?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
The doctors of the future need to be empowered to deliver healthcare sustainably while protecting their patients’ health in the context of a degrading environment. This study aimed to objectively review the extent and nature of the teaching of planetary health and sustainability topics in UK medical education.
Methods
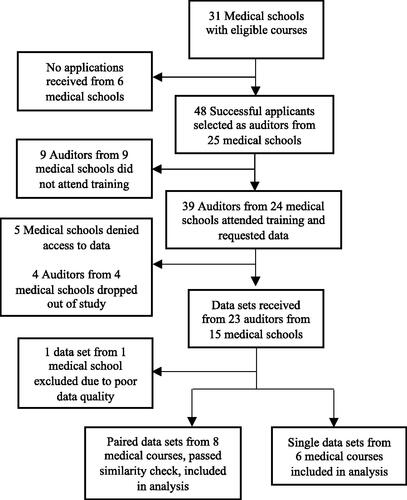
A multi-centre national review of the timetabled teaching sessions in medical courses in the UK during the academic year 2020/2021 against the General Medical Council’s adopted ‘Educating for Sustainable Healthcare – Priority Learning Outcomes’. Medical students were recruited and reviewed the entirety of their own institution’s online teaching materials associated with core teaching sessions using a standardised data collection tool. Learning outcome coverage and estimated teaching time were calculated and used to rank participating medical schools.
Results
45% of eligible UK medical schools were included in the study. The extent of teaching varied considerably amongst courses. Mean coverage of the 13 learning outcomes was 9.9 (SD:2.5) with a mean estimated teaching time of 140 min (SD:139). Courses with dedicated planetary health and sustainability sessions ranked best.
Conclusion
There is large disparity in the education that medical students receive on these topics. Teaching may not adequately prioritise sustainability or reflect advances in planetary health knowledge.
Practice points
Medical education on planetary health and sustainability topics varies widely amongst UK medical schools.
UK medical education does not necessarily reflect recent advances in planetary health knowledge.
Greater educational focus is required on sustainability in healthcare.
Centrally mandated teaching on these topics may improve disparity in education.
This study’s methodology provides a possible approach for future curriculum evaluations.
Introduction
Medical educators need to prepare doctors for the challenges they and their patients will face in the coming decades. One major challenge is anthropogenic environmental change (Romanello et al. Citation2021).
Environmental change and degradation threaten to destabilise the fabric of society upon which our health is so reliant, from global politics to cellular structures. Climate change is one of the greatest threats (WHO Citation2022). Future generations will suffer excess mortality and morbidity through extreme weather events (Ebi et al. Citation2021; Weilnhammer et al. Citation2021), changing vector ecology (Caminade et al. Citation2019), mass migration (Clement et al. Citation2021), drought and famine (Pokhrel et al. Citation2021). Global biodiversity loss, through soil degradation, urbanisation and deforestation, will threaten food security (FAO Citation2019), increase the incidence of zoonotic disease (Keesing and Ostfeld Citation2021) and may even alter the human microbiome (Cardinale Citation2012; Mills et al. Citation2019; Roe Citation2019). Pollution already cuts global life expectancy by an estimated 3 years (Lelieveld et al. Citation2020; Fuller et al. Citation2022). And resource depletion and a harsher global climate will make it harder for health systems to tackle these forthcoming challenges.
In this context, it is paradoxical that the healthcare industry is a major contributor to environmental degradation. In the UK it accounts for around 4–5% of emissions, close to that of aviation or shipping (Pichler et al. Citation2019; Lenzen et al. Citation2020). While the NHS’s commitment to Net Zero poses movement in the right direction there is much work still to do and will require systemic organisational change from students to executives (NHS England and NHS Improvement 2020).
As well as embracing sustainability, clinicians need to be empowered to protect their patients’ health in this changing environment. They need to understand and manage the direct and indirect impacts of environmental change on patients’ health. The recent publication and Medical School Council endorsement of the comprehensive guidance document ‘Education for sustainable healthcare – A curriculum for the UK’ is a significant step towards embedding these topics into UK medical curricula (Tun and Martin, Citation2022). However, to date there is no mandated coverage of these topics and there have been no comprehensive reviews of current UK teaching practices.
In 2013 the term planetary health was coined and later launched as a concept and science by the Rockefeller Foundation and the Lancet. Planetary health is defined as ‘the health of human civilisation and the state of the natural systems on which it depends’ (Whitmee et al. Citation2015). In recent years the concept has gained momentum in academic and medical circles.
In 2019 the Planetary Health Report Card (PHRC), a student-led initiative was launched. It measures universities’ performance across a variety of planetary health metrics, including medical curricula (Hampshire et al. Citation2022). The PHRC has gained much traction and has helped raise the profile of planetary health in medical education.
