, Citation2019, p. 1). This psychosocial contribution hypothesis has since been bolstered by a peer reviewed study with first person reports (Littman, Citation2021).
Rosenthal’s (Citation2021) review sidesteps the challenge the psychosocial hypothesis may pose to his assumptions about gender identity, by presenting the rise in cases it addresses as neither a puzzle nor due to an actual rise in the numbers of those with gender dysphoria. He calls the rise “a notable change in our understanding of the TGD population” (p. 583), suggesting it is only the understanding, not the population, that is changing. He lists reasons for the rise (as fact) which describe why those with gender dysphoria might now be more likely to come forward or to be diagnosed, e.g., greater acceptance. These reasons are consistent with increased recognition of his assumed “fundamental” gender identities rather than the actual underlying number of cases changing (perhaps due to external influences). However, he does not show that his interpretation is better supported by the evidence than one which treats the rise in cases as intrinsic or some combination of the two. The potential validity of Littman’s hypothesis, possible contribution to the rise in cases, and unclear relation to Rosenthal’s (Citation2021) hypothesized fundamental gender identity remain (Arnoldussen et al., Citation2022; French National Academy of Medicine, Citation2022).
3. Care is medical intervention, with agreed upon eligibility criteria well supported by evidence
A key component of Rosenthal’s (Citation2021) approach is his claim that one’s fundamental gender identity can be accurately recognized upon reaching a requisite level of “psychological development and self-awareness” (p. 582). He appears to imply this level may be reached at or around pubertal onset, as he states (p. 585): “Longitudinal studies have indicated that the emergence or worsening of gender dysphoria with pubertal onset is associated with a very high likelihood of being a transgender adult.”
Rosenthal (Citation2021) explains that “this observation is central to the rationale for medical intervention in eligible transgender adolescents” (p. 585). His assumption of not only a fundamental but possibly “ingrained” gender identity can be seen here to have profound implications, as it frames irreversible medical intervention as a response to what he assumes is a fundamental (and in some interpretations of his approach, unchanging) personal characteristic.
However, beyond the fact that the general durability of Rosenthal’s assumed gender identity (and corresponding trans-identification) has not been established, and appears in conflict with the evidence as mentioned earlier, the particular “central” observation to which Rosenthal (Citation2021) refers is not supported by the paper he cites for it (Cohen-Kettenis, Delemarre-van de Waal, & Gooren, Citation2008). First of all, the authors focus on those with childhood onset, explicitly requiring it for medical interventions they discuss. They make no claim regarding outcomes for the distinct presentation of gender dysphoria “emerging” at pubertal onset. In addition, their own references do not establish that the behavior of gender dysphoria right when puberty begins determines how long gender dysphoria will continue, even for early onset gender dysphoria (Biggs, Citation2022b). Gender dysphoria present beyond puberty is not determinative either according to Cohen-Kettenis et al. (Citation2008), as they describe a group of adolescents where gender dysphoria did not persist, who “after long term assessment (which, depending on the degree of gender dysphoria and nonrelated pathology, could take a year or even longer) were not deemed eligible for early treatment, and they did not pursue SR [genital surgery] at later ages” (p. 1894). Rosenthal’s proposed milestone for identifying gender identity, upon which he claims medical intervention rests, is unsupported by the evidence he provides.
A. Eligibility criteria and expert lack of consensus
In addition, the medical intervention eligibility to which Rosenthal (Citation2021) refers is a major point of concern and disagreement among his expert colleagues. One of the most longstanding and important expert concerns in this field is avoiding medical intervention for those with transient gender dysphoria (creating “false positives” [Delemarre van de Waal & Cohen-Kettenis, Citation2006, p. S132; Terhune et al., Citation2022]). Thus the foundational (note the reliance upon it in Hembree et al., [Citation2017]) Dutch Protocol for youth medical transition tried to lower the likelihood of false positives by requiring pre-pubertal, early onset dysphoria (“lifelong extreme” [Delemarre van de Waal and Cohen-Kettenis, 2006, p. S131]), psychological stability, a supportive environment, and a firm grasp of reality and the limits of transition (Delemarre van de Waal & Cohen-Kettenis, 2006; de Vries & Cohen-Kettenis, Citation2012). In addition, social transition before endocrinological intervention was discouraged, due to fears it would solidify gender dysphoria that would have otherwise resolved. Another approach to try to reduce false positives involves exploration of the possible contribution of mental health or other factors to a given person’s gender dysphoria (Ayad et al., Citation2022; Edwards-Leeper & Anderson, Citation2021; Levine, Citation2021). There are medical intervention criteria as well in WPATH’s 7th “standards of care” (Coleman et al., 2012) to which Rosenthal (Citation2021) frequently refers, and in its update (Coleman et al., 2022). However, in a formal guideline review (Dahlen et al., Citation2021), ⅚ of the reviewers did not recommend the 2012 version (the last reviewer recommended only if modified) as a guideline, while the 2022 version is ‘prone to bias’ due to methods employed, with ‘recommendations that cannot yet be relied upon’ (Dahlen, Meads, & Bewley, Citation2022), and neither is “evidence-based” (Dahlen et al., Citation2022; Sinai, Citation2022).
Neither the Dutch protocol criteria nor any other have been shown to identify who might have good long-term outcomes without any medical and/or surgical interventions, who will require these interventions and who might be harmed by them. Thus the serious risk of medicalizing transient gender identity and creating false positives remains (Levine et al., Citation2022). Even though Rosenthal (Citation2021) includes a section on ethical dilemmas, he makes no mention of this crucial uncertainty regarding eligibility for medical intervention and the accompanying dilemma it poses. These issues underlie much of the disagreement between experts, which he also does not mention.
B. Neglect of mental health interventions and assumption of minority stress
In line with implying eligibility for medical intervention can be clearly identified, Rosenthal (Citation2021) equates his gender dysphoria “models of care” solely with medical intervention for those who are “eligible.” (The only alternative to medical intervention that Rosenthal, [Citation2021] appears to consider is no treatment, cautioning that the “stance of not intervening until more is known is not a neutral option” [p. 581].) Unsaid is that alternatives to “alignment of physical sex characteristics with gender identity” (p. 585) such as mental health interventions are sometimes successful at resolving gender dysphoria on their own. Even in Rosenthal’s (Citation2021) framing, such alternatives might be suitable for some of those “seeking medical services” mentioned at the beginning of the review, not all of whom can be assumed to be eligible for medical intervention. As several case studies link gender dysphoria to mental distress, autism spectrum disorders, etc. (Churcher-Clarke and Spiliadis, Citation2019; Evans, Citation2022; Withers, Citation2020), and given that a high fraction of young people currently present with comorbidities (Kaltiala-Heino et al., Citation2018), mental health based approaches might even be the most appropriate for many present-day gender dysphoria cases.
Instead, when touching on the topic of mental illness, Rosenthal (Citation2021) steers readers away from its possible contributing role to gender dysphoria, saying that being transgender “should no longer be considered a mental illness” (p. 581). He connects mental health challenges and gender dysphoria in the opposite direction, stating that “many of the mental health challenges faced by transgender youth are not intrinsic to being transgender, but rather are a consequence of such youth not feeling accepted for who they are” (p. 585). This minority stress assumption for mental health concerns is part of the affirmative model: “if there is pathology, it more often stems from cultural reactions (e.g., transphobia, homophobia, sexism) rather than from within the child” (Hidalgo et al., Citation2013, p. 285). The minority stress assumption sidelines the critical clinical question of to “what extent GD may be a reaction to a range of preceding psychosocial stressors” (Thompson, Gillberg, Wilson, Sarovic, & Sämfjord, Citation2022, p. 26; see also Kozlowska, Chudleigh, McClure, Maguire, & Ambler, Citation2021; Levine et al., Citation2022). Rosenthal (Citation2021) does note mental health evaluations may surface comorbidities, but then follows by suggesting how awareness and potential accessibility of medical intervention might have a positive impact: he does not mention that understanding the relation of these comorbidities to gender dysphoria may be relevant for determining suitable treatment (perhaps even revealing reasons to avoid medical intervention). Excluding consideration of underlying mental health issues as a possible developmental origin for gender dysphoria and suggesting only one source (minority stress) for mental health issues can create a bias that interferes with proper diagnosis, impeding or even precluding what may be the most appropriate treatment.
