Abstract
Purpose
The hope that reliably testing clinicians’ competencies would improve patient safety is unfulfilled and clinicians’ psychosocial safety is deteriorating. Our purpose was to conceptualise ‘mutual safety’, which could increase benefit as well as reduce harm.
Methods
A cultural-historical analysis of how medical education has positioned the patient as an object of benefit guided implementation research into how mutual safety could be achieved.
Results
Educating doctors to abide by moral principles and use rigorous habits of mind and scientific technologies made medicine a profession. Doctors’ complex attributes addressed patients’ complex diseases and personal circumstances, from which doctors benefited too. The patient safety movement drove reforms, which reorientated medical education from complexity to simplicity: clinicians’ competencies should be standardised and measurable, and clinicians whose ‘incompetence’ caused harm remediated. Applying simple standards to an increasingly complex, and therefore inescapably risky, practice could, however, explain clinicians’ declining psychosocial health. We conducted a formative intervention to examine how ‘acting wisely’ could help clinicians benefit patients amidst complexity. We chose the everyday task of insulin therapy, where benefit and harm are precariously balanced. 247 students, doctors, and pharmacists used a thought tool to plan how best to perform this risky task, given their current clinical capabilities, and in the sometimes-hostile clinical milieus where they practised. Analysis of 1000 commitments to behaviour change and 600 learning points showed that addressing complexity called for a skills-set that defied standardisation. Clinicians gained confidence, intrinsic motivation, satisfaction, capability, and a sense of legitimacy from finding new ways of benefiting patients.
Conclusion
Medical education needs urgently to acknowledge the complexity of practice and synergise doctors’ and patients’ safety. We have shown how this is possible.
1. The need for reform in medical education
What more than anything arouses involvement, effort, emotion, excitement, and frustration among frontline hospital staff is encounters with real live patients. (Engeström Citation2018)
In the early twenty-first century, public concern that medical practice was harming patients (Kohn et al. Citation2000) undermined confidence in the medical profession. The rise of competency-based medical education (CBME: (Carraccio and Englander Citation2013)) to the status of a paradigm coincided with, and seems to have resulted from, pressure to improve safety (Holmboe et al. Citation2017). Experience has shown, though, that improving healthcare safety is far more complex than assuring individual competence. Meanwhile, a worrying new threat to healthcare is emerging: doctors, globally, appear less motivated to benefit patients (Nishigori Citation2020). Work-life balance is influencing trainees’ choice of subspecialty (Douglas et al. Citation2018). Trainees’ poor psychosocial health, which causes sickness absences and career breaks, (West and Coia Citation2019; Dornan et al. Citation2020; Wilson and Simpkin Citation2020) is worsening the already problematic fragmentation of healthcare teams (Holmboe et al. Citation2011). This article reports a series of thematically linked projects (a programme), which explored the history of reform in medical education and how future healthcare could be made safer for doctors as well as patients. The aim was to explore how ‘mutual safety’ could be 1) conceptualised and 2) optimised.
Hippocrates, in the 5th century BC, elevated medicine to the status of a profession by asking doctors to swear an oath, which remains a moral foundation of medical practice. (Hippocratic Oath Citationn.d.) The Hippocratic oath obliged doctors to ensure that artful use of treatments was more likely to benefit than harm patients. The oath placed the education of doctors on a firm foundation too: teaching is a moral imperative; education should be integral to practice; and students should perpetuate professional behaviours when they eventually become teachers. Accordingly, this article assumes that medical education should optimise benefit to patients.
Practice points
Doctors’ demotivation and poor psychological health are becoming serious threats to healthcare safety.
Doctors’ complex mix of attributes provides the human touch, which makes healthcare much greater than a series of correct actions.
There is an inherent tension between the recent rule that patients must not be harmed and the time-honoured rule that patients should benefit as much as prevailing circumstances allow.
Simplifying doctors’ work to standardised competencies allows the assessment tail to wag the clinical practice dog.
Mutual safety capitalises on synergies between their individual best interests to optimise patient benefit and bolster doctors’ confidence, intrinsic motivation, satisfaction, and wish to continue practising.
The unfolding narrative that follows recapitulates the course of a research programme. Section 2 argues that medical practice and education are two tightly linked aspects of a single complex activity. Section 3 uses Cultural-Historical Activity Theory (CHAT (Engeström Citation2018)) to identify tensions that result from regarding medical education as simple. Section 4 reports a complex intervention, which used CHAT to advance Section 3’s argument. Section 5 evaluates the programme and Section 6 proposes implications for practice and research.
2. The complexity of practice
Previous authors have debated whether medical education is better conceptualised as simple or complex (Regehr Citation2010; Norman Citation2011; Cristancho et al. Citation2019; Woodruff Citation2019). Simplicity is well exemplified by training non-clinicians to perform basic life support. (BLS) When a person collapses in the street and has no signs of life, THE solution is to compress their chest and inflate their lungs rhythmically. Doing this competently on a manikin fulfils one condition to become a first-aider. Treating breast cancer is, of course, more complicated than BLS. A radiologist interprets the patient’s mammogram, a cytologist interprets the biopsy, a surgeon performs the mastectomy, and an oncologist gives chemotherapy. Despite more people and technologies being involved, advocates for the simplicity of CBME assume that individual competence is the educational key to safer care. Simplicity advocates assume that breast cancer is, ultimately, a standard disease (a ‘determinate situation’) which will respond in predictable ways to standardised clinical behaviour. If a woman has a poor outcome, it follows logically that someone or something in the system performed incompetently.