Given the complexity of analysing and comparing different medical school curricula, there is an opportunity for the utilisation of an alternative robust methodology to audit medical schools’ inclusion of planetary health and sustainability topics. This could offer an additional perspective to the PHRC, facilitate a detailed analysis of current teaching and further establish a baseline against which future progress can be measured.
A promising methodology for objectively auditing full medical curricula was developed for the Global Health Education in UK Medical Schools (GHEMS) study (Bandyopadhyay et al. Citation2019; Incision UK Citation2020). This involved employing medical students to act as auditors to independently review the entirety of their medical school’s teaching materials against a set of learning outcomes, using a strict data collection tool. This approach allows for the collection of highly detailed data and good accuracy; students are well placed to navigate and understand their respective curricula. Students, too, benefit from involvement in research (Jacobs and Cross Citation1995; Boyle et al. Citation2017).
To utilise the GHEMS methodology, an appropriate set of learning outcomes is required. In the last decade, several sets of learning outcomes have been proposed to help guide the teaching of planetary health and sustainability topics (Maxwell and Blashki Citation2016; GCCHE Citation2020; Guzmán et al. Citation2021; IMECCS 2021; Shaw et al. Citation2021; Hampshire et al. Citation2022). In the UK, medical teaching must meet the learning outcomes set out by the General Medical Council’s (GMC) Outcomes for Graduates (GMC Citation2018). In 2014, in response to a request from the GMC, the Centre for Sustainable Healthcare published ‘Educating for Sustainable Healthcare – Priority Learning Outcomes’ (Thompson et al. Citation2014; Centre for Sustainable Healthcare Citation2014). These are referenced as further reading in the GMC's Outcomes for graduates, see Supplementary Table 1. At the point of initiating this study these were the only planetary health relevant learning outcomes referenced by the GMC and therefore represented the closest option to a gold standard for UK medical education.
Study objectives
The primary objective of this study was to assess the extent and nature of the teaching of planetary health and sustainability topics in the core curricula of UK medical schools.
The secondary objectives were:
To identify a method for use as a future tool for auditing planetary health and sustainability teaching in medical schools.
To set a baseline performance of planetary health and sustainability teaching against which to benchmark future progress.
To provide feedback to individual medical schools to identify potential improvements that could be made to their curriculum.
Methods
The study design was adapted from the GHEMs study protocol (Bandyopadhyay Citation2019). The primary difference was the addition of estimated teaching time and the use of ‘Educating for Sustainable Healthcare – Priority Learning Outcomes’. The study design was reviewed by an international panel of environmental health and public health educators to ensure a robust methodology. The methodology was further refined by a 2019 pilot study of 3 medical schools (Imperial College, University of Bristol and University of Southampton), feedback from which was incorporated into the design. The principal change following the pilot was the exclusion of elective or student selected units from the study. As these units were non-mandatory for all students, it was not possible to accurately identify the proportion of students attending such teaching sessions. In addition, data collection during the pilot was considered too labour intensive by the pilot student auditors. The study was therefore designed to only capture core teaching, thereby reflecting all students’ experience rather than those selecting specific units or modules. Student auditors from the pilot were invited to help design and facilitate the subsequent study.
All UK GMC-registered medical schools which had taught a complete course by the end of the academic year 2021 were eligible for participation. Only undergraduate courses were included in the analysis due to insufficient data for graduate courses. The word ‘course’ is used here on to describe undergraduate medical courses, rather than the term ‘school’ which refers to the medical institution which potentially provide either or both undergraduate and graduate courses.
Data collection
Data collection was undertaken by ‘auditors’, drawn from students from any year of eligible medical schools. Recruitment was conducted through student groups, social media sites and direct communication with medical schools. Students were invited to send in applications that were reviewed by the research team. The aim was to recruit two medical students from each eligible medical school in the UK to act as auditors.
Successful applicants were required to attend a two-part online teaching session lasting 90 min. The first part provided a ‘climate, sustainability and health crash course’, covering topics relevant to each learning outcome. The second part provided training on the use of the study’s excel-based data collection tool, attached as Supplementary Materials, and how to obtain permissions from universities and access to online learning materials. Auditors were also provided with a flow chart and timetable for data collection.
Auditors requested a full timetable of all core (not student-selected) teaching sessions and associated online materials for all years of study in the academic year 2020/2021 from their own medical school. Once access was obtained, auditors independently assessed all their medical courses’ teaching sessions against the sub-learning outcomes (SLOs), see Supplementary Table 1, using the data collection tool. The research team was available for support, whilst remaining independent of the auditing process itself.
Assessing the extent of sub-learning outcome teaching
Teaching for each SLO was quantified in two ways: coverage of SLOs and estimated teaching time (ETT). Universities were anonymously ranked based on total learning outcome coverage and ETT.
