?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
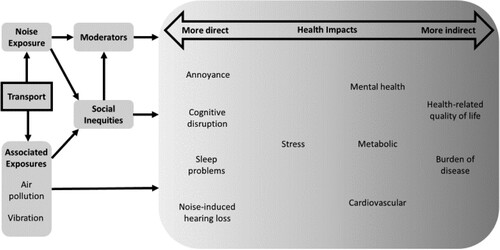
The relationship between transport noise and health outcomes is complex, in part because of the large number of factors involved as well as the range of health impacts, both direct and indirect. To enable the reader to come to grips with the complexity, we have divided the health outcomes into groups: those that are more directly linked to transport noise exposure and those that are more indirectly linked. Four health outcomes, namely annoyance, cognitive disruption, sleep problems, and noise-induced hearing loss, can be directly attributable to transport noise exposure. Less direct outcomes are stress, mental health, metabolic health, cardiovascular health, and overall health-related quality of life. Stress may occur as a direct response to noise, or may occur in response to the aforementioned direct effects. The stress response is a survival mechanism in the short term, but in the long term, stress may lead to systemic health conditions, namely metabolic and cardiovascular outcomes, and to mental health conditions. Finally, a global health outcome that incorporates all of the more direct outcomes is health-related quality of life. Other exposures associated with transport noise that may explain parts of the health outcomes need to be acknowledged, including exposure to social inequities, air pollution, and vibration. These may all be more likely to be experienced by people who are exposed to transport noise in the community and may thus influence the outcomes. Finally, transport noise appears to have more impact on health in those who are noise sensitive, thus noise sensitivity is a key moderator of all the effects observed.
1. Introduction
Transport is an important component of human society, integral to connectedness and economic prosperity. A by-product of transport is the creation of noise. The effects of noise on exposed communities range from direct psychophysiological responses to noise exposure (annoyance, cognitive disruption, sleep problems, and noise-induced hearing loss), to less direct effects such as mental health issues and physical health problems. The mechanisms are complex and involve interactions between the primary noise exposure and higher-level reactions; for example, stress can be a response to noise, but may also occur indirectly from reduced or poor sleep, or as a result of noise-induced hearing loss.
Several reviews have been published (e.g. Basner et al., Citation2014) including a set of eleven articles about the WHO European environmental noise guidelines (WHO Environmental noise guidelines for the European region, Citation2017). This article presents a more recent review and is intended for a wider audience based on a process model developed to elucidate the complex and interrelated nature of exposure to noise and impacts.
Noise exposure, including that from transport, does not occur in isolation from other factors influencing health. Those experiencing negative social inequities, such as poverty, poorer nutrition, or lower levels of education may be more likely to be living in places close to sources of transport noise; therefore, apparent health effects of noise may actually reflect the impact of social inequity. Furthermore, transport produces both air pollution and ground vibration which also impact health and well-being separately.
presents a process diagram of the health impacts of transport noise on which the structure of this paper is based, beginning with consideration of social inequities, air pollution, and vibration as concomitants of environmental exposure to transport noise. The moderating factors are then addressed, followed by discussion of the key health impacts starting with the more direct and then those that are more indirect.
For clarity, the review was structured around a process diagram (), and aimed to be accessible to readers with little prior background in the area. Space is therefore dedicated to explaining the underlying principles as well as describing research in each area. The literature review is narrative in style, and authors were assigned topics within their areas of expertise as well as contributing overall. The search and criteria were therefore subjective.
2. Associated exposures
Transport noise is likely to be associated with other exposures that impact health, including fumes from internal combustion engines, and vibration caused either directly by heavy vehicles, or indirectly, as a by-product of high-level noise.
2.1. Air pollution
Vehicles produce air pollution including carbon monoxide, hydrocarbons and nitrogen oxides as well as particulate matter, presenting a health risk when inhaled (World Health Organization, Citation2014). Findings of direct associations between road traffic noise level and air pollution are mixed. For example, a significant correlation was found between nitrogen dioxide as a surrogate for traffic air pollution and noise measured at fixed sites (Foraster et al., Citation2009), whereas little correlation was found between air pollution levels and noise from road traffic in mobile measures from cyclists (Gelb & Apparicio, Citation2021).
Since exposure to both noise and air pollution impact negatively on health, the two need to be disentangled. In this respect, two studies are of note. The first is a study involving school-aged children (Clark et al., Citation2012) in which it was found that air pollution did not moderate the relationship between road traffic noise exposure, and cognitive or mental health measures. The second was a study that measured both annoyance and HRQoL that found no interaction between air pollution annoyance and noise annoyance, implying that air pollution and noise impact health independently (Shepherd et al., Citation2016). This lack of research has led to appeals for further research (Tzivian et al., Citation2015).
2.2. Vibration
At a physical level, audible sound is an acoustic wave by which mechanical energy is propagated through the atmosphere. Acoustic waves can also produce sensations of vibration that are felt rather than heard. In the context of transportation noise, the majority of transport modes produce ground-borne (i.e. rail, road) or airborne (i.e. aviation) vibrations that may interact with audible noise to amplify health effects. For example, low frequency aircraft noise can displace structures and their contents, and produce greater annoyance responses in houses bereft of acoustic insulation (Fidell et al., Citation2002). Typically, vibration is not considered as a separate impact from noise, and more research is required to disentangle the effects of vibration and noise on annoyance (Anciaes et al., Citation2017) and other health outcomes.
In terms of the cohorts affected by vibration, research has largely focused upon its impact on transport users, such as passengers or vehicle controllers, while neglecting those passively exposed to transport vibration, such as those living in communities located close to noise sources. In the case of railway noise, in a laboratory-based study, Maigrot et al. (Citation2020) suggested that the presence of vibration does not amplify annoyance to noise, a finding replicated in a population health study on passenger trains (Maclachlan et al., Citation2018). However, this study did not consider freight trains. Ogren et al. (Citation2017) estimated that rail-related vibration velocities of 0.48 and 0.98 mm/s resulted in 20% and 40% annoyance responses, respectively. This is consistent with the findings of Woodcock et al. (Citation2016) suggesting that annoyance increases if the vibration-induced rattle is audible. Di et al. (Citation2019) reported that perceived vibration moderates the relationship between noise exposure and noise annoyance, more for trains than road traffic, because trains produce more vibration even at equal sound pressure levels (Yokoshima et al., Citation2021). Finally, vibration from freight trains is linked to sleep disturbance, which in turn may mediate the relationship between train noise and annoyance (Smith et al., Citation2016).
3. Social inequities
The relationships between transport noise and social inequities are complex. Transport noise (and associated air pollution and vibration) may tend to be experienced more by people who cannot afford to live away from major roads, railways, or airports, and have homes without sound insulation. Furthermore, social inequity is well known to be associated with health outcomes of many kinds (e.g. Marmot et al., Citation2012), so may be involved in the causal pathway between noise exposure and health outcomes.
Social inequity can have geographical, economic, social and cultural contexts, all of which are important variables in assessing the impacts of traffic noise exposure (Bocquier et al., Citation2012). However, evidence is mixed. Some studies have indicated that marginalised, disadvantaged and minority groups experience higher levels of traffic noise than those who live in affluent neighbourhoods (see Dreger et al., Citation2019 for a review) and are less likely to be protected by noise barriers (Audrin et al., Citation2022). Other studies suggest that the relationship between noise exposure from road traffic and annoyance is stronger in more affluent neighbourhoods and those with higher levels of education (Meline et al., Citation2013). This contrary view is supported by findings that people with higher socioeconomic status experienced higher noise levels than disadvantaged communities (Havard et al., Citation2011). This finding could be attributed to the Parisian context where affluent people could afford to live centrally, and disadvantaged are restricted to housing areas located on the outer boundaries of the city. However, when spatial autocorrection is accounted for, there is mixed evidence of unequal exposure to traffic noise according to equity (Verbeek, Citation2019). Thus, the issue is complex and likely to be highly context-specific.
4. Moderators of the impact of transport noise on health
Noise sensitivity and fear associated with the noise source have been identified as two key elements that predict annoyance with noise (Miedema & Vos, Citation1999). It has been suggested that noise sensitivity might be a marker of susceptibility to health conditions, or of a tendency to report them (Fyhri & Klaeboe, Citation2009), implying that noise may not be a necessary contributor to health outcomes. Other data have suggested that noise sensitivity as a trait is a better predictor of adverse health outcomes than noise exposure (Park et al., Citation2017). On the other hand, noise sensitivity was found not to relate to health in a non-noise-exposed group, whereas in a noise-exposed group, more noise-sensitive people experienced poorer health (Welch et al., Citation2013). This implies that noise sensitivity is indeed a moderator of the effect of road traffic noise, with the same effect shown in the case of exposure to aircraft noise (Welch et al., Citation2018). On the other hand, van Kamp et al. (Citation2004) suggest that noise and noise sensitivity are two independent predictors of annoyance, a theory which received support from Paunovic et al. (Citation2009).