Advocates for complexity would argue that human health and wellbeing is not merely a binary between benefit and harm. Patients and clinicians are individuals with values and free will (agency), which allow them to work together well one day and less well the next. Technologies can behave unpredictably too: a biopsy may be unsuitable for analysis, equipment may fail, and any powerful therapy can have side-effects, some of which are unpredictable. Occasionally, all these things will go wrong at once with potentially disastrous consequences though, serendipitously, no harm might occur, or even benefit. Complexity thinkers would argue that it would better serve a woman to treat HER breast cancer as a part of a greater whole and acknowledge her individuality.
It would be silly to suggest that BLS is better served by complexity thinking or, indeed, psychoanalysis by simplicity thinking. In between those extremes, the best way of conceptualising clinical problems is less clear. If ability to take the right action were the only criterion for choosing a doctor, patients would be better served by robots than human beings. In reality, doctors’ complex mix of attributes provides ‘the human touch’, which makes healthcare far more than a series of correct actions. As life expectancy increases and health technology advances, doctors manage ever more indeterminate problems, resulting from multi-morbidity, interactions between psychological, social, and somatic causes of ill health, and the contributions of multiple actors. Doctors who are skilled at addressing biological problems may be incapable of addressing psychosocial ones because allowing a ‘simple’ disease to be indeterminate takes them outside their comfort zone. The under-resourced, busy contexts, and anti-social hours in which doctors have to deliver care and the unpredictable potential for treatment of serious diseases to cause harm as well as benefit can make the simplest problems indeterminate. Having used the term indeterminate and determinate to explain why education and practice can be conceptualised as complex or simple, we will now only use the latter terms.
This research assumes, as Hippocrates mandated, that human agency should be allowed to make clinical situations complex (Callus et al. Citation2020). Doctors’ most important tasks, therefore, are to interpret situations (Cristancho et al. Citation2017) and increase the agency of patients and fellow clinicians in order to solve these. Such complex relationships can only truly exist in real practice. The contexts in which doctors learn to care for patients must therefore be the contexts where doctors balance real benefit and harm. Education research within this complexity is in its infancy.
3. A cultural history of the present
3.1. CHAT as an example of complexity thinking
Vygotsky, who laid the foundations of CHAT, (Wertsch Citation1991) departed from the simplicity assumptions of his compatriot Pavlov, whose psychology emphasised the deterministic effect of environmental stimuli on human behaviour. Vygotsky explored, experimentally, how interactions with people, material artefacts, and the language of learning environments, create a complex ‘Zone of Proximal Development’, which gives children agency to learn and develop. This process is cultural-historical, because the influences that mediate learning are products of the history of the culture in which children and adults learn. By mediating learning, these influences become part of their identities. Vygotksy’s theory is a social one because it regards individual agency as part of a greater, social whole. Leontiev (Johnston and Dornan Citation2015) incorporated Vygotsky’s concept of mediated learning in his formulation of what is now known as CHAT.
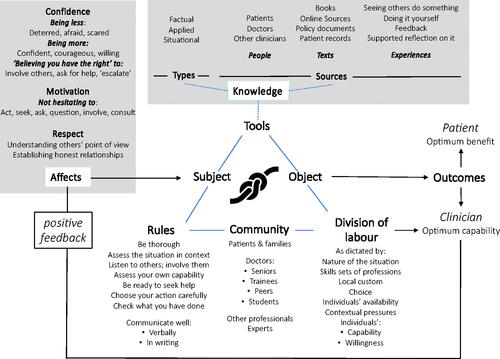
The central assumption of CHAT is that people learn by participating in social activities. Every activity is orientated towards an ‘object’. The object has been described as ‘a vision, often utopian’, which the activity makes concrete (Sannino et al. Citation2016). Section 1 explained how Hippocrates made the patient the object of the activity of medical education. Clinicians are the subjects of this activity, which has two main outcomes: patient benefit, and clinical education. Members of clinical communities optimise those outcomes by dividing the labour of caring for patients. As clinicians learn and change, practice communities do so too. Clinical activity is mediated by tools (e.g. stethoscopes), the language of practice, and tacit or explicit rules (eg to maintain confidentiality). Interactions between these factors are orientated towards the patient as the cultural-historical object of medical education.
CHAT is a complexity theory because it regards any activity as an open system, which feeds back on itself and is open to external influences. This complexity underpins CHAT’s most important contribution to practice improvement: ‘contradictions’ are inevitable features of any activity system (Engeström Citation2018). Carefully examining these can optimise benefit. In medical education, the imperative to manage a demanding workload by practising faster, for example, may contradict the imperative to practise slower, for the sake of better clinical education. CHAT encourages clinical educators faced with such a contradiction to consider whether, for example, a division of labour that gave students greater agency to define patients’ complex problems before a trained clinician saw them could be cost-effective. This article explores an inherent contradiction between the simplicity rule ‘doctors should be trained not to harm patients’ and the complexity rule ‘doctors should be educated to benefit patients as much as possible under prevailing circumstances’.