Coverage was defined as a medical course providing any teaching relevant to that SLO. No attempt was made to qualify the depth of coverage as this was considered too complex and subject to bias.
ETT was calculated as the estimated time spent on teaching an SLO within a particular teaching session. For example, in a lecture lasting 60 min with 100 slides and 2 slides relevant to an SLO, it was deemed that 1.2 min was spent on this SLO. If more than one SLO was covered in these slides the estimated time was divided equally amongst each SLO covered. Estimating teaching time allowed for greater granularity of analysis beyond that of binary coverage data.
SLOs associated with LO1 were anticipated to have the most comprehensive teaching as such auditors were asked to specify exact topics covered in teaching sessions to allow for more detailed analysis.
Data cleaning and verification
Auditors submitted data sets independently to the central research team. Each data point was individually checked by one member of the research team to confirm it matched the description of the learning event provided by the auditor. In cases of ambiguity, the auditor was contacted for clarification. For courses where there were two data sets provided, these were manually merged to ensure no double counting. Auditor descriptions of teaching events were also used to establish if the medical course had dedicated core sustainability or planetary health teaching sessions.
Presenting back to faculties
Auditors were given individualised presentation packs to deliver to their faculty. Information within these presentations included individual course rankings, detailed analyses of SLO coverage and ETT compared to the participating course average. These packs also highlighted opportunities for improvement and provided references to useful resources.
Results
Learning outcome data was collected for 45% (14/31) of eligible medical schools, see . ETT data was available for 13/14 of participating courses and as such, ETT analysis only refers to these courses.
The teaching of learning outcomes
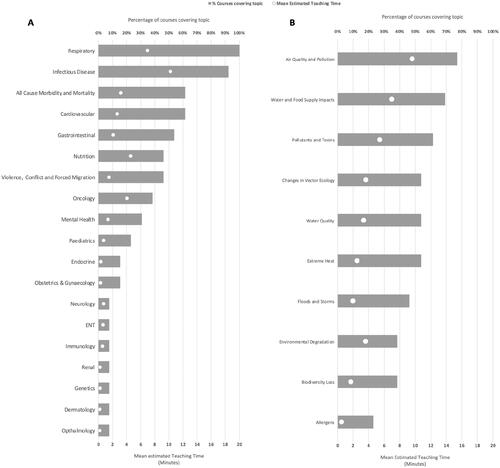
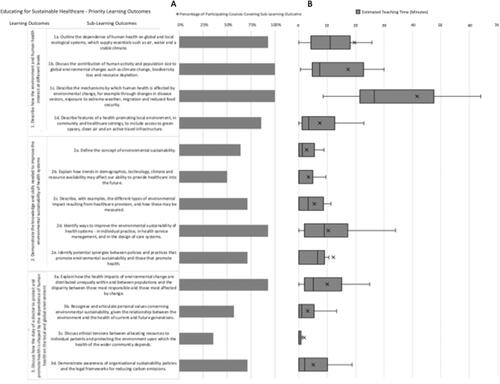
Amongst participating medical courses there was mean coverage of 9.9 (SD:2.5) and median of 10 (IQR:8.5–12) of the 13 SLOs. 35% of courses covered fewer than 10 SLOs. Only one medical course covered all 13 SLOs. The mean ETT on all topics related to SLOs was 140 (SD:139) min with a median of 100 (IQR:74–149) min with a range of 35–566 min. ETT and mean coverage varied considerably amongst SLOs, see .
Figure 2. (A) Overall coverage of Sub-Learning Outcomes (SLO)s amongst participating courses. Coverage data available for 14 courses. (B) Estimated teaching time per SLO, the box indicates 2nd to 3rd quartiles, whiskers indicate 1st and 4th quartiles, median indicated by the line across the box, x indicates mean, statistical outliers excluded from the analysis. Estimated teaching time data available for 13 courses.
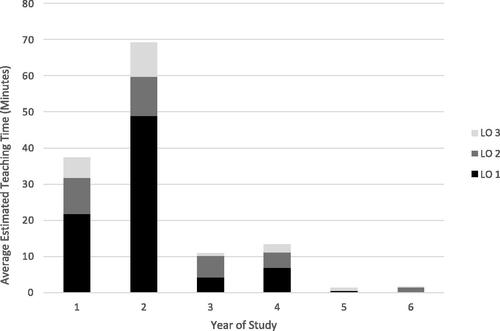
Most of the ETT of the SLOs was spent in the traditional preclinical years 1 and 2 of study. In these years, teaching on LO1 constitutes 66% percent of total SLO ETT. Proportionally, ETT of LO2 and 3 increase in the later years of study, see . Overall, 84% of total ETT on these topics was through lectures and 13% through smaller group sessions.
