ABSTRACT
Using data from Understanding Society, this paper provides a comprehensive account of the associations between ethnic and racial harassment (ERH), mental health and ethnic attachment for ethnic minorities living in England. We find an association between ERH and poor mental health measured using GHQ for ethnic minorities, even after controlling for a rich array of individual and area level characteristics. We find that ethnic attachment, measured as ethnic identity and co-ethnic friendship ties, moderates this association but solely for UK born ethnic minorities. In contrast to previous research, we further find that living in areas of high co-ethnic concentration appears to exacerbate the association between ERH and mental ill-health.
Introduction
In the UK, surveys have documented ethnic and racial harassment (ERH hereafter) and discrimination experienced by ethnic minorities since the 1960s (Daniel Citation1968; Virdee Citation1997; Nandi, Luthra, and Benzeval Citation2016). Recent evidence shows that around 10 per cent of adults across ethnic minority groups in England report physical or verbal attacks in a public place due to their ethnicity, nationality or religion. It is also well established that ERH is associated with poorer health outcomes, particularly mental health, in the UK (Wallace, Nazroo, and Bécares Citation2016; Becares, Nazroo, and Stafford Citation2009; Becares et al. Citation2012; Karlsen et al. Citation2005; Karlsen and Nazroo Citation2002; Halpern and Nazroo Citation1999) and elsewhere (Becares et al. Citation2012; Paradies Citation2006; Veling et al. Citation2007). Given the high and increasing prevalence of ERH in the UK, other European countries, US and Canada (FRA Citation2018; FBI Citation2017; Nandi, Luthra, and Benzeval Citation2016), it is important to seek potential protective factors that may reduce the negative impact of ERH on mental health. Drawing on a larger body of literature on the well-being of minorities in the UK, we posit that ethnic attachment may provide protection for minorities experiencing ERH.
Our study improves upon previous research on ERH, ethnic attachment and mental health in two respects. First, using the rich data in Understanding Society, our study examines a wide range of measures of ethnic attachment, including ethnic identity and co-ethnic social ties, as well as the ethnic composition of the local neighbourhood. These data also include a wider set of social and demographic characteristics than the current evidence base, allowing us to better control for potential confounders of the relationship between ERH and mental health. Second, our work takes into account the fact that the composition of the minority population is changing in the UK (and other western countries): as of the 2011 Census, over 40 per cent of those reporting an Asian identity, and nearly half of those reporting a Black minority identity, were UK born. Building on recent work which demonstrates important differences in mental health and its correlates by immigrant generation (Dorsett, Rienzo, and Weale Citation2019), we investigate whether the moderating impact of ethnic attachment on the association between ethnic and racial harassment and mental health differs across generations (UK born and foreign-born minorities).
Background
Ethnic and racial harassment and mental health
Research has found consistently high levels of ERH and discrimination experienced by ethnic minorities since the 1960s in the UK (Daniel Citation1968; Virdee Citation1997; Nandi, Luthra, and Benzeval Citation2016; FBI Citation2017; FRA Citation2018), corroborated with evidence from qualitative studies among Caribbean, African, and South Asian populations documenting “everyday encounters with interpersonal racism in public spaces, on the streets, in stores” (Foner Citation2018, 1115; Poynting and Mason Citation2007; Stevens, Hussein, and Manthorpe Citation2012). The most recent survey data finds that in 2009/2010, around 10 per cent of adults across ethnic minority groups in England reported physical or verbal attacks in a public place due to their ethnicity, nationality or religion (Nandi, Luthra, and Benzeval Citation2016).
Research on the mental health consequences of ERH demonstrates a strong link between the two: qualitative and clinical studies consistently find that discrimination is associated with indicators of mental health such as nonspecific stress, psychological wellbeing and perceptions of mastery and control (Williams, Neighbors, and Jackson Citation2003). Racial discrimination leads to stress both when experienced interpersonally as well as when experiences of discrimination in housing, healthcare and the labour market result in worse socio-economic opportunities (Karlsen and Nazroo Citation2002). Existing research on ethnic minorities based on Understanding Society (2009), EMPIRIC (2000) and FNSEM (1994) surveys, have clearly established that even after controlling for indirect channels, via statistical adjustments of socio-economic status or social class, there is an association between ERH (and in some cases employment discrimination) and poorer mental health (Wallace, Nazroo, and Bécares Citation2016; Becares, Nazroo, and Stafford Citation2009; Karlsen et al. Citation2005; Karlsen and Nazroo Citation2002; Halpern and Nazroo Citation1999). In this study, we also estimate the association between ERH and mental health but acknowledge potential heterogeneity among ethnic minorities by place of birth and control for a wider range of potential confounders.