CHAT follows Lewin’s maxim that the best way to understand a complex problem is to try to change it, (Krapp Citation2015) which is a reason for medical education researchers to change practice, not just observe it. The term ‘formative intervention’ describes change projects conducted by CHAT researchers (e.g. (Engeström Citation2018; Diniz et al. Citation2021; Meijer et al. Citation2021; Morris et al. Citation2021)) and the term ‘expansive learning’ describes the catalytic process that turns contradictions into new educational possibilities.
3.2. Flexner bringing science to bear on complex situations
In the early twentieth century, the professional imperative to balance benefit and risk was accentuated by developments in laboratory science, which now made it possible for ‘a random patient with a random disorder, who consulted a physician chosen at random, (to have) a better than 50-50 chance of benefiting from the encounter ‘(Ludmerer Citation1985). The quality of medical education was compromised, though, by a contradiction. Business-minded Deans had changed the patient from Hippocrates’ moral object of benefit to a fiscal object of revenue from students’ fees. The activity of medical education used out-of-date knowledge as an instructional tool and reduced students – the subjects of the activity - to rote-learners. This resulted in a very variable and often low standard of medical education (Bonner Citation2002).
The Carnegie Foundation for the Advancement of Teaching commissioned a visionary pedagogue, Abraham Flexner, to recommend how to optimise benefit. His report (Flexner Citation1910) argued that the biopsychosocial nature of clinical problems made them complex. Doctors had, therefore, to choose optimum courses of action within the limits of medical knowledge and technology. Science was a tool that could help students learn to ‘study patients’ actual situations with keen attention, and free of presuppositions.’ Students had to learn how to integrate, critically, a wide range of knowledge and continue to do so lifelong.
Flexner reset the rules to two years of university-provided education with stiff entry requirements preceding two years of deep immersion in practice. Recognising the epistemic complexity that was resulting from the rapid expansion of medical knowledge, Flexner used the elite Johns Hopkins University as a model for his recommendations. He did not, as Lewin would have advised, test the effects of his recommendations before finalising them, with the undesirable consequence that US medical education became less accessible to women and members of minorities. His careful analysis did, though, turn a contradiction at one moment in history into enduring, global improvement in the quality of medical education.
3.3. Reducing harm simplistically
In the final years of the twentieth century, opinion leaders were advocating strongly for curricula to have defined, measurable learning outcomes. The twenty-first century was ushered in by the influential report ‘To err is human’, which begins with the sentence: ‘Health care in the United States is not as safe as it should be – and can be’ (Kohn et al. Citation2000). Education researchers had, meanwhile, developed two eminently implementable tools: simulation; and reliable assessments of clinicians’ ability to demonstrate competencies under test conditions (Reid et al. Citation2021). CBME, the result, was a trinity of assessing simple outcomes in simplified contexts to make simple judgements of individuals’ fitness to practise. CBME brought medicine within educators’ control.
The year 2010 marked the centenary of the Flexner report. The Carnegie Foundation commissioned influential scholars to recommend, anew, how to educate doctors to benefit American people (Cooke et al. Citation2010). The Lancet commissioned experts to recommend ways of improving global health (Frenk et al. Citation2010). Both reports recommended that clinicians’ competencies should be standardised, which consolidated CBME’s status as a paradigm. The recommendations introduced new contradictions, though, which presents in detail. Recommending that doctors should approach patients holistically acknowledged implicitly that clinical problems are complex, and yet competence is simple. It was proposed that (inter)nationally agreed, standardised competencies should be the currency of a global, interprofessional labour market. argues that such a huge Lego model of interchangeable competencies could never have been agile enough to address a real global health threat like COVID-19. Later publications (Irby and Hamstra Citation2016) showed that these contradictions arose because assessment, which requires simplicity for reliability, was wagging the dog of professional practice, whose strength lies in the ability of doctors to manage complexity.
Table 1. Contradictions that result from attempting to reduce harm simplistically.
The most potentially damaging contradictions result from changing the object of medical education from the time-honoured complex object (patient-as-optimal-benefit-despite-risk) to a simple object (patient-as-no-harm). This transformed a professional education, which made doctors ‘useful’ because they could benefit patients, to a market-oriented training, which would give doctors the right to earn in exchange for certified competence. It also divorced education, which was now to be simple, from the stubbornly complex practice of healthcare. Since the time of Hippocrates, students had entered medicine to fulfil their professional vocation to manage complex, risky situations in order to benefit patients. This had been motivating enough for doctors both to work long days and get out of bed at night. Certification of competence could never substitute for this. More demotivating still, the simplistic logic that equates competence with benefit makes it possible to equate harm with incompetence. CBME placed medical professionalism in a harmful bind, which could compromise doctors’ intrinsic motivation to care for patients.
Theory and empirical evidence suggest that this contradiction has, indeed, compromised clinicians’ professionalism. Anyone whose work is emotionally demanding is prone to burnout and poor mental health (Samra Citation2018). Doctors are prone to burnout; (Simpkin et al. Citation2018) more so than non-doctors, despite being more resilient (West and Coia Citation2019). Poor psychological safety, reluctance to speak about personally sensitive matters, and feelings of inadequacy are endemic in medical workplaces (West and Coia Citation2019; Atherley and Meeuwissen Citation2020). Student clinicians are particularly susceptible to negative emotions and poor mental health, particularly when supervisors have unreasonable expectations, behave unsupportively, and regard sharing doubts and seeking help as signs of weakness (Dyrbye and Shanafelt Citation2016; Atherley and Meeuwissen Citation2020). Clinicians who feel psychologically unsafe deliver less good care (Atherley and Meeuwissen Citation2020). CBME, by creating identity conflict between external and internal ideals within a risky practice, could cause ‘pathological altruism’, (Samra Citation2018) where tensions between doctors’ wishes to do the best for patients and the scope to do so result in aberrant behaviour (Sun Citation2018).