Learning outcome 1 analysis
LO 1 had the best coverage, with all universities covering at least 3 of the associated SLOs with a mean coverage of 95% (SD:8%) and median of 100%. Mean ETT for associated SLOs was 86 (SD:99) min with a median of 55 (IQR43:73) min.
Detailed analysis of SLO 1c showed that the most taught environmental mechanism by which human health is affected by environmental change was ‘air quality and pollution,’ see . ETT on this mechanism related mostly to respiratory health (66%), oncology (16%) and cardiovascular health (8%). See Supplementary Table 2. The least discussed environmental mechanisms were biodiversity loss and allergens, see .
Learning outcomes 2 and 3 analysis
SLOs associated with LO2 and LO3 had a mean coverage of 70% (SD:27%) and 64% (SD:26%), respectively. Mean ETT for associated SLOs were 34 (SD:29) min and 20 (SD:19) min, respectively. One university did not cover any SLOs associated with LO3.
Ranking of medical courses
Universities were ranked according to the total coverage of learning outcomes, then by ETT, see .
Figure 5. Courses were ranked in terms of total estimated teaching time and total sub-learning outcome coverage. (1 is the highest rank), they were placed into three categories: Courses with both dedicated planetary health and sustainability teaching sessions; courses with either dedicated planetary health (PH) or sustainability (Sust) teaching sessions; courses with no dedicated planetary health or sustainability teaching sessions.
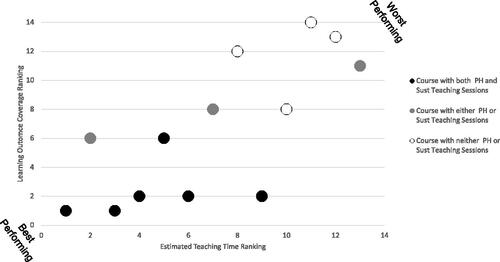
50% of courses had dedicated sustainability teaching sessions and 57% had sessions on planetary health. Overall, the courses which covered the most SLOs and had the most ETT were those which had both dedicated planetary health and/or sustainability teaching sessions as well as topics interweaved throughout the rest of the course. Those that performed worst had no dedicated sessions, with teaching mainly focusing on traditional environmental and occupational health topics with little reference to climate and sustainability throughout the course.
Discussion
This study attempted to objectively quantify the level of planetary health and sustainability relevant teaching at UK medical schools. Among the 14 participating medical courses there was widely varying coverage and ETT of SLOs. The results are important for both participating and non-participating medical schools, education leads and policymakers.
Disparity of extent and nature of teaching
The results of this study the support those found by the PHRC by demonstrating a wide disparity in medical education on planetary health and sustainability issues (Hampshire et al. Citation2022). In particular, the depth of coverage of these topics, measured as ETT, varies considerably: from only 35 min up to 9 h. Medical courses which ranked highest in our analysis appeared to have prioritised planetary health and sustainability with dedicated sessions on these topics, while those that ranked lowest offered little teaching beyond that of basic environmental and occupational health topics. This suggests that medical students in the UK will exit medical school with vastly different knowledge bases and may leave some with outdated impressions of the importance of specific topics. This issue is likely not limited to the UK, with an international survey of medical students finding that only 11% of almost 3000 medical schools globally provided any formal planetary health education (Omrani et al. Citation2020).
The field of planetary health has fostered a new appreciation of the complex interactions between the health of the planet and that of the human population. This complexity is not yet reflected in many medical curricula. For instance, one of the most discussed mechanisms by which environmental change affects human health was ‘pollution.’ Within this mechanism, our analysis showed that teaching focused mostly on respiratory health rather than cardiovascular health. The literature, however, suggests that pollution contributes to similar or more cardiovascular mortality than respiratory (Lelieveld et al. Citation2020; Rodopoulou et al. Citation2022). The impact of climate change and pollution on other health conditions such as chronic kidney disease also appears neglected (Tsai et al. Citation2021). In addition, the poor coverage of biodiversity in teaching is concerning given its clinical relevance to zoonotic disease (especially in the context of COVID-19) (Schmeller et al. Citation2020; Lawler Citation2021; Platto Citation2021), inflammatory and atopic disease (Haahtela Citation2019, Prescott et al. Citation2018).
In addition to understanding the risk that environmental degradation poses to health it is also important thatstudents are empowered to reduce their environmental impact as future health professionals. Yet these topics remain under-represented in medical curricula. ETT on sustainability related SLOs was much less than that on more environmental risk related SLOs and only half of the courses had dedicated teaching sessions on sustainability.
Given these findings, it appears the UK medical school system is not appropriately preparing many students for the challenges that environmental degradation poses to human health, to deliver healthcare sustainably, or to deliver a Net Zero NHS.