4. Medical interventions have been demonstrated to be effective and safe
Before turning to consequences of medical intervention, it is appropriate to first provide background regarding available evidence. Rosenthal (Citation2021) mentions the “relative paucity of outcomes data” (p. 581) and that “long-term safety and efficacy studies are needed to optimize care” (p. 589), but it is not only that the quantity of studies that is low or that care is not optimized, it is also that the quality is so low that the ability to make reliable outcome estimates is compromised.
In his review, Rosenthal (Citation2021) repeatedly refers to clinical guidelines and standards of care, which may give an impression of established, widely accepted, evidence-based protocols. The limitations of the WPATH guidelines (his “standards of care”, although WPATH themselves refer to them as guidelines [WPATH, EPATH, USPATH, AsiaPATH, CPATH, AusPATH, & PATHA., Citation2020; Malone, Hruz, Mason, Beck, et al:, Citation2021]) are described above. The Endocrine Society guidelines (Hembree et al., Citation2017), to which Rosenthal (Citation2021) also frequently refers, grade the evidence and report “low” and “very low” quality GRADE behind most of their own adolescent and childhood recommendations (three of the recommendations have ungraded supporting evidence, and moderate quality evidence backs the recommendation of counseling for fertility preservation). Low quality GRADE evidence means (Balshem et al., Citation2011, Table 2): “(o)ur confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect”. Very low quality GRADE is defined as “very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect.”
Other relevant evidence reviews have also been recently completed, some predating Rosenthal (Citation2021) but not mentioned by him. The UK National Institute for Health and Care Excellence (NICE) evidence reviews (2020a; 2020b; focusing on under 18's) found the quality of evidence for puberty blockers and cross sex hormones on gender dysphoria, mental health and quality of life for gender dysphoric youth to be very low certainty using modified GRADE. Sweden has independently found the scientific evidence insufficient to assess safety or efficacy (Swedish National Board of Health & Welfare, Citation2022), and after its own evidence review (Brignardello-Petersen & Wiercioch, Citation2022), Florida Medicaid (Citation2022) concluded that “(t)he available medical literature provides insufficient evidence that sex reassignment through medical intervention is a safe and effective treatment for gender dysphoria.” Likewise, a Cochrane review (Haupt et al., Citation2020, p. 2), “found insufficient evidence to determine the efficacy or safety of hormonal treatment approaches for transgender women in transition.”
A. Overstated mental health benefit of medical intervention
In spite of these low and very low quality/certainty evidence findings, Rosenthal (Citation2021) describes the research evidence as “compelling” (p. 581), saying it has “confirmed” (p. 586) and “demonstrated” (p. 581; p. 586, twice) the “clear” (p. 581, twice; p. 582), even “life-saving” (p. 581, twice; p. 586), benefit of medical intervention. If gender identity were fundamental, and medical intervention eligibility determination accurate, such outcomes might be expected. However, as listed above, multiple rigorous evidence reviews have found the available research evidence too limited to reliably estimate outcomes. (In particular, “life-saving” is an inaccurate claim and raises concerns of suggesting suicide to vulnerable populations [Levine et al., Citation2022].) Even before his review appeared, several of the papers Rosenthal (Citation2021) cites in support of his claims had already had their overall quality assessed as “poor” by the NICE evidence reviews (2020a; 2020b), and an attempt to reproduce one of his cited studies, de Vries, Steensma, Doreleijers, and Cohen-Kettenis (Citation2011), had already failed (Carmichael et al., Citation2021). Two others of his cited papers do not show cause and effect (Becker et al., Citation2018; Turban, King, Carswell, & Keuroghlian, Citation2020) and thus cannot demonstrate that the interventions caused a given outcome. His remaining reference is the 2014 de Vries et al. report of outcomes for the Dutch Protocol. This study evaluated 55 young people at least one year past final surgery (Rosenthal’s [Citation2021, p. 586] “prospective 6-year follow-up study”), and does not support his strong claims of benefit either.
It is worth elaborating further regarding de Vries et al. (Citation2014), given its prominence. As mentioned earlier, the Dutch Protocol criteria required psychological stability initially, and in this study participants continued to be psychologically stable, with a small mental health improvement. (However, ongoing mental health interventions might have confounded this result.) Their gender dysphoria was found to be much more improved after surgery, but this was confounded by de Vries et al. changing the evaluation questions after surgery. Before surgery, a natal girl would be asked how much they liked or hated being a girl and then, after surgery, how much they liked or hated being a boy (or vice versa for a natal boy), leading to a possible improvement just due to the change in assessment instrument (see more discussion in Levine et al., [Citation2022]). Furthermore, the only Dutch Protocol long term study outcome that appears to be available is of the very first transitioned teen (Cohen-Kettenis, Schagen, Steensma, de Vries, & Delemarre-van deWaal, Citation2011); at 22 years past the start of the process he had “dissatisfaction and shame about his genital appearance” (p. 845). Thus, in spite of being the foundation upon which youth transition rests, the Dutch Protocol is highly incomplete (see also Biggs, [Citation2022b] for more detailed analysis).
In addition, there is no reason to expect that even de Vries et al.’s (Citation2014) limited outcomes would apply to the current clinical population, most of whom would violate one or more of the Dutch Protocol eligibility criteria listed earlier. That is, most have late (pubertal and post-pubertal) onset gender dysphoria, frequently present with co-morbid and untreated mental health problems (Kaltiala-Heino et al., Citation2018), have families which might be in conflict, and their expectations of medical transition are often not backed by reality. (For adults, mental health improvement has not been demonstrated either: in a large recent study, after reanalysis of the data and correction, no advantage was found for either hormones or surgeries for any of their outcome measures [Bränström & Pachankis, Citation2020a; Citation2020b].)
Claims of mental health benefit from medical intervention are also often used to argue that a randomized controlled study would be unethical. Rosenthal (Citation2021) states: “While randomized controlled trials are often considered the gold standard, this approach to study hormonal interventions in TGD youth has not been considered feasible or ethical” (p. 588). While a randomized controlled trial might be difficult, for instance due to challenges in recruiting participants, it would not necessarily be unethical. The unethical thing may be the continuation of the “affirmative” medical and surgical path in light of all the questions and concerns that exist. A randomized controlled study would only be unethical if medical interventions were known to help and this is, despite Rosenthal’s (Citation2021) claims, not known.
B. Adverse physical outcomes for medical intervention
For puberty blockers, there is a dearth of studies regarding their adverse effects when used to treat gender dysphoria, as Rosenthal (Citation2021) notes. He reports some findings of bone mineral density harm (omitting a reanalysis [Biggs, Citation2021] which found worse outcomes), risks to fertility, and two inconclusive brain studies (one is a single case study finding an IQ drop of 10 points in 28 months). Rosenthal states that puberty blockers are “considered fully reversible” (p. 585), a commonly mentioned expectation based upon on-label use for precocious puberty, which may or may not carry over to off-label use with older gender dysphoric youth. However, he leaves unstated other adverse puberty blocker effects which similarly may or may not carry over from other uses, such as additional evidence for decreased IQ (Hayes, Citation2017; Mul et al., Citation2001), decreased male sexual desire (Turner & Briken, 2019), and (in animal studies) reduced maturity and long term impairment of spatial memory (Hough et al., Citation2017; Citation2019). If any such brain effects occur when treating gender dysphoria, they might interfere with a young person learning to make better decisions or better understand their body (Cass, Citation2022), perhaps undermining the frequently stated goal of using puberty blockers to “buy time.”
