Abstract
Purpose
Medical students’ transition to postgraduate training, given the complexity of new roles and responsibilities, requires the engagement of all involved stakeholders. This study aims to co-create a transition curriculum and determine the value of involving the key stakeholders throughout such transition in its design process.
Methods
We conducted a mixed-methods study involving faculty/leaders (undergraduate/postgraduate), final-year medical students, and chief residents. It commenced with eight co-creation sessions (CCS), qualitative results of which were used to draft a quantitative survey sent to non-participants, followed by two consensus-building CCS with the original participants. We applied thematic analysis for transcripts of all CCS, and mean scores with standard deviations for survey analysis.
Results
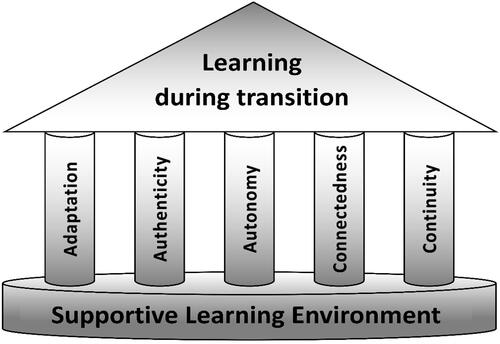
We identified five themes: adaptation, authenticity, autonomy, connectedness, and continuity, embedded in the foundation of a supportive environment, to constitute a Model of Learning during Transition (MOLT). Inclusion of various stakeholders and optimizing their representation brought rich perspectives to the design process. This was reinforced through active students’ participation enabling a final consensus.
Conclusions
Bringing perspectives of key stakeholders in the transition spectrum enriches transition curricula. The proposed MOLT can provide a guide for curriculum designers to optimize the final year of undergraduate medical training in preparing students for postgraduate training with essential competencies to be trained.
Introduction
The transition from undergraduate to postgraduate medical training is accompanied by marked change in context and responsibilities, which necessitates good preparation. This challenges medical schools, which regard students’ preparation for postgraduate training as their primary responsibility (Elnicki et al. Citation2015). This struggle is perceived by postgraduate educators, who recognize the lack of preparedness of newly graduated trainees (Lyss-Lerman et al. Citation2009; Hauff et al. Citation2014). Similarly, students feel poorly prepared to fulfil common clinical and professional responsibilities when they start postgraduate training (Benson et al. Citation2015; Minter et al. Citation2015). Wolf et al. (Citation2014) explored students’ perspectives regarding the purpose and value of the final year and recommended involving them in decisions made about modifying final year curricula and structure. Chang and colleagues also investigated new resident’s perspectives regarding their transition to residency experience (Chang et al. Citation2020). While previous work studied students’ experiences and requirements for transition, medical students’ engagement with staff in designing their transition to postgraduate training has not been fully explored. An approach to this is investigated within this study.
Medical education literature regarding active student participation in curriculum design is growing. Many approaches for involving students with learning and teaching have been advocated, yet when the aim is to optimise the efficacy of the learning environment, co-creation is the most suitable approach (Könings et al. Citation2014; Martens et al. Citation2019). It is an evolving approach that actively engages students with staff in designing an effective learning environment (Martens et al. Citation2019). It is defined as the collaborative work between staff and students in creating components of curricula and/or pedagogical approaches (Bovill et al. Citation2016). While many institutions have adopted student engagement approaches in curricular transformation and large-scale curriculum reforms and student curricular boards, there are few reports on how students currently in transition shape their preparation for postgraduate training (Milles et al. Citation2019; Scott et al. Citation2019; Geraghty et al. Citation2020).
Undergraduate curriculum development, including transition to clinical practice, is still regarded as the primary responsibility of medical schools. While many institutions have adopted student engagement approaches, deficiencies and struggles of newly graduating students are often identified by postgraduate leaders and educators. During transition, medical school graduates migrate across educational and health care systems and would most benefit from a shared responsibility to support their optimal preparation for their careers as new doctors in training (Morgan et al. Citation2020). Studies indicate that postgraduate educators and leaders have valuable expertise and views on the skills that final year students should possess before entering graduate medical education (Angus et al. Citation2014; Pereira et al. Citation2016; Pearlman et al. Citation2017). Ruskin and colleagues proposed a tripartite co-creation framework involving students with workplace partners and university staff, acknowledging the value of contributions consistent with each participant’s expertise and perspective (Ruskin and Bilous Citation2020). Thus, while students provide unique perspective on the education program through experiencing the full transition, engaging postgraduate educators and leaders in the co-creation process should bring valuable and meaningful input to the transition curriculum.
Purpose
We implemented a co-creation study involving final-year medical students with college leaders and faculty, together with clinical faculty. The power differential between students and faculty can threaten active student participation through fear of repercussions for sharing their opinion (Johnson‐Bailey and Cervero Citation1998; Stalmeijer et al. Citation2014). Creating a psychological safe environment was a prerequisite for a successful student engagement (Könings et al. Citation2021). Also, the difficulty of including all students’ voices in the design process due to class size carries the risk of gaps in student representation (Matthews et al. Citation2018; Bovill Citation2020). To optimize key stakeholder representation, the views of non-participating students and other stakeholders were explored through a questionnaire. Ultimately, we aimed to answer the following research questions: What are the components of a co-created model that are developed by engaging students in transition with college and clinical faculty and chief residents? What is the value of including stakeholders across the transition spectrum? What is the added value of optimizing stakeholder representation in the co-created model? And finally, how is students’ active participation best established in the co-creation process?
