ABSTRACT
Health self-management technology has the potential to significantly improve the Quality of Life of patients suffering from chronic diseases. However, designing the technology involves numerous highly context-dependent design decisions. In this paper, we analyse a case study of self-monitoring technology in the field of congestive heart failure. We analyse the design process of the technology from the perspective of design trade-offs. Three important trade-offs related to health self-monitoring technology are described in detail, related to patient autonomy, technology appropriation, and patient well-being. For each of the trade-offs, various mediating factors that influence design decisions are described in detail. On a practical level, this analysis can inform future developments in self-management technology. In addition, this design trade-off analysis provides intermediary knowledge that can contribute to a better theoretical understanding of health self-management technology.
1. Introduction: design trade-offs for quality of life
As people’s life expectancy raises due to evolutions in health care, side effects of an aging population become increasingly visible. These side effects include a significant rise in the prevalence of chronic diseases, and, associated with this, a significant rise in healthcare costs (Brennan et al. Citation2017). This makes the prevention and management of chronic diseases one of the important challenges in contemporary healthcare.
For both prevention and management of chronic diseases, a healthy lifestyle is required. Beyond maintaining a healthy lifestyle, patients often need to adhere to a complex therapeutic regimen. For example, in order to stay as healthy as possible, patients are stimulated to engage in physical activity, need to take specific dietary advice into account, and are required to take several types of medication at specific times. Not adhering to medication intake or dietary restrictions might worsen the patient’s health.
Technology can be used to support people in maintaining such a healthy lifestyle and improving their health. For instance, it can facilitate health self-management by providing people with data about their (health) behaviour, and by giving them personalised feedback (Nunes et al. Citation2015). Specifically, technology-enhanced self-management is an attractive approach for patient empowerment (Nunes et al. Citation2015), as this allows patients to take control of their disease, and hospitals to reduce costs as patients become less dependent on caregivers (Swan Citation2009). As such, self-management is not only interesting for caregivers, but beneficial for patients, as it can contribute significantly to their quality of life (Ramachandran et al. Citation2007).
Chronic disease has been shown to adversely affect patients’ Quality of Life (Megari Citation2013): their ‘perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns’ (World Health Organisation Citation1996). As patients with chronic conditions need to manage their condition on a day-to-day basis (Schulman-Green et al. Citation2012), self-management technology can influence Quality of Life (QoL) in important ways (Ramachandran et al. Citation2007). First, there is the medical impact: if self-management technology succeeds in helping patients manage their disease in a better way, this can have significant short-term health benefits (Barlow et al., Citation2002). Second, the way in which health management is supported and facilitated can have an important impact on the patients’ well-being more generally, making people feel less anxious, more responsible and in control of their lives.
From a design perspective, Fisher states that ‘to understand, foster, nurture, and support QoL is one of the most challenging design problems of the digital age (Fischer Citation2018a, 27). QoL, as a broad objective to be achieved through design, is an intricate, often highly context-dependent problem with no optimal solutions: a solution in one specific situation might not work in another situation. Therefore, design trade-offs are an important, unavoidable part of design for QoL (Fischer Citation2018a): design decisions that are made on a continuum of possibilities (Fischer Citation2018b), rather than a dichotomous choice. The design process of technology for the improvement of QoL typically consists of numerous trade-offs, and therefore, they are an important topic that needs to be investigated further.
In this paper, we investigate a specific case study in self-management technology. The case study we describe is HeartMan, a H2020 project developing a self-management system for patients with chronic heart failure, a disease that renders patients unable to be physically active. We select a subset of important design trade-offs that were made during the design of the technology, and investigate various aspects in detail: why the trade-off is important, which aspects were relevant in making design decisions, etc. By making choices and trade-offs in the development of health self-management technology explicit, we can both inform future developments in self-management technology by offering insight in important design decisions, and contribute to the theoretical understanding of self-management technology.
2. Related work
2.1. Self-care and self-management technology
The relationship between self-care and self-management is not always clear (Richard and Shea Citation2011). As we will show below, Human–Computer Interaction (HCI) literature often uses the term ‘self-care’ (e.g. Fitzpatrick and Ellingsen Citation2013; Nunes et al. Citation2015). However, ‘self-care’, and a number of related concepts such as ‘self-management’ and ‘self-monitoring’ are often used synonymously. To achieve conceptual clarity, these concepts have been investigated by Richard and Shea (Citation2011): we base our choice to use the term ‘self-management’ in the remainder of this paper on the definitions by Richard and Shea. They define ‘self-care’ as ‘the ability to care for oneself and the performance of activities necessary to achieve, maintain, or promote optimal health (including activities specific to acute and chronic health conditions)’ (Richard and Shea Citation2011, 261). This is a ‘broad concept subsuming self-management, self-monitoring, and symptom management when performed by [the patient him- or her-]self’ (Richard and Shea, 261). Self-management, on the other hand, is defined as ‘the ability of the [patient], in conjunction with family, community, and healthcare professionals, to manage symptoms, treatments, lifestyle changes, and psychosocial, cultural, and spiritual consequences of health conditions (particularly chronic diseases)’ (Richard and Shea, 261). This ‘incorporates self-monitoring and symptom management, but broader in that it addresses the management of emotional/psychosocial, functional, and physical/comfort ramifications of a disease’ (Richard and Shea, 261).
Many studies in HCI literature use the broader term ‘self-care’ to discuss and investigate self-management technologies from various perspectives. For instance, Fitzpatrick and Ellingsen (Citation2013), in their review of CSCW (Computer-Supported Co-operative Work) literature on healthcare technology, discuss ‘self-care’, related to telecare and telemonitoring, as one of the directions in which healthcare is expanding. Care is increasingly moving into the patients’ homes, ‘with decreasing levels of professional involvement’ (Citation2013, 637). On the level of practical design work, Fitzpatrick and Ellingsen’s review covers both design explorations as well as applications and devices that have been developed.