Clinicians, we conclude, are entitled to be ‘safe’ and patients can benefit from this. Education must reacknowledge the complexity and inherent risk of medical practice. We conceptualise ‘mutual safety’ as a biopsychosocial good, which results from developing clinicians’ capability to optimise benefit and minimise harm. Mutual safety is equitably distributed between patients and clinicians, capitalises on synergies between their interests, and sustains clinicians’ intrinsic motivation. Education and healthcare are, according to this conceptualisation, two closely related parts of a single practice, which is made complex by patients’ and clinicians’ exercise of agency. Since health problems are more or less complex, the safest clinicians will be those who are familiar with complexity, can attend to contextual factors, and analyse problems before trying to solve them. Because of its complexity, mutual safety can only exist as an aspiration, which energises healthcare education and practice. Section 4 reports a formative intervention, whose goal was to refocus medical education on the patient in order to expand the possibilities for mutual safety.
4. A formative intervention to optimise mutual safety
4.1. The research programme
All individual empirical projects that contributed to this programme had research ethics approval. The work took place in Northern Ireland (NI), a region of the United Kingdom (UK) with a population of two million people. Health and Social Care is delivered by five Health and Social Care Trusts, which are part of the UK National Health Service (NHS). NI had one medical school until recently and has one agency responsible for postgraduate medical education and one for postgraduate pharmacy education. Two universities jointly educate postgraduate nurses.
4.2. Articulating the problem
The starting point was an intersection between medical education and practice, where harm results from clinical care provided by foundation trainees (FTs: newly qualified doctors in generalist 2-year residencies). The NHS, which provides FTs’ workplace education, depends heavily on them to look after hospitalised patients under sometimes scanty supervision. In 2007, the national regulator of foundation training, concerned that FTs’ prescribing was harming patients, commissioned us to measure the frequency of errors and examine their causes (The EQUIP study (Dornan et al. Citation2009)). We found that over 9% of their prescriptions contained errors, which often resulted from the complexity of practice in difficult working conditions. We next conducted a randomised controlled trial of giving FTs feedback on errors in antibiotic prescriptions. A pharmacist used behavioural techniques in small group discussions to empower FTs to address error-producing conditions in everyday practice. This reduced the prevalence of error (McLellan et al. Citation2016).
4.3. Creating urgency by highlighting a bind
National policy, however, was still dominated by CBME so we chose next to research a problem that defies simplistic solutions: using insulin to treat hospitalised patients with diabetes. Insulin is a powerful drug. Too little allows blood glucose to becoming damagingly high (hyperglycaemia) and too much makes blood glucose damagingly low (hypoglycaemia). The ‘therapeutic window’ between these extremes is narrow and unpredictably variable in sick, hospitalised patients. This creates a bind because prescribing the same insulin dose could, on one day, cause a patient to become hypoglycaemic (incompetent act) on the next day optimise blood glucose (competent act), and on the next day allow blood glucose to become dangerously high (incompetent act, for diametrically opposite reason to hypoglycaemia). Experience teaches doctors to optimise benefit, whilst accepting that harm cannot be eliminated completely. Insulin treatment is an important problem because FTs write about 70% of prescriptions for the people with diabetes who occupy 1 in 6 UK hospital beds. The error rate for insulin prescriptions is four times greater (30% or higher) than for prescriptions overall and extended hospital stays, hypoglycaemia, and hyperglycaemia are endemic. No nationally coordinated improvement effort has resulted and the most serious ill-effects of diabetes care have barely improved over the last decade (Rayman and Kar Citation2020).
4.4. Turning the bind into possibilities for expansive learning
The term expansive learning describes how CHAT helped us address the contradictions in and move towards a more collaborative and future-focused way of practising.
4.4.1. Forming a community
describes how we formed a community of diabetes care and clinical education to change practice.
Table 2. How the intervention was designed to turn contradictions into expansive learning.
4.4.2. Critically questioning present assumptions
The team’s attempts to implement best evidence (from our own trial: Section 4.2) identified further binds. First, a simplistic distinction between error and non-error proved unhelpful for insulin because, whilst errors could be identified retrospectively when they caused harm, the team found most errors indefinable prospectively for reasons explained in Section 4.3. Second, the low staffing level that makes practice harmful also stops FTs being released simultaneously for group education. These limitations demanded a new solution.
4.4.3. Modelling the new solution
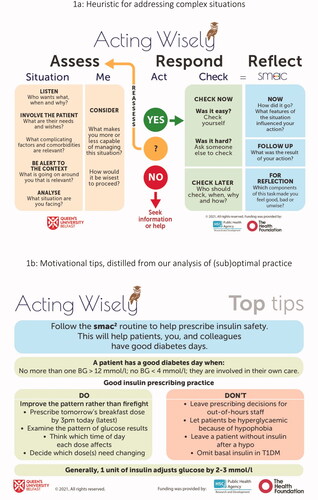
Optimising mutual safety in complex clinical situations requires clinicians to learn new behaviours, for which Capability-Opportunity-Motivation-Behaviour (COM-B) theory provides a framework (Michie et al. Citation2011). This theory predicts that clinicians will adopt new behaviours when they are motivated to do so. ‘Motivation’ is of two types: reflective (deliberate), and automatic (habit). Clinicians need to break unsuitable, automatic habits and refocus their motivation into a more deliberative type of behaviour. Two main factors influence this motivation: clinicians’ psychological capability, and the opportunities provided by the social environments in which clinicians practice. Theories about clinical harm, (Reason Citation2008) uncertainty, (Fox Citation2000) and implementation science (Damschroder Citation2020) augmented COM-B to provide a heuristic (thought tool) shown in and a pedagogy described in , whose aim was to help clinicians learn to act wisely.
