Abstract
Introduction
For Small-Group Active Learning (SMAL) to be effective, students need to engage meaningfully in learning activities to construct their knowledge. Teachers can have difficulty engaging their students in this process. To improve engagement, we aimed to identify the diversity in medical students’ appreciation of SMAL, using the concepts of epistemic beliefs and approaches to learning.
Method
Q-methodology is a mixed-method research design used for the systematic study of subjectivity. We developed a set of 54 statements on active learning methods. In individual interviews, first-year medical students rank ordered their agreement with these statements and explained their reasons. Data were analyzed using a by-person factor analysis to group participants with shared viewpoints.
Results
A four-factor solution (i.e. profiles) fit the data collected from 52 students best and explained 52% of the variance. Each profile describes a shared viewpoint on SMAL. We characterized the profiles as ‘understanding-oriented’, ‘assessment-oriented’, ‘group-oriented’, and ‘practice-oriented’.
Discussion
The four profiles describe how and why students differ in their appreciation of SMAL. Teachers can use the profiles to make better-informed decisions when designing and teaching their SMAL classes, by relating to students’ epistemic beliefs, and approaches to learning. This may improve student motivation and engagement for SMAL.
Introduction
Small-group active learning methods are effective in developing students’ knowledge, skills, and personal and professional attributes (Rocca Citation2010; Onyura et al. Citation2016; Schneider and Preckel Citation2017). They are therefore an important component of many medical programmes, and medical students increasingly spend their contact time in small-group settings (Irby and Wilkerson Citation2003; Mann Citation2011). To be effective, active learning methods require students to engage meaningfully in learning activities to construct their own knowledge (Chi Citation2009). Students, however, can be reluctant to engage as they feel that these methods are not an effective or efficient use of their study time (Deslauriers et al. Citation2019). Consequently, active learning becomes a source of negative emotions, like frustration and anxiety (Kilgour et al. Citation2016), as well as a reason for students to complain (Henderson et al. Citation2012). In addition, teachers who perceive their students to resist active learning methods might be unable or unwilling to use these methods, and revert to less effective (i.e. more passive) learning methods, like lecturing, that require little student engagement (Graffam Citation2007; Michael Citation2007; Chi Citation2009; Henderson et al. Citation2012).
Practice points
First-year medical students vary in their appreciation of small-group active learning, resulting from differences in epistemic beliefs and approaches to learning.
Students may be more motivated for active learning methods when these match with their motives and preferences.
Usually, teachers have multiple activities to choose from when designing their classes. By choosing and adapting activities that cater to different profiles, student engagement could be stimulated.
Teachers could start a ‘meta-conversation’ about learning with their students to aid learning. In doing so, they can acknowledge different motives and preferences for learning, and elaborate on the value of learning activities for different students.
Although (medical) education research has identified many factors that influence students’ appreciation of active learning methods, these mainly focus on aspects of curricula, courses, teacher behaviors, and student sociodemographic characteristics (Rocca Citation2010; Frambach et al. Citation2014; Kilgour et al. Citation2016; Srivastava and Waghmare Citation2016; Deslauriers et al. Citation2019). Only recently have researchers begun to investigate the student’s perspective more deeply in an attempt to explain their continued reluctance towards active learning (Deslauriers et al. Citation2019; Owens et al. Citation2020). These studies suggest that student appreciation of active learning is not a ‘one-size-fits-all’ issue. Because students have different beliefs about knowledge and learning, strive for different goals, and employ different learning strategies, they appreciate active learning differently. We need a better understanding of students’ diversity in appreciation of active learning to help teachers to improve all students’ motivation for these types of learning activities.
Two conceptual frameworks help us to investigate students’ diversity in perception of active learning. Epistemic beliefs are beliefs about the nature of knowledge and the process of learning. Students have different beliefs about how to obtain, perceive, organize, and use knowledge (Schommer Citation1994; Eastwood et al. Citation2017). Perry’s model of intellectual and moral development describes different stages students can be at, ranging from dualist beliefs (black-and-white thinking: there is one correct answer to everything, students need to memorize these answers), to multiplistic beliefs (problems can have multiple answers and even when contradicting each other, all answers can be correct, knowledge is subjective), to relativistic beliefs (some answers are better than others, depending on your stance or context), to committed beliefs (using personal values to evaluate answers)( Perry Citation1968; Eastwood et al. Citation2017). Relating epistemic beliefs to active learning; students in the dualistic stage appreciate teaching and learning activities that will help them to obtain the clear-cut correct answer to questions, while later stages are more open for activities that allow multiple answers to question to coexist, or even activities that allow students to conclude different answers.
Approaches to learning is a related concept and identifies the motives (i.e. goals) and strategies of students for learning. Traditionally, a deep and surface approach were distinguished (Entwistle Citation1991; Biggs and Tang Citation2011). A deep learning approach indicates a student’s motive for meaningful understanding and the use of associated learning strategies like relating new knowledge to prior knowledge. A surface learning approach indicates a motive of meeting minimal requirements and relying on rote memorization strategies. Nowadays, an additional strategic learning approach is distinguished, indicated by a student’s motive of high achievement, and use of both deep and surface learning strategies. Relating approaches to learning to active learning: surface learners favor subject-matter experts to tell them what they should know. Deep learners favor activities that allow them to use higher order thinking skills. Both epistemic beliefs and approaches to learning affect how students perceive and value active learning methods, which in turn affects how willingly students engage in active learning methods (Chiu et al. Citation2016).