Methods
Design
A mixed-methods study was conducted in three stages, seeking the yield of a broader picture and more comprehensive support for validity (Creswell and Clark Citation2017). Eight CCS were organized, each involving faculty/leaders, either undergraduate or postgraduate, with final year medical students and chief residents. Qualitative data from these sessions were used to draft a quantitative questionnaire about the proposed ideas for the transition curriculum. It was sent to non-participants of the CCS from the four stakeholder groups to optimize the representation of the whole local community. This was followed by two consensus-building CCS that involved participants from the four stakeholder groups and yielded rich qualitative data on the final proposed curriculum.
Setting
The study was conducted at two institutions: the Qatar University College of Medicine (QU-CMED) in collaboration with Hamad Medical Corporation (HMC). HMC is the primary graduate medical training organization in the State of Qatar and holds Accreditation Council of Graduate Medical Education International (ACGME-I) accreditation. The QU-CMED program is six years, adopting an integrated curriculum in which Problem Based Learning is the main pedagogy in the early years. Upon graduation, these students join residency programs at HMC.
Participants
The study included four stakeholder groups. Using purposeful sampling, we selected medical students at the start of their final year who were identified by AA, who is a university faculty involved in students’ teaching in the pre-clinical years, as being high contributors to college activities: members of committees such as assessment and curriculum committees, and students’ association; thus they represent information-rich participants. We also invited college faculty including members of the curriculum development committee, clinical faculty (residency program or associate directors, and core faculty), and chief residents of major residency programs. These participants are involved in postgraduate and undergraduate medical education and are information-rich on the point of interest (Patton Citation2002). Invitations to take part in co-creation sessions (CCS) were via email, to include a description of the study purpose and emphasis on voluntary and confidential participation.
Additionally, all members of the different stakeholder groups were invited to fill out the questionnaire. shows participants of both the CCS and the questionnaire. Nine program directors/associate program directors/core faculty, nine college faculty/leaders, five chief residents, and 23 final-year medical students participated in the CCS. 82 out of 210 (response rate = 39%) responded to the survey; nine (45%) final year medical students, eight (53%) college faculty/leaders, 50 (35%) program directors/associate program directors/core faculty and 15 (45%) chief residents.
Table 1. Study participants.
Data collection
The principal data collection was through a total of ten online CCS between June and December 2020. To involve stakeholders who did not participate in the CCS, a questionnaire was drafted to explore their perspectives. Study approval was obtained from both QU and HMC Ethical Review Boards. Participation was voluntary and all participants provided informed consent. All responses were anonymized through coding participants’ names and de-identifying all quotes.
Co-creation session procedure
Developing the moderator guide
The CCS discussion was guided through a moderator guide (Supplementary Table 1), structured to follow the elements of Schlossberg’s transition theory (STT) as a conceptual framework. The STT is comprised of three components: (1) ‘Approaching Transitions’ which involves the identification of the individual’s perspective of where they are placed within the transition and whether they are ‘moving in,’ ‘moving through’ or ‘moving out’ (2)‘Taking stock of coping resources: The 4S system’ that involves identifying the transitioning individual’s perspective of their coping resources and places them into categories of ‘situation,’ ‘self,’ ‘support’ and ‘strategies’ and lastly (3) ‘Taking charge: strengthening resources,’ integrates several counseling techniques with the focus on developing the transitioning individual’s coping resources (Schlossberg and Goodman Citation2005). The guide was developed based on the 4S system where ‘Situation’ refers to how the transition is perceived by the trainees; ‘self’ is about personal resources needed for transition; ‘support,’ signifies the support needed for transition, and finally, ‘strategies’ describe desirable approaches that can facilitate students’ transition. All authors reviewed and adjusted the moderator guide which was further refined after debriefing on the initial two CCS.
Creating a psychological safe environment
To ensure a psychological safe environment for student engagement, participants were gathered online in the ‘main room’ at the start of each session, to provide a 20-min-orientation during which they were re-introduced to the purpose of the study, the co-creation concept including definition, goal, and the importance of including all participant voices in the discussion. The elements of a successful student partnership including power distribution, sense of belonging, inclusivity, and responsibility were explained, and participants were reassured of confidentiality and anonymization of data collection.
Conducting the session
Co-creation involves the active engagement of students in developing curricula with staff (Bovill et al. Citation2016). During the process, students collaborate with course faculty to form a curriculum planning team to design course content and processes (Mihans et al. Citation2008; Bovill Citation2014; Könings et al. Citation2021). Thus, in each session, CCS included representatives from the students and the faculty. In the first phase of this project, eight CCS were organized: three included students together with college faculty and five involved students with clinical faculty and chief residents. Each session was attended by a new group of participants. All CCS were online, each lasted for 120 min, moderated by one of the authors and attended by a scribe. After orientation, participants were divided into 2–3 breakout rooms depending on the number of participants, ensuring equal representation from faculty and students; each session included 3 students and 3 faculty. For 90 min, participants discussed key questions encompassing the final year curriculum requirements and strategies to accomplish them. After 90 min, all participants re-joined and continued a plenary discussion, after scribes shared summaries from each subgroup (30 min).