Potential confounders: local environment, socio-demographic characteristics and personality
Although it is impossible to establish an indisputable causal relationship between ERH and mental health with observational data, by controlling for a large array of individual and contextual variables that may be correlated with both mental health and ERH, we seek to reduce the influence of omitted variables which may bias our results. For instance, individuals living in disadvantaged areas may be more at risk of experiencing ERH and suffer poorer mental health (Karlsen and Nazroo Citation2002). Similarly individuals of lower socio-economic status experience a range of stressors which negatively impact their mental health; as they may also be more reliant on public transport and frequent public spaces more, they also experience a higher risk of exposure to ERH. We also anticipate that individuals with higher levels of neuroticism, a personality trait, will be more likely to perceive and report ERH as well as experience poorer mental health. Subjective wellbeing has been found to be associated with personality traits (Diener and Lucas Citation1999; Boyce Citation2010) and some researchers recommend that personality should be used to account for individual traits in models of wellbeing (Carbonell-i-Ferreri and Frijjters Citation2004). We believe this may also be true for measures of mental ill-health and hence include our results both before and after the addition of personality traits as controls.
It may also be the case that individuals who are more likely to experience greater stress and anxiety may also be more likely to perceive treatment as discriminatory and to report it (reverse causality). While we cannot control for all potential confounders nor completely rule out reverse causality, this study improves upon previous research, most of which was based on older data from the 1990s, by including controls above the usual socio-economic and demographic indicators.
Ethnic attachment
We also assess the potentially “buffering” impact of ethnic attachment in reducing the association between ERH and mental health. Researchers posit that there are individual, social, cultural and environmental factors that may moderate the relationship between socio-economic disadvantage, discrimination and mental health (Friedli Citation2009). Such factors could be resources available to the individual or behavioural practices they engage in. Drawing from a more general literature on ethnic inequality (Mossakowski Citation2003; Rumbaut Citation1994), much of the research on resilience or protective factors for ethnic minorities has focused on indicators of ethnic attachment.
Ethnic attachment is loosely defined as a strong affiliation with, or social embeddedness within, the co-ethnic community (Maliepaard, Lubbers, and Gijsberts Citation2010). Some studies of ethnic minorities in the UK (Heim, Hunter, and Jones Citation2011) and the USA (Phinney et al. Citation2001; Mossakowski Citation2003) have found that a strong identification with one’s ethnic culture can provide a sense of belonging and positive self-concept, which protects individuals from the mental health consequences of discrimination and ERH. However, American studies have demonstrated that this buffering effect varies across different minority groups (Pascoe and Smart Richman Citation2009) and is stronger among the foreign born, rather than the US born (Mossakowski et al. Citation2019). A smaller-scale study, focusing on 174 young minority members in the UK, found that the buffering impact of ethnic identity did not hold for those raised in the UK (Howe, Heim, and O'Connor Citation2014, 2471): “Racism, identity and psychological well-being are interrelated but the nature of their relation changes, with length of residence in adopted countries and experiences with their institutions (especially educational institutions with young people) highlighted as potentially significant.”
Another form of ethnic attachment is social connections to those of the same ethnicity (co-ethnics). The relationship between social disconnectedness, perceived isolation and poor physical and mental health is well documented for the general population (Berry et al. Citation1987; Richards Citation2016), but less is known about ethnic minorities. There is some evidence that co-ethnic friendships can offer a deeper, stronger source of support for ethnic minorities, than other friendships, which may be particularly helpful when facing ERH (Byng Citation1998). For instance, Reynolds (Citation2007) documents the value of shared experiences and values within same ethnic friendships for Caribbean origin minorities in the UK. On the other hand, a recent study of South Asian youth in London found that cross-group ties, particularly to majority group members, offered greater protection for minority group members facing discrimination (Bagci et al. Citation2017).
Partially due to a lack of data of ethnic attachment, much of the quantitative literature on ethnic attachment focuses on ethnic density, specifically the proportion of co-ethnic residents in the local area (various geographies are used). The positive association between the proportion of co-ethnic residents in an area and mental health is often referred to as the ethnic density effect and is theorized to derive from enhanced social cohesion, mutual social support, a stronger sense of community and belongingness (Becares, Nazroo, and Stafford Citation2009; Becares et al. Citation2012) and lower acculturation stress (Schofield et al. Citation2017). Living in areas of high ethnic density is also expected to lower exposure to ERH due to lesser likelihood of contact with majority group members (Halpern and Nazroo Citation1999; Becares, Nazroo, and Stafford Citation2009; Dustmann, Fabbri, and Preston Citation2011), and to “buffer” its impact on health when it does occur (Becares, Nazroo, and Stafford Citation2009; Karlsen and Nazroo Citation2002; Pickett and Wilkinson Citation2008). There is also evidence of considerable heterogeneity in the ethnic density effect, both by the characteristics of the neighbourhoods themselves (Becares et al. Citation2012) and between the UK and foreign born (Dorsett, Rienzo, and Weale Citation2019; Schofield et al. Citation2017).
Generation status, harassment and health
A final contribution of this paper is to differentiate between foreign born (first generation) and UK born ethnic minorities (second+ generation) when examining the relationship between ERH, mental health and ethnic attachment (Dorsett, Rienzo, and Weale Citation2019; Nandi, Luthra, and Benzeval Citation2016). We expect higher reports of ERH and a more detrimental mental health impact of ERH for the latter group for a number of reasons.