For cross sex hormones, Rosenthal (Citation2021) describes several of the risks as “mild”, concluding there are “in general, no clinically significant adverse effects with gender-affirming sex hormones” (Box 2, p. 587). (At another point he qualifies this statement [p. 588].) He does recommend counseling and gives details about fertility preservation for those about to start puberty blockers or hormones, but does not otherwise mention the risks of hormones to fertility. Also left out are the the risk of impaired sexual function accompanying the atrophy and histological changes to gonads (Cheng, Pastuszak, Myers, Goodwin, & Hotaling, Citation2019), the associated harm to bone mineral density (Delgado-Ruiz, Swanson, & Romanos, Citation2019), the observed shrinkage of the hippocampus (Gomez et al., 2020; Holmes, Citation2016, Pol et al., Citation2006), associated significant increases seen in strokes, venous thromboembolic events, and heart attacks (Getahun et al., Citation2018; Nota et al., Citation2019), associated large increase in multiple sclerosis (Pakpoor et al., Citation2013), and possibly increased rates of depression (Fuss et al., Citation2015). In addition, testosterone can lead to pain from vaginal and uterine atrophy (Obedin-Maliver, Citation2016) and estrogen even has an FDA box warning, the strongest warning a drug can receive, for its on-label uses (National Academies of Sciences, Engineering, and Medicine, et al., 2020). A shorter lifespan is also observed (de Blok et al., [Citation2021]; if followed by surgery, findings by Dhejne et al., [Citation2011] are also relevant). Some of these omitted risks appear on consent forms (see for example those from the University of Iowa Hospitals and Clinics [n.d.a; n.d.b]) and some appear in the long term as part of the (expected) lifetime use of hormones; all of these potential adverse effects omitted by Rosenthal (Citation2021) are relevant in order for a patient or their parents to give informed consent.
Rosenthal (Citation2021) does note the medications are off-label (as a challenge to care), but of course, off-label means that the FDA has not established that benefits outweigh the risks when any of these medications are used to treat gender dysphoria. In fact, an evidence review for treatment of adolescents by the Swedish National Board of Health and Welfare (Citation2022) found exactly the opposite: “The NBHW deems that the risks of puberty suppressing treatment with GnRH-analogues and gender-affirming hormonal treatment currently outweigh the possible benefits, and that the treatments should be offered only in exceptional cases” (p. 3).
Detransition does not represent medical harm and is rare
Although Rosenthal (Citation2021) mentions detransition, he does not mention that it might cause distress and even devastation. He presents only a positive anecdote of a single detransitioner, an adolescent who took puberty blockers for a year and then hormones for less than a year (Turban, Carswell, & Keuroghlian, Citation2018) and who “did not regret the decision […] feeling that their experience was vital to their consolidating their gender identity” (p. 586).
This benign detransition example is in stark contrast to the numerous detransitioner reports of debilitating regret found in the medical literature (D’Angelo, Citation2018; Evans, Citation2021; Withers, Citation2020) and online (Detrans Voices, n.d.). Sixty percent of the detransitioners in a recent peer reviewed study (a convenience sample [Vandenbussche, Citation2021]) reported needing help coping with feelings of regret and in Littman’s (Citation2021) convenience sample of detransitioners, “most respondents (64.6%) indicated that if they knew then what they know now, they would not have chosen to transition” (p. 3364). (Note that Vandenbussche, [Citation2021] also included 31% social transitioners.) The increasing numbers of detransitioners and their reported distress are spurring many of the calls for more research and increased caution regarding medical interventions in youth (Butler & Hutchinson, Citation2020; Evans, Citation2021; Griffin, Clyde, Byng, & Bewley, Citation2021; Levine et al., Citation2022; Malone, Citation2021).
Rosenthal also refers to detransition as “rare” (p. 586), which might be expected to hold if eligibility for medical intervention was appropriately determined, but it is in fact currently unknown how often false positives occur, how often people regret, or how often people try to undo or stop their medical interventions or otherwise detransition (Levine et al., Citation2022). Rosenthal (Citation2021) supports his assertion of rarity by saying there is a “relatively low” (p. 586) rate of discontinuation of medical intervention, citing studies which find those on puberty blockers tend to continue on to cross sex hormones. However, this says nothing about discontinuation rates of lifelong hormones. For instance, in one recent study, almost 30% of a group of teens and young adults who were receiving hormones appeared to discontinue them after 4 years (Roberts, Klein, Adirim, Schvey, & Hisle-Gorman, Citation2022). The discontinuation fraction in the group from this study might increase if followed up longer; for reference, depending on the sample population, medicalization criteria and intervention, the observed average or median observed times to regret or detransition in studies have ranged from 3 to 10 years (Dhejne, Öberg, Arver, & Landén, Citation2014; Littman, Citation2021; Vandenbussche, Citation2021; Wiepjes et al., Citation2018).
For specific numbers, Rosenthal (Citation2021) quotes a problematic low reported regret rate after gonadectomy of less than 1% for adults at a single clinic (Wiepjes et al., Citation2018). This study measured regret by searching clinic records for those who both reversed hormones after gonadectomy and expressed regret. The study lost track of 36% of the clinic patients, as they stopped coming for their lifetime treatment (which treats 95% of those in the Netherlands). It is unknown if these 36% restarted hormones elsewhere or discontinued entirely; for this and other reasons the study authors point out that their regret number might be inaccurate. Nonetheless, Rosenthal (Citation2021) quotes the <1% regret rate without including these qualifications.
More generally, regret underestimates are also likely because patients might not inform their clinicians; only 24% of detransitioners in Littman’s (Citation2021) convenience sample did so. Regret studies are often also inaccurate due to premature measurements of outcomes (sufficient time frames are suggested by the long observed regret times mentioned above), inappropriate measurement instruments and sample bias (D’Angelo, Citation2018; Expósito-Campos & D'Angelo, 2021). As detransition is a potential adverse outcome, it is important to report that the rate is unknown, rather than extremely small as claimed in Rosenthal (Citation2021).
Discussion
Currently, there is a dramatic rise in the number of young people seeking help for gender dysphoria and/or reporting trans-identification. There is a dearth of understanding of both gender dysphoria and how to best support young people dealing with it; Rosenthal (Citation2021) rightly recognizes there are “gaps in knowledge” (p. 589). Given the accompanying significant expert disagreements (including how to distinguish transient gender dysphoria), and one treatment option offering serious lifelong medical intervention with unclear outcomes and often irreversible consequences, decisions about treatment are fraught and ethical informed consent is crucial. Levine et al. (Citation2022) discuss how properly informed consent for the care of gender dysphoric and trans-identified young people is currently impeded by “erroneous professional assumptions; poor quality of the initial evaluations; and inaccurate and incomplete information shared with patients and their parents.”
These erroneous professional assumptions are in part caused by the many inaccurate or unsupported statements which have appeared in the peer-reviewed research literature, which often then get repeated and distorted (Clayton et al., 2021). For example, Cantor (Citation2020) found that Rafferty et al. (2018) misrepresented their cited evidence in order to support the adoption of the affirmative model by the American Academy of Pediatrics. Above, many omissions and limitations in the Nature review by Rosenthal (Citation2021) are discussed. These issues undercut the five key points upon which his review rests and could lead to inaccurate estimates of risks and benefits of medical intervention and a lack of awareness of (possibly more appropriate and less invasive) non-medical or psychiatric alternatives.
Many similar omissions and limitations are present in another review currently available only in preliminary form by Lee and Rosenthal (Citation2023). This second review quotes additional references for evidence of benefit, including a double mastectomy study with a too short (1–5 year) follow up time, high loss (28%) to follow up and an unvalidated scale, for improvement of “chest dysphoria.” In support of mental health improvement with medicalization, the second review quotes two additional recent papers which cannot show cause and effect (Green, DeChants, Price, & Davis [Citation2022] and Turban, King, Kobe, Reisner, & Keuroghlian [Citation2022], see Biggs, et al. [Citation2022a] for discussion of further limitations of Turban et al. [Citation2022]).