For Nunes et al. (Citation2015), one of the defining characteristics of self-care technology is ‘not to learn facts about a condition, but to influence its course through practical everyday actions, maintaining a satisfactory quality of life for as long as possible’ (Citation2015, 2). The authors have focused on technology in use in their review of self-care technologies. Based on their review of self-care technologies in use, they identified six tensions that ‘foreground critical issues of designing for the self-care setting’ (Citation2015, 3), and a number of key opportunities for advancing research in self-care technologies. In this paper, we will frame tensions similar to those identified by Nunes et al. as ‘design trade-offs’, and analyse them from this perspective.
2.2. Design trade-offs
A trade-off can be defined as ‘a situation in which you balance two opposing situations or qualities’ (Cambridge dictionary, Citation2018). With a history going back to the 1980s (Fischer Citation1987), the concept of design trade-offs is not new in HCI. The concept of design trade-offs has recently gained new interest, specifically in relation to QoL (Fischer Citation2018a). Fischer argues that especially ‘wicked’ design spaces related to Quality of Life are suitable to be explored through the lens of design trade-offs, (Citation2018a, 28), as they typically involve several trade-offs that have different implications in terms of impact on people’s lives. Indeed, QoL-related design is often characterised by ‘wicked problems’ (Rittel and Webber Citation1973): problems that ‘have no definitive formulation, no stopping rule, and no boundaries’ (Fischer Citation2018a, 28). Formulating solutions to these wicked problems involve design trade-offs: ‘situation[s] that involves losing one quality or aspect of something in return for gaining another quality or aspect’ (Fischer Citation2018a, 28–29). An analysis of design trade-offs, therefore, can be a tool to analyse and understand complex design spaces, ultimately widening the design space (Fischer Citation2018a, 30) by looking beyond the surface level of wicked problems, and exposing the truly limiting factors that underlie a trade-off.
In the design of self-management technology, several authors have already described such design trade-offs, such as the self-management trade-off between designing for patient autonomy on the one hand and designing for increased physician control on the other hand (see, e.g. Nunes and Fitzpatrick Citation2017). We build on this work, based on a specific case study of a CHF self-management technology. As such, the contribution of this paper is situated especially in the use of Fischer’s view on design trade-offs for QoL to offer a more detailed exploration, analysis and grounding of these trade-offs. We offer a practical, contextualised account of how specific trade-offs manifest themselves in practice, and which mediating factors need to be considered in order to make appropriate design decisions. As such, we aim to (see also Fischer Citation2018a):
Highlight important facets of the complex problem of self-management, and show how they played a role in the HeartMan system trade-offs.
Identify the underlying limiting factors related to these trade-offs. Some trade-offs are mediated by contextual elements that might not be relevant to the trade-offs, at first sight. We show how such mediating factors can and do play a role in specific design decisions.
Provide evidence that there are no ‘decontextualized sweet spots’ (Fischer Citation2018a, 27): there are no context-independent right or wrong answers for the design of self-management technology. We show how specific contextual factors in the project have influenced design decisions in the project.
3. Case study: [HeartMan]
3.1. In general
The specific case study we describe is HeartMan, a H2020 project developing a self-management system for patients with chronic heart failure (CHF). CHF is a disease that renders patients unable to be physically active. It is characterised by the fact that the heart cannot pump enough blood to supply the body with sufficient oxygen and nutrients. In most developed countries, 1–2% of the population suffers from CHF (Cook et al. Citation2014). While the disease cannot be cured, it usually deteriorates over time. Therefore, treatment is mostly focused on mitigating the symptoms.
HeartMan was conceptualised as a self-management system: by providing people with data about their (health) behaviour, and by giving them personalised feedback, HeartMan allows patients to prevent the disease and its symptoms from getting worse. The system uses a decision support system based on predictive computer models, in order to personalise the advice and interventions to each individual patient. Tailored lifestyle modifications, based on evidence-based predictive models, aim to improve the patients’ health and QoL.
The HeartMan system consists of a mobile application () connected to a wristband () measuring the patients’ vital functions, including heart rate monitoring and variability, activity monitoring, galvanic skin response and skin temperature. This information about the patients’ health and activity is processed by mathematical models that are able to predict when the patient’s health or wellbeing is likely to get worse. When such conditions are detected, the system will suggest actions the patient can take in order to prevent such worsening.
Figure 1. The HeartMan mobile self-monitoring application home screen, with sections on physical activity, nutrition, medication, and mental support.

In addition to the measurement of vital functions and the predictive technology, cognitive behavioural therapy is used to help patients change life-long habits, such as changing dietary habits, or (a lack of) physical activity. Patients are psychologically profiled and monitored to recognise the cognitive dissonance between the desire to be healthy on one hand, and the reluctance to adopt a healthy lifestyle on the other hand. This profiling allows for personalised interventions that exploit the dissonance to achieve behaviour change. Furthermore, mindfulness exercises (mental exercises and simple practical exercises) are expected to make the patients more receptive to the interventions, as well as improve their mood and symptoms. The combination of tracking health data, predictive modelling of the patients’ health, and cognitive behavioural therapy makes the HeartMan system a technology that allows for self-monitoring of various therapeutic aspects.