4.4.4. Testing and implementing the model
The thought tool was used in two ways. One was to help clinicians behave in mutually safe ways at the point of caring for patients. The other was to help them reflect, after the event, on personally significant experiences and learn mutually safer future behaviours.
4.4.5 Consolidating and transferring the practice
Between 2017 and 2020, we educated 249 clinicians (141 FT1 and 23 FT2 trainees, 79 senior medical students, and 6 prescribing pharmacists) in 243 reflective conversations. The conversations were facilitated on 118 occasions by pharmacists and on 60, 51, and 14 occasions respectively by doctors, nurses, and people with diabetes. We also transferred the pedagogy to regional curricula for nurse and pharmacist prescribers, not described in detail here.
5. Evaluation
The 247 conversations resulted in approximately 1000 commitments to behaviour change and 600 learning points, which included both intellectual and practical capabilities and affects such as becoming less fearful and more confident, motivated, and rewarded. These quotations show how, by legitimising complexity, the intervention increased two participants’ agency:
I learned that, in between a good and a bad decision, there is often a ’valid decision’, which can help manage patients safely. With insulin, a valid decision is often the only option. (Dyad: FT1 - Pharmacist as discussant)
(I learned that), if I can justify my actions and document them thoroughly, patient care can be safer and more effective. (FT1 – Pharmacist)
The following narrative, , and describe how the intervention helped clinicians break out of the bind created by the simplistic object of solely avoiding harm and, by positioning patients as the object of optimum benefit, improved mutual safety.
Table 3. How the intervention made practice potentially safer for clinicians.
5.1. Breaking out of binds
We coined the term ‘hypophobia’ to describe how an overriding fear of causing hypoglycaemia exposed patients to harm caused by hyperglycaemia. This quotation describes a clinician learning to break out of that bind:
Insulin prescribing scared me throughout medical school; in the early stages of F1, I feared giving someone too much insulin so tended to let them run high. I looked at the (test results from the previous day) and tended not to make too many changes to doses even if the patient’s blood glucose was high. (FT1 – Pharmacist)
5.2. Optimising benefit to patients
Analysis of participants’ 1000 commitments to optimise practice supports three main conclusions: 1) many interacting factors made any clinical action more or less appropriate. 2) Information resources, capability to practise, patient benefit, and learning outcomes were in dynamic, bidirectional relationships with one another. 3) The processes through which these processes and outcomes interacted were, like clinical presentations and clinical actions, complex.
uses Activity Theory as a framework to represent the findings pictorially. The main tool was information. Participants drew on applied and contextual information more than the codified information provided by books and guidelines. Patients’ records gave information, which could make complex situations clearer and document previous actions, which it was ‘safe’ for clinicians to repeat. Information came from people, prior experience, and material resources but rarely, before our intervention, from any structured process of feedback. Any prescription involved at least four members of the community, vicariously if not in person: the prescriber; the patient, who may have been more expert in insulin therapy than the clinician; a nurse who may have been less experienced than the prescriber but had to administer the insulin and resuscitate the patient if hypoglycaemia resulted; and a supervising clinician, who was usually absent and sometimes less capable of treating diabetes than the prescriber. The division of labour between stakeholders was dictated by a whole range of contextual factors. Participants told us how, before the intervention, many implicit rules helped them get by, often just to the end of a shift when someone else would become responsible for the patient. shows the major effect of the intervention: changing the rules to ones that could optimise participants’ capability.
The following commitment to advocate for the patient within a hierarchically organised medical team shows the intervention increasing a junior clinician’s agency:
I won’t be afraid to speak up as the patient’s advocate and ask for clarification of plans; if one person does it maybe others will too. (FT1 – Pharmacist)
The next commitment illustrates how, as a result of the intervention, a junior clinician made a SMART commitment to embrace complexity:
I will speak to (hospitalised) patients to understand how meals in hospital compare with meals at home. Do they test at home and what results do they get? How would they manage these results themselves? (Medical student – Nurse)
The collective behaviour that optimised mutual safety is described, in CHAT terminology, as ‘knotworking’ (represented by the knot at the centre of ): ‘a rapidly pulsating, distributed, and partially improvised orchestration of a collaborative performance among otherwise loosely connected actors.’ Knotworking is, as earlier work has shown, (Lingard et al. Citation2012) very characteristic of the way clinicians practise.
5.3. Optimising benefit to clinicians
Potential benefit resulted from giving clinicians more agency to manage complex situations and become more capable as a result. shows some affective benefits, which resulted directly from optimising patient benefit. uses verbatim quotations to analyse benefit to clinicians in finer-grained detail.