For inclusivity and to increase stakeholder representation, the proposed requirements and strategies generated during the eight CCS were summarized in a short online questionnaire. All scribe notes recorded during the eight CCS were collected together to develop a long list of strategies and support measures to prepare final-year medical students. This generated a list of 54-item-questionnaire included: 28 items that addressed the requirements for the final year and 26 items focused on the approaches to achieve those requirements (of which 18 items directly focused on strategies and 8 items focused on support). The items elicited participants’ agreement with the level of importance on a 5-point Likert scale ranging from (1) ‘Essential’ to (5) ‘Not important.’ Open-ended questions were added for additional comments. The questionnaire was reviewed by a group of six participants from the four stakeholder groups involved in the CCS for face and content validity, before sending it out to all students and staff not involved in the CCS. Invitation emails with two reminders included a description of the study and a link to the online questionnaire on the Qualtrics survey platform. The items showed acceptable internal consistencies with a Cronbach’s alpha: of .89 for the 28 items on requirements, and .94 for the 26 items focused on the strategies and support (.92 for the 18-items-strategies subscale and 0.86 for the eight-items-support subscale).
The data collected from this survey, together with the summary of the requirements and strategies in the eight CCS formed the discussion areas in two final CCS, the consensus sessions. Each of these consensus sessions included representatives from all four stakeholder groups who participated in the previous eight sessions: students, college and clinical faculty and chief residents. Discussions followed the same protocol as the eight CCS.
All discussions in the ten CCS were recorded, later transcribed, and transcripts summarised.
Data analysis
Guided by the STT, we performed a thematic analysis of the CCS transcripts using Atlas.ti qualitative software, version 8.4.0. We followed the stages of open and axial coding in an iterative process, discussed the codes, and constructed categories and subcategories in an analytic process of constant comparison (Corbin and Strauss Citation1990). Two authors SS and AA coded two CCS transcripts independently and then discussed the coding framework. SS and KK co-coded another CCS, revised the coding framework and reached a consensus. The remaining eight transcripts were then coded by SS and the codes were clustered into themes. These were discussed with all members of the research team, who reviewed the templates and the themes (including emerging themes) to reach consensus. For the questionnaire analysis on respondents’ choices of requirements and strategies that prepare students for practice, mean scores per item were calculated using the total set of item/code scores of the level of importance. In the light of the research questions, we computed mean scores per item for the questionnaire data on strategies and support. Data were analysed using Statistical Package for Social Sciences (SPSS®) version 27 (IBM Statistics for Windows; IBM Corp, Armonk, New York, USA).
Reflexivity
To ensure reflexivity, the authors have paid great attention to their practices and judgment during data collection and analysis to avoid any bias or influence. CCS were moderated by MA, AA, and AC who were not directly involved in assessing students during the clerkship phase. They introduced themselves and their background and built trust through an explanation of the study goals and content of the informed consent. The main author SS has a role as a clerkship director, involved in student teaching and evaluations; however, she engaged in reflexivity through collaboratively analyzing the data with KK, an expert in health professions education, not affiliated with the two institutions where the study was conducted. The final coding scheme was reviewed by KK, MA, and RK, and the research team for consensus.
Results
Guided by the STT, we collected and analysed the data to develop a co-created model of learning during the transition by involving students in transition together with college and clinical faculty and chief residents. The model (MOLT) is demonstrated in and includes the five pillars: Adaptation, Authenticity, Autonomy, Connectedness, and Continuity rooted in the supportive learning environment. Besides the model, we report the value of including stakeholders across the transition spectrum, the value of maximizing their representation, and finally, the dynamic nature of CCS which reflects active students’ participation. In the supporting quotes, college faculty are identified with (F), clinical faculty with (C), chief residents with (CR), and medical students with (S). All themes, categories, codes, and quotes are presented in supplementary tables 2 and 3.
The model of learning during transition (MOLT)
To answer the first research question, we identified five recurring themes as the pillars for students’ learning during transition to postgraduate education that are underpinned by a foundation of a supportive environment. Students need to adapt, be immersed in authentic experiences, provided with autonomy, feel connected and experience continuity of learning during transition.
Adaptation
Participants described the importance of students’ adaptation to the new clinical environment during transition. This included thorough orientation to clinical rotations with ‘specific goals and objectives’ (C) communicated to both students and faculty. Likewise, students need to be introduced to residency programs and familiarized with ‘the structure and approach of the institution that they are working with’ (F). Participants emphasized training students on ‘skills of resilience, time management, and work-life balance’ (F) in order for them to adapt. As expressed by students: ‘If I were allowed to know how to manage, like, what to do after the hospital, how I can come back and finish writing up my notes, at the same time studying and managing to be a student but at the same time training at the hospital, it would be great if we have some guidance on that’ (S).
Authenticity
Participants placed emphasis on authentic learning and immersing students in the real clinical environment. Learning is facilitated through shadowing experiences and providing students with more clinical responsibilities where they ‘follow the norms of the rotations’ (C), ‘are exposed to the emergencies’ (CR) and ‘own patients’ (F). In keeping with the same rationale, participants were in favour of more hands-on training, in the form of ‘simulations and case-based discussions which are better than to have lectures’ (S).