In this study, we aimed to identify the diversity in medical students’ appreciation of small-group active learning, based on their epistemic beliefs and approaches to learning. Ultimately, this knowledge may help teachers to improve engagement in active learning in their classes by tailoring to different needs and wishes. Teachers can make better-informed decisions about specific learning activities and communicate their value in relation to students’ epistemic beliefs, and approaches to learning.
Method
Setting
We conducted this study at the Faculty of Medicine of the Vrije Universiteit Amsterdam (FMVU) in the Netherlands. Medical education in the Netherlands is competency-based (derived from the CanMeds framework) and consists of three years of preclinical education (Bachelor’s degree programme) followed by three years of clinical education (Master’s degree programme) (van Herwaarden et al. Citation2009). The FMVU has approximately 2300 students studying in the Bachelor and Master programmes.
This study took place in the Bachelor phase of medical training. At the start of their first year, students enrol in study groups of twelve students. These groups are formed for a semester and meet twice per week for two hours to discuss written patient cases and work on accompanying assignments (designed to help students relate clinical signs and symptoms to underlying mechanisms). There are fifty-four meetings spread out over the academic year. Students themselves are responsible for preparing and leading the meetings, taking notes, asking, and answering questions, giving presentations, and providing each other with feedback. Students collaborate between meetings to work on the cases and prepare the presentations. Teachers (called tutors) take on the role of facilitators during study group meetings; they focus on the process of the meeting and observe individual contributions to the learning process of the group. They also assess the professional behavior of students at the end of a semester. Some tutors have a medical background, but this is not a necessity as the tutors do not have to function as content experts.
Study design
Q-methodology
We used Q-methodology for this study. Q-methodology is a mixed-method research technique used for the systematic study of subjective viewpoints (Brown Citation1980; Stephenson Citation1993/1994; Watts and Stenner Citation2012). It allows researchers to obtain a rich and differentiated understanding of participants’ perspectives of the topic under study (McKeown Citation2001; Ramlo Citation2016). This aligns with the aim of this study. Q-methodology has been used in (medical) education research before, for example to understand graduate medical trainee’s attitudes towards teaching (Dotters-Katz et al. Citation2016), to inform curricular change (Roberts et al. Citation2015), and to elicit student attitudes towards their studies (Young and Shepardson Citation2018). Other aspects of education that have been studied using Q-methodology are e-learning (Khatri Citation2010), assessment (Fokkema et al. Citation2014), and self-regulated learning (Berkhout et al. Citation2017). Following the guidelines provided by Watts and Stenner (Citation2012), we set up this study in five steps: (1) Q-set development, (2) participant selection, (3) data collection (Q-sorting), (4) data analysis and (5) factor interpretation. These steps are described below in detail.
Step 1: Q-set development
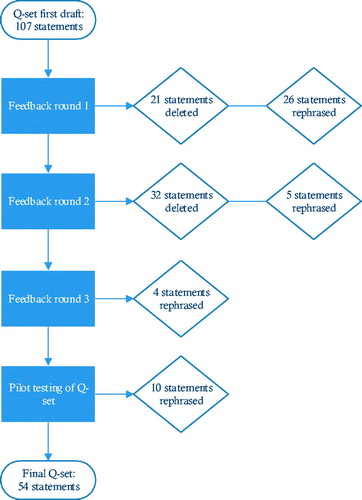
The Q-set, or the set of statements about the research topic, was specifically developed and tailored to our research questions to cover all possible viewpoints (). For our first draft, we reviewed relevant literature (on active learning, epistemic beliefs, approaches to learning), the medical school’s educational policy documents, and student evaluation forms of the study group meetings in previous years. We also observed study group meetings and interviewed various stakeholders. As a result of this work, we developed statements in four categories: preferred roles and responsibilities of the students themselves (in- and out of class), their study group, their tutor, and expectations from their medical school.
Then, we revised the Q-set through three rounds of feedback. In round 1, we asked two educational professionals and two researchers to review the statements using a think-aloud procedure. This allowed us to delete or rephrase unclear statements. In round 2, the research team then assessed the relevance, phrasing, overlap, and completeness of the Q-set. In round 3, we discussed the Q-set with other researchers from the Research in Education team of FMVU. Finally, we pilot tested our Q-set with the study group coordinator, two tutors, and two students. We again used a think-aloud procedure to assess the clarity of the statements. The final Q-set consisted of 54 statements (), which aligns with general recommendations to stay between 40 and 60 statements (Watts and Stenner Citation2012). For publication purposes, we translated the original statements into English (and checked our translation using back-translation by a native English speaker with Dutch fluency).
Table 1. Q-set statements and factor arrays (i.e. how a prototypical student in a factor would rank order the statements).
Step 2: Participant selection
The selection of participants is important in Q-methodology, as researchers want to explore (or demonstrate) the existence of viewpoints. Watts and Stenner (Citation2012), therefore, recommend thinking critically about which sampling strategies will help to achieve that goal and determine relevant sociodemographic criteria. We chose to use a variety of strategies, as different students might be responsive to different strategies, thus increasing our chances of including as many viewpoints as possible. We invited students to participate during the opening lecture for first-year medical students, we went to their study group meetings, sent out an email to all first-year students, and distributed leaflets on the campus. We also invited students to ask a peer to participate; someone who they thought would have an interesting perspective (snowballing). In our communication we stressed that we aimed to include students with varied preferences and that all preferences would be valued, especially students who feel they might have distinct preferences.