3.2. Human-centered design in [HeartMan]
In order to design self-management technology that is accepted by the patients and that has the desired effects, an extensive human-centered design process was implemented, in which the HeartMan technology was designed and evaluated. In order to investigate the users’ everyday lives and their specific needs relating to their illness, two studies were carried out with Belgian and Italian heart patients. All patients in the studies were recruited directly via the hospitals that took part in the clinical trial. The first study was a diary study, in which patients kept a diary for a period of 10–14 days (n = 19 in Belgium, n = 18 in Italy). The diary contained questions and assignments that relate to everyday activities and habits, such as the patients’ experience, disease management, and their social network (see also Appendix A). The second study was a follow-up interview study (see also Appendix B), conducted with the majority of the patients who participated in the diary study (n = 14 in Belgium, n = 15 in Italy). In this interview study, patients participated in semi-structured interviews in which the output of the diary study was discussed in more detail. The interviews lasted approx. one hour, and were conducted at their homes. These diaries and interviews were coded and analysed by two researchers.
Based on the diary studies, interviews, and input from the technical partners, initial designs of the HeartMan application were made. These designs were iteratively tested and refined in three iterations of user testing, with increasingly realistic and interactive mock-ups and prototypes. Eventually, the resulting system was evaluated in a four-month clinical trial (minimum system use of twelve weeks), in which 39 CHF patients participated in Belgium (23 patients in the intervention group), and 30 in Italy (15 patients in the intervention group).
Ethical approval for activities in the user-centered design trajectory, and for the clinical trial of the HeartMan system was given by the ethical boards of all three Belgian hospitals involved: OLVZ Aalst, AZ Maria Middelares, and Ghent University Hospital. In Italy, ethical approval was obtained at Comitato Etico Lazio 1.
4. Method
So far, there is no agreed-upon, structured analytic method available for the description of design trade-offs, or the generation of ‘intermediary knowledge’ that bridges practice and theory. For the analysis presented below, we draw upon different related sources: we were inspired by Höök and Löwgren’s (Citation2012) description of how strong concepts can be constructed, and Dalsgaard and Dindler’s (Citation2014) description of how bridging concepts can be constructed by drawing upon theory as well as practice.
Based on these sources, we used a combination of literature review and a review of practical design decisions in the HeartMan project:
We draw upon the HCI literature in self-management technology, listing the important themes and tensions that are described. We focused on recently published (2009–2019) review articles on health self-management technology in the main HCI venues (major conferences such as ACM CHI, NordiCHI, PervasiveHealth and journals such as ACM TOCHI, CSCW, International Journal of Human–Computer Studies, Behaviour and Information Technology) in order to focus on recurrent themes. Starting from these articles, we broadened our scope to include descriptions of specific systems, to learn about specific, case-specific tensions and trade-offs.
We draw upon project knowledge, trade-offs and decisions within the HeartMan consortium, including, but not limited to, the human-centered design trajectory. We reviewed recommendations resulting from the human-centered process, and we compared them to the design decisions that were eventually made in the project (based on project consortium meeting minutes). In this comparison, it was crucial to consider other factors (contextual, administrative, technical, etc.) that influenced these design decisions.
We matched the themes in HCI literature (step 1) with the project knowledge, trade-offs and decisions (step 2). In an iterative process, going back and forth between literature and case study, we identified several trade-offs, of which three main trade-off categories are described below.
This results in a fine-grained analysis of three prevalent trade-offs in health self-management technology. Based on the HeartMan case study, we analyse these themes, providing detailed insight in different aspects that are interrelated with the trade-offs, and how these aspects influence these trade-offs.
Based on the interplay between literature, theory and applied case study described above, we:
Provide insight in a concrete case study that can add to the state of the art in the literature on self-management technology;
Present a detailed analysis of three categories of important trade-offs in self-management technology. We first summarise the relevant literature on the specific trade-off. Afterwards, we add the perspective of the HeartMan project, and discuss the novel perspective it brings on the trade-off. This analysis can offer new insights in the field, widen the self-management technology design space (Fischer Citation2018a), and, ultimately, guide future developments of self-management technology.
5. Design trade-offs
5.1. Patient autonomy versus external control
5.1.1. In literature
A central concept to the development of self-management applications such as the HeartMan system, is patient empowerment. Several aspects of patient empowerment have already been discussed in the literature, including more theoretical discussions (e.g. Skinstad and Farshchian Citation2016), and more practical descriptions of systems that facilitate patient empowerment (e.g. Storni Citation2014). Nunes et al. (Citation2015), in their review of self-care technologies in HCI discuss several ‘design-related tensions’, the first of which relates to the conceptualisation of self-management.
Nunes et al. acknowledge that in the trade-off between patient autonomy and external control, ‘there does not seem to be an ideal solution, but rather different approaches with distinct requirements and outcomes. Understanding these two, sometimes opposite, poles of a spectrum has important implications for design’ (Citation2015, 28). The authors discuss several mediating aspects specifically related to this continuum, including health literacy (gaining a better understanding about their condition’s characteristics and management), and the importance of specific care decisions (smaller decisions can be left to the patient, while more important ones should be taken by the clinician). More generally, Nunes et al. advise to provide patients with the most autonomy possible, as this ‘should be preferred over over-monitoring and over-controlling’ (Citation2015, 28).
5.1.2. Control and autonomy: the system as a third agent
We argue that the trade-off between patient autonomy and external control goes beyond the relationship between formal and informal caregivers (Grönvall and Verdezoto Citation2013; Berry, Lim et al. Citation2017) on the one hand, and patients on the other. Moving even beyond human caregivers, advances in technology have added a technological factor to this trade-off. Systems such as the HeartMan system are able to adapt to the patient’s changing condition, and can offer tailored advice based on machine learning algorithms. The system’s potential autonomy in creating therapeutic advice creates a new situation in which the trade-off becomes one between autonomy on the part of the patient, the system, and the doctor.