Beyond this second review, many of the issues highlighted in Rosenthal (Citation2021) are in common with statements and policies espoused by others who also emphasize medical intervention (sometimes along with social transition). The US HHS office of Population Affairs (Citation2022) and the American Academy of Pediatrics (Rafferty et al., 2018) also both fail to note that mental health or other noninvasive interventions may help gender dysphoria resolve even in the absence of medical intervention or social transition. Rosenthal’s (Citation2021) inaccurate claims that studies demonstrate mental health benefit of medical intervention are echoed widely (e.g, see the US HHS office of Population Affairs, [Citation2022] and AusPATH, [Citation2022]; the latter was rebutted by Clayton, et al., [Citation2022]). The Endocrine Society (Citation2020) position statement also downplays or omits many of the known serious physical dangers of medical intervention and also inaccurately claims evidence “demonstrating a durable biological element underlying gender identity” (see Malone, Hruz, Mason, Beck, et al. [Citation2021] for a rebuttal of many of its points). The regret and detransition rates are also inaccurately claimed to be low in section 5.7 of WPATH’s new version 8 guidelines (Coleman et al., 2022). These new version 8 WPATH guidelines also do not mention the NICE (Citation2020a; Citation2020b) evidence reviews, similar to Rosenthal (Citation2021); they also omit the Swedish (Swedish National Board of Health & Welfare, Citation2022) and Florida (Brignardello-Petersen & Wiercioch, Citation2022) evidence reviews appearing after Rosenthal (Citation2021) and state: “Therefore, a systematic review regarding outcomes of treatment in adolescents is not possible. A short narrative review is provided instead” (Coleman et al., 2022, p. S46).
This direct comparison of evidence in the research literature with Rosenthal (Citation2021), a review containing omissions and limitations also found in other prominent sources, may make it easier for practitioners, patients and their families to understand the current state of knowledge, including where uncertainties and controversies exist. In addition, it is hoped that more awareness of these uncertainties will increase support for follow-up studies of the large number of young people who have already begun lifetime medicalization, in order to capture outcomes at or beyond the observed average regret times, which range from 3 to 10 years in studies of different cohorts. Systematic outcome studies are badly needed. Similarly, the resolution of gender dysphoria via psychological intervention for some, who then avoid lifetime medicalization including risks to fertility, sexual function, and longevity, motivates support for studies to improve understanding and improvements to these non-medicalized and psychiatric approaches, and increased access to practitioners skilled in these methods (which may require increased training as well). And importantly, the substantial needs of detransitioners, a rapidly growing community, call for research as to how to help them, including psychological, medical and financial resources and community recognition and support.
There are serious challenges in deciding how to best support those currently suffering gender dysphoria, given how little is known about this complex condition. Accurately describing what the evidence currently says and does not say, and what further evidence is needed, is crucial.
Acknowledgements
I am grateful to the Editor, reviewers and several of my colleagues for their thoughtful and helpful criticisms and suggestions.
Disclosure statement
The author has previously communicated disagreement to Dr. Rosenthal about treatment protocols in his clinic.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- American College Health Association. (2021). American College Health Association-National College Health Assessment III: Undergraduate Student Reference Group Data Report Spring 2021. Boston: ACHA-NCHA III. https://www.acha.org/documents/ncha/NCHA-III_SPRING-2021_UNDERGRADUATE_REFERENCE_GROUP_DATA_REPORT.pdf
- American Psychiatric Association. What is Gender Dysphoria? (2020). Retrieved April 27, 2022 from https://www.psychiatry.org/patients-families/gender-dysphoria/what-is-gender-dysphoria
- Amicus Brief of Medical Groups, Brandt vs. Rutledge et al. (January 19, 2022). United States Court of Appeals for the Eighth Circuit, Appellate Case: 21-2875. Retrieved October 12, 2022 from https://www.aclu.org/legal-document/brandt-et-al-v-rutledge-et-al-amicus-brief-medical-groups
- Anderson, E. (2022a, January 3). Opinion: When it comes to trans youth, we’re in danger of losing our way. The San Francisco Examiner. Retrieved April 27, 2022 from http://www.sfexaminer.com/opinion/are-we-seeing-a-phenomenon-of-trans-youth-social-contagion/
- Anderson, E. (2022b, April 12). A transgender psychologist has helped hundreds of teenstransition. But rising numbers have her concerned. Los Angeles Times. Retrieved April 12, 2022 from https://www.latimes.com/world-nation/story/2022-04-12/a-transgender-psychologist-reckons-with-how-to-support-a-new-generation-of-trans-teens
- Arnoldussen, M., de Rooy, F.B.B., de Vries, A.L.C., van der Miesen, A. I. R., Popma, A., & Steensma, T. D. (2022). Demographics and gender-related measures in younger and older adolescents presenting to a gender service. European child & adolescent psychiatry. Advance online publication. doi:10.1007/s00787-022-02082-8
- AusPATH. (2022). Australian informed consent standards of care for gender affirming hormone treatment. Australia: Australian Professional Association for Trans Health. auspath.org.au
- Ayad, S., D’Angelo, R., Kenney, D., Levine, S.B., Marchiano, L., & O’Malley, S. (2022). A Clinical Guide for Therapists Working with Gender-Questioning Youth Version 1. Gender Exploratory Therapy Association. Retrieved December 2, 2022 from https://genderexploratory.com/wp-content/uploads/2022/12/GETA_ClinicalGuide_2022.pdf
- Bailey, M., & Blanchard R. (2017). Gender dysphoria is not one thing. 4thwavenow. RetrievedApril 29, 2022 from https://4thwavenow.com/2017/12/07/gender-dysphoria-is-not-one-thing/
- Balshem, H., Helfand, M., Schünemann, H. J., Oxman, A. D., Kunz, R., Brozek, J., Vist, G. E.,Falck-Ytter, Y., Meerpohl, J., Norris, S., & Guyatt, G. H. (2011). GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology, 64(4), 401–406. doi:10.1016/j.jclinepi.2010.07.015
- Bangalore Krishna, K. B., Fuqua, J. S., Rogol, A. D., Klein, K. O., Popovic, J., Houk, C. P.,Charmandari, E., & Lee, P. A. (2019). Use of gonadotropin-releasing hormone analogs in children: update by an international consortium. Hormone research in paediatrics, 91(6), 357–372. doi:10.1159/000501336
- Becker, I., Auer, M., Barkmann, C., Fuss, J., Möller, B., Nieder, T. O., Fahrenkrug, S.,Hildebrandt, T., & Richter-Appelt, H. (2018). A Cross-Sectional Multicenter Study of Multidimensional Body Image in Adolescents and Adults with Gender Dysphoria Before and After Transition-Related Medical Interventions. Archives of Sexual Behavior, 47(8), 2335–2347. doi:10.1007/s10508-018-1278-4
- Biggs, M. (2021). Revisiting the effect of GnRH analogue treatment on bone mineral density inyoung adolescents with gender dysphoria. Journal of Pediatric Endocrinology & Metabolism: JPEM, 34(7), 937–939. doi:10.1515/jpem-2021-0180
- Biggs, M. (2022a). Comment on Turban et al. 2022: Estrogen is associated with greater suicidality among transgender males, and puberty suppression is not associated with better mental health outcomes for either sex (Version 1). figshare. doi:10.6084/m9.figshare.19018868.v1