Q-methodological studies do not benefit from large numbers of participants, mainly because they are interested in establishing the existence of viewpoints in their sample, which theoretically can be achieved with as many participants as there are viewpoints. That is why the sampling procedure is so important. A general guideline is to include fewer participants than items in the Q-set (Watts and Stenner Citation2012). Therefore, we aimed to include 50 students in the study.
All first-year bachelor’s students (N = 350) of FMVU were eligible to participate, as we aimed to identify the diversity in appreciation for active learning of students who enter medical schools. All students willing to participate were included.
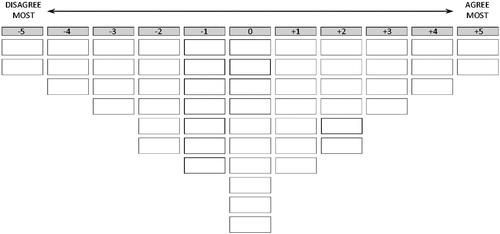
Step 3: Data collection
We collected the data for this study between September and December 2018. Participants took part in a one-hour interview (with JWG, AdlC, or research assistant) on the campus. Before the interview, students were informed about the goals and methods of the study, could ask questions, and signed the informed consent form. At the beginning of the interview, participants filled out a questionnaire about their sociodemographic characteristics (age, gender, educational background, marital status, student member association, amount of volunteer or paid work, socioeconomic status, ethnic background, living situation). Then they did the Q-sorting procedure: rank ordering the Q-set statements according to agreement on a grid with a prearranged frequency distribution (). The interviewer observed this process and photographed the completed Q-sort for quantitative analysis (see step 4). Next, the interviewer asked participants to elaborate on the reasons behind their choices (e.g. could you tell me your reasons for putting these statements at ‘agree most’?). The interviewer also asked about observed behaviors during the Q-sorting process (e.g. when a student hesitated before placing a statement on the grid or laughed when reading a statement). These observations might indicate important thoughts and feelings about statements. Answers to these questions were written down on a blank piece of paper. This semi-structured ‘post-sorting interview’ comprised the qualitative data for this study. In Q-methodological studies, these data are not recorded, transcribed, and analyzed, as in qualitative methods, but used to evaluate factor solutions (step 4) and to enrich factor interpretations (step 5).
Step 4: Data analysis
We used PQMethod version 2.35 to perform factor analysis on the Q-sorts (Schmolck Citation2014). PQMethod is a software program specifically developed for performing by-person (instead of by-item) factor analyses in Q-methodological studies. In line with Watts and Stenner’s (Citation2012) recommendations, we employed the centroid method of factor analyses, with varimax rotation, complemented with manual rotations. The centroid method leaves researchers ‘… free to consider any data set from a variety of perspectives, before selecting the rotated solution which they consider to be the most appropriate and theoretically informative.’ (Watts and Stenner Citation2005). This method suited our aim to include as many students in the factors as possible. Other methods, like principal component analysis, do not offer this freedom as they prescribe on statistical criteria alone which solution to accept (Akhtar-Danesh Citation2016). This is also the reason for complementing the varimax rotation with manual rotations; to evaluate if we could add extra students to a factor.
Three researchers (JWG, AdlC, RK) evaluated the outcomes of the factor analyses (i.e. factor solutions) and decided on the accepted solution through consensus. Our criteria for accepting a solution were statistical (eigenvalues of >1.00, minimal total explained variance of 35%, and at least 2 Q-sorts per factor), qualitative (corroboration of the factor solution by the post-sorting interview data) and methodological (are the factors coherent, differentiated and recognizable) (Watts and Stenner Citation2012). As a final step, we used the study’s conceptual framework to characterize the profiles.
Step 5: Factor interpretation
We followed the structured method for factor interpretation provided by Watts and Stenner (Citation2012). We started with the calculation of factor arrays (weighted averages of the Q-sorts in a factor, see ). Factor arrays show how a prototypical student in a factor would rank order the statements. We then interpreted the factor by looking at the highest and lowest ranking statements, statements in a factor that significantly deviated from other factors, and finally at items in the middle. At this point, we combined the quantitative and qualitative data, to enrich the factor interpretation and to explain any existing intra-factor discrepancies. Finally, we wrote up a description of each factor and checked its accuracy.
Ethics
The Ethical Review Board of the Netherlands Association for Medical Education approved the study (dossier number 1062).
Results
Participant characteristics
Fifty-two first-year medical students participated in an interview between September and December. This means that students had between 1 and 3 months experience with the study group meetings. Forty-one participants were female. Their mean age was 18.6 years, with a range of 17–23. Seventy-one percent immediately enrolled in medical school following high school graduation (students without previous studies or gap years). These findings are roughly representative for the first-your medical student population of FMVU.