Autonomy
Participants recognized the value of students taking an active role in their learning during transition, in contrast to passive responsiveness to the change in environment. Examples suggested by participants were students determining their needs, ‘then it’s our role to, to say that we need… to be covered’ (S), taking initiative in their learning and drafting their portfolio to determine gaps in their knowledge and skills. Most participants suggested providing students with elective rotations to learn from and ‘reflect on everything and learn from every example’ (F).
Connectedness
For the students to learn in the new clinical environment, they should ‘become part of the team’ (S) and ‘should feel that they are from a part or member of the system they are rotating in or are working and so they can fit’ (C). Students feel connected to faculty through direct supervision and frequent feedback because ‘supervisors, they are not only good clinicians, they are good educators so they focus on identifying the student’s weaknesses and strengths and discuss this with students’ (S) and it is students’ ‘right to ask for supervision’ (C).
Continuity
Building on students’ learning attained during the college was described by participants as a ‘spiral concept where things are revisited and reemphasized …’ (F). Students need to build on previous knowledge and evaluate for any gaps’ (S). Moreover, sequential learning at the workplace was felt to impact students learning where students first observe, ‘get to sit down and see how it’s properly done’ (S) then perform, ‘once they’ve seen it the next time, they should be given a chance’ (C).
The foundation of learning: the supportive environment
During transition, students are challenged with the new busy clinical environment of multi-cultural and diverse population of ‘real patients with real problems, real families and relatives’ (F). Our results demonstrated that for students to learn through these five pillars, several identified support-rich resources are required, being: postgraduate educators, residents, peers, and college leaders. Clinical faculty provide students with support through supervision, feedback, and career counselling together with mentoring because ‘people fall down even later on in their career, and they always need some sort of mentorship support to get back on the feet and, you know, get back into life’ (F). They also facilitate a safe learning environment with ‘a reporting system that does not threaten the doctor to admit to the mistake’ (F). Therefore, college leaders should choose enthusiastic clinical faculty and provide them with faculty development programs, teaching awards, affiliation titles, and protected time for teaching so they become equipped to teach undergraduate medical students, had they not already the experience. Residents support students professionally through engaging them in case presentations and evidence-based medicine activities such as journal clubs. Psychologically, they help to ‘remove the stress from the first year of residency’ (S) by voicing their challenges and measures to deal with difficult times during training. Peer support was identified through ‘study groups’ (S) and ‘sort of platform that they can learn from each other’ (F). Lastly, college leaders/faculty support students through provision of psychological and career counselling because at this stage of transition, students feel ‘kind of insecure’ (F).
During the last two consensus sessions, all stakeholders reviewed strategies that emerged from the CCS. The consensus group agreed on the importance of strategies that comprises the MOLT. They noted that while the list of strategies was quite comprehensive in scope, students were looking for their current gaps at this stage of development and focused on ‘things that will have a direct impact on their practice as new residents’ (S). They concluded that the curriculum is dynamic and evolving, necessitating frequent CCS to be ‘repeated a little down the line again in time’ (F) as students progression and maturity would further determine their needs.
Value of inclusion of stakeholders across the transition spectrum
This theme aims to answer the second research question regarding the value of including stakeholders across the transition spectrum by comparing the content of the co-created model developed by students with clinical faculty and chief residents (model 1) and that developed with college faculty (model 2). The main differences were: dominance of certain pillars, the focus on preparatory measures and specification of terminologies ().
Table 2. Differences between the two models.
Dominance of certain pillars
While there was equal representation of all pillars in both models, two main pillars received more attention and dominated the discussion within the models. The authenticity pillar dominated discussions in model 1 (students with postgraduate faculty) with a detailed description of best measures to immerse students in real situations ‘Medical students should take part of graded responsibility which is the main pillar in residency training such as involved actively in on call duty, admit and do follow up on their patients’ (C). On the contrary, model 2 (students with undergraduate trainers) participants emphasized on the continuum pillar and that curriculum is built in a spiral pattern ‘which means things are revisited, reemphasized’ (F) as students advance. This implies a difference in views of stakeholders across the transition spectrum.
Focus on preparatory measures
Model 1 had more emphasis on practical measures that prepare students in transition for residency. For example, in the adaptation theme, students’ orientation to clinical rotations and introduction to various residency programs were mandatory ‘so students will be interested in specialties they will pursue and not become demotivated when they join’ (C). However, the model 2 adaptation pillar had more focus on the students’ preparation from personal perspectives such as students’ empowerment in decision making, building their skills of coping with pressure, time management, and work-life balance, and exploring their passion for medicine ‘let’s say if you like to read literature about medicine, if you like to write, try something about medicine, which means having to incorporate your passion with your medical practice’ (F). Similarly, in the autonomy pillar, the importance of reflective practice was only emphasized in model 2 with college faculty.
Specification in terminologies
Difference in specifications were identified in both models. Being involved in clinical training, participants of model 1 provided specific description of students’ clinical duties such as ‘taking on call shifts’ (S), covering ‘inpatient and outpatient services’ (CR), and ‘shadowing senior trainees’ (C) and performing their duties and taking responsibility through ‘owning patients’ (C). Moreover, they recommended specifically introducing ACGME-I competencies and assessment tools, used in postgraduate training, to students during the final year so ‘that would be an easy selling for them’ (CR). The role of supervision and feedback in students’ learning during transition was more specified in model 1. The spiral concept of learning and reflective learning was only specified in model 2.