- Biggs, M. (2022b). The Dutch Protocol for Juvenile Transsexuals: Origins and Evidence.Journal of sex & marital therapy, 1–21. Advance online publication. doi:10.1080/0092623X.2022.2121238
- Blanchard, R. (1989). The concept of autogynephilia and the typology of male gender dysphoria.The Journal of Nervous and Mental Disease, 177(10), 616–623. doi:10.1097/00005053-198910000-00004
- Bockting, W. O. (1999). From construction to context: Gender through the eyes of thetransgendered. Siecus Report, 28(1), 3–7. Retrieved November 17, 200 from https://siecus.org/wp-content/uploads/2015/07/28-1.pdf
- Bockting, W. O., Knudson, G., & Goldberg, J. M. (2006). Counseling and Mental Health Carefor Transgender Adults and Loved Ones. International Journal of Transgenderism, 9(3-4), 35–82, doi:10.1300/J485v09n03_03
- Bränström, R., & Pachankis, J. E. (2020a). Reduction in mental health treatment utilizationamong transgender individuals after gender-affirming surgeries: A total population study. American Journal of Psychiatry, 177(8), 727–734. doi:10.1176/appi.ajp.2019.19010080
- Bränström, R., & Pachankis, J. E. (2020b). Correction to Bränström and Pachankis. (2020).American Journal of Psychiatry, 177(8), 734–734. doi:10.1176/appi.ajp.2020.1778correction
- Brignardello-Petersen, R., & Wiercioch, W. (2022). Effects of Gender Affirming Therapies in People with Gender Dysphoria: Evaluation of the Best Available Evidence. Agency for Health Care Administration Florida Medicaid Generally Accepted Professional Medical Standards Determination on the Treatment of Gender Dysphoria Attachment C. Retrieved Aug 2, 2022 from https://ahca.myflorida.com/letkidsbekids/docs/AHCA_GAPMS_June_2022_Attachment_C.pdf
- Butler, C., & Hutchinson, A. (2020). Debate: The pressing need for research and services forgender desisters/detransitioners. Child and Adolescent Mental Health. 25, 45–47. doi:10.1111/camh.12361
- Cantor, J. M. (2020). Transgender and Gender Diverse Children and Adolescents: Fact-Checking of AAP Policy. Journal of sex & marital therapy, 46(4), 307–313. doi:10.1080/0092623X.2019.1698481
- Carmichael, P., Butler, G., Masic, U., Cole, T. J., De Stavola, B. L., Davidson, S., Skageberg,E.M., Khadr, S., & Viner, R. M. (2021). Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PloS one, 16(2), e0243894. doi:10.1371/journal.pone.0243894
- Cass, H. (2021). Cass Review. Entry 5. Evidence and Epidemiology. Retrieved April 27, 2022from https://cass.independent-review.uk/entry-5-evidence-epidemiology-october-2021/
- Cass, H. (9 July 2022). Independent review of gender identity services for children and young people-further advice. Letter to John Stewart, National Director, Specialised Commissioning, NHS England. Retrieved September 26, 2022 from https://cass.independent-review.uk/wp-content/uploads/2022/07/Cass-Review-Letter-to-NHSE_19-July-2022.pdf
- Cass Review. (2022a). Independent review of gender identity services for children and young people: Interim report. Retrieved March 10, 2022 from https://cass.independent-review.uk/publications/interim-report/
- Cass Review. (2022b). Response to NHS England consultation: Draft interim servicespecification for specialist gender dysphoria services for children and young people. Retrieved December 7, 2022 from https://cass.independent-review.uk/wp-content/uploads/2022/12/Cass-Review-Consultation-Response-FINAL-SUBMSSION.pdf
- Cheng, P. J., Pastuszak, A. W., Myers, J. B., Goodwin, I. A., & Hotaling, J. M. (2019). Fertilityconcerns of the transgender patient. Translational Andrology and Urology, 8(3), 209–218. doi:10.21037/tau.2019.05.09
- Churcher Clarke, A., & Spiliadis, A. (2019). ‘Taking the lid off the box’: The value of extendedclinical assessment for adolescents presenting with gender identity difficulties. ClinicalChild Psychology and Psychiatry, 24(2), 338–352. doi:10.1177/1359104518825288
- Clayton, A. (2022). Commentary on Levine et al.: A Tale of Two Informed Consent Processes. Journal of sex & marital therapy, 1–8. Advance online publication. doi:10.1080/0092623X.2022.2070565
- Clayton, A., Malone, W. J., Clarke, P., Mason, J., & D'Angelo, R. (2022). Commentary: The Signal and the Noise-questioning the benefits of puberty blockers for youth with gender dysphoria-a commentary on Rew et al. (2021). Child and adolescent mental health, 27(3), 259–262. doi:10.1111/camh.12533
- Cohen-Kettenis, P. T., Delemarre-van de Waal, H. A., & Gooren, L. J. (2008). The treatment ofadolescent transsexuals: changing insights. The Journal of Sexual Medicine, 5(8), 1892–1897. doi:10.1111/j.1743-6109.2008.00870.x
- Cohen-Kettenis, P. T., Schagen, S. E., Steensma, T. D., de Vries, A. L., & Delemarre-van deWaal, H. A. (2011). Puberty suppression in a gender-dysphoric adolescent: a 22-year follow-up. Archives of Sexual Behavior, 40(4), 843–847. doi:10.1007/s10508-011-9758-9
- Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., DeCuypere, G., Feldman, J., Fraser, L., Green, J., Knudson, G., Meyer, W. J., Monstrey, S., Adler, R. K., Brown, G. R., Devor, A. H., Ehrbar, R., Ettner, R., Eyler, E., Garofalo, R., Karasic, D. H., … & Zucker, K. (2012). Standards of care for the health of transsexual, transgender, andgender-nonconforming people, version 7. International Journal of Transgenderism,13(4), 165–232. doi:10.1080/15532739.2011.700873
- Coleman, E., Radix, A. E., Bouman, W. P., Brown, G. R., de Vries, A. L. C., Deutsch, M. B., Ettner, R., Fraser, L., Goodman, M., Green, J., Hancock, A. B., Johnson, T.W.,Karasic, D. H., Knudson, G. A., Leibowitz, S.F., Meyer-Bahlburg, H. F. L., Monstrey, S. J., Motmans, J., Nahata, L., … & Arcelus, J. (2022). Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 23 (sup1), S1–S259, doi:10.1080/26895269.2022.2100644
- Council for Choices in Healthcare Finland (COHERE Finland). (June 16, 2020). Medicaltreatment methods for dysphoria associated with variations in gender identity in minors – recommendation. Retrieved Sep 23, 2022 from https://palveluvalikoima.fi/documents/1237350/22895008/Summary_minors_en+(1).pdf/fa2054c5-8c35-8492-59d6-b3de1c00de49/Summary_minors_en+(1).pdf
- Dahlen, S., Connolly, D., Arif, I., Junejo, M. H., Bewley, S., & Meads, C. (2021). Internationalclinical practice guidelines for gender minority/trans people: systematic review and quality assessment. BMJ Open, 11(4), e048943. doi:10.1136/bmjopen-2021-048943
- Dahlen, S., Meads, C., & Bewley, S. (October 21, 2022). WPATH Standards of Care: A new edition using outdated methods weakens the trustworthiness of content. Rapid Response. BMJ Open, 11(4), e048943. Retrieved November 10, 2022 from https://bmjopen.bmj.com/content/11/4/e048943.responses
- D’Angelo, R. (2018). Psychiatry’s ethical involvement in gender-affirming care. Australasian Psychiatry, 26(5), 460–463. doi:10.1177/1039856218775216
- de Graaf, N. M., Giovanardi, G., Zitz, C., & Carmichael, P. (2018). Sex Ratio in Children and Adolescents Referred to the Gender Identity Development Service in the UK (2009-2016). Archives of Sexual Behavior, 47(5), 1301–1304. doi:10.1007/s10508-018-1204-9
- Delemarre-Van De Waal, H. A., & Cohen-Kettenis, P. T. (2006). Clinical management of genderidentity disorder in adolescents: a protocol on psychological and paediatric endocrinology aspects. European Journal of Endocrinology, 155(suppl_1), S131–S137. doi:10.1530/eje.1.02231
- Delgado-Ruiz, R., Swanson, P., & Romanos, G. (2019). Systematic Review of the Long-TermEffects of Transgender Hormone Therapy on Bone Markers and Bone Mineral Density and Their Potential Effects in Implant Therapy. Journal of Clinical Medicine, 8(6), 784. doi:10.3390/jcm8060784
- DeTrans Voices, (n.d.). Retrieved April 29, 2022 from https://www.detransvoices.org/ de Vries, A.L., Cohen-Kettenis, P.T. (2012). Clinical management of gender dysphoria in children and adolescents: the Dutch approach. Journal of Homosexuality, 59(3):301–20.