The level of annoyance from a sound is predicted by economic benefit – with those who stand to benefit less annoyed than those who do not (Ouis, Citation2001). Moreover, noises that are out of place lead to more annoyance than noise sources that are expected (e.g. mechanical sounds in the countryside are more annoying than road traffic in the city). Thus, factors such as attitudes towards the noise source have a significant influence on a person’s reaction to noise (Crichton et al., Citation2015). This complex of factors can be regarded as governing a person’s likelihood of judging a given sound as noise, and a model of noise sensitivity as the outcome of a process linking attitudes, states, traits, and neurophysiology has recently been proposed (Welch et al., Citation2022).
5. Health impacts
5.1. Annoyance
Models have been developed to predict the relationship between noise exposure and annoyance, often assessed on the basis of the percentage of people “highly annoyed” by the noise, according to noise levels. Guski et al. (Citation2017) present a systematic review of such studies for road traffic aircraft, and rail, with moderate evidence of relationships identified for aircraft and rail and low for road traffic. Some studies have established curves that relate noise levels from transport specifically (most often using the day-night average sound level, or Ldn) and the percentage of highly annoyed people, as determined through community-based surveys (Miedema & Vos, Citation1999; Ouis, Citation2001). These studies show that differences exist in the level of annoyance between sources of transport noise. Specifically, according to the WHO (Citation2018) at a noise level of 60 dB Lden, the percentage of the population “highly annoyed” by the noise reaches 15%, 17.4% and 36% for road traffic noise, railway and aircraft noise, respectively. On the other hand, some research has shown that railway noise leads to lower levels of annoyance than either road traffic or aircraft noise at the same noise level (Gidlof-Gunnarsson et al., Citation2012; Lechner et al., Citation2019), while aircraft noise always causes higher annoyance for a given sound level.
Noise combines with other aspects of exposure to cause annoyance. For a given level of exposure, more people are annoyed when exposed to noise from both road and rail than when exposed to one or the other individually (Ohrstrom et al., Citation2007). Moreover, noise from rail has been found to be more annoying when also combined with ground vibrations (Gidlof-Gunnarsson et al., Citation2012). It is accepted that noise annoyance cannot be completely explained by acoustical factors associated with a noise source, as is illustrated by the different annoyance reactions exhibited by individuals to the same noise (Shepherd et al., Citation2010).
5.2. Cognitive disruption
Cognition involves the brain processing information provided by the sensory modalities or information retrieved from memory. Typically, this information processing, in the guise of problem-solving and decision-making, is invested in the realisation of goal-directed behaviours, be they task completion or relaxation (Andringa & Lanser, Citation2013). Given the crucial role that cognition plays in survival and vitality, any exogenous agent (such as transportation noise) degrading cognitive function can be classified as a direct health effect (Salomon et al., Citation2003).
As outlined in , the relationship between noise and cognition is influenced by other factors so is unlikely to be modelled by a monotonic dose–response function. Noise from transport sources can acutely impair cognitive function by directly interfering with working memory (Millar, Citation1979), directing attention away from relevant stimuli, or increasing cognitive load and task demands (Szalma & Hancock, Citation2011). Indirectly, the relationship between noise and cognitive function may be mediated by disturbed sleep, whereby noise-degraded sleep induces fatigue and cognitive impairment, while cognition itself can induce poor sleep through enduring cognitive arousal, allowing noise to sustain its direct effect. Note too that sleep can be a protective factor against noise, allowing the individual to remain in states of low cognitive arousal and therefore suppressing the direct effect of noise upon cognition.
Annoyance manifests a strong emotional reaction to the noise, which in turn interferes with cognitive processes by focusing attention onto the noise source at the expense of other tasks. Massonnie et al. (Citation2022) argue for a distinction between annoyance and interference, and by performing an evaluative function on incoming auditory stimuli, cognition itself can amplify annoyance. Furthermore, vulnerable individuals exhibiting the trait of noise sensitivity may have impaired cognitive function due to ineffective attentional filters or reduced working memory capacity. As such, noise-sensitive individuals may be more likely to experience transport-related sleep disturbance or noise annoyance, and, consequently, exhibit further cognitive impairment. Finally, when noise impedes cognitive function and overwhelms coping strategies, a stress response can be triggered. When a stressor is relentless, as can be the case with transport noise, it can lead to chronic sympathetic over-arousal and negative health outcomes. This over-arousal, in turn, can lead to a state of hypervigilance, which can negatively influence attentional processes.
The existing literature fails to provide a definitive account of how transport noise impacts cognition, nor quantify the degree to which transport noise impedes cognitive function. The medley of epidemiological and laboratory-based findings is contradictory, and, without exception, studies call for further research in the area. However, the majority draw similar conclusions, that task-irrelevant transport noise can degrade task performance and impair learning (Thompson et al., Citation2022). Easier tasks are negatively affected by transport noise, but harder cognitive tasks are not (e.g. Halin, Citation2016). The suggestion here is that more demanding tasks engage a more refined locus of attention and are less vulnerable to auditory distraction, or that more demanding tasks rely on additional memory processes that are not burdened by noise. Of relevance, Ellermeier et al. (Citation2020) noted that annoyance by road traffic noise was reduced during a cognitively demanding task, illuminating a possible explanation for these findings.
In terms of the three main transport modalities (aviation, rail, road) research has largely consisted of laboratory studies of these noise sources in isolation, or epidemiological studies such as Bodin et al. (Citation2015), who reported that “combined” exposure (rail and road) is positively associated with concentration problems. In older adults, Mac Domhnaill et al. (Citation2021) reported no relationship between road traffic noise and either memory or processing speed. Mehri et al. (Citation2018) found marginally better performance with respect to complex tasks undertaken in quiet versus a road traffic noise condition, and reported no effect of introversion/extroversion. Aviation noise is reported to degrade cognitive learning, possibly because lower-flying aircraft may elicit fear in some and thus induce a higher cognitive load caused by selective filtering (Trimmel et al., Citation2012).
In the case of children, who are viewed as a vulnerable group in need of protection, a 20-dB increase in aviation noise has been found to be associated with a two-month reading delay (Klatte et al., Citation2017). Matheson et al. (Citation2010) found reduced recognition memory performance, but not cued recall or prospective memory, in a sample of children exposed to aviation noise.
Multiple studies indicate that reaction time is increased when individuals are exposed to nocturnal rail noise, potentially mediated by sleep debt. This is of relevance to Europe where maximum acceptable levels may be increased by 5 dB(A) in the case of rail noise on the basis of it being perceived as less annoying than other sources of noise for the same intensity level (e.g. Bodin et al., Citation2015).
5.3. Sleep problems
A lack of sleep impacts people psychologically and, over time, physiologically (Watson et al., Citation2015). The range of health measures influenced by sleep (e.g. levels of stress, cardiovascular health and mental health) and noise are similar (), while sleep itself is also influenced by noise; this has led to the idea that sleep disruption due to noise may mediate the health impacts of noise, either in whole or in part (Shepherd et al., Citation2010).
Noise from transport sources can impact sleep by preventing people from falling asleep, awakening them or disturbing sleep. A recent meta-analysis has explored these different sleep effects due to noise, including transport noise (Basner & McGuire, Citation2018). Overall, transport noise increased the odds of all three types of self-reported sleep problems by 2–3 per 10 dB increase in night-time noise levels. Interestingly, this increase was observed overall only when participants were explicitly asked about sleep disturbance due to a particular noise source; for example, “How much have you been disturbed in your sleep by railway noise at night when you are sleeping in your house over the last 12 months?” (Hong et al., Citation2010). On the other hand, effects were much reduced when participants were asked without specific reference to noise (e.g. Bartels et al., Citation2021). Since the effect was significant (and dose-responsive) when the reminder was given, the implication is that a specific prompt in the question may improve the accuracy of recall about noise-related sleep problems, rather than artificially increasing the effect.