Enhancing the teaching of planetary health and sustainability topics
Multiple approaches to improving coverage of these topics have been proposed, from whole modules to more gentle ‘infusion’ approaches (Tun et al. Citation2020; Bevan and Roderick Citation2021; Kligler et al. Citation2021; Slimings et al. Citation2022). Although, there is no consensus yet as to which approach is best, this study suggests that a two-pronged approach of dedicated lectures with material interspersed throughout the course appears most effective in terms of achieving good coverage of LOs. However, this does not necessarily equate to better educational outcomes for students - particularly as most curricula are densely packed with little room for extra teaching. Further work is required to understand the most efficient approach for both students and educators to improve knowledge and values.
Interestingly, teaching time on planetary health and sustainability topics in medical school did not necessarily correlate with coverage of the listed learning outcomes. This suggests that course directors are not prioritising the coverage of the LOs used in this study. One reason for this could be that these LOs are only listed as ‘further reading’ by the GMC learning outcomes for graduates. Within the core GMC Learning outcomes for graduates there is only one mention of sustainability and no mention of planetary health. Even with the welcome addition of the Medical School Council endorsed ‘Education for sustainable healthcare – A curriculum for the UK’ (Tun and Martin Citation2022), this is still only listed as further reading by the GMC. For systemic change, such guidance would need to be central to the GMC’s outcomes for graduates.
As planetary health is a new science, there is limited educator confidence and knowledge (Wellbery et al. Citation2018; Shea et al. Citation2020; Goldman et al. Citation2021). Equally, sustainability in healthcare has historically not received much attention in medical education. It is therefore perhaps unsurprising that there is a considerable range in the coverage of the learning outcomes shown by this study. Without a concerted effort by experienced and interested medical faculties to overcome this, such topics are unlikely to appear in the curriculum at individual institutions. As such, there is a need for educator support and training on these topics. Collaborative interuniversity approaches appear to be an effective method for improving educator confidence and capacity on the teaching of these topics so may represent a promising way to improve coverage of these topics in curricula (Walpole and Mortimer Citation2017).
It appears that planetary health and sustainability topics are most extensively covered in the early years of medical education. There is an opportunity for medical courses to change the timing of the teaching of these topics to reflect the student journey. In the early years of medical school students when students learn about pathology and epidemiology, the introduction of planetary health themes in these early years would complement existing teaching. As students enter clinical practice a greater emphasis could be placed on sustainability in healthcare, to reinforce its importance as students gain more clinical exposure and make the transition from student to doctor.
Strengths and limitation of methodology
This study adapted the GHEMS study’s methodology for assessing curricula by including ETT. This study has several limitations. Using ETT as a surrogate marker for the extent of teaching will carry a degree of inaccuracy, as it is not possible to calculate exactly how much time educators spent teaching SLOs during individual teaching sessions, this is especially true in courses with a greater focus on problem-based or peer-to-peer learning. The addition of ETT however allows for a quantifiable representation of the depth of teaching of learning outcomes beyond that of the binary coverage and enables granular analysis of specific topics taught.
A further limitation with evaluating curricula in this way is auditor subjectivity. We attempted to reduce subjectivity as much as possible with auditors reviewing all course teaching materials using a rigid data collection tool, a standardised teaching session, materials to guide auditors, constantly available support from the research team and having data collected by two auditors independently (where possible). However, this risk could not be entirely negated, and some minor auditor subjectivity was likely present.
Only a relatively small number of medical courses were included, limiting the generalisability of the findings and ability to set a meaningful baseline. Future studies employing this methodology would benefit from starting auditor recruitment early and recruiting both graduate and undergraduate students from medical schools. The results, however, still provide valuable insight into the likely variance of the teaching of these topics across UK medical schools.
Data collection was restricted by the possible limited release of online teaching materials by medical schools. The data does not capture sessions that were not timetabled, where materials were not available online or instances of free-flowing discussions. This may also partially account for the higher ETT in the early years of medical courses, where teaching is more formalised and curriculum-driven, rather than the more ad-hoc clinical teaching in later years and which would require a different methodology to capture. On balance, however, as medical schools tend to make most core teaching session materials available online to students, the data is expected to closely reflect the true coverage of the learning outcomes.
The exclusion of student selected or elective units means that there will likely be some underrepresentation of the total level of learning outcome coverage amongst medical courses. However, the focus on core teaching means that the results reflect the baseline teaching that all the medical students at participating courses receive as part of their central education. Additionally, in order to drive systemic change, it may be of more importance to educate those students who would not voluntarily select units which cover planetary health and sustainability.
Overall, this study demonstrated that the GHEMS methodology is a replicable methodology for evaluating medical school curricula against a set of defined learning outcomes. Involvement in research also infers benefits to the auditors and provides participating courses with a free in-depth analysis of their course with opportunities for improvement highlighted. This methodology, therefore, provides a widely beneficial approach to assessing curricula and could be used for future curriculum assessments in the field of planetary health and sustainability. Future work could also include auditor views on involvement and follow-up of participating courses to assess if actions were made on the basis of audit findings.