First, there is evidence that immigrants are self-selected on health and so generally they are healthier, including having better mental health, than the native population (Dorsett, Rienzo, and Weale Citation2019) when they arrive. Second, being born and socialized in the adopted country, the second+ generations’ understanding of the main language in the host country and its subtleties as well as expectations for fair treatment are likely to be better than the foreign born (Bartram Citation2010). In contrast, the foreign born may be more accepting of poor treatment due to their outsider status and different frame of reference (Gelatt Citation2013), and hence are less likely to report ERH and/or suffer from such experiences. Finally, the foreign born tend to reside in areas of higher co-ethnic concentration and to socialize less with the majority population (Heath Citation2014), which may impact both their exposure to ERH and their interpretation of it.
Hypotheses
From this review, we expect that those who experience ERH will report poorer mental health than those who do not but that the association of ERH with mental ill-health will reduce after we include individual and community level controls. We also expect the association between ERH and mental ill-health to be stronger for second+ generation as compared to their foreign-born counterparts. Finally, we expect ethnic attachment to be associated with better mental health (main effect) as well as to weaken the association between ERH and mental ill-health (moderation effect).
Data and methods
Survey description
We used data from Understanding Society: the UK Household Longitudinal Study (UKHLS) (University of Essex et al. Citation2018), a longitudinal survey that started in 2009 with a nationally representative sample of around 26,000 UK households, and an Ethnic Minority Boost Sample of around 4,000 households.
All adult (16+ year old) household members are eligible for personal interviews (mostly by face-to-face) every year where they are asked about different aspects of their lives, with some sensitive questions like mental health being asked in a self-completion questionnaire. In the first, third and fifth waves of the survey (2009–2014) a sub-sample (the Extra Five Minutes Sample, which includes the Ethnic Minority Boost Sample) was asked questions on harassment and mental health. We pooled responses from all three waves, restricting the analysis sample to 16+ year old ethnic minorities, that is, those who self-reported their ethnic groups as any group other than white British or white Irish, who answered questions on harassment and who had valid responses to the mental health measures in the self-completion questionnaire.
To measure the ethnic composition of the neighbourhood of residence we linked the respondent’s survey information to the 2011 UK Census information from the Lower Super Output Area (LSOA, a geographic unit containing 672 households on average) where the respondent lives. In UKHLS, respondents are asked the same ethnic group question as the 2011 UK Census (Box 1 in the Online Appendix for the ethnic group categories). So, for each respondent, the proportion co-ethnic in the neighbourhood was computed as the proportion (percent) of individuals in their LSOA with the same ethnic group category as their self-reported one. We also included a continuous measure of the Index of Multiple Deprivation (IMD) for England, an index which ranks local areas (LSOA) in terms of relative deprivation across multiple domains: income; employment; health and disability; education; crime; barriers to housing and services; and living environment (ONS Citation2009, DCLG Citation2011). As the IMD is not consistent across countries in the UK and as 95 per cent of ethnic minorities live in England, we further restricted the final sample to residents of England.
Variables and measures
Ethnic and racial harassment (ERH)
ERH is a broad concept and can include a range of experiences. For this paper, we focused on reports of ethnically or racially motivated verbal or physical abuse which occurred in a public space. The vast majority – 87 per cent – of reported ethnically or racially motivated abuse in our sample occurred in a public space. This definition also closely approximates the definition of harassment set out in the UK Equality Act 2010.
We operationalized ERH by coding a person to have experienced ERH if (i) they report they have been insulted, called names, threatened or shouted at or physically attacked in a public place in the past year and (ii) give the reason for that to be their ethnicity, religion or national identity. These places include “on public transport”, “public buildings such as shopping centres, shops or pubs”, “outside: on the street, in parks or public places” etc.
Mental health
We measured mental health by the 12-item General Health Questionnaire (GHQ) module. This is a measure of psychological distress incorporating both anxiety and depression. The Likert type responses are recoded so that higher scores indicate more psychological distress, and then summed up (0-36). We included this as a continuous variable to capture the full breath of psychiatric distress in the population. The GHQ was introduced in 1978 and has been widely tested for validity and reliability (Jackson Citation2007), including for inter-ethnic comparisons (Bowe Citation2017).
Ethnicity and generation
We created ethno-religious categories using information from the 2011 Census ethnic group question and questions on respondent’s current religion or (if no current religion) the religion they were brought up in. We proxied (migrant) generation by the country of birth: we coded any ethnic minority born in the UK as second+ generation and all those born outside the UK as the first generation.
Ethnic attachment
In addition to the proportion co-ethnic described above, we also considered a number of individual measures of ethnic attachment:
the proportion of respondent’s friends who are of the same ethnic group.
the number of respondent’s three closest friends who are of the same ethnic group.
Using Berry’s framework of ethnic identity acculturation (see Berry et al. Citation1987) we categorized individuals into four acculturation groups based on the relative strength of their ethnic and British identities (Nandi and Platt Citation2015): strong ethnic and weak British identity (Separated), strong ethnic and British identities (Integrated), strong British and weak ethnic identities (Assimilated), weak British and ethnic identities (Marginalized). In a separate specification, we isolate the role of strong ethnic identity only (separated and integrated versus assimilated and marginalized).