- de Blok, C. J., Wiepjes, C. M., van Velzen, D. M., Staphorsius, A. S., Nota, N. M., Gooren, L. J.,Kreukels, B. P., & den Heijer, M. (2021). Mortality trends over five decades in adult transgender people receiving hormone treatment: a report from the Amsterdam cohort of gender dysphoria. The Lancet. Diabetes & Endocrinology, 9(10), 663–670. doi:10.1016/S2213-8587(21)00185-6
- de Vries, A. L., & Cohen-Kettenis, P. T. (2012). Clinical management of gender dysphoria in children and adolescents: the Dutch approach. Journal of Homosexuality, 59(3), 301–20.
- de Vries, A. L., McGuire, J. K., Steensma, T. D., Wagenaar, E. C., Doreleijers, T. A., & Cohen-Kettenis, P. T. (2014). Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics, 134(4), 696–704. doi:10.1542/peds.2013-2958
- de Vries, A. L., Steensma, T. D., Doreleijers, T. A., & Cohen-Kettenis, P. T. (2011). Pubertysuppression in adolescents with gender identity disorder: a prospective follow-up study. The Journal of Sexual Medicine, 8(8), 2276–2283. doi:10.1111/j.1743-6109.2010.01943.x
- Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L., Långström, N., & Landén, M. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PloS one, 6(2), e16885. doi:10.1371/journal.pone.0016885
- Dhejne, C., Öberg, K., Arver, S., & Landén, M. (2014). An analysis of all applications for sexreassignment surgery in Sweden, 1960-2010: prevalence, incidence, and regrets. Archives of Sexual Behavior, 43(8), 1535–1545. doi:10.1007/s10508-014-0300-8
- Edwards-Leeper, L., & Anderson, E.(2021, November 24). The mental health establishment isfailing trans kids. Washington Post. Retrieved April 24, 2022 from https://www.washingtonpost.com/outlook/2021/11/24/trans-kids-therapy-psychologist/
- Endocrine Society. (December 16, 2020). Transgender Health: An Endocrine Society Position Statement. Retrieved September 29, 2022 from https://www.endocrine.org/advocacy/position-statements/transgender-health.
- Evans, M. (2021). Freedom to think: The need for thorough assessment and treatment of genderdysphoric children. BJPsych Bulletin, 45(5), 285–290. doi:10.1192/bjb.2020.72
- Evans, S., & Evans, M. (2021). Gender Dysphoria: A Therapeutic Model for Working with Children, Adolescents and Young Adults. Oxfordshire: Phoenix Publishing House.
- Evans, M. (2022). ‘If only I were a boy …’: Psychotherapeutic Explorations of Transgender inChildren and Adolescents. British Journal of Psychotherapy, 38, 269–285. doi:10.1111/bjp.12733
- Florida Medicaid. (2022). Generally Accepted Professional Medical Standards Determinationon the Treatment of Gender Dysphoria. Retrieved June 6, 2022 from https://ahca.myflorida.com/letkidsbekids/docs/AHCA_GAPMS_June_2022_Report.pdf
- Frigerio, A., Ballerini, L., & Valdés Hernández, M. (2021). Structural, Functional, and Metabolic Brain Differences as a Function of Gender Identity or Sexual Orientation: A Systematic Review of the Human Neuroimaging Literature. Archives of sexual behavior, 50(8), 3329–3352. doi:10.1007/s10508-021-02005-9
- French National Academy of Medicine. (2022). Medicine and gender transidentity in childrenand adolescents, Retrieved November 17, 2022 from https://www.academie-medecine.fr/la-medecine-face-a-la-transidentite-de-genre-chez-les-enfants-et-les-adolescents/?lang=en
- Fuss, J., Hellweg, R., Van Caenegem, E., Briken, P., Stalla, G. K., T’Sjoen, G., & Auer, M. K.(2015). Cross-sex hormone treatment in male-to-female transsexual persons reduces serum brain-derived neurotrophic factor (BDNF). European Neuropsychopharmacology: the Journal of the European College of Neuropsychopharmacology, 25(1), 95–99. doi:10.1016/j.euroneuro.2014.11.019
- Getahun, D., Nash, R., Flanders, W. D., Baird, T. C., Becerra-Culqui, T. A., Cromwell, L., Hunkeler, E., Lash, T. L., Millman, A., Quinn, V. P., Robinson, B., Roblin, D., Silverberg, M. J., Safer, J., Slovis, J., Tangpricha, V., & Goodman, M. (2018). Cross-sex Hormones and Acute Cardiovascular Events in Transgender Persons: A Cohort Study. Annals of Internal Medicine, 169(4), 205–213. doi:10.7326/M17-2785
- Ghorayshi, A. (November 4, 2022). Florida Restricts Doctors From Providing Gender Treatments to Minors. The New York Times. Retrieved November 13 from https://www.nytimes.com/2022/11/04/health/florida-gender-care-minors-medical-board.html
- Gómez, Á., Cerdán, S., Pérez-Laso, C., Ortega, E., Pásaro, E., Fernández, R., Gómez-Gil, E., Mora, M., Marcos, A., Del Cerro, M., & Guillamon, A. (2020). Effects of adult male rat feminization treatments on brain morphology and metabolomic profile. Hormones and behavior, 125, 104839. doi:10.1016/j.yhbeh.2020.104839
- Green, A. E., DeChants, J. P., Price, M. N., & Davis, C. K. (2022). Association of Gender-Affirming Hormone Therapy With Depression, Thoughts of Suicide, and Attempted Suicide Among Transgender and Nonbinary Youth. The Journal of adolescent health: official publication of the Society for Adolescent Medicine, 70(4), 643–649. doi:10.1016/j.jadohealth.2021.10.036
- Griffin, L., Clyde, K., Byng, R., & Bewley, S. (2021). Sex, gender and gender identity: Are-evaluation of the evidence. BJPsych Bulletin, 45(5), 291–299. doi:10.1192/bjb.2020.73
- Haupt, C., Henke, M., Kutschmar, A., Hauser, B., Baldinger, S., Saenz, S. R., & Schreiber, G. (2020). Antiandrogen or estradiol treatment or both during hormone therapy intransitioning transgender women. Cochrane Database of Systematic Reviews, (11). doi:10.1002/14651858.CD013138.pub2
- Hayes, P. (2017). Commentary: Cognitive, Emotional, and Psychosocial Functioning of Girls Treated with Pharmacological Puberty Blockage for Idiopathic Central Precocious Puberty. Frontiers in Psychology, 8, 44. doi:10.3389/fpsyg.2017.00044