The relative impact of transport noise from the three main sources: air, road and rail has been investigated in laboratory research using polysomnography (Elmenhorst et al., Citation2019). Aircraft noise exposures were less likely to awaken participants than noise from the other two sources; this is in contrast to the association in self-reported sleep disturbance in the field where aircraft noise is rated as more disturbing than noise from road or rail (e.g. Lechner et al., Citation2021). On the other hand, some field research has found that fewer people were annoyed by given levels of night-time aircraft noise than road or rail, but that the function relating the number of noise events to annoyance was steeper for aircraft noise than road and rail (Weidenfeld et al., Citation2021). Little research has explored the influence of the number of noise events on sleep, but one study on rail noise found that the number of freight train movements was the best predictor (compared to LAeq or the total number of trains of all types) of self-reported awakening (Pennig et al., Citation2012). This raises the question of the effect of vibration associated with noise exposures, which have been shown to increase sleep disturbances and awakenings with polysomnography (Smith et al., Citation2016).
Sleep and noise annoyance may covary; in other words, both annoyance with noise leads to sleep problems, and sleep problems due to noise cause a person to find noise more annoying. This association is present for self-reported sleep disturbance, but not for objectively-measured sleep disturbance (Frei et al., Citation2014). This implies that a person who is disturbed by noise during sleep may be unaware of this, and that the sleep disturbance can occur irrespective of whether they rate noise as annoying when conscious.
Relatively little research has been carried out into the impact of transport noise on children’s sleep. While some studies have found a significant effect (Tiesler et al., Citation2013), others showed effects that were only significant when sorted by gender groups, for example, in girls, but not in boys (Weyde et al., Citation2017). The inconsistency of findings may reflect the difficulty of conducting research in this area, and the need to make assumptions about noise exposures and sleep issues. One study avoided some of these issues by comparing children’s sleep to that of their parents, so levelling estimation biases; this showed that children’s sleep was less influenced by traffic noise than that of their parents (Ohrstrom et al., Citation2006).
5.4. Noise-induced hearing loss
In occupational exposure, 85dBA has been accepted as the limit for an eight-hour exposure in many jurisdictions, even though noise-induced hearing loss (NIHL) may occur at this level (Fink, Citation2017). Exposure to high levels at or above 85 dBA may, over time, lead to noise-induced hearing loss (International Standards Organisation, Citation2013). It has been recommended that 70dBA or even lower be adopted as a safe standard for the public (Fink, Citation2017). There is limited research related to NIHL with transport noise. However, recent research supports the 70dBA proposition as traffic noise of more than 70dBA after adjusting for confounders, has been found to contribute to hearing loss (Wang et al., Citation2021). It has also been suggested that the synergistic effect of an average 74.3dBA of traffic noise and ototoxic air pollution may impair hearing (Caciari et al., Citation2013).
Traffic noise is particularly loud in high density cities, as demonstrated by findings from an Indian study (Kumar & Jain, Citation1994). The research reported that sound level measurements in auto-rickshaws (range 81-96dBA) were highest, followed by buses (77-92dBA), trucks (83-90dBA) and private cars (65-80dBA). These levels of noise suggest that drivers and frequent passengers are at risk of noise-induced hearing loss over time (Kumar & Jain, Citation1994). Land transportation workers are also at risk, with more than 50% of the participants in a cohort of 1000 freight truck drivers having hearing loss (Rezaei & Alipour, Citation2015).
There is a risk of NIHL in people who spend time near road traffic. For example, in 110 Kathmandu traffic police who, on average, worked in the role for approximately 12 years, over half experienced mild hearing loss . Similar potential association of hearing loss among police personnel and traffic noise has been reported in research from other countries (e.g. Win et al., Citation2015).
Hearing loss, especially at higher frequencies, occurs in air crews and is significantly associated with age, flight duration and aircraft type, with helicopter pilots being particularly at risk (Atalay et al., Citation2015). Airport workers who have worked for a duration of more than 5 years have been found to be three times as likely to experience hearing loss than workers with a shorter duration of service (Nasir & Rampal, Citation2012). The duration of time spent on ships has been found to be a predictor of hearing impairment amongst ship workers (Irgens-Hansen et al., Citation2015), with those working in engine rooms being more at risk of NIHL than other ship personnel (Kaerlev et al., Citation2008).
The literature to date mostly concerns transport operators, passengers, and traffic personnel. There is little evidence related to traffic noise and NIHL among those who live close to transport networks.
5.5. Stress
Stress refers to both outcomes and processes. It occurs in response to environmental and psychological factors, and is typically an adaptive response in the short term but leads to harms in the long term: for example, an increase in cardiovascular arousal can increase the blood supply to muscles, rendering an organism stronger and faster, but in the long term, this can lead to greater vulnerability to cardiovascular disease.
Another relevant usage of the term “stress” is oxidative stress, a key mechanism in noise-induced hearing loss (Henderson et al., Citation2006) that may also occur in the cardiovascular system during noise exposure (Schmidt et al., Citation2013). In this section, we focus specifically on psychophysiological stress, rather than oxidative stress.
Psychophysiological stress occurs directly in response to transport noise exposure, and indirectly as a result of the other responses to noise (). This makes it an integral part of the proposed model where initial noise exposure may cause, for example, reduced sleep, leading to a stress reaction in a person and other health effects, which in turn contribute to stress and are exacerbated by stress responses. In other words, stress is the pivotal factor in the associations between transport noise and health.
By its nature, stress cannot be measured directly, though proxies are used which capture activity at different points in the stress response. Many of these are measurable responses of the cardiovascular system (e.g. blood pressure) and are therefore covered in that section. There are also two main biochemical markers: cortisol and adrenaline. These hormones are the end-products of two different, but related, processes that occur as a result of transport noise exposures, and which have a causal role in the other health outcomes: one pathway is mediated by the sympathetic nervous system, and results in adrenaline release and stimulation of receptors that cause increased heart-rate and greater blood supply to muscles as well as increases in blood sugar; the other is mediated by the hypothalamic–pituitary–adrenal axis, resulting in cortisol release, which increases blood sugar levels and can suppress activity in parts of the immune system.
Early work demonstrating an association between stress hormones and noise exposure in the laboratory and the field was summarised by Babisch (Citation2003). In that article, despite demonstrating overall changes in both adrenaline and cortisol in response to noise exposure, Babisch drew attention to the difficulty in comparing between studies, where the time constants, natural rhythms, and individual variations in the expression of the different hormones can vary widely and are hard to control. This is most likely why findings often show effects in one aspect but not another: for example, higher levels of adrenaline, but not cortisol, were measured after exposure to aircraft noise during sleep (Schmidt et al., Citation2013), whereas other studies (e.g. Wagner et al., Citation2010) have shown effects of transport noise exposure on cortisol. More recent reviews on this topic have in general reached similar conclusions: that stress hormones are a useful marker of stress that also provide some insight into the causal pathway, especially with respect to cardiovascular health problems (Daiber et al., Citation2019).
5.6. Mental health
A mental health condition is characterised by the enduring presence of mental distress that negatively impacts day-to-day functioning, and which can be classified on a continuum from mild to severe using a recognised diagnostic system. Estimating the relationship between transport-related noise and mental health conditions needs to be asked in relation to the affected population. Firstly, for those already experiencing poor mental health, the Stress Hypothesis conceptualises transportation noise as a stressor that exacerbates established symptoms of mental illness by acting as a toxic stressor. Here, the amplification of pre-existing symptoms such as sleep difficulties, cognitive impairments and hypervigilance may potentially be mediated by noise sensitivity, a common trait across mental health conditions.
The Vulnerability–Stress model (Goh & Agius, Citation2010) can account for the individual differences in resilience to transport noise. This model describes an interaction between an individual’s predisposition to a mental health condition and the life stressors (e.g. noise) they encounter, where the two combine to create a threshold that, when exceeded, leads to the development of a mental health condition. In this scheme, exposure to noise and the resultant stress could lead to learned helplessness (e.g. depression), hypervigilance due to a failure to habituate (e.g. anxiety), or cognitive overload (e.g. schizophrenia) that, if chronic, could develop into clinical disorders.
Any direct effect of transport noise upon mental health will likely be accompanied by indirect effects in the guise of mediating or moderating effects. While the literature has yet to definitively identify risk and protective factors (Stansfeld et al., Citation2021), noise sensitivity, sleep disturbance and annoyance have been mooted for the former, and coping resources and social support for the latter. However, there is a need for further conceptual work to be carried out. For example, should noise sensitivity be operationalised as a personality trait or as a symptom of mental illness itself? Additionally, is noise annoyance a risk factor or an outcome in its own right? On this matter, the development of a standardised medical description of noise annoyance that is both clinically relevant and suitable for population-based studies is necessary. For example, categorisation systems list “irritability” as a symptom of anxiety. Is this equivalent to noise annoyance? Though it might be intuitive to think that noise annoyance moderates the relationship between transport noise and mental health outcomes, the actual data do not strongly support this hypothesis (Stansfeld et al., Citation2021).