Controls
We controlled for age, sex and socio-economic factors. Socio-economic status is proxied by the log of equivalized gross monthly household income (equivalized using the modified OECD scale) and the highest occupation (using National Statistics Socio-economic Classification) in the household. We additionally included educational qualification, employment status and marital status of the respondent. We also included Big Five personality measures from Wave 3 where sets of 3 questions measure each trait: Openness to Experience, Conscientiousness, Extraversion, Agreeableness and Neuroticism. We computed the score for each trait by taking the average of three items (Heineck Citation2011).
Sample description
After dropping observations with missing values of the variables, our final sample size is 7,644 ethnic minority individuals living in England. Compositional differences in socio-demographic characteristics across ethno-religious groups and generations are as expected (Tables A1 and A2 in Online Appendix). We find that the proportion reporting experiencing ERH ranges from 4 per cent among Other white groups to 10 percent among Indian Sikhs. The average GHQ score also varies across ethnic groups, with African Christians reporting the lowest level and Indian Sikhs the highest (9.73 vs 12.22). While there is no generational difference in reporting of ERH, UK born ethnic minorities report more psychological distress than the first generation (GHQ scores 11.68 vs 10.99). For reference, the average GHQ score of the white British population is 10.06.
Estimation methods
We estimated Ordinary Least Squares models (OLS) with GHQ as a continuous variable.
As we pooled data from multiple waves, have multiple participants from the same household, and the sample is clustered in design, we estimated clustered standard errors.
To adjust for differential attrition across survey waves and to ensure our analytic sample was representative of the target population of ethnic minorities covered by the Ethnic Minority Boost, we constructed post-stratification weights for age, sex, and ethnicity from the 2011 Census. The number of weighted observations is 7,193. Including weights in analysis increases the standard errors of our estimates, and thus we present these results in the main text as the more conservative and robust estimates. Unweighted results are substantively similar, though usually with smaller standard errors, and are also available upon request.
We first estimated a model of GHQ with no controls other than ERH and then progressively added potential confounders. Next, we included each measure of ethnic attachment as the main effect and as interactions with ERH to examine whether they “buffer” the impact of ERH on GHQ.
We also interacted the variables of interest (ERH; ERH interacted with ethnic attachment) with generational status (UK born or not) to identify generational differences. Finally, we examined whether the association of ERH and mental health varied by ethnic group, age and sex.
We conducted a series of sensitivity checks which are discussed in detail in Section “Sensitivity checks”.
Results
Ethnic and racial harassment and GHQ
The estimated OLS coefficient of ERH in the models (1–8) where we successively added controls are shown in and the coefficients for all the variables in Model 8 are in .
Table 1. Estimated OLS coefficient of ethnic and racial harassment (ERH) from models of mental health (GHQ) among ethnic minorities in England [Higher GHQ scores signify worse mental health].
Table 2. Estimated model [8] of mental health (GHQ) among ethnic minorities in England [Higher GHQ scores signify worse mental health].
We find that reporting ERH is associated with poorer mental health among ethnic minorities in England. Compared to those who have not experienced ERH, the GHQ of those who have was 1.98 points higher (on a 0–36 scale). The estimated coefficient for ERH in all 8 models discussed here are statistically significant at 1 per cent level of significance. This coefficient for ERH increased to 2.13 once we control for age and sex (see Models 2 and 3). This is expected, as we know that older people are less likely to report ERH (Nandi, Luthra, and Benzeval Citation2016), but more likely to report poorer mental health (see ). However, after we controlled for socio-economic and other demographic factors (Models 4–6 in ), there was little change in the estimated association of ERH and GHQ (2.16). In other words, although worse socio-economic circumstances (lower income and occupational status) are clearly associated with poorer mental health (see ) the experience of ERH cuts across all socio-economic groups. After including personality traits in Model 7 the coefficient of ERH reduced to 1.80. Personality traits were associated with ERH (in a separate model, those with a higher degree of neuroticism were more likely to report ERH, for instance) as well as associated with GHQ in the expected directions: those with higher neuroticism score (or negative affect), lower conscientiousness score and lower agreeableness score reported poorer mental health. Finally, in Model 8 we also included ethnic group and generation, but these hardly changed the ERH coefficient (1.80 vs 1.78).
To summarize, we found that net of this extensive range of controls, there is a strong association between ERH and mental ill-health with 1.8 point difference in GHQ between those who experience ERH and those who do not. Using the estimated difference and standard errors in GHQ between the employed and unemployed of 1.34 (see ) as a benchmark, we see that experiencing ERH is comparably associated with GHQ as being unemployed.
We used Model 8 as the base model specification for all subsequent analysis. Introducing an interaction between ERH and generation (Table A3 in the Online Appendix), we found that even though the association of ERH and mental health was higher for UK born ethnic minorities (2.05 vs 1.66), as we expected, this difference was not statistically significant. We also tested whether this differed by ethno-religious groups and found that the association of ERH with GHQ was lower for Chinese and Caribbean groups as compared to Indian non-Muslim-non-Sikh groups (Table A3 in the Online Appendix).
Ethnic attachment
To test whether the individual and aggregate measures of ethnic attachment acted as moderators in the association between ERH and mental health, we first added each, one by one, to Model 8. We see that, as expected, nearly all measures of ethnic attachment (living in an area with higher proportion co-ethnics after controlling for local area deprivation, maintaining a strong ethnic identity, reporting a friendship network comprised of half or more co-ethnic friends, and having three co-ethnic best friends in contrast to no co-ethnic friends) are negatively associated with psychological distress and thus are protective of mental health for ethnic minorities in England (see ).