Student profiles
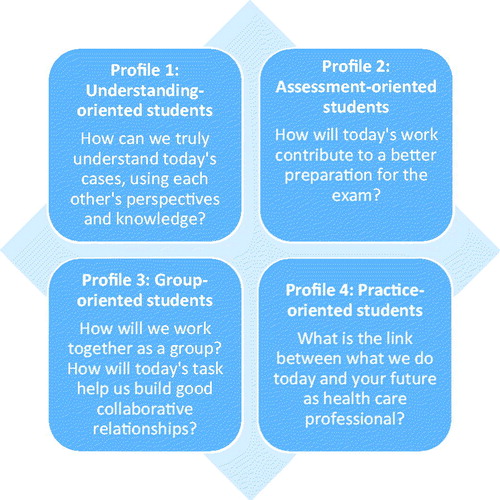
We decided on a four-factor solution using our criteria for evaluating factor solutions (see step 5 above). Each factor represents a group of students with similar viewpoints about small-group active learning. shows the Q-set statements, with the factor arrays (how a prototypical student in a factor would rank order the statements). The four factors explained 52% of the study variance. Forty-seven Q-sorts loaded significantly on one of the factors, one Q-sort was confounded (loaded on more than one factor), and four Q-sorts did not load on any factor (). As the factors represent students and not items (as in other factor analysis), we will use the word ‘profile’ instead of factor when describing their viewpoints below. The four profiles are summarized in . The descriptions below provide the subjective viewpoints of students in the profiles. The information in parentheses (e.g. 50 +4) refers to the specific statement number in the Q-set (between 1 and 54), and its position in the factor array (between −5 and +5).
Table 2. Q-sorts defining the four factors.
Table 3. Summary of the four profiles.
Profile 1: Understanding-oriented students
Profile 1 explains 16% of the study variance. Fifteen students load significantly onto this factor.
Role of students – Students in profile 1 are intrinsically motivated to broaden and deepen their understanding of everything related to medicine. They want to be challenged via questions, problems, and discussions with others (44 +5). Becoming a good doctor is more important to them than passing exams (25 +1). They are motivated by learning how to analyze and solve all sorts of problems (52 +4). They view themselves as mature learners and accordingly want to be responsible for their own learning, including learning from their own mistakes (36 −4, 46 −1).
Role of study groups – Students in profile 1 value working together with their peers in study groups (9 −5). For optimal learning, they feel it is the responsibility of all members to do their assignments well and to participate in the learning process (23 0, 33 +3). Members of the study group should not let other activities in their lives interfere with their responsibility to the learning of the group (42 −1). Study groups should ensure that all members feel safe to say what they think, as that provides an extra opportunity to learn from multiple perspectives (28 +5, 48 +4). Students in this profile prioritize learning over the social aspect of study groups (5 −2). Study group meetings can be tailored to students’ wants and needs, making them preferable over large-group lectures (39 −4). As students in this profile value in-depth discussions (29 +2), they do not mind when group meetings run late (3 +1).
Role of tutors – Tutors’ main task is to motivate students to engage with the material and challenge them to find their own answers. In fact, tutors should refrain from giving answers as this limits learning (26 +3). Tutors should be passionate, as this motivates students (47 +2). Their role is to facilitate, and not control, the process (32 −4, 1 −1). Tutors do need to have some medical knowledge to facilitate the learning (e.g. by knowing which questions to ask) (37 +2, 51 −3).
Role of medical school – Medical training should challenge students to learn about the social, ethical, and research side of medicine, and not only be about treating patients (50 +4). There should be space for multiple viewpoints and discussions (34 0, 35 −3, 14 −5). Schools should also develop a system in which students themselves are responsible for learning, which allows making mistakes as part of learning, and that provides trust and autonomy to students to learn in their own way (8 −3).
Profile 2: Assessment-oriented students
Profile 2 explains 11% of the study variance. Eight students load significantly onto this factor.
Role of students – For students in profile 2, the goal is to pass exams. All educational activities should help with this goal (25 +5). This means that they want to learn what the ‘right and wrong’ answers are, and they feel frustrated when there is no such answer (35 +2). They are looking for efficiency in learning and are therefore not interested in anything other than what is being assessed (54 −3).
Role of study groups – Students value collaboration with peers, because it allows them to ask questions and improve their understanding of assessment-related knowledge (9 −5). Therefore, all students in a group should feel free to ask any questions they have (28 +4) and there should be a good atmosphere (48 +3). However, study groups consisting of students voicing diverse perspectives complicates learning, as it is then difficult to conclude correct answers. Groups of like-minded students are preferable (10 −3). A diverse group can have more intragroup friction and miscommunication, which costs time and distracts from learning (48 +3, 24 −1).
Role of tutors – Tutors’ main task is to make sure that students understand the content correctly (51 −5). Hence, tutors should have studied medicine (37 +5) and explain the content clearly (7 +2, 22 +2). They should answer questions rather than challenging students to find their own answers (26 −4). They should also check the quality of students’ assignments (8 +1). Furthermore, tutors should be available for (study-related and personal) problems that might interfere with their goal of passing exams (11 +4, 12 +4, 41 +2, 42 +3). Students in this profile do not have the desire for a personal connection with their tutor (40 −4), nor do they expect passion from tutors in facilitating study groups (47 −1). To help with students’ study efforts, tutors should know everything about the study programme (53 +2). Finally, tutors should not have high expectations for students, as this might mean students have to work harder for a passing grade (46 −4).