New aspects of the autonomy trade-off become apparent, including the reliability of automatically generated advice: reliability and trust become important factors. The HeartMan interview study already showed that interpersonal trust plays an important role in the relationship between physician and patient. Half of the interview participants reported initial trust issues, due to, for instance, faulty diagnoses, contradictory advice, and a lack of transparency (see also quote below). Preliminary results from the HeartMan clinical trial point to similar issues in the patients’ relationship with the technology: when self-management technology malfunctions, or shows information or advice which contradicts the patients’ experiences, the patients’ trust in the technology will diminish. Therefore, factors such as the system’s accuracy, and its transparency towards patients are crucially important in the ‘patient autonomy vs. external control’ trade-off.
Yes, that [medication] is changed regularly, but I especially regret that the different specialists don’t, or hardly communicate. They don’t discuss with the cardiologists or the diabetes specialists. Nobody discusses with each other but they keep adding medication.
5.1.3. Mediating factor: patient characteristics
In addition to the patients’ health literacy, we have identified several patient characteristics as important additional factors in the trade-off between autonomy and control. While Nunes et al. (Citation2015) mention ‘the personality of the patient’ as an additional factor, there are several related factors.
The patients’ digital literacy is an important mediating factor in offering autonomy. In HeartMan, we considered this as an important factor in the ability of a patient to engage with self-management technology. While some patients are confident technology users in their everyday lives, others received their first smartphone during the intake visits of the HeartMan clinical trial. Among the diary study respondents, only one-third of the CHF patients used a smartphone before the clinical trial. This variability in terms of digital literacy has a number of implications.
During the HeartMan trial, a distinction was made between patients with high and low digital literacy. The patients with high literacy received a full explanation about the HeartMan technology, and its functionalities. These more proactive users were encouraged to navigate through the various functions of the app themselves, and explore the details of the HeartMan app. The patients with lower digital literacy were asked to primarily react to notifications (on nutrition, mental support, medication, and physical activity) in the app.
We consider this segmentation in proactive and reactive users as a basic personalisation of technology usage. While the HeartMan technology is personalised based on each patient’s individual health condition, the app does not provide personalisation of the functionality itself. Given the variation in digital literacy, distinguishing between proactive and reactive use provides a basic distinction in how deeply the patients engage with the technology.
A second important patient characteristic that influences the trade-off between patient autonomy and doctor control, is the patient’s existing perception of patient empowerment, and the division of work between patient and doctor (see also Fitzpatrick and Ellingsen Citation2013; Skinstad and Farshchian Citation2016). As most patients are used to a more traditional relation with their doctor (who is in control of the disease management), it can be difficult for them to understand that through technology, this division of work can change, offering them more autonomy. As Andreassen and Trondsen (Citation2010, 282) state: ‘patients tend to behave passively and expect the doctor to take control.’
In the HeartMan system, the primary goal is self-management of CHF. However, as a secondary benefit, relevant patient data (heart rate, blood pressure) is also sent to the hospital, to allow clinicians to fine-tune the patients’ treatment. In presenting the HeartMan system to patients, self-management was clearly stressed as the primary goal of the system, but mentioning data sharing with hospitals as a secondary goal had an important effect. For some patients and their informal caregivers, the perceived benefit of the HeartMan app was primarily the data sharing with the hospital (see also the interview quote below). As such, these patients understood the HeartMan system foremost as a remote monitoring app, instead of a self-management app. For these patients, the main goal was reassurance: data sharing with the hospital meant that they would be tracked closely.
While the HeartMan system intended to empower patients, patients’ existing attitudes and perception of the system emphasise their dependence on the doctor’s expertise (Derboven Citation2018), confirming them in their passive role. This observation creates a new challenge for self-management technology, which can be framed as a trade-off related to the question whether all empowering all patients should be the ultimate goal of self-management technology.
If someone would monitor and would be able to take action immediately. Something like that would be interesting. … It would be interesting in case something would happen to you, that someone would be able to take action right away. If you fall in the street and nobody passes by, then you're just lying there, you know what I mean.
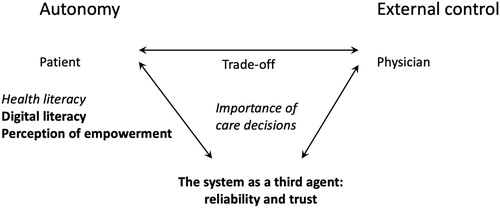
5.1.4. Patient autonomy versus external control: summary
The discussion of the trade-off between patient autonomy and external control has been summarised in . In the trade-off, we have identified two mediating factors that mediated the design decisions made in the HeartMan project. On the one hand, digital literacy is an important factor which can have an important influence on the extent to which patients can take responsibility and control. On the other hand, the patient’s perception of, and position on empowerment is important in the changing relation between physician and patient. Beyond patient and physician, we have identified the system itself as a potential third agent in control, as self-management apps will become able to automatically generate personalised advice.
5.2. Appropriation versus closing technology to change
5.2.1. In literature
People who use technology in their daily lives often start using it on their own terms, reinterpreting and appropriating it. This adoption process in which people reinterpret the technology they use has been called ‘appropriation’ (e.g. Dourish Citation2003), and has been analysed from a variety of angles, including cognitive science, design, and the social sciences (Derboven Citation2017). From a design perspective, Dix (Citation2007) has argued that in its design, technology can allow for, or prevent appropriation. When technology allows for appropriation, it is ‘open’ to change, whereas when it prevents appropriation, it is ‘closed’ to change (see also Nunes et al. Citation2015).
Related to health applications, Nunes et al. point to the fine line between allowing patients to appropriate technology by adapting it to their own life and habits on the one hand, and safety concerns related to not using health-care technology as it was intended by the designer (Citation2015, 29). While everyday health technologies can be appropriated and domesticated without important safety concerns (see, e.g. Carter, Green, Thorogood Citation2013), the situation can be different for chronic disease management. For instance, Storni (Citation2010) describes a situation in which a blood pressure monitor is appropriated by a patient in a highly problematic way. Nunes et al. (Citation2015) suggest a trade-off: even though safety concerns are crucial in healthcare settings, allowing for some flexibility might be necessary, for instance to address different cases of the same condition, or to address different patients’ needs. In other words: patient-specific needs and preferences call for malleable self-management technology that considers ‘the psychological fit between users and interactive systems’ (Cabitza and Simone, Citation2017).