Table 3. Estimated OLS coefficients from mental health (GHQ) models among ethnic minorities in England – Ethnic attachment measures included [Higher GHQ scores signify worse mental health] [95% CI in parentheses].
Next, we interacted with these factors with ERH to see if the association of ERH with GHQ was lower for those with greater ethnic attachment (see ). We did not find any evidence of these ethnic attachment variables providing a buffer effect against ERH; rather, living in an area with a higher proportion of co-ethnics appears to exacerbate the impact. The association between ERH and mental health is stronger for minorities living with a higher proportion of co-ethnics than for those living in less ethnically concentrated areas.
Table 4. Estimated OLS coefficients from a model of mental health (GHQ) among ethnic minorities in England – ERH interactions with ethnic attachment measures [Higher GHQ scores signify worse mental health] [95% CI in parentheses].
Finally, in a series of three-way interactions in Model 8, we tested whether specific ethnic attachment factors operate differently by generation: ERH*ethnic attachment*UK born. As the results of such interactions are difficult to interpret in table format we present them in (also presented in table format in Table A5 in the Online Appendix). The mental health difference between those who do and do not experience ERH is smaller for the second generation when they have a higher than average attachment to their ethnic identity and a higher proportion of co-ethnic friends; the opposite is true for the foreign born. For the first generation, none of the measures of ethnic attachment qualify as protective factors. The fact that ethnic attachment appears to have countervailing effects on UK and foreign born minorities (the signs of the interactions are often in opposite directions for each subpopulation), explains why we did not find any moderating effect for all ethnic minorities. Individual ethnic attachment factors are beneficial for UK born minorities, but not the foreign born.
Figure 1. Predicted mental ill-health (GHQ) score at different levels of ethnic attachment for those experiencing ethnic and racial harassment (ERH) or not, separately for ethnic minorities born in the UK and born outside the UK. Higher GHQ scores represent worse mental health. Notes: Based on pooled Understanding Society data from Waves 1, 3 and 5, estimated using weighted OLS with cluster robust standard errors; p-values **<0.01 *<0.05, +<0.10; Models also control for age, sex, marital status, education, activity status, NSSEC, household income, personality traits, ethnic group and generation. Higher scores of GHQ mean worse mental health.
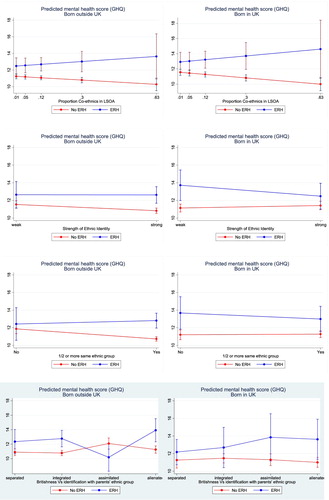
In contrast, ethnic density appears to be detrimental for all generations.
To further explore this last unexpected result, we investigate potential mechanisms underlying this exacerbating relationship. One possibility is that the proportion co-ethnic in the local area may not actually serve as a proxy for social support. For instance, if living among co-ethnics is not a choice but rather a constraint, we would not expect assumptions of social support buffering to hold. To examine this possibility further, we tested the association between a respondent’s stated preference to move and the proportion co-ethnic in the local area and found a negative association for all generations. In other words, those who said they preferred to move were less likely to live in areas with a high proportion co-ethnics. We also found that those who lived in areas of a higher proportion co-ethnic were also likely to report higher neighbourhood attachment. This suggests that co-ethnic density is providing social support and belonging, and thus we rejected a lack of social support in co-ethnic neighbourhoods as an explanation for the exacerbating effect of co-ethnic density on the mental health consequences of ERH.
Sensitivity checks
We further conducted a series of sensitivity checks to examine potential heterogeneity in associations by age and gender. We did not find a statistically significant difference in the association between ERH and mental ill-health between men and women, or minorities of different ages (Table A4 in the Online Appendix).
We also tested for sensitivity to the measure of mental health used, rerunning the models with the mental health component of SF12 (MCS) and a measure of mental wellbeing (WEMWBS). The results (Table A6 in the Online Appendix) were robust across these different measures.
Finally, we also tested for sensitivity to different definitions of generational status. In this paper we have defined the second generation as ethnic minorities born in the UK, however, those foreign born who arrived at an early age would have been socialized in the UK and may therefore behave similarly to ethnic minorities born in the UK. To test whether this was true, we re-estimated Model 8 after changing the definition of second generation to (i) include those who arrived to the UK before age 6, and (ii) include those arrived to the UK before age 12. These groups are often referred to as the 1.5 generation. The results are similar across definitions (Table A7 in the Online Appendix).
Discussion and conclusion
In this paper, using data from Understanding Society (2009–2014), we examined the relationship between experiencing ethnic and racial harassment (ERH) and mental ill-health (as measured by GHQ) of ethnic minorities living in England. Our study finds that even after controlling for a wide range of potential confounders, including the Big 5 personality traits, ERH has a strong and robust association with psychological distress. To provide context, this association is comparable in size to the association between unemployment and psychological distress.