Maximizing stakeholder representation
Stakeholder representation was maximized through a questionnaire that was sent to those who did not participate in CCS. All strategies and support measures identified from scribes’ notes in the CCS were highly rated by survey respondents with mean values ranging from 3.50 to 4.59 ( and ). Bedside teaching sessions and shadowing experiences received the highest responses while more specific courses in pain management and research skills scored the least. Teaching faculty were found to be the dominant support for students in transition, therefore allocation of enthusiastic faculty and training them to teach students in the clinical environment were highly rated as support measures that can be provided by the college. The consensus group reflected on survey respondents’ views stating that ‘It’s quite logic’ (C), ‘It is a very, very good effort to put down all these aspects’ (F), concluding that inclusivity of key stakeholders across the spectrum of transition is of high importance.
Table 3. Questionnaire responses regarding importance of strategies: mean scores and standard deviations of all respondents (N = 82).
Table 4. Questionnaire responses; importance of support measures with mean scores and standard deviations of all respondents to the questionnaire (N = 82).
Active student participation: Process analysis
To answer the third research question, we report the dynamics of the discussion to reflect active student participation in the CCS under four categories: Emotions and reactions, students’ initiation of thoughts, faculty response to students’ ideas, students’ response to faculty ideas, and thought alignment. In the following section, all C, F and CR are referred to as faculty.
Emotions and reactions
More familiarity was noticed between participants in CCS with college faculty; evident by humour and laughter, comfort with openness, addressing each other by name, and relating to their experiences during the pre-clerkship phase: ‘we have done many scenarios as you remember, Dr. XX …’ (S).
Students’ initiation of ideas and response to faculty
During all CCS, students have frequently initiated new thoughts and started new threads such as: ‘So, as graduating students, we need also …’ (S). While students showed agreement with most of faculty suggestions, they expressed disagreement with some strategies. This might be facilitated by the perceived mutual respect and compassion described below.
Faculty response to students’ ideas
This was characterized with apparent respect in all sessions. Faculty not only gave students turns to speak without interruptions, but frequently asked for permission to speak ‘I just want to speak out’ (C), ‘May I add something to what the student said before?’ (CR), In addition, they acknowledged students’ ideas by saying ‘I think the mentor issue is very good’ (C), and ‘Yeah, I agree with the thought…’ (F) and showed compassion by addressing students’ worries ‘So just want our dear students to relieve this stress about being independent and being alone in the middle for the night, having to deal with a lot of complex cases’ (CR).
Alignment of thoughts
This was achieved with frequent clarification provided by faculty in areas of debate or when students expressed their concerns by stating phrases such as: ‘we would not expect a student to know…,’ ‘this is more advanced for a newly joining resident’ (C).
Discussion
This study provides insights into the opinions of students transitioning, together with those of college and clinical faculty and chief residents that exquisitely intertwine through co-creation to develop a model for learning during the transition MOLT (). It also investigated the value of inclusivity of those stakeholders and of increasing stakeholder representation. Key emergent findings were students’ adaptation, authenticity, autonomy, connectedness, and continuity, grounded within the foundation of a supportive learning environment to facilitate student transition. Each stakeholder brought different focus and specifications to the MOLT. Expansion of stakeholders supported the final consensus on the MOLT. This is a novel study utilizing the concept of co-creation that involved students in transition in designing their final year curriculum with college and clinical faculty and chief residents. The study findings suggest the value for students, college and postgraduate training leaders in preparing students during transitions.
There was concordance among stakeholders on the five pillars that constitute the MOLT. Ideally, students should adapt to the new learning environment through clear introduction to expectations and requirements, with training in coping and time management skills during their final year of medical school. These were seen in previous studies as essential mandatory requirements for residency preparation and in lowering stress scores and prompting high academic achievement (Abdulghani et al. Citation2014; Steiner-Hofbauer and Holzinger Citation2020; Accreditation Council for Graduate Medical Education Citation2021). Authenticity, achieved by providing students with greater responsibility and shadowing experiences stood as a strong pillar. This aligns with previous study findings, resulting in enhanced students’ confidence and competency for entrustment decisions (Kitsis and Goldsammler Citation2013; Fürstenberg and Harendza Citation2017). Learning from authentic experiences needs to be maximized, with autonomy where students take initiative, reflect on their learning and determine their needs. This supports the notion of self-regulation (Berkhout et al. Citation2017) that maximizes experiential learning (White Citation2007; Woods et al. Citation2011). The pillar of students’ connectedness and integration within health professional teams is crucial and was shown in previous studies to support students’ identification as emerging doctors (van den Broek et al. Citation2020). Finally, to overcome gaps in learning during transition, the concept of continuity with spiral learning, revisiting pre-clinical material, links with previous studies demonstrating that skills learned during pre-clerkship are of great value for real-life clinical training (Margolius et al. Citation2020) and clear handover from medical school to residency facilitates smooth transition (Dallaghan et al. Citation2021). The supportive learning environment within MOLT mirrors findings in previous studies demonstrating enhanced students’ ability to formulate their learning goals and navigate the new learning environment (Berkhout et al. Citation2017) through peer and resident support, mentoring (Choi et al. Citation2019), and developing faculty as students’ supervisors (Simpson et al. Citation2019). Collectively, all these pillars are required for student transition.