Undertaking a meta-analysis, Lan et al. (Citation2020) reported a significant dose–response association between transport noise and anxiety . Furthermore, they reported no significant differences across aviation, railway, and road noise, reflecting earlier work (Clark et al., Citation2020). Focusing on aviation noise around Frankfurt airport, Beutel et al. (Citation2016) reported strong links between noise annoyance and anxiety, while a multi-airport European study (the HYENA study) reported a relationship between aircraft noise and the use of anxiety-reducing medication (Floud et al., Citation2011). The quality of data in all this work has been questioned by the authors, who appealed for further research.
Similar conclusions have been drawn with regards transportation noise and depression (Beutel et al., Citation2016; Clark et al., Citation2020), that there is a positive correlation between the two. However, the integrity of the evidence is questionable and further research is required. Furthermore, both anxiety and depression seem to be affected equally by transportation noise, perhaps not an unexpected finding given the commonly-reported relationship between the two. Little transport-related noise research has been undertaken on other clinical populations such as schizophrenia, autism spectrum disorder, or bipolar disorder (but see van Kamp and Davies (Citation2013)), encouraging future studies in this area.
5.7. Metabolic health outcomes
The stress mechanisms reported above may be expected to lead to metabolic health effects, including being overweight and diabetes, due to the release of cortisol and adrenaline, as described in earlier reviews (Munzel et al., Citation2017; van Kempen et al., Citation2018). Body-mass index (BMI), and the associated categorisations “overweight” (BMI > 25) and “obese” (BMI ≥ 30) were found to be higher in people exposed to more road traffic noise, as was waist circumference (Foraster et al., Citation2018). In this study, longitudinal effects (i.e. increases in BMI/waist with exposure to transport noise over time) were less clear than were the overall associations; however in another much larger study (N = 39,720, about ten times the number of participants), these effects were detectable (Christensen et al., Citation2015). This implies that the associations detected cross-sectionally are the result of small increases in body fat occurring at greater rates over many years in those exposed to transport noise. Presumably, the mechanisms underlying this increased rate of fat deposit are multiple, including the cortisol mechanism described earlier, as well as stress-related behaviour changes, loss of sleep, and multiple biochemical changes as have been reviewed elsewhere (Tomiyama, Citation2019).
The level of road traffic noise predicted new cases of diabetes in a cohort of people aged 50–64 years: incidence ratios increased by around 10% per 10-dB increase in traffic noise exposure during the prior five year period, implying a dose–response effect of transport noise level on the risk of diabetes (Sorensen et al., Citation2013). These findings have been supported by later work, some of which showed non-significant trends that may represent a causal role of poorer sleep quality (Eze et al., Citation2017). To explore this hypothesis, research with simulated traffic noise, presented at 45 dB Leq for four nights during sleep, resulted in participants experiencing greater glucose responses than a control group sleeping in simulated quieter natural conditions (Thiesse et al., Citation2018). This research demonstrated short-term effects consistent with the field studies. Interestingly, however, sleep quality did not vary between groups, implying that the mechanism underlying the metabolic changes was not sleep dependent. Later research has shown activation of the amygdala to be a key mediator in the association between transport noise exposure and both visceral adiposity and diabetes (Osborne et al., Citation2021). This may imply that the emotional/limbic system response to the noise is the primary cause of these health effects, a hypothesis that fits well with the stress-hormone mechanisms.
5.8. Cardiovascular
Laboratory, field and epidemiological studies have established that noise contributes to cardiovascular disease outcomes and the incidence of cardiovascular diseases (Münzel et al., Citation2018, Citation2021). Meta-analyses of studies looking into the association between road traffic noise and ischemic heart diseases concluded that road traffic noise could increase the likelihood of cardiovascular diseases by about 6–8% (e.g. Vienneau et al., Citation2015). As a dose response relationship, the risk of heart diseases grows with increases in road traffic noise levels above 60 dB Leq (Babisch, Citation2008). A study of approximately 4000 participants reported an odds ratio of 1.8 of developing myocardial infarction in people who lived on streets with sound levels greater than 70 dB Leq for at least 10 years, compared with those who lived on streets with levels less than or equal to 60 dB Leq (Babisch et al., Citation2005). This finding is supported by a population-based study which found that those living in areas of high noise (>70 dB Leq) had a 22% greater coronary heart disease mortality than people living in areas of low noise (58 dB Leq) (Gan et al., Citation2012). A retrospective study of approximately six million people residing near airports found an association between aircraft noise and hospital admission rates for cardiovascular disease from areas where noise levels were >55 dB Leq (Correia et al., Citation2013). The key findings suggest that noise levels, and the length of residency in high noise areas, are associated with the risk of developing cardiovascular diseases.
Interestingly, a Swiss study of approximately 4.4 million participants found no association between aircraft noise and cardiovascular diseases overall, but reported significant risks for some cardiovascular outcomes such as myocardial infarction, heart failure and ischemic stroke (Heritier et al., Citation2017). The night ban on air traffic in Switzerland was offered as an explanation for the weaker overall association. This study also reported a significant association between railway noise and ischemic heart diseases and myocardial infarction. Road traffic noise was found to be significantly associated with all cardiovascular disease outcomes apart from stroke. A recent longer follow-up study found similar associations where, after adjusting for air pollution, road traffic and railway noise exposure were associated with the majority of cardiovascular disease-related mortality (Vienneau et al., Citation2022). A significant finding of this study was that exposure-response relationships increased from low noise levels, as much as 20 dB below the WHO guideline limits of 53 dB Lden for road traffic, 54 for railway, and 45 for aircraft.
5.9. Health-related quality of life
Quality of Life is:
an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. It is a broad ranging concept affected in a complex way by the person’s physical health, psychological state, personal beliefs, social relationships and their relationship to salient features of their environment. (Kuyken, Citation1995, p. 1404)
Transport noise influences HRQoL: Dratva et al. (Citation2010) and Shepherd et al. (Citation2013) both found a significant negative reduction in HRQoL with road traffic noise. Moreover, greater noise sensitivity was associated with poorer HRQoL in those exposed to transport noise, but not in those living in quieter areas (Welch et al., Citation2018). In participants exposed to aviation noise, HRQoL was reduced through annoyance and sleep disruption, and the effect was greater in more noise sensitive people (Shepherd et al., Citation2010). In the case of road traffic, air pollution is a stronger predictor of scores in the physical domain of HRQoL while noise is a stronger predictor in the psychological, social and environmental domains (Shepherd et al., Citation2016). This is consistent with the predominance of studies in the literature investigating objective measures of health, such as mortality and admissions to hospital in the case of air pollution and measures such as HRQoL in the case of environmental noise. These results suggest that the mitigation of traffic effects requires both air quality and noise to be addressed (Shepherd et al., Citation2010).
5.10. Burden of disease
Disability-Adjusted Life Years (DALYs) are a weighted combination of years of life lost and years lost to disability attributed to a health risk factor or condition. As such, they attempt to aggregate the overall influence of multiple health conditions on a person or population. They are a quantification and combination of multiple estimates that provide a synthesis and a simple metric allowing comparison against other potential risks.
Estimates of the DALYs attributed to transport noise exposure have been conducted in an attempt to provide a generalised view of its impact. In a study of excess exposures to environmental health risk conducted over twenty years in Barcelona, transport noise was deemed to account for 36% of the DALYs lost (Mueller et al., Citation2017). In another study conducted in Warsaw, 46% of the DALY’s lost due to transport (including the effects of air pollution and injuries) were attributed to noise (Tainio, Citation2015). Other research has attributed DALYs lost attributed to traffic noise on national levels in Sweden (Eriksson et al., Citation2017) and Germany (Tobollik et al., Citation2019), in both cases showing that most of the lost DALYs nationally attributed to transport noise were from road transport. Overall the evidence from DALYs demonstrates that many years of healthy life are lost to the various impacts of transport-related noise, and the measure provides a useful metric for policy-makers.