We have demonstrated the need to examine ethnic inequalities in mental ill-health separately by migrant generation. UK born ethnic minorities reported statistically significantly worse mental health than the first generation, as well as a stronger association of ERH with mental ill-health, although this latter association is not statistically significant. Whereas the bulk of the literature documenting generational differences in the UK focuses on their improving socio-economic profile (Algan et al. Citation2009; Cheung and Heath Citation2007), our findings challenge this narrative of upward mobility and integration and demonstrate the continuing psychological stress associated with minority status, especially from experiences of overt racial hostility, even among the UK born. This research aligns with emerging cross-national evidence of an “integration paradox” (Steinmann Citation2019), namely increased reports of discrimination among those more settled in the receiving country.
This paper further casts doubt on assumptions of a uniformly positive association between integration and minority outcomes by showing how the buffering effect of ethnic attachment varies by generation. The negative association between ERH and mental health was reduced for UK born minorities with strong ethnic identities and co-ethnic friendship networks, but not for foreign-born minorities. In other words, our research suggests that for the second generation, ethnic attachment is particularly protective against mental ill-health associated with experiences of ERH. This is in line with Social Identity Theory (Tajfel and Turner Citation1979) where “simply being a member of a group provides individuals with a sense of belonging that contributes to a positive self-concept” (Phinney Citation1990).
We investigated “the ethnic density effect”, but, in contrast to previous findings (Becares et al. Citation2012), we did not find any evidence that living in high ethnic density areas is protective. Rather, we found that living among co-ethnics exacerbates the impact of ERH on mental ill-health for all generations. We examined whether this result was due to ethnic minorities experiencing less social support in more co-ethnic neighbourhoods but did not find any support for this. Specifically, proportion of co-ethnic in local area was negatively associated with preference to move and positively associated with neighbourhood attachment (measured using the modified Buckner scale).
Our findings support an interpretation of an integration paradox: ethnic minorities who feel most at home in their local area are harmed the most by discrimination. In contrast, the UK born minorities who maintain a strong sense of identity and personal links to individuals from parents’ origin countries are protected from ERH’s harmful mental health association.
Although we demonstrate the importance of disaggregating analyses by generation and of including multiple measures of ethnic attachment as resilience factors, this focus has limited our analysis in other ways. First, due to sample size restrictions and ethnic attachment factors not being asked every year, we were not able to use the fixed effects methods that longitudinal data allow, which would provide a better estimate of the causal effect of ERH on mental health. Second, we were not able to estimate the impact of repeated exposures to ERH as this was recorded in two-year intervals and the ethnic attachment measures were recorded in three or more year intervals. Third, the ethnic minority boost sample of Understanding Society lacks coverage of white minority groups necessary to test whether the relationships we observe here hold for all minority groups or only those who are visible minorities. Finally, this paper, as do all survey analyses of ERH, relies on self-reports, which may be biased in ways that confound our main findings of generation differences. For instance, we cannot say definitively whether members of the second generation actually experience ERH more, or simply recognize and feel confident enough to report ERH in a survey more. We hope to conduct qualitative interviews in the future as a way to explore in more depth generational differences in experiences of and reporting of ERH as well as intersections of these with specific origins, sex, and age.
In the meantime, this paper provides a robust estimate of the association between reports of ERH and mental ill-health, and is the first to highlight generational differences in ethnic attachment as protective factor. Our key findings that there is a high mental health cost of ERH and that there are only a few factors which qualify as protective factors raise the alarm for tackling hate crimes and hate incidents which have been increasing over the last years in many western countries (O’Neill Citation2017; FBI Citation2017; FRA Citation2018). We challenge the accepted view among policy makers that ethnic minority integration is a panacea for an ethnically divided society, highlighting the protective and beneficial effects of having a strong ethnic attachment for ethnic minorities.
Supplemental Material
Download MS Word (254 KB)Acknowledgements
We thank seminar and conference participants at the University of Essex, University of East Anglia and the Annual Conference of the British Society for Population Studies 2016, Laia Becares, Rupert Brown, John Donovan, Moira Dustin, Ratna Dutt, Faiza Elahi, Adeeba Malik, Ebony Riddell Bamber, Shamit Saggar and Mark Walters for their helpful comments and suggestions. Understanding Society is an initiative funded by the Economic and Social Research Council and various Government Departments, with scientific leadership by the Institute for Social and Economic Research, University of Essex, and survey delivery by NatCen Social Research and Kantar Public. The research data are distributed by the UK Data Service.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Algan, Y., C. Dustmann, A. Glitz, and A. Manning. 2009. “The Economic Situation of First and Second-Generation Immigrants in France, Germany and the United Kingdom.” The Economic Journal 120: F4–F30. doi:10.1111/j.1468-0297.2009.02338.x.
- Bagci, S., M. Kumashiro, A. Rutland, P. Smith, and H. Blumberg. 2017. “Cross-Ethnic Friendships, Psychological Well-Being, and Academic Outcomes: Study of South Asian and White Children in the UK.” European Journal of Developmental Psychology 14 (2): 190–205. doi:10.1080/17405629.2016.1185008.