Role of medical school – The medical school should design the study groups in such a way that they optimally support students in preparing for the exams (25 +5). Lectures, in which students can learn from experts, are actually preferred over study groups, as students immediately learn the correct understanding of a topic (39 +1). Study assignments should not be too challenging (14 −2). The focus of the programme should lie on clinical content knowledge, rather than personal development and a broader perspective on patient care (50 −2, 54 −3).
Profile 3: Group-oriented students
Profile 3 explains 13% of the study variance. Ten students load significantly onto this factor.
Role of students – For students in profile 3 learning how to collaborate with others is most important, as they see this as an essential skill for any future career. Groups also fulfill important needs for students, like a sense of belonging, support, opportunities for new friendships, and learning. They, therefore, want to contribute to a good group atmosphere (48 +5). They believe that the best way to learn medical topics is by discussing and relating their ideas with those of their peers (39 −2). They believe learning occurs in dialogue, and that it is important to develop their own opinions by relating to those of others (28 +5).
Role of study groups – Students feel they gain new insights by discussing and explaining to each other, and see opportunities to build their social network (making friends) by collaborating (9 −5). Students see the group as a support system as well, and being friends with one another can stimulate well-being, enjoyment, and study success. Study groups should be responsible for the learning process. In doing so, they practice collaboration skills needed in any future career. Therefore, they should have autonomy in deciding how to collaborate (36 −5, 43 +2). They should also be able to solve any intra-group problems themselves (13 +3). Essential ingredients are inclusive atmospheres (48 +5), and equality among members (28 +5).
Role of tutors – Tutors are not the same as teachers, as tutors do not need to explain any content (22 0). Tutors do not have to be role models who discuss their own experiences, nor do they have to have studied medicine (1 −4, 2 −2, 37 −4). Their role is to observe and guide the group process and give feedback to students on their long-term development (16 +4). Tutor feedback is seen as more valuable than peer feedback because a tutor can be more critical – this includes addressing students’ disruptive behaviors should these occur. They should be available for discussing students’ personal problems (12 +3).
Role of medical school – Medical schools should design study groups to serve multiple purposes: they should help students to prepare for exams (25 +4), to learn communication and collaboration skills (50 +4), and to build a social support network. The medical school should provide clear boundaries within which autonomy is given to groups. Assignments should be clearly linked to practice, to increase motivation and getting a good overview of the profession (34 +2).
Profile 4: Practice-oriented students
Profile 4 explains 13% of the study variance. Fourteen students load significantly onto this factor.
Role of students – Students in profile 4 want to learn to think like a doctor. They want to learn how to analyze and solve problems (52 +4). They view ‘struggling’ with complex and challenging assignments as a necessary and enjoyable aspect of learning, as this allows them to construct their knowledge (14 −5, 44 +4) and to prepare for a future in clinical practice. If they are not sufficiently challenged, they get bored and demotivated. They are interested in learning about all the roles and responsibilities they will fulfill, including personal and professional development (52 +4, 54 +4). Students want to be responsible for both the learning process and achieving the desired learning outcomes (36 −5).
Role of study groups – Students like to collaborate with peers who think differently from themselves (9 −4, 10 0, 15 +1), as their perspectives are opportunities for rich feedback (18 +2). Students in this profile see the process of collaboration as preparation for their future careers in multidisciplinary teams. An open and safe group atmosphere is important so that all students feel free to say what they want (48 +5, 28 +5). Study groups are also an opportunity to develop friendships (5 +1).
Role of tutors – Tutors’ main task is to stimulate group collaboration at the start and then to minimize their activity, and ultimately ‘become obsolete’. Students feel they should be able to manage themselves, as they will not have anyone holding their hand when they are a doctor. Tutors do not have to share personal experiences or explain the content (2 −2, 7 −2). Students in this profile do not need tutors for personal and study-related problems (11 0, 12 −3). The tutor does not need to show an interest in students or the group (21 0), nor are students looking for a personal connection with the tutor (4 −4). Students also do not want the tutor to tell them exactly what to do and when to do it (36 −5), nor to function as a classroom manager (32 −1) or to give them compliments (17 −4).
Role of medical school – Medical schools should offer opportunities to prepare for a future career in clinical practice, including communication, collaboration, personal and professional development (54 +4, 50 +3, 34 +2). It is important that the school allows for tailoring to personal interests (49 +3), and provides suitable and difficult challenges (14 −5, 44 +4). This includes accounting for different levels of competencies. Digital learning tools might be suitable for these purposes (30 +1).
Discussion
In this study, we identified four student profiles that describe shared viewpoints on appreciation of small-group active learning. Although the profiles have some degrees of overlap, each profile can be characterized by distinct preferences for students’ own role in the learning process, their study groups, their tutors, and how they would like to be supported in their learning by their medical school. These preferences correspond to the students’ motives for learning. Students stated in the interviews how their motivation and engagement was (at least partly) dependent on the perceived match between their viewpoint and the learning activities. Comparing the profiles shows why engaging all students in a class can be difficult for teachers: they have conflicting preferences. When a teacher aligns with the preferences of one profile, for example with profile 1 by engaging in an in-depth group discussion not directly related to the course objectives, students in another profile might not see the value of that learning activity (in this case profile 2 would question the value of the discussion for the assessment).