Disparities in perspectives between model 1 and model 2 support the value of inclusivity (). Our discussions involving students with college faculty concentrated on the importance of personal measures such as coping and time management skills for students’ preparation. As demonstrated in previous studies, non-clinical teachers appear influenced by the learner-centred environment where their teaching role requires a good communicator, motivator, with good organizational skills (Al-Mohaimeed Citation2018). As they provide advice for students over long periods of time and see developing trends in medical student experience, they can inform on their resilience strategies (Farquhar et al. Citation2018). Our results show that the continuity pillar with spiral learning and revisiting college learning was more emphasized with college faculty in respect of bridging the ‘bumpy’ (Franzen et al. Citation2015) gap between medical school and residency. Notably, clinical teachers including residency program leads and educators perform their educational tasks in parallel to patient care and chief residents have wide responsibilities and duties, including administrative tasks (such as duty schedules) and education of junior residents and medical students (Young et al. Citation1996). Hence, sessions with postgraduate educators and CR provided specific descriptions of the clinical duties and practical measures such as authentic experiences and supervision.
Finally, it is worth considering that gathering students with curricula experts does not necessarily guarantee successful co-creation. Active student participation in co-creation requires a psychological safe environment to enhance learner motivation to participate, increase teacher motivation to listen and be open to feedback (Könings et al. Citation2021). Our discussions were characterized by respect, compassion, and acknowledgment from faculty, which facilitated students’ contribution. Previous work showed that faculty can frame co-creation by responding respectfully and appreciatively to learners’ input and feedback (Edmondson Citation2018). Finally, increasing representation of stakeholders confirmed the CCS participants’ views and added value and strength to the curriculum.
Strengths, weaknesses, and future research
In general, the components of our model are in line with previous studies. It is the model itself and its design that is novel. We consider it a strength that we were able to define pillars and the supportive environment that gave rise to the MOLT. Our co-creation design facilitated active student participation, inclusiveness of stakeholders and optimized their representation, to allow for a comprehensive model. However, the study has some limitations to be considered. Although a mixed methods approach was adopted to broaden the participation, we may not have captured a full range of opinions from non-participants. The study findings were drawn from a sample of participants, all of which belonged to a single undergraduate and a single postgraduate institution that may not be completely transferable to other institutions. Testing the effects of the implementation of the co-created transition curriculum was beyond the scope of this study, Future research might explore practical application of the MOLT in different settings and at various transition points across medical training. Since our study was undertaken in medical education, we invite investigation of its application in non-medical fields. Finally, we do not know whether the addition of other stakeholder groups, such as patients, nursing or ward pharmacy staff might further improve the MOLT. We suggest investigation of how such groups perceive and might add to the MOLT.
Implications for practice
In general, when organising transitional curricula, undergraduate institutions are encouraged to move from more traditional approaches of curriculum development and invite students and postgraduate leaders to contribute measures to enhance students’ preparation. It is worthwhile that college leaders realise that inclusion of students in transition provides rich information on their needs and gaps (Minter et al. Citation2015; Chang et al. Citation2020). Moreover, involving students with stakeholders responsible for their undergraduate and postgraduate education in a co-creation setting, further shapes the curricula to what is required (Lyss-Lerman et al. Citation2009). Curriculum designers might benefit from the MOLT in designing curricula for students in transition, focusing on the five pillars together with the supportive learning environment to provide students with rich educational experiences. This particularly holds for medical training since students move from undergraduate to postgraduate education, challenged by their new roles and responsibilities. Lastly, a psychological safe environment enables students’ openness in sharing their views of learning during transition with faculty.
Conclusions
The proposed co-created MOLT provides a model that integrates strategies and supports facets of transition and endorses a guide for developing curricula to determine a ‘fit for purpose’ final year of undergraduate medical training. This study proposes that engaging key stakeholders in the transition spectrum in co-creation bring rich perspective to the transition curriculum. This invites further research into maximizing students’ learning during transition.
Author contributions
SS, KK and RK conceptualized the study. SS, KK, MA and RK were involved in the design of the study. SS, MA, AA, AC were responsible for data collection. SS, KK, MA and AA were involved in coding and data analysis. SS, KK, SR, MA and RK were involved in the interpretation of data. SS produced the first draft of the paper but all authors (SS, KK, MA, AA, AC and RK) contributed to iterative drafting and refinement of the manuscript. All authors (SS, KK, MA, AA, AC and RK) approved the final version of the manuscript for submission.
Ethical approval
Participation was voluntary and all participants returned signed informed consent via email before participating in the study. Verbal consent was restated during the CCS orientation and obtained before recording the CCS. The survey included the research information sheet that explained the aim of the study and the autonomy participation and confidentiality. Expedited ethical approval was obtained by QU and HMC Ethical Review Boards QU-IRB 1348-EA/20 and HMC- MRC-01-20-265.
Glossary
ACGME-I: Accreditation Council of Graduate Medical Education International.
Supplemental Material
Download MS Word (23.2 KB)Acknowledgements
The authors would like to thank all students and faculty who participated from both institutions for their contribution to the developing the model of learning and most gratefully acknowledge the students who acted as scribes and Dr. Abdullatif Al-Khal the director of medical education at Hamad Medical Corporation for his support of the project.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Data availability statement
Upon reasonable request, the corresponding author can provide data generated and analysed during the study.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
Shireen Suliman
Shireen Suliman, MBBS, MEHP, is a Consultant at the Internal Medicine department at Hamad Medical Corporation and Clinical Assistant Professor and Clerkship Director at the College of Medicine, QU Health at Qatar University.