6. Conclusions
We have described the main health outcomes associated with transport noise () in terms of direct and indirect outcomes. It is clear that annoyance, cognitive disruption, sleep problems, and noise-induced hearing loss occur in direct response to noise exposure. These four outcomes of human exposure to noise tend to be greater in those with greater traffic noise exposure. They may also occur in response to each other: for example, a person might feel annoyed by noise because it awakened them; or a person might be unable to fall asleep because they are feeling annoyed by noise. At the second level of health outcomes is stress which may occur in response to any of the four aforementioned outcomes, and may in itself be a direct response to noise. In this, it appears to have a pivotal role in that it can also be regarded as a causal factor in the more indirect health outcomes. The third level of health outcomes includes mental health, metabolic, and cardiovascular health outcomes. These are likely to be mediated by stress, but may also be influenced by the more direct outcomes. At the fourth level, health-related quality of life and DALYs are most global and general measures of health that have been shown to be influenced by noise exposure. Again, they might be influenced by any of the other outcomes to the left of it in , or might be a response to noise in itself. We have acknowledged that other associated influences on health might play a role: social inequities, air pollution, and vibration are all potentially present in those who are more exposed to transport noise. It is hard to tease apart the effects of noise from these effects, but dose-responsiveness of health outcomes to noise has been shown in many cases and provides some level of assurance. Finally, exposure to the sound of transport may not lead to some health outcomes, especially those mediated by stress, unless a person is noise sensitive. This moderator of the association between transport noise and health is complex, but important and more research into its nature is needed.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Anciaes, P. R., Metcalfe, P. J., & Heywood, C. (2017). Social impacts of road traffic: Perceptions and priorities of local residents. Impact Assessment and Project Appraisal, 35(2), 172–183. https://doi.org/10.1080/14615517.2016.1269464
- Andringa, T. C., & Lanser, J. J. L. (2013). How pleasant sounds promote and annoying sounds impede health: A cognitive approach. International Journal of Environmental Research and Public Health, 10(4), 1439–1461. https://doi.org/10.3390/ijerph10041439
- Atalay, H., Babakurban, S. T., & Aydin, E. (2015). Evaluation of hearing loss in pilots. Turkish Archives of Otorhinolaryngology, 53(4), 155–162. https://doi.org/10.5152/tao.2015.1330
- Audrin, T., Apparicio, P., & Séguin, A.-M. (2022). Aircraft noise and environmental equity in Montréal: A comparison of noise indicators and an analysis of the impacts of COVID-19. Transportation Research Part D: Transport and Environment, 106, 103274. https://doi.org/10.1016/j.trd.2022.103274
- Babisch, W. (2003). Stress hormones in the research on cardiovascular effects of noise. Noise and Health, 5(18), 1–11. https://www.scopus.com/inward/record.uri?eid=2-s2.0-0038460319&partnerID=40&md5=afdfd9622aad3bb77627e67345828a18
- Babisch, W. (2008). Road traffic noise and cardiovascular risk. Noise & Health, 10(38), 27–33. https://doi.org/10.4103/1463-1741.39005
- Babisch, W., Beule, B., Schust, M., Kersten, N., & Ising, H. (2005). Traffic noise and risk of myocardial infarction. Epidemiology, 16(1), 33–40. https://doi.org/10.1097/01.ede.0000147104.84424.24
- Bartels, S., Ogren, M., Kim, J. L., Fredriksson, S., & Waye, K. P. (2021). The impact of nocturnal road traffic noise, bedroom window orientation, and work-related stress on subjective sleep quality: Results of a cross-sectional study among working women. International Archives of Occupational and Environmental Health, 94(7), 1523–1536. https://doi.org/10.1007/s00420-021-01696-w
- Basner, M., Babisch, W., Davis, A., Brink, M., Clark, C., Janssen, S., & Stansfeld, S. (2014). Auditory and non-auditory effects of noise on health. Lancet, 383(9925), 1325–1332. https://doi.org/10.1016/s0140-6736(13)61613-x
- Basner, M., & McGuire, S. (2018). WHO environmental noise guidelines for the European region: A systematic review on environmental noise and effects on sleep. International Journal of Environmental Research and Public Health, 15(3), 519. https://doi.org/10.3390/ijerph15030519
- Beutel, M. E., Junger, C., Klein, E. M., Wild, P., Lackner, K., Blettner, M., & Munzel, T. (2016). Noise annoyance is associated with depression and anxiety in the general population – The contribution of aircraft noise. PLoS One, 11(5), e0155357. https://doi.org/10.1371/journal.pone.0155357
- Bocquier, A., Cortaredona, S., Boutin, C., David, A., Bigot, A., Chaix, B., & Verger, P. (2012). Small-area analysis of social inequalities in residential exposure to road traffic noise in Marseilles, France. European Journal of Public Health, 23(4), 540–546. https://doi.org/10.1093/eurpub/cks059
- Bodin, T., Bjork, J., Ardo, J., & Albin, M. (2015). Annoyance, sleep and concentration problems due to combined traffic noise and the benefit of quiet side. International Journal of Environmental Research and Public Health, 12(2), 1612–1628. https://doi.org/10.3390/ijerph120201612
- Caciari, T., Rosati, M. V., Casale, T., Loreti, B., Sancini, A., Riservato, R., & Tomei, G. (2013). Noise-induced hearing loss in workers exposed to urban stressors. Science of The Total Environment, 463-464, 302–308. https://doi.org/10.1016/j.scitotenv.2013.06.009
- Christensen, J. S., Raaschou-Nielsen, O., Tjonneland, A., Nordsborg, R. B., Jensen, S. S., Sorensen, T. I. A., & Sorensen, M. (2015). Long-term exposure to residential traffic noise and changes in body weight and waist circumference: A cohort study. Environmental Research, 143, 154–161. https://doi.org/10.1016/j.envres.2015.10.007
- Clark, C., Crombie, R., Head, J., Van Kamp, I., Van Kempen, E., & Stansfeld, S. A. (2012). Does traffic-related air pollution explain associations of aircraft and road traffic noise exposure on children's health and cognition? A secondary analysis of the United Kingdom sample from the RANCH project. American Journal of Epidemiology, 176(4), 327–337. https://doi.org/10.1093/aje/kws012
- Clark, C., Crumpler, C., & Notley, H. (2020). Evidence for environmental noise effects on health for the United Kingdom policy context: A systematic review of the effects of environmental noise on mental health, wellbeing, quality of life, cancer, dementia, birth, reproductive outcomes, and cognition. International Journal of Environmental Research and Public Health, 17(2), 393. https://doi.org/10.3390/ijerph17020393
- Correia, A. W., Peters, J. L., Dominici, F., Correia, A. W., Peters, J. L., Levy, J. I., & Dominici, F. (2013). Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: Multi-airport retrospective study. BMJ: British Medical Journal, 347(3), f5561–f5561. https://doi.org/10.1136/bmj.f5561
- Crichton, F., Dodd, G., Schmid, G., & Petrie, K. J. (2015). Framing sound: Using expectations to reduce environmental noise annoyance. Environmental Research, 142, 609–614. https://doi.org/10.1016/j.envres.2015.08.016
- Daiber, A., Kroller-Schon, S., Frenis, K., Oelze, M., Kalinovic, S., Vujacic-Mirski, K., & Munzel, T. (2019). Environmental noise induces the release of stress hormones and inflammatory signaling molecules leading to oxidative stress and vascular dysfunction-signatures of the internal exposome. Biofactors, 45(4), 495–506. https://doi.org/10.1002/biof.1506