Conclusion
Current medical education varies widely in the teaching of planetary health and sustainability topics. When these topics are taught at medical school, the teaching may not concentrate on the most important areas according to planetary health research. Given the NHS’s net zero commitment a more concerted effort to teach sustainable healthcare is required. This study suggests that central guidance and mandated learning outcomes would help ensure students receive adequate education on these matters. The study presents a possible methodology through which medical school curricula could be objectively audited in the future.
Ethical approval
Ethics was sought from the University of Southampton ethics committee. It was however deemed that ethics approval was not required.
Glossary
Planetary Health: ‘The achievement of the highest attainable standard of health, wellbeing, and equity worldwide through judicious attention to the human systems—political, economic, and social—that shape the future of humanity and the Earth’s natural systems that define the safe environmental limits within which humanity can flourish. Put simply, planetary health is the health of human civilisation and the state of the natural systems on which it depends.’
Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, Ezeh A, Frumkin H, Gong P, Head P, et al. 2015. Safeguarding human health in the Anthropocene epoch: report of the Rockefeller Foundation–Lancet Commission on planetary health. The Lancet. 386(10007):1973–2028.
Supplemental Material
Download Zip (40.4 KB)Acknowledgements
Professor Paul Roderick (University of Southampton).
Disclosure statement
The authors report there are no competing interests to declare.
Additional information
Notes on contributors
James Bevan
Dr James Bevan, BMBS, BSc, previously a corporate sustainability consultant, James completed academic foundation training at University Hospital Southampton in August 2022. He has worked with organisations such as Harvard TH Chan School of Public Health, Icahn School of Medicine at Mount Sinai and Public Health England on climate and sustainability matters. He is the international lead for the International Medical Education Collaboration on Climate and Sustainability and is the first planetary health education fellow at the University of Southampton. He is currently studying for an MSc in Tropical Medicine and International Health at the London School of Tropical Medicine.
Rachel Blyth
Dr Rachel Blyth, BMBS, BSc, is currently a foundation year 2 doctor at St. George’s hospital London and about to commence internal medical training at Chelsea and Westminster hospital. She is a budding dermatologist with an interest in medical education. She has a 1st class degree in Neuroscience from King’s College London and completed her medical degree at the University of Southampton.
Benjamin Russell
Dr Benjamin Russell, BMBS, BSc, qualified in 2020 from Southampton Medical School and started his medical career as a doctor at St Mary’s and West Middlesex hospitals in London. He is a GP trainee in London.
Lydia Holtgrewe
Lydia Holtgrewe is a 4th year medical student at the University of Southampton, and a 2nd year MPH student at Yale School of Public Health. Her current degree work is centred around the epidemiology of microbial diseases with a focus on Tuberculosis. Her other research interests include oncology and regulatory affairs for pharmaceutical products. As European Coordinator at Universities Allied for Essential Medicines she is promoting equitable access to medicines at European universities and worldwide.
Annie Hoi Ching Cheung
Annie Hoi Ching Cheung is a 5th year medical student at Imperial College London, where she has also recently graduated with an intercalated degree in Biomedical Engineering. She is particularly interested in sustainability, humanitarian aid, and paediatrics.
Isobel Austin
Isobel Austin, BMBS, BSc, is a University of Southampton graduate starting as an FY1 in 2022. She has a BSc in Environmental Science and a particular interest in the impact of environmental degradation on human health.
Viraj Shah
Viraj Shah has completed his first three years of medical school at Imperial College London and is currently intercalating in Healthcare Management. His interests lie within surgery, healthcare innovation & improvement and global health. He is passionate about both research and medical education and looks forward to marrying the two in his future career.
Megan Butler
Megan Butler is a 3rd medical student at the University of Bristol. She has current research interests in Medical Education, Cardiology and Orthopaedics and clinically is interested in dermatology.
Simon Fraser
Dr Simon Fraser, BM, MSc, DM, FFPH, MRCGP, FHEA, DRCOG, DCH, is an associate professor of public health at the University of Southampton, previously a GP but retrained in public health. He has research interests in long term conditions and health inequalities. He leads teaching on health service organisation and evaluation in the Southampton MSc in Public Health and is evidence-based medicine lead for the Southampton graduate medicine programme (BM4).
References
- Bandyopadhyay S, Shortland T, Wadanamby S, Thomas H, Gurung B, Akhbari M, Trout I, Patel R, Sharma K, Fitzgerald J, et al. 2019. Global Health Education in UK Medical Schools (GHEMS) study protocol. J Global Health Rep. 3:e2019052.