Epistemic beliefs
We found that students in profile 2 have dualistic beliefs (‘there are correct and incorrect answers, and teachers should tell me so I can memorize them’). Students in profiles 1, 3, and 4 have multiplistic beliefs (‘multiple answers can be correct and discussing those is important for learning’). We did not find students with relativistic or committed beliefs in our sample. This is not surprising as students are expected to evolve more sophisticated beliefs over the course of their medical study (Eastwood et al. Citation2017). We found that students have low motivation and engagement when there is a mismatch between their beliefs and the teacher’s expectations or learning activities. When teachers design their classes to include learning activities in which there are no clear-cut right answers (i.e. cater to students with multiplistic beliefs), one can imagine how students with dualistic beliefs would be less motivated to engage. These students would experience the learning activity as an ineffective and inefficient use of their study time.
Studies on epistemic beliefs show that it is effective to explicitly address and reflect on epistemological themes to promote more sophisticated beliefs (Eastwood et al. Citation2017). Related to this study, this means that teachers should acknowledge different epistemic beliefs among their students and elaborate on the importance of small-group active learning for their development. This will help to align student beliefs and teacher expectations. A recent study by Deslauriers et al. (Citation2019) adds to that by recommending that teachers help students to appreciate active learning early in the learning process. Teachers could take time to elaborate on the value and requirements of active learning and introduce formative or summative feedback early in the course to help students see their development. This could help to improve student motivation for active learning.
Approaches to learning
We identified aspects of deep learning (predominantly in profile 1), surface learning (predominantly in profile 2), and vocational learning (predominantly in profile 4). These findings correspond with Mattick and Knight’s study on medical students’ approaches to learning (Citation2009). Mattick and Knight also describe the importance of social factors for learning. In our study, we identified one profile that places social motivation at the very center of their learning (profile 3). In this profile, social motivation was seen as important and was positive (social support and opportunity for making friends). This differs from the findings by Mattick and Knight, who found that social motivation only became important in clinical stages of medical training, and comprised of humiliation-avoidance, showing off to others and feeling negative emotions when not doing what is required.
Mattick and Knight (Citation2009), along with other studies into approaches to learning, recommend teachers to stimulate deep learning as it is supposed to be associated with academic achievement (Dinsmore and Alexander Citation2012). However, a recent systematic review of meta-analyses shows deep learning to ‘have no systematic relation with achievement’ (Schneider and Preckel Citation2017). On the contrary, it is suggested that teachers help their students to employ a strategic approach to learning; to regulate their learning strategies as required from a task or activity combined with a motivation for achievement (Schneider and Preckel Citation2017). Related to the current study, this means that teachers can help their students by relating students’ motives and preferences to the course’s learning and assessment activities and elaborate on what is needed for success. Most often, students will probably have to employ a combination of approaches: engaging with peers to construct meaning from a learning activity or understanding how an exam helps to prepare for future practice. As especially students’ perception of assessment requirements affect how students approach learning, we do recommend teachers to design sound (formative and summative) assessment activities (Watling and Ginsburg Citation2019).
Implications for practice
As stated before, student engagement in small-group active learning is the result of many interacting factors, ranging from curriculum design to teacher behaviors to student sociodemographic characteristics. This study gives more insight into the students’ perspective: when and why do they appreciate active learning? We identified four profiles to answer that question. Teachers could use knowledge of the profiles to make better decisions when designing and teaching their class.
When designing a class, teachers can reflect on the active learning methods they employ and anticipate which students might engage more easily (and why), and which students might be reluctant to engage (and why). To give some examples: students in profile 1 (understanding-oriented) usually engage easily in in-depth group discussions when it sparks their interest, while students in profile 2 (assessment-oriented) might want to understand the relevance for the assessment first. Students in profile 3 (group-oriented) usually engage easily in collaborative exercises that strengthen their relationships, like escape rooms (Guckian et al. Citation2020), while students in profile 4 (practice-oriented) might be critical about its value for their future profession. Typically, teachers have multiple activities to choose from when designing their classes. By choosing and adapting activities that cater to different profiles, student engagement could be stimulated.
When teaching a class, teachers could start a ‘meta-conversation’ to aid the learning of students, by acknowledging the different motives and preferences, and elaborating on the value of the learning activity for different students (the Q-set and Q-sorting procedure used in this study could be transformed into a learning activity for this purpose). Often when teachers introduce a learning activity, they do so briefly and get started. Not many teachers talk explicitly about how learning might take place. This leaves students to have to interpret the value of the activity for their learning. We propose that in the introduction of each class, teachers address the concerns and preferences of each profile by answering a few questions (). One important caveat: our proposal assumes sound basic course design principles, like constructive alignment, to be in place.
Strengths and limitations
The use of Q-methodology allowed us to identify authentic viewpoints of medical students regarding small-group active learning. By interviewing first-year students at the start of the academic year, we have gained an in-depth understanding of students who enter medical school. Designing our study using the conceptual frameworks of active learning, epistemic beliefs, and approaches to learning allowed us to better understand the origins of the specific preferences of students and improves the generalizability of our findings. However, the profiles reflect the preferences of participants in this study. We do not know how biased our sample was and if we have missed existing preferences. We are aware that some students are more inclined to participate in (medical) educational research than others and have tried to counteract this by communicating explicitly our wish to include all sorts of students. We have focused on the relationship between students’ appreciation for active learning and engagement. As students indicated in the interviews (and as is known from literature), other factors also affect their engagement.