- Di, G. Q., Zhao, C. X., Lin, Q. H., & Fan, M. C. (2019). Study on annoyance and sleep disturbance induced by combined noises from road traffic and viaduct rail transit. Acoustics Australia, 47(3), 229–237. https://doi.org/10.1007/s40857-019-00167-0
- Dratva, J., Zemp, E., Dietrich, D. F., Bridevaux, P. O., Rochat, T., Schindler, C., & Gerbase, M. W. (2010). Impact of road traffic noise annoyance on health-related quality of life: Results from a population-based study. Quality of Life Research, 19(1), 37–46. https://doi.org/10.1007/s11136-009-9571-2
- Dreger, S., Schüle, S. A., Hilz, L. K., & Bolte, G. (2019). Social inequalities in environmental noise exposure: A review of evidence in the WHO European region. International Journal of Environmental Research and Public Health, 16(6), 1011. https://www.mdpi.com/1660-4601/16/6/1011 https://doi.org/10.3390/ijerph16061011
- Ellermeier, W., Kattner, F., Klippenstein, E., Kreis, M., & Marquis-Favre, C. (2020). Short-term noise annoyance and electrodermal response as a function of sound-pressure level, cognitive task load, and noise sensitivity. Noise & Health, 22(105), 46–55. https://doi.org/10.4103/nah.NAH_47_19
- Elmenhorst, E. M., Griefahn, B., Rolny, V., & Basner, M. (2019). Comparing the effects of road, railway, and aircraft noise on sleep: Exposure-response relationships from pooled data of three laboratory studies. International Journal of Environmental Research and Public Health, 16(6), 1073. https://doi.org/10.3390/ijerph16061073
- Eriksson, C., Bodin, T., & Selander, J. (2017). Burden of disease from road traffic and railway noise – A quantification of healthy life years lost in Sweden. Scandinavian Journal of Work Environment & Health, 43(6), 519–525. https://doi.org/10.5271/sjweh.3653
- Eze, I. C., Foraster, M., Schaffner, E., Vienneau, D., Heritier, H., Rudzik, F., & Probst-Hensch, N. (2017). Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. International Journal of Epidemiology, 46(4), 1115–1125. https://doi.org/10.1093/ije/dyx020
- Fidell, S., Pearsons, K., Silvati, L., & Sneddon, M. (2002). Relationship between low-frequency aircraft noise and annoyance due to rattle and vibration. Journal of the Acoustical Society of America, 111(4), 1743–1750. https://doi.org/10.1121/1.1448339
- Fink, D. J. (2017). What is a safe noise level for the public? American Journal of Public Health, 107(1), 44–45. https://doi.org/10.2105/ajph.2016.303527
- Floud, S., Vigna-Taglianti, F., Hansell, A., Blangiardo, M., Houthuijs, D., Breugelmans, O., & Team, H. S. (2011). Medication use in relation to noise from aircraft and road traffic in six European countries: Results of the HYENA study. Occupational and Environmental Medicine, 68(7), 518–524. https://doi.org/10.1136/oem.2010.058586
- Foraster, M., Eze, I. C., Vienneau, D., Schaffner, E., Jeong, A., Heritier, H., & Probst-Hensc, N. (2018). Long-term exposure to transportation noise and its association with adiposity markers and development of obesity. Environment International, 121, 879–889. https://doi.org/10.1016/j.envint.2018.09.057
- Foraster, M., Medina-Ramon, M., Basagana, X., Bouso, L., Elosua, R., Juvinya, D., & Deltell, A. (2009). Noise and air pollution correlation and its determinants in the City of Girona. Epidemiology, 20(6), S180–S180. https://doi.org/10.1097/01.ede.0000362608.59588.84
- Frei, P., Mohler, E., & Roosli, M. (2014). Effect of nocturnal road traffic noise exposure and annoyance on objective and subjective sleep quality. International Journal of Hygiene and Environmental Health, 217(2-3), 188–195. https://doi.org/10.1016/j.ijheh.2013.04.003
- Fyhri, A., & Klaeboe, R. (2009). Road traffic noise, sensitivity, annoyance and self-reported health – A structural equation model exercise. Environment International, 35(1), 91–97. https://doi.org/10.1016/j.envint.2008.08.006
- Gan, W. Q., Davies, H. W., Brauer, M., Davies, H. W., & Koehoorn, M. (2012). Association of long-term exposure to community noise and traffic-related air pollution with coronary heart disease mortality. American Journal of Epidemiology, 175(9), 898–906. https://doi.org/10.1093/aje/kwr424
- Gelb, J., & Apparicio, P. (2021). Cyclists’ exposure to atmospheric and noise pollution: A systematic literature review. Transport Reviews, 41(6), 742–765. https://doi.org/10.1080/01441647.2021.1895361
- Gidlof-Gunnarsson, A., Ogren, M., Jerson, T., & Ohrstrom, E. (2012). Railway noise annoyance and the importance of number of trains, ground vibration, and building situational factors. Noise & Health, 14(59), 190–201. https://doi.org/10.4103/1463-1741.99895
- Goh, C., & Agius, M. (2010). The stress-vulnerability model how does stress impact on mental illness at the level of the brain and what are the consequences? Psychiatria Danubina, 22(2), 198–202.
- Guski, R., Schreckenberg, D., & Schuemer, R. (2017). WHO environmental noise guidelines for the European region: A systematic review on environmental noise and annoyance. International Journal of Environmental Research and Public Health, 14(12), 1539. https://doi.org/10.3390/ijerph14121539
- Halin, N. (2016). Distracted while Reading? Changing to a hard-to-read font shields against the effects of environmental noise and speech on text memory. Frontiers in Psychology, 7. https://doi.org/10.3389/fpsyg.2016.01196
- Havard, S., Reich, B. J., Bean, K., & Chaix, B. (2011). Social inequalities in residential exposure to road traffic noise: An environmental justice analysis based on the RECORD cohort study. Occupational and Environmental Medicine, 68(5), 366–374. https://doi.org/10.1136/oem.2010.060640
- Henderson, D., Bielefeld, E. C., Harris, K. C., & Hu, B. H. (2006). The role of oxidative stress in noise-induced hearing loss. Ear and Hearing, 27(1), 1–19. https://doi.org/10.1097/01.aud.0000191942.36672.f3
- Heritier, H., Vienneau, D., Roosli, M., Héritier, H., Vienneau, D., Foraster, M., & Röösli, M. (2017). Transportation noise exposure and cardiovascular mortality: A nationwide cohort study from Switzerland. European Journal of Epidemiology, 32(4), 307–315. https://doi.org/10.1007/s10654-017-0234-2
- Hong, J., Kim, J., Lim, C., Kim, K., & Lee, S. (2010). The effects of long-term exposure to railway and road traffic noise on subjective sleep disturbance. Journal of the Acoustical Society of America, 128(5), 2829–2835. https://doi.org/10.1121/1.3493437
- International Standards Organisation. (2013). Acoustics – Estimation of noise-induced hearing loss. International Organization for Standardization.
- Irgens-Hansen, K., Sunde, E., Bråtveit, M., Baste, V., Oftedal, G., Koefoed, V., & Moen, B. E. (2015). Hearing loss in the royal Norwegian navy: A cross-sectional study. International Archives of Occupational and Environmental Health, 88(5), 641–649. https://doi.org/10.1007/s00420-014-0988-8
- Kaerlev, L., Jensen, A., Nielsen, P., Olsen, J., Hannerz, H., & Tuchsen, F. (2008). Hospital contacts for noise-related hearing loss among Danish seafarers and fishermen: A population-based cohort study. Noise and Health, 10(39), 41–45. https://doi.org/10.4103/1463-1741.40822
- Karimi, M., & Brazier, J. (2016). Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics, 34(7), 645–649. https://doi.org/10.1007/s40273-016-0389-9