- Bevan J, Roderick P. 2021. Infusing climate change and sustainability into the medical school curriculum. BMJ Opinion. [accessed 2022 Jun 1]. https://blogs.bmj.com/bmj/2021/06/07/infusing-climate-change-and-sustainability-into-the-medical-school-curriculum/.
- Boyle S, Cotton S, Myint P, Hold G. 2017. The influence of early research experience in medical school on the decision to intercalate and future career in clinical academia: a questionnaire study. BMC Med Educ. 17(1):245.
- Caminade C, McIntyre K, Jones A. 2019. Impact of recent and future climate change on vector-borne diseases. Ann N Y Acad Sci. 1436(1):157–173.
- Cardinale B, Duffy J, Gonzalez A, Hooper D, Perrings C, Venail P, Narwani A, Mace G, Tilman D, Wardle D, et al. 2012. Biodiversity loss and its impact on humanity. Nature. 486(7401):59–67.
- Centre for Sustainable Healthcare. 2014. Educating for sustainable healthcare – expanded learning outcomes. [accessed 2022 Jun 1]. https://sustainablehealthcare.org.uk/educating-sustainable-healthcare-expanded-learning-outcomes.
- Clement V, Kanta K, de Sherbinin A, Jones B, Adamo S, Schewe J, Sadiq N, Shabahat E. 2022. Groundswell part 2 : acting on internal climate migration. Washington: World Bank.
- Ebi K, Vanos J, Baldwin J, Bell J, Hondula D, Errett N, Hayes K, Reid C, Saha S, Spector J, et al. 2021. Extreme weather and climate change: population health and health system implications. Annu Rev Public Health. 42:293–315.
- FAO. 2019. The state of the world’s biodiversity for food and agriculture. Rome. Food and Agriculture Organisation.
- Fuller R, Landrigan P, Balakrishnan K, Bathan G, Bose-O'Reilly S, Brauer M, Caravanos J, Chiles T, Cohen A, Corra L, et al. 2022. Pollution and health: a progress update. The Lancet Planetary Health. 6(6):e535–e547.
- General Medical Council. 2018. Outcomes for graduates 2018. London, UK: General Medical Council.
- Global Consortium on Climate and Health Education (GCCHE). 2020. Climate & health key competencies for health professions students. GCCHE. https://www.publichealth.columbia.edu/research/global-consortium-climate-and-health-education/core-competencies-0.
- Goldman R, Zajac L, Geller R, Miller M. 2021. Developing and implementing core competencies in children’s environmental health for students, trainees and healthcare providers: a narrative review. BMC Med Educ. 21;503.
- Guzmán C, Aguirre A, Astle B, Barros E, Bayles B, Chimbari M, El-Abbadi N, Evert J, Hackett F, Howard C, et al. 2021. A framework to guide planetary health education. Lancet Planetary Health. 5(5):e253–e255.
- Haahtela T. 2019. A biodiversity hypothesis. Allergy. 74(8):1445–1456.
- Hampshire K, Islam N, Kissel B, Chase H, Gundling K. 2022. The Planetary Health Report Card: a student-led initiative to inspire planetary health in medical schools. Lancet Planetary Health. 6(5):e449–e454.
- IMECCS. 2022. Materials and Resource Bank [Internet]. [accessed 2022 Jun 1]. https://www.imeccs.org/.
- Incision UK. 2020. Global health education in medical schools (GHEMS): a national, collaborative study of medical curricula. BMC Med Educ. 20:44.
- Jacobs C, Cross P. 1995. The value of medical student research: the experience at Stanford University School of Medicine. Med Educ. 29(5):342–346.
- Keesing F, Ostfeld R. 2021. Impacts of biodiversity and biodiversity loss on zoonotic diseases. Proc Natl Acad Sci USA. 118(17):e2023540118.
- Kligler S, Clark L, Cayon C, Prescott N, Gregory J, Sheffield P. 2021. Climate change curriculum infusion project: an educational initiative at one U.S. medical school. J Climate Change Health. 4:100065.
- Lawler OK, Allan HL, Baxter PWJ, Castagnino R, Tor MC, Dann LE, Hungerford J, Karmacharya D, Lloyd TJ, López-Jara MJ, et al. 2021. The COVID-19 pandemic is intricately linked to biodiversity loss and ecosystem health. Lancet Planet Health. 5(11):e840–e850.
- Lelieveld J, Pozzer A, Pöschl U, Fnais M, Haines A, Münzel T. 2020. Loss of life expectancy from air pollution compared to other risk factors: a worldwide perspective. Cardiovasc Res. 116(11):1910–1917.
- Lenzen M, Malik A, Li M, Fry J, Weisz H, Pichler P, Chaves L, Capon A, Pencheon D. 2020. The environmental footprint of health care: a global assessment. Lancet Planet Health. 4(7):e271–e279.
- Maxwell J, Blashki G. 2016. Teaching about climate change in medical education: an opportunity. J Public Health Res. 5(1):673. jphr.2016.673.