Future research
A follow-up study with the same participants might show how the students and profiles develop over time, and what the causes of these developments are. For example, research shows that clinical experience influences the epistemic beliefs of medical students (Eastwood et al. Citation2017). It is unclear how perceptions of, and preferences for, active learning changes as more sophisticated epistemic beliefs evolve. This offers potentially valuable information for improving medical education. In addition, as we have given suggestions for teachers to improve motivation and engagement of students for (active) learning, the impact of these suggestions could be investigated. How effective are our suggestions in terms of student and teacher appreciation of active learning? Do they help teachers to motivate and engage students? A third suggestion is to focus on teacher appreciation of active learning. Teachers vary in their appreciation of active learning, depending on their conceptions of teaching and learning (Jacobs et al. Citation2014). Their appreciation might be reflected in their teaching practices, favoring other types of learning. This future study could yield suggestions to improve teacher motivation for active learning, as the current study did for students.
Conclusion
It can be difficult for medical teachers to motivate and engage their students in small-group active learning methods. In this study, we have identified four profiles that describe when and how students might be motivated for small-group active learning. We have used the concepts of epistemic beliefs and approaches to learning to explain the diversity in students' appreciation for active learning. Teachers can use the profiles to reflect on the use of active learning in their courses and relate to the different motives and preferences of medical students. This allows teachers to optimize their course design choices regarding active learning, as well as communicating about it with their students, so that all students have higher motivation and engagement.
Glossary
Q methodology: Is a research technique, and associated set of theoretical and methodological concepts, originated and developed by William Stephenson, which focuses on the subjective or first-person viewpoints of its participants. The basic method combines the gathering of data in the form of Q sorts and their subsequent intercorrelation and factor analysis. A well-delivered Q study reveals the key viewpoints extant among a group of participants and allows those viewpoints to be understood holistically and to a high level of qualitative detail.
Definition from Watts S, Stenner P. 2012. Doing Q methodological research: theory, method and interpretation. London: SAGE Publications Ltd. DOI: 10.4135/9781446251911.
Acknowledgment
We would like to thank Femke Dijkstra for her help with the data collection and analysis.
Disclosure statement
The authors have no conflict of interest to declare.
Additional information
Funding
Notes on contributors
J. W. Grijpma
J. W. Grijpma is a PhD student in Medical Education at Research in Education, Amsterdam UMC, and a teacher educator at LEARN! Academy, Vrije Universiteit Amsterdam.
A. de la Croix
A. de la Croix is an Assistant Professor at Research in Education, Faculty of Medicine Vrije University, Amsterdam. She is a qualitative researcher with a background in linguistics, teaching, and teacher training. Her mission is to help educators to stimulate meaningful and reflective interactions in higher education.
J. H. Kleinveld
J. H. Kleinveld, PhD, psychologist, works as study group coordinator at the Faculty of Medicine, Vrije Universiteit Amsterdam, Department of Education Strategy and Policy, and teacher at the Amsterdam University Medical Center, Department of Clinical Genetics.
M. Meeter
M. Meeter, PhD, is a full professor of Education Sciences at Vrije Universiteit Amsterdam, the Netherlands.
R. A. Kusurkar
R. A. Kusurkar, MD, PhD, is an Associate Professor and Research Programme Leader at Research in Education, Amsterdam UMC, Faculty of Medicine Vrije Universiteit Amsterdam, Amsterdam, the Netherlands.
References
- Akhtar-Danesh N. 2016. An overview of the statistical techniques in q methodology: is there a better way of doing Q analysis? Operant Subjectivity. 38(3–4):29–36.
- Berkhout JJ, Teunissen PW, Helmich E, van Exel J, van der Vleuten CP, Jaarsma DA. 2017. Patterns in clinical students’ self-regulated learning behavior: a Q-methodology study. Adv Health Sci Educ Theory Pract. 22(1):105–121.
- Biggs JB, Tang C. 2011. Teaching for quality learning at University. 4th ed. Maidenhead: McGraw Hill Education & Open University Press.
- Brown SR. 1980. Political subjectivity: applications of Q methodology in political science. New Haven (CT): Yale University Press.
- Chi MTH. 2009. Active-constructive-interactive: a conceptual framework for differentiating learning activities. Top Cogn Sci. 1(1):73–105.
- Chiu Y-L, Liang J-C, Hou C-Y, Tsai C-C. 2016. Exploring the relationships between epistemic beliefs about medicine and approaches to learning medicine: a structural equation modeling analysis. BMC Med Educ. 16(1):181.
- Deslauriers L, McCarty LS, Miller K, Callaghan K, Kestin G. 2019. Measuring actual learning versus feeling of learning in response to being actively engaged in the classroom. Proc Natl Acad Sci USA. 116(39):19251–19257.
- Dinsmore DL, Alexander PA. 2012. A critical discussion of deep and surface processing: what it means, how it is measured, the role of context, and model specification. Educ Psychol Rev. 24(4):499–567.
- Dotters-Katz S, Hargett CW, Zaas AK, Criscione-Schreiber LG. 2016. What motivates residents to teach? The attitudes in clinical teaching study. Med Educ. 50(7):768–777.