5.2.2. Prior patient habits as a mediating factor: flexible adherence and flexible technology use
From the perspective of a medical treatment, it might seem relevant to medical professionals to prevent appropriation in technology related to therapy adherence and disease self-management as much as possible. In the end, the stricter patients adhere to their therapy, the better the results from the treatment will be. However, this does not consider the patients’ prior habits related to their treatment.
Patients with chronic diseases build specific habits related to their treatment, and to managing their disease. User research in the HeartMan project showed that patients adapt and adjust doctor’s advice to make it practically applicable in everyday life: while some advice is followed to the letter, patients reported that other advice can be very difficult to adhere to. We call this practice, which was reported by the majority of the patients in the HeartMan interviews, ‘flexible adherence’. This flexible adherence ranges from changes in the advised time to take specific medicines (e.g. to prevent stomach aches at night) to deviations from dietary restrictions (see also the interview quote below). As such, flexible adherence is related to appropriation and personalisation: when patients choose to deviate from the advice offered by the technology, the technology could support them in this. Repeating over and over again the same advice the patient has chosen not to adhere to, can be very demotivating. To cope with this flexible adherence, technology could consider the patient’s preferences, and avoid demotivating repetition of advice that is not relevant or not feasible for a specific patient. As the majority of the patients in the HeartMan study reported some form of flexible adherence, there was a clear patient need for support in making these choices related to flexible adherence, advising patients to what extent they can treat advice in a flexible way, and when it is a bad idea to deviate from the prescribed therapy. However, the clinical trial setting (see also the next paragraph on the test setting as a mediating factor), made it difficult to include this type of flexibility in the HeartMan application.
And can you always adhere to the advice to restrict your fluid intake?
R2: It’s difficult.
And what makes it difficult for you?
I say: when you are thirsty, you have to drink … Yes, that is … I am also a diabetic. I have a dry mouth sometimes; then I will drink something.
5.2.3. The test setting as a mediating factor: appropriation and clinical trials
While in literature, evaluation of technology and clinical trials are not often related to appropriation (see, e.g. Nunes et al. Citation2015), a clinical trial can have important consequences for the technology in terms of appropriation. In a clinical trial, the technology is validated by investigating the health effects of this specific technology in a group of patients. In order to accurately measure these effects in the HeartMan trial, the trial participants all received the same technology, and the same self-management functionality offering personalised medical advice tailored to the patient’s individual health status. However, while the HeartMan system is personalised based on the patients’ medical background, other factors were not considered in this personalisation: every patient was offered the same functionality. In the clinical trial setting, the goal was to compare health outcomes in an intervention group of patients that used the HeartMan system, and a control group of patients that received standard care. Allowing for appropriation and personalisation would have important consequences for the trial setting, as the intervention group would no longer be homogeneous: patients would all use slightly different, personalised versions of the technology. Such personalised versions of the technology would imply that much larger patient groups are needed to conduct a valid trial.
Technology appropriation could be beneficial for patients suffering from chronic diseases, for instance in terms of their digital literacy. As mentioned before, patients in the HeartMan trial received somewhat different instructions based on their digital literacy. This approach, however, has some risk associated with it: a potential consequence of this approach is that the results of evaluating self-management technology in a clinical trial are influenced by the patients’ skills in using the technology. As a result, rather than strictly measuring the effectiveness of the therapeutic advice in itself, part of the variation in the clinical effect measured by a trial could be attributed to the variation in patients’ digital literacy (full use versus limited use).
A self-monitoring application allowing for appropriation could allow for richer nuances in the spectrum between full use and partial use. In other words, whereas an application closed to change leads to a more radical difference between use (for patients with high digital literacy) and partial non-use (for patients with low digital literacy), an application open to appropriation can allow all patients to engage in the self-management functionality in a more personalised way.
In sum, both validation in a clinical trial (as a part of the development process, and often a requirement to be able to bring a medical technology to the market) and user appropriation have distinct, different benefits, which are not always compatible, for the reasons outlined above. This suggests that for the design trade-off between design for appropriation and closing technology to change, the validation strategy can be an important mediating factor.
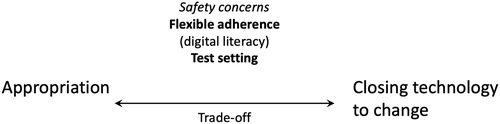
5.2.4. Appropriation versus closing technology to change: summary
The discussion of the trade-off between appropriation and closing technology to change has been summarised in . In the trade-off, we have identified two external factors that mediated the design decisions made in the HeartMan project. On the one hand, patients’ existing habits and flexible adherence are important factors. In this respect, technology that allows for appropriation can allow patients to personalise the technology to their specific situation and preferences. On the other hand, the external factor of clinical trial evaluation has an important impact on how appropriation can be approached in a specific technology.
5.3. Orientation: a medical versus a more holistic well-being approach
Self-management apps hold the promise of several healthcare benefits, including improving treatment adherence, early detection of medical complications, etc. (McCurdie et al. Citation2012). However, while self-management apps should efficiently provide information and encourage users to achieve goals, the constant access to detailed health data can also become overwhelming and induce additional stress and anxiety (Derboven et al. Citation2018). This observation introduces the design trade-off between a strictly medical focus, and a more holistic, well-being-oriented approach.