- Hembree, W. C., Cohen-Kettenis, P. T., Gooren, L., Hannema, S. E., Meyer, W. J., Murad, M. H., Rosenthal, S. M., Safer, J. D., Tangpricha, V., & T'Sjoen, G. G. (2017). Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology and Metabolism, 102(11), 3869–3903. doi:10.1210/jc.2017-01658
- HHS office of Population Affairs. (March 2, 2022). Gender-Affirming Care and Young People. Retrieved September 29, 2022 from https://opa.hhs.gov/sites/default/files/2022-03/gender-affirming-care-young-people-march-2022.pdf
- Hidalgo, M.A., Ehrensaft, D., Tishelman, A.C., Clark, L.F., Garofalo, R., Rosenthal, S.M., Spack, N.P., & Olson, J. (2013).The Gender Affirmative Model: What We Know and What We Aim to Learn. Human Development, (56), 285–290. doi:10.1159/000355235
- Holmes, D. (2016). Cross-sex hormones alter grey matter structures. Nat Rev Endocrinol, 12, 686. doi:10.1038/nrendo.2016.177
- Hough, D., Bellingham, M., Haraldsen, I. R., McLaughlin, M., Robinson, J. E., Solbakk, A. K., & Evans, N. P. (2017). A reduction in long-term spatial memory persists after discontinuation of peripubertal GnRH agonist treatment in sheep. Psychoneuroendocrinology, 77, 1–8. doi:10.1016/j.psyneuen.2016.11.029
- Hough, D., Robinson, J. E., Bellingham, M., Fleming, L. M., McLaughlin, M., Jama, K., Haraldsen, I., Solbakk, A. K., & Evans, N. P. (2019). Peripubertal GnRH and testosterone co-treatment leads to increased familiarity preferences in male sheep. Psychoneuroendocrinology, 108, 70–77. doi:10.1016/j.psyneuen.2019.06.008
- Kaltiala-Heino, R., Bergman, H., Työläjärvi, M., & Frisén, L. (2018). Gender dysphoria inadolescence: current perspectives. Adolescent Health, Medicine and Therapeutics, 9, 31–41. doi:10.2147/AHMT.S135432
- Kozlowska, K., Chudleigh, C., McClure, G., Maguire, A. M., & Ambler, G. R. (2021). Attachment Patterns in Children and Adolescents with Gender Dysphoria. Frontiers in Psychology, 11, Article 582688. doi:10.3389/fpsyg.2020.582688
- Lee, J. Y., & Rosenthal, S. R. (2023). Gender-Affirming Care of Transgender and Gender-Diverse Youth: Current Concepts. Annual Review of Medicine, 74, 1. doi:10.1146/annurev-med-043021-032007
- Lemma, A. (2018). Trans-itory identities: some psychoanalytic reflections on transgender identities. The International journal of psycho-analysis, 99(5), 1089–1106. doi:10.1080/00207578.2018.1489710
- Levine, S. B. (2018). Transitioning Back to Maleness. Archives of sexual behavior, 47(4), 1295–1300. doi:10.1007/s10508-017-1136-9
- Levine, S. B. (2021). Reflections on the Clinician's Role with Individuals Who Self-identify as Transgender. Archives of sexual behavior, 50(8), 3527–3536. doi:10.1007/s10508-021-02142-1
- Levine, S. B., Abbruzzese, E., & Mason, J. W. (2022). Reconsidering Informed Consent forTrans-Identified Children, Adolescents, and Young Adults. Journal of Sex & Marital Therapy. 1–22. Advance online publication. doi:10.1080/0092623X.2022.2046221
- Littman, L. (2018). Parent reports of adolescents and young adults perceived to show signs of arapid onset of gender dysphoria. PloS one, 13(8), e0202330. doi:10.1371/journal.pone.0202330
- Littman, L. (2019). Correction: Parent reports of adolescents and young adults perceived to showsigns of a rapid onset of gender dysphoria. PloS one, 14(3), e0214157. doi:10.1371/journal.pone.0214157
- Littman, L. (2020). The Use of Methodologies in Littman (2018) Is Consistent with the Use ofMethodologies in Other Studies Contributing to the Field of Gender Dysphoria Research: Response to Restar (2019). Archives of Sexual Behavior, 49(1), 67–77. doi:10.1007/s10508-020-01631-z
- Littman, L. (2021). Individuals Treated for Gender Dysphoria with Medical and/or SurgicalTransition Who Subsequently Detransitioned: A Survey of 100 Detransitioners. Archives of Sexual Behavior, 50(8), 3353–3369. doi:10.1007/s10508-021-02163-w
- Malone, W. (2021 Sep 17). Time to Hit Pause on ‘Pausing’ Puberty in Gender-Dysphoric Youth.Medscape. Retrieved April 22, 2022 from https://www.medscape.com/viewarticle/958742
- Malone, W. J., Hruz, P. W., Mason, J. W., & Beck, S. (2021). Letter to the Editor from William J. Malone et al: “Proper Care of Transgender and Gender-diverse Persons in the Setting of Proposed Discrimination: A Policy Perspective”. The Journal of clinical endocrinology and metabolism, 106(8), e3287–e3288. doi:10.1210/clinem/dgab205
- Marchiano, L. (2017) Outbreak: On Transgender Teens and Psychic Epidemics, PsychologicalPerspectives, 60(3), 345–366, doi:10.1080/00332925.2017.1350804
- Marek, S., Tervo-Clemmens, B., Calabro, F. J., Montez, D. F., Kay, B. P., Hatoum, A. S., Donohue, M. R., Foran, W., Miller, R. L., Hendrickson, T. J., Malone, S. M., Kandala, S., Feczko, E., Miranda-Dominguez, O., Graham, A. M., Earl, E. A., Perrone, A. J., Cordova, M., Doyle, O., Moore, L. A., … & Dosenbach, N. U. F. (2022). Reproducible brain-wide association studies require thousands of individuals. Nature, 603(7902), 654–660. doi:10.1038/s41586-022-04492-9
- Mul, D., Versluis-den Bieman, H., Slijper, F., Oostdijk, W., Waelkens, J., & Drop, S. (2001). Psychological assessments before and after treatment of early puberty in adopted children. Acta Paediatrica, 90, 965–971. doi:10.1111/j.1651-2227.2001.tb01349.x
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division;Board on Health Sciences Policy, Committee on the Clinical Utility of Treating Patients with Compounded Bioidentical Hormone Replacement Therapy. (2020 July 1). Appendix H Boxed warnings on U.S. Food and Drug Administration–approved estrogen and testosterone products. In L. M. Jackson, R. M. Parker, & D. R. Mattison, (Eds.), The Clinical Utility of Compounded Bioidentical Hormone Therapy: A Review of Safety, Effectiveness, and Use. Washington (DC): National Academies Press (US); Retrieved May 2, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK562883/.