- Mills J, Brookes J, Gellie N, Liddicoat C, Lowe A, Sydnor H, Thomas T, Weinstein P, Weyrich L, Breed M. 2019. Relating urban biodiversity to human health with the ‘Holobiont’ concept. Front Microbiol. 10:550.
- NHS England and NHS Improvement. 2022. Delivering a ‘net zero’ national health service. London: NHS England and NHS Improvement.
- Omrani O, Dafallah A, Paniello Castillo B, Amaro B, Taneja S, Amzil M, Sajib M, Ezzine T. 2020. Envisioning planetary health in every medical curriculum: an international medical student organization’s perspective. Med Teach. 42(10):1107–1111.
- Pichler P, Jaccard I, Weisz U, Weisz H. 2019. International comparison of health care carbon footprints. Environ Res Lett. 14(6):064004.
- Platto S, Zhou J, Wang Y, Wang H, Carafoli E. 2021. Biodiversity loss and COVID-19 pandemic: the role of bats in the origin and the spreading of the disease. Biochem Biophys Res Commun. 538:2–13.
- Pokhrel Y, Felfelani F, Satoh Y, Boulange J, Burek P, Gädeke A, Gerten D, Gosling S, Grillakis M, Gudmundsson L, et al. 2021. Global terrestrial water storage and drought severity under climate change. Nat Clim Chang. 11(3):226–233.
- Prescott S, Wegienka G, Logan A, Katz D. 2018. Dysbiotic drift and biopsychosocial medicine: how the microbiome links personal, public and planetary health. Biopsychosoc Med. 12:7.
- Rodopoulou S, Stafoggia M, Samoli E, Bauwelinck M, Vienneau D, Oftedal B, Andersen Z, Janssen N, Katsouyanni K, Brunekreef B, et al. 2022. Long-term exposure to ambient particulate matter components and mortality: results from six European administrative cohorts within the ELAPSE project. Sci Total Environ. 25(809):152205.
- Roe D. 2019. Biodiversity loss—more than an environmental emergency. Lancet Planet Health. 3(7):e287–e289.
- Romanello M, McGushin A, Di Napoli C, Drummond P, Hughes N, Jamart L, Kennard H, Lampard P, Solano Rodriguez B, Arnell N, et al. 2021. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 398(10311):1619–1662.
- Schmeller D, Courchamp F, Killeen G. 2020. Biodiversity loss, emerging pathogens and human health risks. Biodivers Conserv. 29(11–12):3095–3102.
- Shaw E, Walpole S, McLean M, Alvarez-Nieto C, Barna S, Bazin K, Behrens G, Chase H, Duane B, El Omrani O, et al. 2021. AMEE Consensus Statement: planetary health and education for sustainable healthcare. Med Teach. 43(3):272–286.
- Shea B, Knowlton K, Shaman J. 2020. Assessment of climate-health curricula at international health professions schools. JAMA Netw Open. 3(5):e206609.
- Slimings C, Sisson E, Larson C, Bowles D, Hussain R. 2022. Adaptive doctors in Australia: preparing tomorrow’s doctors for practice in a world destabilised by declining planetary health. Environ Educ Res. 28(5):786–801.
- Thompson T, Walpole S, Braithwaite I, Inman A, Barna S, Mortimer F. 2014. Learning objectives for sustainable health care. Lancet. 384(9958):1924–1925.
- Tsai H, Wu P, Huang J, Chen S. 2021. Environmental pollution and chronic kidney disease. Int J Med Sci. 18(5):1121–1129.
- Tun S, Wellbery C, Teherani A. 2020. Faculty development and partnership with students to integrate sustainable healthcare into health professions education. Med Teach. 42(10):1112–1118.
- Tun S, Martin T. 2022. Education for sustainable healthcare – a curriculum for the UK. London, UK: Medical Schools Council.
- Walpole SC, Mortimer F. 2017. Evaluation of a collaborative project to develop sustainable healthcare education in eight UK medical schools. Public Health. 150:134–148.
- Weilnhammer V, Schmid J, Mittermeier I, Schreiber F, Jiang L, Pastuhovic V, Herr C, Heinze S. 2021. Extreme weather events in Europe and their health consequences – a systematic review. Int J Hyg Environ Health. 233:113688.
- Wellbery C, Sheffield P, Timmireddy K, Sarfaty M, Teherani A, Fallar R. 2018. It’s time for medical schools to introduce climate change into their curricula. Academic Medicine. 93:1774–1777.
- Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, Ezeh A, Frumkin H, Gong P, Head P, et al. 2015. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation–Lancet Commission on planetary health. Lancet. 386(10007):1973–2028.
- World Health Organisation. 2022. Climate change and health. Who.int. [accessed 2022 Jun 30]. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health.