- Eastwood JL, Koppelman-White E, Mi M, Wasserman JA, Krug Iii EF, Joyce B. 2017. Epistemic cognition in medical education: a literature review. Int J Med Educ. 8:1–12.
- Entwistle NJ. 1991. Approaches to learning and perceptions of the learning environment. High Educ. 22(3):201–204.
- Fokkema JP, Scheele F, Westerman M, van Exel J, Scherpbier AJ, van der Vleuten CP, Dorr PJ, Teunissen PW. 2014. Perceived effects of innovations in postgraduate medical education: a Q study focusing on workplace-based assessment. Academic medicine: journal of the Association of. Acad Med. 89(9):1259–1266.
- Frambach JM, Driessen EW, Beh P, van der Vleuten CPM. 2014. Quiet or questioning? Students’ discussion behaviors in student-centered education across cultures. Stud High Educ. 39(6):1001–1021.
- Graffam B. 2007. Active learning in medical education: strategies for beginning implementation. Med Teach. 29(1):38–42.
- Guckian J, Eveson L, May H. 2020. The great escape? The rise of the escape room in medical education. Future Healthc J. 7(2):112–115.
- Henderson C, Dancy M, Niewiadomska-Bugaj M. 2012. Use of research-based instructional strategies in introductory physics: Where do faculty leave the innovation-decision process? Phys Rev ST Phys Educ Res. 8(2):e020104.
- Irby DM, Wilkerson L. 2003. Educational innovations in academic medicine and environmental trends. J Gen Intern Med. 18(5):370–376.
- Jacobs JC, van Luijk SJ, Galindo-Garre F, Muijtjens AM, van der Vleuten CP, Croiset G, Scheele F. 2014. Five teacher profiles in student-centred curricula based on their conceptions of learning and teaching. BMC Med Educ. 14(1):220.
- Khatri R. 2010. Investigating students’ perceptions of E-learning within an occupational therapy program. Operant Subjectivity. 33(1/2):84–100.
- Kilgour JM, Grundy L, Monrouxe LV. 2016. A rapid review of the factors affecting healthcare students’ satisfaction with small-group, active learning methods. Teach Learn Med. 28(1):15–25.
- Mann KV. 2011. Theoretical perspectives in medical education: past experience and future possibilities. Med Educ. 45(1):60–68.
- Mattick K, Knight L. 2009. The importance of vocational and social aspects of approaches to learning for medical students. Adv Health Sci Educ Theory Pract. 14(5):629–644.
- McKeown B. 2001. Loss of meaning in likert scaling: a note on the. Q Methodolog Alternat. Operant Subject. 24(4):201–206.
- Michael J. 2007. Faculty perceptions about barriers to active learning. College Teach. 55(2):42–47.
- Onyura B, Baker L, Cameron B, Friesen F, Leslie K. 2016. Evidence for curricular and instructional design approaches in undergraduate medical education: an umbrella review. Med Teach. 38(2):150–161.
- Owens DC, Sadler TD, Barlow AT, Smith-Walters C. 2020. Student motivation from and resistance to active learning rooted in essential science practices. Res Sci Educ. 50(1):253–277.
- Perry WG. 1968. Patterns of development in thought and values of students in a liberal arts college: a validation of a scheme. Cambridge (MA): Bureau of study counsel, Harvard University.
- Ramlo S. 2016. Mixed method lessons learned from 80 years of Q methodology. J Mixed Meth Res. 10(1):28–45.
- Roberts JK, Hargett CW, Nagler A, Jakoi E, Lehrich RW. 2015. Exploring student preferences with a Q-sort: the development of an individualized renal physiology curriculum. Adv Physiol Educ. 39(3):149–157.
- Rocca KA. 2010. Student participation in the college classroom: an extended multidisciplinary literature review. Communicat Educ. 59(2):185–213.
- Schmolck P. 2014. PQmethod Version 2.35.
- Schneider M, Preckel F. 2017. Variables associated with achievement in higher education: a systematic review of meta-analyses. Psychol Bull. 143(6):565–600.
- Schommer M. 1994. Synthesizing epistemological belief research: tentative understandings and provocative confusions. Educ Psychol Rev. 6(4):293–319.
- Srivastava T, Waghmare L. 2016. Tutorial in medical education: a review of contextual modifications. Natl J Physiol Pharm Pharmacol. 6(6):494.
- Stephenson W. 1993/1994. Introduction to Q-methodology. Operant Subjectivity. 17(1/2):1–13.
- van Herwaarden CLA, Laan RFJM, Leunissen RRM. 2009. The 2009 framework for undergraduate medical education in the Netherlands. Utrecht, the Netherlands: Dutch Federation of University Medical Centres.
- Watling CJ, Ginsburg S. 2019. Assessment, feedback and the alchemy of learning. Med Educ. 53(1):76–85.
- Watts S, Stenner P. 2005. Doing Q methodology: theory, method and interpretation. Qual Res Psychol. 2(1):67–91.
- Watts S, Stenner P. 2012. Doing Q methodological research: theory, method and interpretation. Los Angeles (CA): Sage Publications.
- Young JM, Shepardson DP. 2018. Using Q methodology to investigate undergraduate students’ attitudes toward the geosciences. Sci Ed. 102(1):195–214.