Karen D. Könings
Karen D. Könings, PhD, is as an associate professor at the department of Educational Development and Research, and the School of Health Professions Education of the Faculty of Health, Medicine and Life Sciences at Maastricht University, the Netherlands.
Margaret Allen
Margaret Allen, MD, is a senior Consultant Rheumatologist and Associate Director of Medical Education at Hamad Medical Corporation, and Associate Professor at College of Medicine, Qatar University, Doha Qatar.
Ayad Al-Moslih
Ayad Al-Moslih, MBBS, MHPE, EMDM, is the Head of preclinical education section at the College of Medicine, QU Health at Qatar University.
Alison Carr
Alison Carr, MD, FRSA, is a Professor and Associate Dean for Clinical Education in the College of Medicine, responsible for the curriculum and assessment of clinical components of the MD program in Qatar University. She is also a Senior Consultant Paediatric Anaesthetist at Sidra Medicine, Doha.
Richard P. Koopmans
Richard P. Koopmans is an internist at the Maastricht University medical Center and Professor of General Internal Medicine, Maastricht, the Netherlands.
References
- Abdulghani HM, Al-Drees AA, Khalil MS, Ahmad F, Ponnamperuma GG, Amin Z. 2014. What factors determine academic achievement in high achieving undergraduate medical students? A qualitative study. Medical Teacher. 36(sup1):S43–S48.
- Accreditation Council for Graduate Medical Education. 2021. Accreditation Council for Graduate Medical Education common program requirements. https://www.acgme.org/what-we-do/accreditation/common-program-requirements/
- Al-Mohaimeed AA. 2018. Comparison between faculty and students perspectives on the qualities of a good medical teacher: a cross-sectional study. Int J Health Sci. 12(1):15–20.
- Angus S, Vu TR, Halvorsen AJ, Aiyer M, McKown K, Chmielewski AF, McDonald FS. 2014. What skills should new internal medicine interns have in July? A national survey of internal medicine residency program directors. Acad Med. 89(3):432–435.
- Benson NM, Stickle TR, Raszka WVJ. 2015. Going “fourth” from medical school: fourth-year medical students’ perspectives on the fourth year of medical school. Acad Med. 90(10):1386–1393.
- Berkhout JJ, Helmich E, Teunissen PW, van der Vleuten CP, Jaarsma ADC. 2017. How clinical medical students perceive others to influence their self‐regulated learning. Med Educ. 51(3):269–279.
- Bovill C. 2014. An investigation of co-created curricula within higher education in the UK, Ireland and the USA. Innov Educ Teach Int. 51(1):15–25.
- Bovill C. 2020. Co-creation in learning and teaching: the case for a whole-class approach in higher education. High Educ. 79(6):1023–1037.
- Bovill C, Cook-Sather A, Felten P, Millard L, Moore-Cherry N. 2016. Addressing potential challenges in co-creating learning and teaching: overcoming resistance, navigating institutional norms and ensuring inclusivity in student–staff partnerships. High Educ. 71(2):195–208.
- Chang LY, Eliasz KL, Cacciatore DT, Winkel AF. 2020. The transition from medical student to resident: a qualitative study of new residents’ perspectives. Acad Med. 95(9):1421–1427.
- Choi AM, Moon JE, Steinecke A, Prescott JE. 2019. Developing a culture of mentorship to strengthen academic medical centers. Acad Med. 94(5):630–633.
- Corbin JM, Strauss A. 1990. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 13(1):3–21.
- Creswell JW, Clark VLP. 2017. Designing and conducting mixed methods research. Thousand Oaks (CA): Sage Publications.
- Dallaghan GLB, Alexandraki I, Christner J, Keeley M, Khandelwal S, Steiner B, Hemmer PA. 2021. Medical school to residency: how can we trust the process? Cureus. 13(4):e14485.
- Edmondson AC. 2018. The fearless organization: creating psychological safety in the workplace for learning, innovation, and growth. Hoboken (NJ): John Wiley & Sons.
- Elnicki DM, Gallagher S, Willett L, Kane G, Muntz M, Henry D, Cannarozzi M, Stewart E, Harrell H, Aiyer M, et al. 2015. Course offerings in the fourth year of medical school: how U.S. medical schools are preparing students for internship. Acad Med. 90(10):1324–1330.
- Farquhar J, Kamei R, Vidyarthi A. 2018. Strategies for enhancing medical student resilience: student and faculty member perspectives. Int J Med Educ. 9:1–6.
- Franzen D, Kost A, Knight C. 2015. Mind the gap: the bumpy transition from medical school to residency. J Grad Med Educ. 7(4):678–680.
- Fürstenberg S, Harendza S. 2017. Differences between medical student and faculty perceptions of the competencies needed for the first year of residency. BMC Med Educ. 17(1):1–8.
- Geraghty JR, Young AN, Berkel TD, Wallbruch E, Mann J, Park YS, Hirshfield LE, Hyderi A. 2020. Empowering medical students as agents of curricular change: a value-added approach to student engagement in medical education. Perspect Med Educ. 9(1):60–65.
- Hauff SR, Hopson LR, Losman E, Perry MA, Lypson ML, Fischer J, Santen SA. 2014. Programmatic assessment of level 1 milestones in incoming interns. Acad Emerg Med. 21(6):694–698.