- Klatte, M., Spilski, J., Mayerl, J., Mohler, U., Lachmann, T., & Bergstrom, K. (2017). Effects of aircraft noise on Reading and quality of life in primary school children in Germany: Results from the NORAH study. Environment and Behavior, 49(4), 390–424. https://doi.org/10.1177/0013916516642580
- Kumar, K., & Jain, V. K. (1994). A study of noise in various modes of transport in Delhi. Applied Acoustics, 43(1), 57–65. https://doi.org/10.1016/0003-682X(94)90041-8
- Kuyken, K. (1995). The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409. https://doi.org/10.1016/0277-9536(95)00112-k
- Lan, Y. L., Roberts, H., Kwan, M. P., & Helbich, M. (2020). Transportation noise exposure and anxiety: A systematic review and meta-analysis. Environmental Research, 191, 110118. https://doi.org/10.1016/j.envres.2020.110118
- Lechner, C., Schnaiter, D., & Bose-O'Reilly, S. (2019). Combined effects of aircraft, rail, and road traffic noise on total noise annoyance – A cross-sectional study in Innsbruck. International Journal of Environmental Research and Public Health, 16(18), 3504. https://doi.org/10.3390/ijerph16183504
- Lechner, C., Schnaiter, D., & Bose-O'Reilly, S. (2021). Application of the noise annoyance equivalents model for aircraft, rail and road traffic noise to self-reported sleep disturbance. Acta Acustica, 5, 12. https://doi.org/10.1051/aacus/2021005
- Mac Domhnaill, C., Douglas, O., Lyons, S., Murphy, E., & Nolan, A. (2021). Road traffic noise and cognitive function in older adults: A cross-sectional investigation of The Irish Longitudinal Study on Ageing. Bmc Public Health, 21(1), 1814. https://doi.org/10.1186/s12889-021-11853-y
- Maclachlan, L., Ogren, M., van Kempen, E., Hussain-Alkhateeb, L., & Waye, K. P. (2018). Annoyance in response to vibrations from railways. International Journal of Environmental Research and Public Health, 15(9), 1887. https://doi.org/10.3390/ijerph15091887
- Maigrot, P., Parizet, E., & Marquis-Favre, C. (2020). Annoyance due to combined railway noise and vibration: Comparison and testing of results from the literature. Applied Acoustics, 165, 107324. https://doi.org/10.1016/j.apacoust.2020.107324
- Marmot, M., Allen, J., Bell, R., Bloomer, E., & Goldblatt, P. (2012). WHO European review of social determinants of health and the health divide. The Lancet, 380(9846), 1011–1029. https://doi.org/10.1016/s0140-6736(12)61228-8
- Massonnie, J., Frasseto, P., Mareschal, D., & Kirkham, N. Z. (2022). Learning in noisy classrooms: Children’s reports of annoyance and distraction from noise are associated with individual differences in mind-wandering and switching skills. Environment and Behavior, 54(1), 58–88. https://doi.org/10.1177/0013916520950277
- Matheson, M., Clark, C., Martin, R., van Kempen, E., Haines, M., Barrio, I. L., & Stansfeld, S. (2010). The effects of road traffic and aircraft noise exposure on children’s episodic memory: The RANCH project. Noise & Health, 12(49), 244–254. https://doi.org/10.4103/1463-1741.70503
- Mehri, A., Alimohammadi, I., Ebrahimi, H., Hajizadeh, R., & Roudbari, M. (2018). Effect of traffic noise on mental performance with regard to introversion and task complexity. Applied Acoustics, 132, 118–123. https://doi.org/10.1016/j.apacoust.2017.11.019
- Meline, J., Van Hulst, A., Thomas, F., Karusisi, N., & Chaix, B. (2013). Transportation noise and annoyance related to road traffic in the French RECORD study. International Journal of Health Geographics, 12(1), 44. https://doi.org/10.1186/1476-072x-12-44
- Miedema, H. M. E., & Vos, H. (1999). Demographic and attitudinal factors that modify annoyance from transportation noise. Journal of the Acoustical Society of America, 105(6), 3336–3344. https://doi.org/10.1121/1.424662
- Millar, K. (1979). Noise and the rehearsal-masking hypothesis. British Journal of Psychology, 70(NOV), 565–577. https://doi.org/10.1111/j.2044-8295.1979.tb01732.x
- Mueller, N., Rojas-Rueda, D., Basagana, X., Cirach, M., Cole-Hunter, T., Dadvand, P., & Nieuwenhuijsen, M. (2017). Health impacts related to urban and transport planning: A burden of disease assessment. Environment International, 107, 243–257. https://doi.org/10.1016/j.envint.2017.07.020
- Münzel, T., Sørensen, M., & Daiber, A. (2021). Transportation noise pollution and cardiovascular disease. Nature Reviews Cardiology, 18(9), 619–636. https://doi.org/10.1038/s41569-021-00532-5
- Munzel, T., Sorensen, M., Gori, T., Schmidt, F. P., Rao, X. Q., Brook, J., & Rajagopalan, S. (2017). Environmental stressors and cardio-metabolic disease: Part I-epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. European Heart Journal, 38(8), 550–556B. https://doi.org/10.1093/eurheartj/ehw269
- Münzel, T., Sørensen, M., Schmidt, F., Schmidt, E., Steven, S., Kröller-Schön, S., & Daiber, A. (2018). The adverse effects of environmental noise exposure on oxidative stress and cardiovascular risk. Antioxidants & Redox Signaling, 28(9), 873–908. https://doi.org/10.1089/ars.2017.7118
- Nasir, H., & Rampal, K. (2012). Hearing loss and contributing factors among airport workers in Malaysia. The Medical Journal of Malaysia, 67(1), 81–86.
- Ogren, M., Gidlof-Gunnarsson, A., Smith, M., Gustavsson, S., & Waye, K. P. (2017). Comparison of annoyance from railway noise and railway vibration. International Journal of Environmental Research and Public Health, 14(7), 805. https://doi.org/10.3390/ijerph14070805
- Ohrstrom, E., Barregard, L., Andersson, E., Skanberg, A., Svensson, H., & Angerheim, P. (2007). Annoyance due to single and combined sound exposure from railway and road traffic. Journal of the Acoustical Society of America, 122(5), 2642–2652. https://doi.org/10.1121/1.2785809
- Ohrstrom, E., Hadzibajramovic, E., Holmes, M., & Svensson, H. (2006). Effects of road traffic noise on sleep: Studies on children and adults. Journal of Environmental Psychology, 26(2), 116–126. https://doi.org/10.1016/j.jenvp.2006.06.004
- Osborne, M. T., Naddaf, N., Abohashem, S., Radfar, A., Ghoneem, A., Dar, T., & Tawakol, A. (2021). A neurobiological link between transportation noise exposure and metabolic disease in humans. Psychoneuroendocrinology, 131, 105331. https://doi.org/10.1016/j.psyneuen.2021.105331
- Ouis, D. (2001). Annoyance from road traffic noise: A review. Journal of Environmental Psychology, 21(1), 101–120. https://doi.org/10.1006/jevp.2000.0187
- Park, J., Chung, S., Lee, J., Sung, J. H., Cho, S. W., & Sim, C. S. (2017). Noise sensitivity, rather than noise level, predicts the non-auditory effects of noise in community samples: A population-based survey. Bmc Public Health, 17(1), 315. https://doi.org/10.1186/s12889-017-4244-5
- Paunovic, K., Jakovljevic, B., & Belojevic, G. (2009). Predictors of noise annoyance in noisy and quiet urban streets. Science of The Total Environment, 407(12), 3707–3711. https://doi.org/10.1016/j.scitotenv.2009.02.033
- Pennig, S., Quehl, J., Mueller, U., Rolny, V., Maass, H., Basner, M., & Elmenhorst, E. M. (2012). Annoyance and self-reported sleep disturbance due to night-time railway noise examined in the field. Journal of the Acoustical Society of America, 132(5), 3109–3117. https://doi.org/10.1121/1.4757732
- Rezaei, L., & Alipour, V. (2015). Prevalence of noise induced hearing loss among vehicle drivers at Bandar Abbas freight terminal, south of Iran. Environmental Health Engineering and Management Journal, 2(3), 135–139.
- Salomon, J., Chatterji, S., Sadana, R., Ustun, T., & Murray, C. J. L. (2003). Quantifying individual levels of health: Definitions, concepts, and measurement issues. In C. J. L. Murray, & D. B. Evans (Eds.), Health systems performance assessment debates, methods and empiricisms (pp. 900). World Health Organisation.