- Bartram, D. 2010. “International Migration, Open Borders Debates, and Happiness.” International Studies Review 12 (3): 339–361.
- Becares, L., J. Nazroo, and M. Stafford. 2009. “The Buffering Effects of Ethnic Density on Experienced Racism and Health.” Health and Place 15: 700–708.
- Becares, L., R. Shaw, J. Nazroo, M. Stafford, C. Albor, K. Atkin, K. Kiernan, R. Wilkinson, and K. Pickett. 2012. “Ethnic Density Effects on Physical Morbidity, Mortality, and Health Behaviors: A Systematic Review of the Literature.” American Journal of Public Health 102 (12): e33–e66.
- Berry, J., K. Uichol, T. Minde, and D. Mok. 1987. “Comparative Studies of Acculturative Stress.” The International Migration Review 21 (3): 491–511.
- Bowe, A. 2017. “The Cultural Fairness of the 12-Item General Health Questionnaire Among Diverse Adolescents.” Psychological Assessment 29 (1): 87–97.
- Boyce, C. J. 2010. “Understanding Fixed Effects in Human Well-Being.” Journal of Economic Psychology 31 (1): 1–16. doi:10.1016/j.joep.2009.08.009.
- Byng, M. D. 1998. “Mediating Discrimination: Resisting Oppression among African-American Muslim Women.” Social Problems 45 (4): 473–487.
- Carbonell-i-Ferreri, A., and P. Frijjters. 2004. “How Important is Methodology for the Estimates of the Determinants of Happiness?” The Economic Journal 114 (497): 641–659.
- Cheung, S., and A. Heath. 2007. “Nice Work if you can get it: Ethnic Penalties in Great Britain.” Proceedings of the British Academy 137: 507–550.
- Daniel, W. W. 1968. Racial Discrimination in England. London: Penguin Books.
- Department of Communities and Local Government (DCLG). 2011. The English Indices of Deprivation 2010. Neighbourhoods Statistical Release.
- Diener, E., and R. E. Lucas. 1999. “Personality and Subjective Well-Being.” In Wellbeing: The Foundations of Hedonic Psychology, edited by D. Kahneman, E. Diener, and N. Schwarz, 2013–2229. New York, NY: Russell Sage Foundation.
- Dorsett, R., C. Rienzo, and M. Weale. 2019. “Intergenerational and Interethnic Mental Health: An Analysis for the United Kingdom.” Population, Space and Place 25: 1–12, e2195.
- Dustmann, C., F. Fabbri, and I. Preston. 2011. “Racial Harassment, Ethnic Concentration, and Economic Conditions.” The Scandinavian Journal of Economics 113 (3): 689–711.
- Federal Bureau of Investigation. 2017. “Hate Crime Statistics, 2017”. Uniform Crime Report.
- Foner, N. 2018. “Race in an era of Mass Migration: Black Migrants in Europe and the United States.” Ethnic and Racial Studies 41 (6): 1113–1130.
- FRA. 2018. Hate Crime Recording and Data Collection Practice Across the EU.
- Friedli, L. 2009. Mental Health, Resilience and Inequalities. Denmark: World Health Organisation Europe.
- Gelatt, J. 2013. “Looking Down or Looking Up: Status and Subjective Well-Being among Asian and Latino Immigrants in the United States.” International Migration Review 47 (1): 39–75.
- Halpern, D., and J. Nazroo. 1999. “The Ethnic Density Effect: Results From a National Community Survey of England and Wales.” International Journal of Social Psychiatry 46 (1): 34–46.
- Heath, A. 2014. “Introduction: Patterns of Generational Change: Convergent, Reactive or Emergent?” Ethnic and Racial Studies 37 (1): 1–9.
- Heim, D., S. C. Hunter, and R. Jones. 2011. “Perceived Discrimination, Identification, Social Capital, and Well-Being: Relationships with Physical Health and Psychological Distress in a UK Minority Ethnic Community Sample.” Journal of Cross-Cultural Psychology 42 (7): 1145–1164.
- Heineck, G. 2011. “Does it pay to be Nice? Personality and Earnings in the UK.” Industrial & Labor Relations Review 64: 1020–1038.
- Howe, C., D. Heim, and R. O'Connor. 2014. “Racism, Identity and Psychological Well-Being: A Longitudinal Perspective on Politically Embattled Relations.” Ethnic and Racial Studies 37 (13): 2457–2474.
- Jackson, C. 2007. “The General Health Questionnaire.” Occupational Medicine 57 (1): 79.
- Karlsen, S., and J. Nazroo. 2002. “Relation Between Racial Discrimination, Social Class, and Health Among Ethnic Minority Groups.” American Journal of Public Health 92 (4): 624–631.
- Karlsen, S., J. Nazroo, K. McKenzie, K. Bhui, and S. Weich. 2005. “Racism, Psychosis and Common Mental Disorder among Ethnic Minority Groups in England.” Psychological Medicine 35: 1795–1803.
- Maliepaard, M., M. Lubbers, and M. Gijsberts. 2010. “Generational Differences in Ethnic and Religious Attachment and Their Interrelation. A Study among Muslim Minorities in the Netherlands.” Ethnic and Racial Studies 33 (3): 451–472.