6. Discussion and conclusions
Our cultural historical analysis argued, as others have done before, (Morcke et al. Citation2013) that the case for replacing supported experiential learning with CBME has not been clearly made. We argue that, to the contrary, CBME may make medical education less able to benefit patients by distancing the epistemologies of education and practice from one another. We argue, further, that this could compound the unsafety of practice by harming clinicians. While CBME remains an ideal pedagogic approach to simple educational tasks such as training clinicians to perform the many standardisable practical procedures in current use, the complexity of practice makes this alone insufficient.
We proposed that mutual, rather than individual, safety should be the goal of medical education. A potent cause of harm to patients and doctors – insulin therapy – allowed us to explore how educational interventions could address complexity. We did this by repositioning patient benefit as the object of the activity of medical education. We took a bottom-up approach, involving a wide range of clinicians who work and learn alongside doctors. We conclude that embracing complexity could increase clinicians’ practical capability, intrinsic motivation, and reward. The disillusionment of doctors makes it ever more important to pursue mutual safety.
Themes in this article have been articulated by earlier authors. Lingard used activity theory and knotworking to trouble the simplistic idea that individual competence can improve the teamworking that characterises clinical practice today (Lingard Citation2010; Lingard et al. Citation2012). Hodges used the metaphor of tea-steeping to advocate for experiential learning in the era of competencies (Hodges Citation2010). Billett demonstrated a complex relational interdependence between learners and the environments in which they learn (Billett Citation2006). He encapsulated what we also have shown: that practitioners learn by (a) engaging in work activities (‘just doing it’), (b) observing and listening, and (c) the physical and social setting of the workplace (‘just being there’) (Billett Citation2014) to which our intervention added the important element of helping student clinicians learn reflectively from those experiences. Finally, a burgeoning literature elaborates our argument that clinical indeterminacy leads to uncertainty, ambiguity, and psychological harm (Ilgen et al. Citation2019; Hancock and Mattick Citation2020). The rigour of this earlier work allowed us to focus specifically on the practical task of reshaping medical education so it can address present and future complexity, uncertainty, and harm.
Our work has important limitations. Our choice of a particularly difficult clinical task makes the transferability of our findings to other aspects of practice uncertain. The region where we did the work may not be representative of other parts of the UK, let alone other countries. Our implementation depended on the enthusiasm of our practice community. The benefits listed in are potential rather than proven and we have provided no proof that patient outcomes improved. We did, however, implement the pedagogy on a large scale and transfer it to the professions of pharmacy and nursing, to clinicians at various different stages of training, and between universities and healthcare provider organisations. We will soon report a more detailed empirical analysis of clinical indeterminacy to increase the potential transferability of the work.
The main practical implication is that education for mutual safety depends heavily on experiential learning. Reflection on experience helps learners develop agency to address future complex situations in ways that abstract teaching before the event cannot. Paradoxically, reflection on complexity can make education simple – for example, ‘don’t be hypophobic’ – without being simplistic. Another implication is that educators need to tailor educational interventions according to the complexity or simplicity of the tasks they wish to influence. We invite readers to access our tools which are covered by creative commons licenses and therefore freely available for use (Making Insulin Treatment Safer Citation2020). We will soon, also, publish our work in ‘toolkit form’ to help educators and faculty developers increase student clinicians’ capability and motivation to benefit patients.
Our work has an important implication for the value system of medical education: educators should foster a culture that supports and encourages clinicians rather than one that is quick to criticise and blame. It has an implication, also, for research: formative interventions guided by CHAT typically start when a practice community has identified a problem, are led by outsiders to practice, involve many people in regular meetings, and have practical impact at a mainly local level. In this case, a small team of clinician-educator-researchers positioned themselves as outsiders to the practice community of which they were part, took the lead in bringing the problem to light, recruited willing practitioners to represent people who could not spare time to participate in change, harnessed practice to make change, and delivered transferable outputs as well as local benefit. Our partial outsider status was at a price: our intervention is not yet fully embedded in medical foundation education regionally, let alone nationally. In mitigation, though, the transferability of the intervention allowed us to move it to other education programmes that were more ready to change.
We conclude by agreeing with Flexner that doctors are professionals and not technicians. They are of value to society because they are capable and willing to address complex problems, which require moral courage, intelligence, and tenacity. Of late, there has been a tendency to regard clinicians as no better than their most recent assessment or appraisal. The poor psychosocial health and demotivation that seems to be resulting is a wake-up call for society to value and nurture medical professionalism and encourage doctors to act wisely in the face of ever-changing and increasing complexity.
Glossary
Mutual safety: A biopsychosocial good, which results from developing clinicians’ capability to optimise benefit and minimise harm. Mutual safety is equitably distributed between patients and clinicians, capitalises on synergies between their interests, and sustains clinicians’ intrinsic motivation.
Expansive learning: A catalytic process, which turns contradictions that hold communities back from working towards a common object into possibilities to develop practice and optimise health outcomes.
Indeterminate: This adjective describes the nature of clinical situations, where multi-morbidity, interactions between psychological, social, and somatic causes of ill health, and the contributions of multiple actors complexify even the simplest patient presentations.