- National Institute for Health and Care Excellence (NICE). (2020a). Evidence review: Gonadotrophin releasing hormone analogues for children and adolescents with gender dysphoria. Retrieved May October 14, 2022 from https://cass.independent-review.uk/wp-content/uploads/2022/09/20220726_Evidence-review_GnRH-analogues_For-upload_Final.pdf
- National Institute for Health and Care Excellence (NICE). (2020b). Evidence review: Gender-affirming hormones for children and adolescents with gender dysphoria. Retrieved October 14, 2022 from https://cass.independent-review.uk/wp-content/uploads/2022/09/20220726_Evidence-review_Gender-affirming-hormones_For-upload_Final.pdf
- NHS England. (October 20, 2022). Interim service specification: Specialist service for children and young people with gender dysphoria (phase 1 providers). Publication reference: PR1937_i. Retrieved October 29, 2022 from https://www.engage.england.nhs.uk/specialised-commissioning/gender-dysphoria-services/user_uploads/b1937-ii-specialist-service-for-children-and-young-people-with-gender-dysphoria-1.pdf
- Nota, N. M., Wiepjes, C. M., de Blok, C., Gooren, L., Kreukels, B., & den Heijer, M. (2019).Occurrence of Acute Cardiovascular Events in Transgender Individuals Receiving Hormone Therapy. Circulation, 139(11), 1461–1462. doi:10.1161/CIRCULATIONAHA.118.038584
- Obedin-Malover, J. (2016). Pelvic pain and persistent menses in transgender men. UCSFTransgender Care. Retrieved April 26, 2022 from https://transcare.ucsf.edu/guidelines/pain-transmen
- Pakpoor, J., Disanto, G., Gerber, J. E., Dobson, R., Meier, U. C., Giovannoni, G., &Ramagopalan, S. V. (2013). The risk of developing multiple sclerosis in individuals seronegative for Epstein-Barr virus: a meta-analysis. Multiple Sclerosis (Houndmills, Basingstoke, England), 19(2), 162–166. doi:10.1177/1352458512449682
- Parkinson, J. (2014). Gender dysphoria in Asperger’s syndrome: a caution. Australasian Psychiatry: Bulletin of Royal Australian and New Zealand College of Psychiatrists, 22(1), 84–85. doi:10.1177/1039856213497814
- Pol, H. E. H., Cohen-Kettenis, P. T., Van Haren, N. E. M., Peper, J. S., Brans, R. G. H., Cahn, W.,Schnack, H. G., Gooren, L. J. G., & Kahn, R. S. (2006). Changing your sex changes your brain: influences of testosterone and estrogen on adult human brain structure. European Journal of Endocrinology, 155(suppl_1), S107–S114. https://eje.bioscientifica.com/view/journals/eje/155/suppl_1/1550107.xml doi:10.1530/eje.1.02248
- Polderman, T., Kreukels, B., Irwig, M. S., Beach, L., Chan, Y. M., Derks, E. M., Esteva, I., Ehrenfeld, J., Heijer, M. D., Posthuma, D., Raynor, L., Tishelman, A., Davis, L. K., & International Gender Diversity Genomics Consortium (2018). The Biological Contributions to Gender Identity and Gender Diversity: Bringing Data to the Table. Behavior Genetics, 48(2), 95–108. doi:10.1007/s10519-018-9889-z
- Rafferty, J., Committee On Psychosocial Aspects Of Child And Family Health, Committee On Adolescence, & Section On Lesbian, Gay, Bisexual, And Transgender Health And Wellness (2018). Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents. Pediatrics, 142(4), e20182162. doi:10.1542/peds.2018-2162
- Ristori, J., & Steensma, T. D. (2016). Gender dysphoria in childhood. International Review ofPsychiatry, 28(1), 13–20. doi:10.3109/09540261.2015.1115754
- Roberts, C. M., Klein, D. A., Adirim, T. A., Schvey, N. A., & Hisle-Gorman, E. (2022). Continuation of gender-affirming hormones among transgender adolescents and adults. The Journal of clinical endocrinology and metabolism, dgac251. Advance online publication. doi:10.1210/clinem/dgac251
- Rosenthal, S. M. (2021). Challenges in the care of transgender and gender-diverse youth: anendocrinologist's view. Nature Reviews. Endocrinology, 17(10), 581–591. doi:10.1038/s41574-021-00535-9
- Schwartz, D. (2021). Clinical and Ethical Considerations in the Treatment of Gender DysphoricChildren and Adolescents: When Doing Less Is Helping More. Journal of Infant, Child, and Adolescent Psychotherapy, (20) 4, 439–449. doi:10.1080/15289168.2021.1997344
- Sinai, J. (2022). The current gender-affirming care model in BC is unvalidated and outdated. BCMedical Journal, 64 (3), 106. https://bcmj.org/letters/current-gender-affirming-care-model-bc-unvalidated-and-outdated
- Singh, D., Bradley, S. J., & Zucker, K. J. (2021). A Follow-Up Study of Boys With GenderIdentity Disorder. Frontiers in Psychiatry, 12, 287. doi:10.3389/fpsyt.2021.632784
- Swedish National Board of Health and Welfare. (2022). Care of children and adolescents withgender dysphoria. Summary. Retrieved April 23, 2022 from https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/kunskapsstod/2022-3-7799.pdf
- Terhune, C., Respaut, R., & Conlin, M. (October 6, 2022). As more transgender children seek medical care, families confront many unknowns. Reuters investigates. Retrieved October 9, 2022 from https://www.reuters.com/investigates/special-report/usa-transyouth-care/
- Thompson, L., Gillberg, C., Wilson, P., Sarovic, D., & Sämfjord, A. (2022). A PRISMAsystematic review of adolescent gender dysphoria literature: mental health. PLOS Global Public Health 2(5)m e0000426. doi:10.1371/journal.pgph.0000426
- Turban, J. L., Carswell, J., & Keuroghlian, A. S. (2018). Understanding Pediatric Patients Who Discontinue Gender-Affirming Hormonal Interventions. JAMA pediatrics, 172(10), 903–904. doi:10.1001/jamapediatrics.2018.1817
- Turban, J. L., King, D., Carswell, J. M., & Keuroghlian, A. S. (2020). Pubertal Suppression forTransgender Youth and Risk of Suicidal Ideation. Pediatrics, 145(2), e20191725. doi:10.1542/peds.2019-1725
- Turban, J. L., King, D., Kobe, J., Reisner, S. L., & Keuroghlian, A. S. (2022). Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PloS one, 17(1), e0261039. doi:10.1371/journal.pone.0261039
- Turner, D., & Briken, P. (2018). Treatment of Paraphilic Disorders in Sexual Offenders or MenWith a Risk of Sexual Offending With Luteinizing Hormone-Releasing Hormone Agonists: An Updated Systematic Review. The Journal of Sexual Medicine, 15(1), 77–93. doi:10.1016/j.jsxm.2017.11.013
- University of Iowa Hospitals and Clinics. (n.d.a). Transgender Hormone Therapy -‐ TestosteroneInformed Consent. Retrieved September 1, 2022 from https://uihc.org/sites/default/files/2022-07/sample_uihc_informed_consent_masculinizing_0.pdf
- University of Iowa Hospitals and Clinics. (n.d.b). Transgender Hormone Therapy -‐ EstrogenInformed Consent. Retrieved September 1, 2022, from https://uihc.org/sites/default/files/2022-07/samle_uihc_informed_consent_feminizing_0.pdf
- Vandenbussche, E. (2021). Detransition-related needs and support: A cross-sectional onlinesurvey. Journal of Homosexuality, 1–19. doi:10.1080/00918369.2021.1919479
- Vrouenraets, L. J., Fredriks, A. M., Hannema, S. E., Cohen-Kettenis, P. T., & de Vries, M. C.(2015). Early Medical Treatment of Children and Adolescents With Gender Dysphoria: An Empirical Ethical Study. The Journal of Adolescent Health: Official Publication of The Society for Adolescent Medicine, 57(4), 367–373. doi:10.1016/j.jadohealth.2015.04.004
- Wiepjes, C. M., Nota, N. M., de Blok, C., Klaver, M., de Vries, A., Wensing-Kruger, S. A., deJongh, R. T., Bouman, M. B., Steensma, T. D., Cohen-Kettenis, P., Gooren, L., Kreukels, B., & den Heijer, M. (2018). The Amsterdam Cohort of Gender Dysphoria Study (1972-2015): Trends in Prevalence, Treatment, and Regrets. The Journal of Sexual Medicine, 15(4), 582–590. doi:10.1016/j.jsxm.2018.01.016
- Withers, R. (2020). Transgender medicalization and the attempt to evade psychological distress.The Journal of Analytical Psychology, 65(5), 865–889. doi:10.1111/1468-5922.12641
- WPATH, EPATH, USPATH, AsiaPATH, CPATH, AusPATH, & PATHA. (December 1, 2020).Statement Regarding Medical Affirming Treatment including Puberty Blockers for Transgender Adolescents. Retrieved September 23, 2022 from https://www.wpath.org/media/cms/Documents/Public%20Policies/2020/FINAL%20Statement%20Regarding%20Informed%20Consent%20Court%20Case_Dec%2016%202020.docx.pdf
- Zucker, K. J. (2017). Epidemiology of gender dysphoria and transgender identity. Sexual Health, 14(5), 404–411. doi:10.1071/SH17067