- Mossakowski, K. 2003. “Coping with Perceived Discrimination: Does Ethnic Identity Protect Mental Health?” Journal of Health And Social Behaviour 44 (3): 318–331.
- Mossakowski, K. N., T. Wongkaren, T. D. Hill, and R. Johnson. 2019. “Does Ethnic Identity Buffer or Intensify the Stress of Discrimination among the Foreign Born and US Born? Evidence From the Miami-Dade Health Survey.” Journal of Community Psychology 47 (3): 445–461.
- Nandi, A., R. R. Luthra, and M. Benzeval. 2016. “Ethnic and Racial Harassment and Mental Health: Identifying Sources of Resilience”, ISER Working Paper Series No. 2016-14.
- Nandi, A., and L. Platt. 2015. “Patterns of Minority and Majority Identification in a Multicultural Society.” Ethnic and Racial Studies 38 (15): 2615–2634.
- Office of National Statistics. 2009. “Understanding Patterns of Deprivation.” Regional Trends 41 (1): 93–114.
- O’Neill, A. 2017. “Hate Crime, England and Wales, 2016/17”. Statistical Bulletin 17/17. Home Office.
- Paradies, Y. 2006. “A Systematic Review of Empirical Research on Self-Reported Racism and Health.” International Journal of Epidemiology 35 (4): 888–901.
- Pascoe, E. A., and L. Smart Richman. 2009. “Perceived Discrimination and Health: A Meta-Analytic Review.” Psychological Bulletin 135 (4): 531–554.
- Phinney, J. 1990. “Ethnic Identity in Adolescents and Adults: Review and Research.” Psychological Bulletin 108 (3): 499–514.
- Phinney, J., G. Horencyzk, K. Liebkind, and P. Vedder. 2001. “Ethnic Identity, Immigration and Wellbeing: An Interactional Perspective.” Journal of Social Issues 57 (3): 493–510.
- Pickett, K., and R. Wilkinson. 2008. “People Like Us: Ethnic Group Density Effects on Health.” Ethnicity & Health 13 (4): 321–334.
- Poynting, S., and V. Mason. 2007. “The Resistible Rise of Islamophobia: Anti-Muslim Racism in the UK and Australia Before 11 September 2001.” Journal of Sociology 43 (1): 61–86.
- Reynolds, T. 2007. “Friendship Networks, Social Capital and Ethnic Identity: Researching the Perspectives of Caribbean Young People in Britain.” Journal of Youth Studies 10 (4): 383–398.
- Richards, L. 2016. “For Whom Money Matters Less: Social Connectedness as a Resilience Resource in the UK.” Social Indicators Research 125: 509–535.
- Rumbaut, R. 1994. “The Crucible Within: Ethnic Identity, Self-Esteem, and Segmented Assimilation among Children of Immigrants.” International Migration Review 28 (4): 748–794.
- Schofield, P., M. Thygesen, J. Das-Munshi, L. Becares, E. Cantor-Graae, E. Agerbo, and C. Pedersen. 2017. “Neighbourhood Ethnic Density and Psychosis – Is There a Difference According to Generation?” Schizophrenia Research 195 (2018): 501–505.
- Steinmann, J. 2019. “The Paradox of Integration: why do Higher Educated new Immigrants Perceive More Discrimination in Germany?” Journal of Ethnic and Migration Studies 45 (9): 1377–1400.
- Stevens, M., S. Hussein, and J. Manthorpe. 2012. “Experiences of Racism and Discrimination among Migrant Care Workers in England: Findings From a Mixed-Methods Research Project.” Ethnic and Racial Studies 35 (2): 259–280.
- Tajfel, H., and J. Turner. 1979. “An Integrative Theory of Inter-Group Conflict.” In The Social Psychology of Inter-Group Relations, edited by W. G. Austin and S. Worchek, 33–47. Monterey, CA: Brooks/Cole.
- University of Essex, Institute for Social and Economic Research, NatCen Social Research, Kantar Public. 2018. Understanding Society: Waves 1-7, 2009-2016 and Harmonised BHPS: Waves 1-18, 1991-2009 [Data Collection]. 10th ed. UK Data Service. SN: 6614, http://doi.org/10.5255/UKDA-SN-6614-11.
- Virdee, S. 1997. “Racial Harassment.” In Ethnic Minorities in Britain: Diversity and Disadvantage, edited by T. Modood, R. Berthoud, J. Lakey, J. Nazroo, P. Smith, S. Virdee, and S. Beishon, 259–289. London: Policy Studies Institute.
- Veling, W., J. P. Selten, E. Susser, W. Laan, J. Mackenbach, and H. Hoek. 2007. “Discrimination and the Incidence of Psychotic Disorders Among Ethnic Minorities in the Netherlands.” International Journal Epidemiology 36 (4): 761–768.
- Wallace, S., J. Nazroo, and L. Bécares. 2016. “Cumulative Effect of Racial Discrimination on the Mental Health of Ethnic Minorities in the United Kingdom.” American Journal of Public Health 106 (7): 1294–1300.
- Williams, D., H. Neighbors, and J. Jackson. 2003. “Racial/Ethnic Discrimination and Health: Findings From Community Studies.” American Journal of Public Health 93 (2): 200–208.