Acknowledgements
The authors acknowledge, with thanks, the substantial contributions to the Act Wisely programme of Rosie Donnelly, Martin Adams, Deborah Millar, Angela Carrington, Heather Daly, and Sara Carse. We thank our many colleagues in Queen’s University Belfast, the Northern Ireland Medical and Dental Training Agency, the Northern Ireland Centre for Pharmacy Learning and Development. We thank colleagues in the five Northern Ireland Health and Social Care Trusts, who are too numerous to mention. We thank Mary Tully for her central role in the whole programme and Professor Gerry Gormley for chairing the Supervisory Board. We thank the people with diabetes in Northern Ireland for acting as a constant source of encouragement, and particularly those who trained to be Patient Advocates. Finally, we thank James Brown, Stephen Doyle, Gerry Gormley, Grainne Kearney, Martina Kelly, Karen Mattick, Clare Morris, Ed Peile, Helen Reid, and Edvin Schei for their fearless critiques of earlier drafts.
Disclosure statement
The authors have no competing interests to declare.
Additional information
Funding
Notes on contributors
Tim Dornan
Tim Dornan MA, DM, FRCP, MHPE, PhD, is an internist and endocrinologist who has research doctorates in both the clinical and learning sciences. His clinical career addressed the complexity of internal medicine and diabetes care and his education career is addressing the complexity of workplace learning.
Ciara Lee
Ciara Lee BA, MB, BCh, BAO, is a medically qualified PhD student who is researching clinical uncertainty. She was a medical student, junior doctor, and researcher in the region where the research was done. She has also worked in England and now works in New Zealand.
Florence Findlay-White
Florence Findlay-White RGN, RMN, RHV, MPhil, is a former diabetes specialist nurse and clinical care adviser in a national patient-focused, interprofessional diabetes charity. She lives and works in Northern Ireland, where she uses counselling principles to educate clinicians to empower diabetic patients for self-care. She has also worked in Scotland and the Republic of Ireland.
Hannah Gillespie
Hannah Gillespie BSc, MB, BCh, BAO, is a junior doctor and PhD student researching medical students' workplace learning. She was a medical student and junior doctor, and is now a researcher in the region where the research was done.
Richard Conn
Richard Conn MB, BCh, BAO, MRCPCH, PhD, is a senior trainee paediatrician and academic clinical lecturer, whose doctoral and ongoing research is in using complexity assumptions to make medical errors a resource for improving patient care.
References
- Atherley A, Meeuwissen SNE. 2020. Time for change: overcoming perpetual feelings of inadequacy and silenced struggles in medicine. Med Educ. 54(2):92–94.
- Billett S. 2006. Relational interdependence between social and individual agency in work and working life. Mind Culture Activ. 13(1):53–69.
- Billett S. 2014. Mimetic learning at work: learning in the circumstances of practice. Dordrecht: Springer.
- Bonner T. 2002. Iconoclast. Abraham Flexner and a life in learning. Baltimore: Johns Hopkins University Press.
- Callus T, et al. 2020. Spanner in the works or cogs in a wheel? Parents and decision making for critically ill young children. In: Danbury, C, editors. Law and ethics in intensive care. 2nd ed. Oxford: Oxford University Press. p. 280.
- Carraccio CL, Englander R. 2013. From Flexner to competencies: reflections on a decade and the journey ahead. Acad Med. 88(8):1067–1073.
- Cooke M, Irby DM, O’Brien BC. 2010. Educating physicians: a call for reform of medical school and Residency. In: Carnegie foundation for the advancement of teaching. San Francisco: Jossey-Bass.
- Cristancho S, Field E, Lingard L. 2019. What is the state of complexity science in medical education research? Med Educ. 53(1):95–104. pp–10.
- Cristancho S, Lingard L, Regehr G. 2017. From problem solving to problem definition: scrutinizing the complex nature of clinical practice. Perspect Med Educ. 6(1):54–57.
- Damschroder LJ. 2020. Clarity out of chaos: use of theory in implementation research. Psychiatry Res. 283:112461. (April 2019).
- Diniz CSG, Bussadori J. C d C, Lemes LB, Moisés ECD, Prado C. A d C, McCourt C. 2021. A change laboratory for maternity care in Brazil: a motherbaby friendly birthing initiative. Medical Teacher. 43(1):19–26.
- Dornan T, et al. 2009. An in depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education. EQUIP study. London: General Medical Council.
- Dornan T, Gillespie H, Armour D, Reid H, Bennett D. 2020. Medical students need experience not just competence. BMJ. 371:m4298.
- Douglas PS, Rzeszut AK, Bairey Merz CN, Duvernoy CS, Lewis SJ, Walsh MN, Gillam L,; American College of Cardiology Task Force on Diversity and Inclusion and American College of Cardiology Women in Cardiology Council 2018. Career preferences and perceptions of cardiology among US internal medicine trainees: factors influencing cardiology career choice. JAMA Cardiol. 3(8):682–691.
- Dyrbye L, Shanafelt T. 2016. A narrative review on burnout experienced by medical students and residents. Med Educ. 50(1):132–149.
- Engeström Y. 2018. Expertise in transition. Expansive learning in medical work. Cambridge: Cambridge University Press.
- Flexner A. 1910. Medical education in the United States and Canada: a report to the Carnegie Foundation for the Advancement of Teaching. New York: Carnegie Foundation for the Advancement of Teaching.
- Fox R. 2000. Medical uncertainty. Revisited’. In: Albrecht, G., Fitzpatrick, R., and Scrimshaw, S, editors. The handbook of social studies in health and medicine (1st ed.). Thousand Oaks: Sage.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P, et al. 2010. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 376(9756):1923–1958.
- Hancock J, Mattick K. 2020. Ambiguity tolerance and psychological wellbeing in medical training: a systematic review. Med Educ. 54(2):125–137.