5.3.1. In literature
Well-being is increasingly being addressed in the HCI community. Several workshops dealing with this topic have been organised, focusing on ‘Interaction Design and Emotional Wellbeing’ (Coyle et al. Citation2012) and ‘Mobile wellbeing’ (Rost et al., Citation2016). Academic work specifically addressing the design trade-off in health technology between a medical vs. a more holistic well-being approach has been scarcer (Derboven et al. Citation2018). However, as Derboven, Voorend et al. state, attention for combination of health self-management and mental support is growing, and it poses particular challenges. While access to personal health data can be overwhelming and stress-inducing (Vandenberghe et al. Citation2018), a well-being approach aims to reduce stress by inviting patients to ‘attentively liv[e] in the moment’ (Zhu et al., Citation2016).
5.3.2. Disease complexity and literacy as a mediating factor: health data, well-being and anxiety
The patients’ ability to understand personal health data is an important factor self-care. This ability is a combination of the nature of the patients’ conditions, and their health literacy: their ability to understand and interpret information related to their condition. When health literacy is low in a traditional doctor-patient relationship, communication between health care professionals and the patient is hampered, and optimal care cannot be achieved (Evangelista et al. Citation2010, 9). Moreover, poor health literacy leads to poor self-care, and poorer physical and mental health (Evangelista et al. Citation2010, 11). For CHF patients, adequate health literacy has been associated with a better understanding of medication and lifestyle modifications. In addition, it has been shown that good health literacy leads to a better understanding of which symptoms may be caused by the disease, and how to respond appropriately to the symptoms (Magnani et al. Citation2018).
Health literacy is often referred to in the context of patient autonomy. In this context, Nunes et al. (Citation2015) state that disease literacy can grow over time: ‘as patients live longer with the condition, they start gaining a better understanding about its characteristics and management, and so they start taking on further responsibilities and control from their clinicians’ (28). Patients with lower health literacy, however, might feel overwhelmed by health data, and feel disempowered and anxious, as they have difficulties in interpreting data, symptoms and responding to it (see also the quote below). This anxiety can be increased by comorbidities: for some patients in the HeartMan study, these co-morbidities could have overlapping symptoms, and contradictory treatment advice.
I was afraid because when I'm not feeling well, sometimes I … . No, it won't start again will it? I've had it once, when I had that mild heart attack a few years ago, I went to sleep and felt that something wasn't right. It all felt too familiar, just like when I had my first heart attack. Yes, my wife was pretty worried too then.
5.3.3. Prior patient habits as a mediating factor: flexible adherence, reassurance and responsibility
In the section on ‘Appropriation versus Closing Technology to Change’, we already discussed how prior patient habits can be important factors in appropriation, and, ultimately, technology acceptance. However, prior patient habits also play an important role on the level of well-being. Supporting patients in a more flexible adherence to the treatment guidelines in a self-management technology can enable patients to transcend the purely medical level, and assist them on a more holistic, well-being level.
This potential for flexible adherence to treatment guidelines points to a related trade-off between reassurance and responsibility. Allowing for flexible adherence can be interpreted as a reassurance strategy: while they can be persuaded to do more, allowing for flexible adherence can reassure patients that they are on the right track. Not allowing for flexible adherence can increase anxiety, as it risks imposing guidelines on patients that are difficult to live up to. In combination with the feeling of being overwhelmed by health data, this can be an important factor. This increase of anxiety is a very real risk: in the recruitment for the HeartMan trial, several patients explicitly mentioned their own well-being and anxiety as a reason not to take part. These patients expected a self-management application would increase their anxiety.
This anxiety is often caused by the patients’ previous experience with important events regarding their condition. In the HeartMan study, almost all participants have gone through one or more major heart failure incidents, which they experienced as very traumatic. These previous traumatic experiences can cause patients to get anxious in general and they are anxious for another episode to happen.
That's why I don't go out much, or go somewhere because it happened a few times that I just fall and that's why I'm more and more afraid to go somewhere. It even keeps me from seeing my son or daughter.
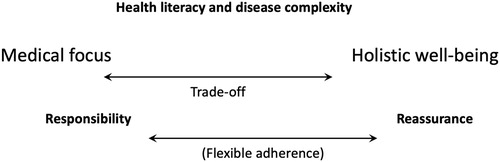
5.3.4. Orientation: a medical versus a more holistic well-being approach – summary
The discussion of the trade-off between a medical versus a more holistic well-being approach has been summarised in . In the trade-off, we have identified two factors that can mediate design decisions. On the one hand, the patients’ health literacy, and the inherent disease complexity is an important factor. Patients tend to become more anxious when their understanding of their condition is lower: therefore, to promote well-being, this understanding is, in itself, an important factor. On the other hand, as in the appropriation trade-off, patients’ existing habits and flexible adherence are important factors to acknowledge. This leads to a related design trade-off between reassurance and responsibility.
6. Discussion
In the previous section, we have focused on three central design trade-offs in the design of health self-management technology (see also for an overview). We have described two existing trade-offs already described in the literature: both the ‘patient autonomy vs. external control’ and the ‘appropriation and personalisation vs. closing technology to change’ trade-offs have already been described in the literature. For these trade-offs, we show how several mediating factors play a role in specific design decisions: as such, we highlight the complexity and richness inherent in the design of self-management technology, and identify important underlying limiting factors that play a role in design decisions (Fischer Citation2018a). In addition, we describe a third important trade-off between a medical versus a more holistic well-being approach. Although this trade-off has not received as much research attention, we believe that this issue will gain more importance in the future, for several reasons. On the one hand, both HCI and healthcare in general increasingly emphasise mental wellbeing as an important focus (Derboven et al. Citation2018). On the other hand, we have discussed how well-being, anxiety and reassurance are also intimately connected to the often-discussed trade-off on patient autonomy.
Table 1. Overview of trade-offs (colour-coded per trade-off), their mediating factors, and more specific project-specific factors that instantiate the mediating factors. Interactions within (dotted lines), and across (full lines) trade-offs are made explicit on the right side of the table.