- Schmidt, F. P., Basner, M., Kroger, G., Weck, S., Schnorbus, B., Muttray, A., & Munzel, T. (2013). Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. European Heart Journal, 34(45), 3508. https://doi.org/10.1093/eurheartj/eht269
- Shepherd, D., Dirks, K., Welch, D., McBride, D., & Landon, J. (2016). The covariance between air pollution annoyance and noise annoyance, and its relationship with health-related quality of life. International Journal of Environmental Research and Public Health, 13(8), 792. https://doi.org/10.3390/ijerph13080792
- Shepherd, D., Welch, D., Dirks, K. N., & Mathews, R. (2010). Exploring the relationship between noise sensitivity, annoyance and health-related quality of life in a sample of adults exposed to environmental noise. International Journal of Environmental Research and Public Health, 7(10), 3579–3594. https://doi.org/10.3390/ijerph7103580
- Shepherd, D., Welch, D., Dirks, K. N., & McBride, D. (2013). Do quiet areas afford greater health-related quality of life than noisy areas? International Journal of Environmental Research and Public Health, 10(4), 1284–1303. https://doi.org/10.3390/ijerph10041284
- Shepherd, D., Welch, D., McBride, D., & Dirks, K. N. (2021). Health-related quality of life across a variety of community contexts. International Journal of Community Well-Being, 4(1), 17–31. https://doi.org/10.1007/s42413-020-00076-5
- Smith, M. G., Croy, I., Hammar, O., & Waye, K. P. (2016). Vibration from freight trains fragments sleep: A polysomnographic study. Scientific Reports, 6(1), 24717. https://doi.org/10.1038/srep24717
- Sorensen, M., Andersen, Z. J., Nordsborg, R. B., Becker, T., Tjonneland, A., Overvad, K., & Raaschou-Nielsen, O. (2013). Long-term exposure to road traffic noise and incident diabetes: A cohort study. Environmental Health Perspectives, 121(2), 217–222. https://doi.org/10.1289/ehp.1205503
- Stansfeld, S., Clark, C., Smuk, M., Gallacher, J., & Babisch, W. (2021). Road traffic noise, noise sensitivity, noise annoyance, psychological and physical health and mortality. Environmental Health, 20(1), 32. https://doi.org/10.1186/s12940-021-00720-3
- Szalma, J. L., & Hancock, P. A. (2011). Noise effects on human performance: A meta-analytic synthesis. Psychological Bulletin, 137(4), 682–707. https://doi.org/10.1037/a0023987
- Tainio, M. (2015). Burden of disease caused by local transport in Warsaw, Poland. Journal of Transport & Health, 2(3), 423–433. https://doi.org/10.1016/j.jth.2015.06.005
- Thiesse, L., Rudzik, F., Spiegel, K., Leproult, R., Pieren, R., Wunderli, J. M., & Cajochen, C. (2018). Adverse impact of nocturnal transportation noise on glucose regulation in healthy young adults: Effect of different noise scenarios. Environment International, 121, 1011–1023. https://doi.org/10.1016/j.envint.2018.05.036
- Thompson, R., Smith, R. B., Karim, Y. B., Shen, C., Drummond, K., Teng, C., & Toledano, M. B. (2022). Noise pollution and human cognition: An updated systematic review and meta-analysis of recent evidence. Environment International, 158, 106905. https://doi.org/10.1016/j.envint.2021.106905
- Tiesler, C. M. T., Birk, M., Thiering, E., Kohlbock, G., Koletzko, S., Bauer, C. P., & Grp, L. I. S. (2013). Exposure to road traffic noise and children’s behavioural problems and sleep disturbance: Results from the GINIplus and LISAplus studies. Environmental Research, 123, 1–8. https://doi.org/10.1016/j.envres.2013.01.009
- Tobollik, M., Hintzsche, M., Wothge, J., Myck, T., & Plass, D. (2019). Burden of disease due to traffic noise in Germany. International Journal of Environmental Research and Public Health, 16(13), 2304. https://doi.org/10.3390/ijerph16132304
- Tomiyama, A. J. (2019). Stress and obesity. In S. T. Fiske (Ed.), Annual review of psychology, Vol 70 (pp. 703–718). https://doi.org/10.1146/annurev-psych-010418-102936
- Trimmel, M., Atzlsdorfer, J., Tupy, N., & Trimmel, K. (2012). Effects of low intensity noise from aircraft or from neighbourhood on cognitive learning and electrophysiological stress responses. International Journal of Hygiene and Environmental Health, 215(6), 547–554. https://doi.org/10.1016/j.ijheh.2011.12.007
- Tzivian, L., Winkler, A., Dlugaj, M., Schikowski, T., Vossoughi, M., Fuks, K., & Hoffmann, B. (2015). Effect of long-term outdoor air pollution and noise on cognitive and psychological functions in adults. International Journal of Hygiene and Environmental Health, 218(1), 1–11. https://doi.org/10.1016/j.ijheh.2014.08.002
- van Kamp, I., & Davies, H. (2013). Noise and health in vulnerable groups: A review. Noise & Health, 15(64), 153–159. https://doi.org/10.4103/1463-1741.112361
- van Kamp, I., Job, R. F. S., Hatfield, J., Haines, M., Stellato, R. K., & Stansfeld, S. A. (2004). The role of noise sensitivity in the noise-response relation: A comparison of three international airport studies. Journal of the Acoustical Society of America, 116(6), 3471–3479. https://doi.org/10.1121/1.1810291
- van Kempen, E., Casas, M., Pershagen, G., & Foraster, M. (2018). WHO environmental noise guidelines for the European region: A systematic review on environmental noise and cardiovascular and metabolic effects: A summary. International Journal of Environmental Research and Public Health, 15(2), 379. https://doi.org/10.3390/ijerph15020379
- Verbeek, T. (2019). Unequal residential exposure to air pollution and noise: A geospatial environmental justice analysis for Ghent, Belgium. SSM – Population Health, 7, 100340. https://doi.org/10.1016/j.ssmph.2018.100340
- Vienneau, D., Saucy, A., Roosli, M., Vienneau, D., Saucy, A., Schäffer, B., & Röösli, M. (2022). Transportation noise exposure and cardiovascular mortality: 15-years of follow-up in a nationwide prospective cohort in Switzerland. Environment International, 158, 106974. https://doi.org/10.1016/j.envint.2021.106974
- Vienneau, D., Schindler, C., Perez, L., Probst-Hensch, N., & Röösli, M. (2015). The relationship between transportation noise exposure and ischemic heart disease: A meta-analysis. Environmental Research, 138, 372–380. https://doi.org/10.1016/j.envres.2015.02.023
- Wagner, J., Cik, M., Marth, E., Santner, B. I., Gallasch, E., Lackner, A., & Raggam, R. B. (2010). Feasibility of testing three salivary stress biomarkers in relation to naturalistic traffic noise exposure. International Journal of Hygiene and Environmental Health, 213(2), 153–155. https://doi.org/10.1016/j.ijheh.2009.08.004
- Wang, T.-C., Chang, T.-Y., Tyler, R. S., Hwang, B.-F., Chen, Y.-H., Wu, C.-M., & Tsai, M.-H. (2021). Association between exposure to road traffic noise and hearing impairment: A case-control study. Journal of Environmental Health Science and Engineering, https://link.gale.com/apps/doc/A672343762/AONE?u=learn&sid=bookmark-AONE&xid=3d19707d
- Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., & Heald, J. L. (2015). Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: Methodology and discussion. Sleep, 38(8), 1161–1183, Article PII sp-00367-15. https://doi.org/10.5665/sleep.4886
- Weidenfeld, S., Sanok, S., Fimmers, R., Puth, M. T., Aeschbach, D., & Elmenhorst, E. M. (2021). Short-term annoyance due to night-time road, railway, and air traffic noise: Role of the noise source, the acoustical metric, and non-acoustical factors. International Journal of Environmental Research and Public Health, 18(9), 4647. https://doi.org/10.3390/ijerph18094647
- Welch, D., Dirks, K. N., Shepherd, D., & McBride, D. (2018). Health-related quality of life is impacted by proximity to an airport in noise-sensitive people. Noise & Health, 20(96), 171–177. https://doi.org/10.4103/nah.NAH_62_17
- Welch, D., Dirks, K. N., Shepherd, D., & Ong, J. (2022). What is noise sensitivity? Noise & Health, 24(114), 158–165. https://doi.org/10.4103/nah.nah_56_21
- Welch, D., Shepherd, D., Dirks, K. N., McBride, D., & Marsh, S. (2013). Road traffic noise and health-related quality of life: A cross-sectional study. Noise and Health, 15(65), 224–230. https://doi.org/10.4103/1463-1741.113513
- Weyde, K. V., Krog, N. H., Oftedal, B., Evandt, J., Magnus, P., Overland, S., & Aasvang, G. M. (2017). Nocturnal road traffic noise exposure and children’s sleep duration and sleep problems. International Journal of Environmental Research and Public Health, 14(5), 491. https://doi.org/10.3390/ijerph14050491
- WHO Environmental noise guidelines for the European region. (2017). https://www.mdpi.com/journal/ijerph/special_issues/WHO_reviews
- Win, K. N., Balalla, N. B. P., Lwin, M. Z., & Lai, A. (2015). Noise-induced hearing loss in the police force. Safety and Health at Work, 6(2), 134–138. https://doi.org/10.1016/j.shaw.2015.01.002
- Woodcock, J., Sica, G., Peris, E., Sharp, C., Moorhouse, A. T., & Waddington, D. C. (2016). Quantification of the effects of audible rattle and source type on the human response to environmental vibration. Journal of the Acoustical Society of America, 139(3), 1225–1234. https://doi.org/10.1121/1.4944563
- World Health Organization. (2014). Burden of disease from ambient air pollution for 2012 (Glob. Health Obs. Data, Issue).
- World Health Organization. (2018). WHO environmental noise guidelines for the European region.
- Yokoshima, S., Morinaga, M., Tsujimura, S., Shimoyama, K., & Morihara, T. (2021). Representative exposure-annoyance relationships due to transportation noises in Japan. International Journal of Environmental Research and Public Health, 18(20), 10935. https://doi.org/10.3390/ijerph182010935