- Johnson‐Bailey J, Cervero RM. 1998. Power dynamics in teaching and learning practices: an examination of two adult education classrooms. Int J Lifelong Educ. 17(6):389–399.
- Kitsis EA, Goldsammler M. 2013. Physician shadowing: a review of the literature and proposal for guidelines. Acad Med. 88(1):102–110.
- Könings KD, Mordang S, Smeenk F, Stassen L, Ramani S. 2021. Learner involvement in the co-creation of teaching and learning: AMEE Guide No. 138. Med Teach. 43(8):924–936.
- Könings KD, Seidel T, van Merriënboer JJ. 2014. Participatory design of learning environments: integrating perspectives of students, teachers, and designers. Instr Sci. 42(1):1–9.
- Lyss-Lerman P, Teherani A, Aagaard E, Loeser H, Cooke M, Harper GM. 2009. What training is needed in the fourth year of medical school? Views of residency program directors. Acad Med. 84(7):823–829.
- Margolius S, Papp K, Altose M, Wilson-Delfosse A. 2020. Students perceive skills learned in pre-clerkship PBL valuable in core clinical rotations. Med Teach. 42(8):902–908.
- Martens S, Meeuwissen S, Dolmans D, Bovill C, Könings K. 2019. Student participation in the design of learning and teaching: disentangling the terminology and approaches. Med Teach. 41(10):1203–1205.
- Matthews KE, Dwyer A, Hine L, Turner J. 2018. Conceptions of students as partners. High Educ. 76(6):957–971.
- Mihans R, Long D, Felten P. 2008. Power and expertise: student-faculty collaboration in course design and the scholarship of teaching and learning. Int J Scholar Teach Learn. 2(2):16.
- Milles LS, Hitzblech T, Drees S, Wurl W, Arends P, Peters H. 2019. Student engagement in medical education: a mixed-method study on medical students as module co-directors in curriculum development. Med Teach. 41(10):1143–1150.
- Minter RM, Amos KD, Bentz ML, Blair PG, Brandt C, D’Cunha J, Davis E, Delman KA, Deutsch ES, Divino C, et al. 2015. Transition to surgical residency: a multi-institutional study of perceived intern preparedness and the effect of a formal residency preparatory course in the fourth year of medical school. Acad Med. 90(8):1116–1124.
- Morgan HK, Mejicano GC, Skochelak S, Lomis K, Hawkins R, Tunkel AR, Nelson EA, Henderson D, Shelgikar AV, Santen SA. 2020. A responsible educational handover: improving communication to improve learning. Acad Med. 95(2):194–199.
- Patton MQ. 2002. Qualitative research and evaluation methods. Vol. 4. Thousand Oaks (CA): Sage Publications.
- Pearlman RE, Pawelczak M, Yacht AC, Akbar S, Farina GA. 2017. Program director perceptions of proficiency in the core entrustable professional activities. J Grad Med Educ. 9(5):588–592.
- Pereira AG, Harrell HE, Weissman A, Smith CD, Dupras D, Kane GC. 2016. Important skills for internship and the fourth-year medical school courses to acquire them: a national survey of internal medicine residents. Acad Med. 91(6):821–826.
- Ruskin J, Bilous RH. 2020. A tripartite framework for extending university-student co-creation to include workplace partners in the work-integrated learning context. High Educ Res Dev. 39(4):806–820.
- Schlossberg NK, Goodman J. 2005. Counseling adults in transition. New York: Springer Publishing Company.
- Scott KW, Callahan DG, Chen JJ, Lynn MH, Cote DJ, Morenz A, Fisher J, Antoine VL, Lemoine ER, Bakshi SK, et al. 2019. Fostering student–faculty partnerships for continuous curricular improvement in undergraduate medical education. Acad Med. 94(7):996–1001.
- Simpson D, Marcdante K, Souza KH. 2019. The power of peers: faculty development for medical educators of the future. J Grad Med Educ. 11(5):509–512.
- Stalmeijer RE, McNaughton N, Van Mook WN. 2014. Using focus groups in medical education research: AMEE Guide No. 91. Med Teach. 36(11):923–939.
- Steiner-Hofbauer V, Holzinger A. 2020. How to cope with the challenges of medical education? Stress, depression, and coping in undergraduate medical students. Acad Psychiatry. 44(4):380–387.
- van den Broek S, Querido S, Wijnen-Meijer M, van Dijk M, Ten Cate O. 2020. Social identification with the medical profession in the transition from student to practitioner. Teach Learn Med. 32(3):271–281.
- White CB. 2007. Smoothing out transitions: how pedagogy influences medical students’ achievement of self-regulated learning goals. Adv Health Sci Educ Theory Pract. 12(3):279–297.
- Wolf SJ, Lockspeiser TM, Gong J, Guiton G. 2014. Students’ perspectives on the fourth year of medical school: a mixed-methods analysis. Acad Med. 89(4):602–607.
- Woods NN, Mylopoulos M, Brydges R. 2011. Informal self-regulated learning on a surgical rotation: uncovering student experiences in context. Adv Health Sci Educ Theory Pract. 16(5):643–653.
- Young MA, Stiens SA, Hsu P. 1996. Chief residency in PM&R: a balance of education and administration. Am J Phys Med Rehabil. 75(4):257–262.