Taken together, these trade-offs highlight several important facets of complex self-management problems. While not exhaustive, discussing specific project-specific design decisions in terms of trade-offs offers the opportunity to derive more abstract, general design knowledge from local, project-specific issues that are often left underexposed.
6.1. Mediating factors in design trade-offs
In the description of design trade-offs in the previous section, we have identified several ‘mediating factors’ that can steer a design decision in a specific direction. These mediating factors are underlying, often contextual elements that are often not related to the trade-offs at first sight, but that do play a significant role in specific design decisions. As such, these are limiting factors that play an important role in the specific design decisions that are being made. Beyond the specifics of the mediating factors that have been described, we can identify general types of mediating factors.
First, there are user-related mediating factors. This type of mediating factor is, of course, an important focus in human-centered design. Both user characteristics and context are important: in the discussion of HeartMan design trade-offs, user characteristics include digital literacy, whereas the social context of users includes existing social habits in the relationship between physician and patient.
Second, there are mediating factors related to the technology itself. Especially in technological research projects, the technology itself constitutes an important element of the trade-offs, proving that a specific technology works in a safe, reliable way. In the HeartMan study, a technology-related factor was the reliability of automatic, system-generated advice. Assuring the quality system-generated advice lead to questions on how to cope with such advice. Is an additional human validation step necessary, or not? In the HeartMan project, the choice was made to keep automatically-generated advice within very strict safety limits (e.g. keeping the upper threshold for the patient’s heart rate during exercise well within the safe zone), eliminating the need for additional physician validation.
Third, there is a type of mediating factor which is not often made explicit in HCI literature, but not often talked about: these are mediating factors related to the context in which the technology is being developed. These can be circumstances that do impact the design, but are external to the (human-centered) design process itself. In the HeartMan project, we encountered such an external factor in the evaluation setting of the HeartMan technology: the clinical trial setting limited the possibility to create personalised experiences adapted to, for instance, the digital and health literacies of individual patients. While this is a healthcare-specific example, other external factors can have an important influence on design decisions as well: for instance, when the variety of available technologies, or the available budget or time for research projects or development are limiting factors. These limiting factors, then, often precede trade-offs during the design trajectory itself, but they do have important implications for the design of the technology. While these factors are typically underexposed in existing literature, they deserve more research attention, in order to map the design implications of these mediating factors in more detail. If this mapping has brought out the true extent of the consequences on design, designers can think about how these factors can be influenced to minimise the limitations they impose on the design process.
We argue that adding the concept of mediating factors to Fischer’s conceptualisation of design trade-offs is productive, as it allows for additional detail in analysing various, sometimes conflicting, factors that lead a design decision towards one specific side of the design trade-off continuum. Furthermore, we have identified several mediating factors that are important to more than one design trade-off. As such, we add further detail to the design trade-offs, by also clarifying the connections between trade-offs. For instance, we have shown that flexible adherence is not only a crucial factor for appropriation of self-management technology, but it also plays an important role in a more holistic understanding of self-management technology. Taking into account flexible adherence allows self-management to move beyond strictly medical requirements to considering the patient as an individual with specific characteristics and preferences.
By making such mediating factors explicit, we contribute to the construction of intermediary knowledge, facilitating the exchange between theory and practice (Dalsgaard and Dindler Citation2014). Describing specific project trade-offs in detail, and linking them to existing literature in this way can both offer inspiration and guidance for future health self-management projects, and contribute to the development of theoretical understanding in the field.
6.2. Design trade-offs and mediating factors in health self-management
From the perspective of health self-management technology, the description of HeartMan trade-offs adds specific elements to the existing discussion of trade-offs in literature, and highlight specific complexities in the field of health self-management. For instance, in the classic dichotomy between physician control and patient autonomy, we have added the system itself as a third agent. As self-management technology will increasingly use machine learning algorithms to generate personalised device based on the patient’s health condition, patients not only will need to have personal trust in their physicians, but also trust the system’s decisions. As such, factors such as the system’s accuracy in offering advice, and the patient’s trust in the system will become increasingly important in the ‘patient autonomy vs. external control’ trade-off.
In our view on trade-offs, we have taken a broad view, and have looked beyond mediating factors that are inherent in the human-centered design process itself. This results in a view on mediation that includes both patient-related characteristics that can be researched in a human-centered design process, but also factors that are beyond the reach of a human-centered design process. Unsurprisingly, many of the mediating factors related to the human-centered design process have already been researched to some extent in existing literature (Fitzpatrick and Ellingsen Citation2013; Nunes et al. Citation2015). External factors such as the limitations imposed by a clinical trial setting, are in principle external to the design process, even though they can have a large impact on the way technology can be left open for change. The clinical trial factor implies that in a healthcare setting, it is useful to raise awareness about the implications of a clinical trial on the design of technology. While Nunes et al. (Citation2015) mention ‘proving’ vs. ‘improving’ strategies for the evaluation of health self-management technology, it is important to explicitly link this to the design of the technology: a ‘proving’ strategy involving a clinical trial implies that the design needs to take into account the specific evaluation strategy, while an ‘improving’ strategy arguably poses less restrictions on the design of the technology.
7. Limitations and future work
The study presented above has discussed design trade-offs that surfaced during the development of a self-management application. By definition, design trade-offs are highly influenced by contextual factors. As Fisher states: there are no ‘decontextualized sweet spots’ (Citation2018a, 27): there are no context-independent right or wrong answers for the design of self-management technology. This is also the case for this study.