- Hippocratic Oath n.d. [accessed 2021 Apr 21]. https://en.wikipedia.org/wiki/Hippocratic_Oath#Text_of_the_oath.
- Hodges BD. 2010. A tea-steeping or i-Doc model for medical education? Acad Med. 85(9 Suppl):S34–S44.
- Holmboe ES, Sherbino J, Englander R, Snell L, Frank JR, ICBME Collaborators 2017. A call to action: the controversy of and rationale for competency-based medical education. Med Teach. 39(6):574–581.
- Holmboe E, Ginsburg S, Bernabeo E. 2011. The rotational approach to medical education: time to confront our assumptions? Med Educ. 45(1):69–81.
- Ilgen JS, Eva KW, de Bruin A, Cook DA, Regehr G. 2019. Comfort with uncertainty: reframing our conceptions of how clinicians navigate complex clinical situations. Adv Health Sci Educ Theory Pract. 24(4):797–809.
- Irby DM, Hamstra SJ. 2016. Parting the clouds. Acad Med. 91(12):1606–1611.
- Johnston J, Dornan T. 2015. Activity theory: mediating research in medical education. In: Cleland, J, Durning, S. J., editors. Researching medical education. Chichester: Wiley Blackwell.
- Kohn L, Corrigan J, Donaldson M. 2000. To err is human: building a safer health system. Washington (DC): Committee on Quality of Health Care in America, Institute of Medicine.
- Krapp K. 2015. A study guide for Kurt Lewin. Framington Hills: Gale.
- Lingard L. 2010. Rethinking competence in the context of teamwork. In: Hodges, B. D., Lingard, L., editors. The question of competence: reconsidering medical education in the twenty-first century. Ithaca: ILR Press.
- Lingard L, McDougall A, Levstik M, Chandok N, Spafford MM, Schryer C. 2012. Representing complexity well: a story about teamwork, with implications for how we teach collaboration. Med Educ. 46(9):869–877.
- Ludmerer KM. 1985. Learning to Heal: the Development of American Medical Education. New York: Basic Books.
- Making Insulin Treatment Safer 2020. [accessed 2021 July 12]. http://www.med.qub.ac.uk/mits/.
- McLellan L, Dornan T, Newton P, Williams SD, Lewis P, Steinke D, Tully MP. 2016. Pharmacist-led feedback workshops to increase appropriate prescribing of antimicrobials. J Antimicrob Chemother. 71doi 10.109(5):1415–1425.
- Meijer LJ, de Groot E, Honing-de Lange G, Kearney G, Schellevis FG, Damoiseaux RAMJ. 2021. Transcending boundaries for collaborative patient care. Medi Teach. 43(1):27–31.
- Michie S, van Stralen MM, West R. 2011. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 6(1):42.
- Morcke A, Dornan T, Eika B. 2013. Outcome (competency) based education: an exploration of its origins, theoretical basis, and empirical evidence. Adv Health Sciences Educ Theory Pract. 18(4):851–863.
- Morris C, Reid A-M, Ledger A, Teodorczuk A. 2021. Expansive learning in medical education: putting Change Laboratory to work. Med Teach. 43(1):38–43.
- Neve H, Hanks S. 2016. When I say … capability. Med Educ. 50(6):610–611.
- Nishigori H. 2020. Why do doctors work for patients? Medical professionalism in the era of neoliberalism. [Thesis]. Maastricht (NL): Maastricht University.
- Norman G. 2011. Chaos, complexity and complicatedness: lessons from rocket science. Med Educ. 45(6):549–559.
- Rayman G, Kar P. 2020. National diabetes inpatient audit, England, 2019. Leeds: NHS digital.
- Reason J. 2008. The human contribution. Unsafe acts, accidents, and heroic recoveries. Boca Raton (FL): CRC Press.
- Regehr G. 2010. It's NOT rocket science: rethinking our metaphors for research in health professions education. Med Educ. 44(1):31–39.
- Reid H, Gormley GJ, Dornan T, Johnston JL. 2021. Harnessing insights from an activity system – OSCEs past and present expanding future assessments. Med Teacher. 43(1):44–49.
- Samra R. 2018. Brief history of burnout. BMJ. 363:k5268.
- Sannino A, Engestrom Y, Lemos M. 2016. Formative interventions for expansive learning and transformative agency. J Learn Sci. 25(4):599–633.
- Simpkin AL, Khan A, West DC, Garcia BM, Sectish TC, Spector ND, Landrigan CP. 2018. Stress from uncertainty and resilience among depressed and burned out residents: a cross-sectional study. Acad Pediatr. 18(6):698–704.
- Sun S. 2018. From defensive altruism to pathological altruism. SAGE Open. 8(2).2158244018782585.
- Wertsch JV. 1991. Voices of the mind. A sociocultural approach to mediated action. Cambridge (MA): Harvard University Press.
- West M, Coia D. 2019. Caring for doctors Caring for patients. London: General Medical Council.
- Wilson HC, Simpkin A. 2020. Why are so many doctors quitting the NHS? BMJ Opinion. [accessed 2021 Apr 21]. https://blogs.bmj.com/bmj/2020/02/06/why-are-so-many-doctors-quitting-the-nhs/.
- Woodruff JN. 2019. Accounting for complexity in medical education: a model of adaptive behaviour in medicine. Med Educ. 53(9):861–873.