Due to the large role of context in design trade-offs, generalisation of trade-off decisions is difficult. However, in this paper, we have abstracted the specific, context-dependent decisions to a higher level of trade-offs: while project-specific details have been discussed in this article, especially these higher-level trade-offs and mediating factors can be useful for other researchers, and for generalisation to other projects. However, further research, and analyses of design trade-offs are necessary to support our analysis, to broaden the research to other trade-offs, and to provide further details.
Furthermore, the HeartMan project specifically targeted CHF patients. Self-management technology has been developed for various (chronic) illnesses, each with their own specific consequences, and patient profiles. This means that, also from the perspective of the diversity of illnesses to be targeted by self-management technology, further research is needed, distinguishing between trade-offs specific to self-management for a specific illness, and trade-offs related to self-management technology more generally.
8. Conclusion
In this paper, we have analysed specific aspects in the development of a health self-monitoring application from the perspective of design trade-offs for Quality of Life, inspired by Fischer (Citation2018a). Using design trade-offs as a lens to look at the design process in the HeartMan project has allowed us to describe specific trade-offs, and analyse them in depth. This analysis of trade-offs, with the addition of important mediating factors, has proved an interesting lens to uncover factors that play a role in design decisions, and analyse them in detail.
Specifically, we have focused on three important trade-offs: patient autonomy versus external control; appropriation versus closing technology to change; and a medical versus a more holistic well-being approach. We have analysed these trade-offs in detail, in terms of mediating factors. These mediating factors are contextual, technology- and user-specific factors that influence and limit the design space, and as such steer the design decisions that are made. Moreover, we have shown how mediating factors can play a role in several design trade-offs, offering an insight in the various interdependencies between context factors and design decisions.
Overall, this analysis provides a case study of design trade-offs in a specific health self-monitoring case study, and frames the design decisions in the case study in a more general discussion of design trade-offs in healthcare technology. As such, the analysis can both inform future developments in self-management technology on a practical level, and contribute to a better theoretical understanding of health self-management technology.
Acknowledgement
The HeartMan project has received funding from the European Union's Horizon 2020 research and innovation programme, grant agreement No 689660. Project partners are Jožef Stefan Institute, Sapienza University Rome, Ghent University, National Research Council Italy, ATOS Spain, SenLab, KU Leuven, Bittium and European Heart Network.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Jan Derboven http://orcid.org/0000-0003-2168-9719
Roos Voorend http://orcid.org/0000-0002-0812-9285
Karin Slegers http://orcid.org/0000-0003-3368-2282
Additional information
Funding
References
- Andreassen, Hege K., and Marianne Trondsen. 2010. “The Empowered Patient and the Sociologist.” Social Theory & Health 8 (3): 280–287. doi:10.1057/sth.2010.9.
- Barlow, Julie, Chris Wright, Janice Sheasby, Andy Turner, and Jenny Hainsworth. 2002. “Self-management Approaches for People with Chronic Conditions: a Review.” Patient Education and Counselling 48: 177–187. doi: 10.1016/S0738-3991(02)00032-0
- Berry, Andrew B.L., Catherine Lim, Andrea L. Hartzler, Tad Hirsch, Edward H. Wagner, Evette Ludman, James D. Ralston. 2017. “How Values Shape Collaboration Between Patients with Multiple Chronic Conditions and Spousal Caregivers.” Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI '17), 5257–5270. New York: ACM.
- Brennan, Paul, Markus Perola, Gert-Jan van Ommen, and Elio Riboli. 2017. “Chronic Disease Research in Europe and the Need for Integrated Population Cohorts.” European Journal of Epidemiology 32 (9): 741–749. doi:10.1007/s10654-017-0315-2.
- Cabitza, F., and C. Simone. 2017. “Malleability in the Hands of End-Users.” In New Perspectives in End-User Development, edited by F. Paternò, and V. Wulf, 137–164. Cham, CH: Springer.
- Cambridge Dictionary. 2018. “Trade-off.” Accessed 30 October 2018.
- Carter, S., J. Green, and N. Thorogood. 2013. “The Domestication of an Everyday Health Technology: A Case Study of Electric Toothbrushes.” Social Theory & Health 11 (4): 344–367. doi: 10.1057/sth.2013.15
- Cook, C., G. Cole, P. Asaria, R. Jabbour, and D. R. Francis. 2014. “The Annual Global Economic Burden of Heart Failure.” International Journal of Cardiology 171 (3): 368–376. doi: 10.1016/j.ijcard.2013.12.028
- Coyle, David, Conor Linehan, Karen Tang, and Sian Lindley. 2012. “Interaction Design and Emotional Wellbeing.” In CHI '12 Extended Abstracts on Human Factors in Computing Systems (CHI EA '12), 2775–2778.
- Dalsgaard, Peter, and Christian Dindler. 2014. “Between Theory and Practice: Bridging Concepts in HCI Research.” Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI '14), 1635–1644. New York: ACM.
- Derboven, Jan. 2017. “Beyond Designers’ Intentions. A Semiotic Exploration of Technology Interpretation and Appropriation.” PhD diss., University of Leuven.
- Derboven, Jan. 2018. “HeartMan: (Self-)Managing Chronic Heart Failure.” CEUR Workshop Proceedings 2101, 8–14
- Derboven, Jan, Roos Voorend, Gennaro Tartarisco, Flavia Marino, Giovanni Pioggia, Sebastiano Nucera, and Katleen Van der Gucht. 2018. “mhealth and Psycho-physical Well-being.” Proceedings of the 10th Nordic Conference on Human-Computer Interaction (NordiCHI '18), 952–955. New York, ACM.
- Dix, Alan. 2007. “Designing for Appropriation.” Proceedings of the 21st British HCI Group Annual Conference on People and Computers: HCI … But Not As We Know It, Vol. 2, 27–30. Swindon: BCS Learning & Development Ltd. http://dl.acm.org/citation.cfm?id=1531407.1531415
- Dourish, Paul. 2003. “The Appropriation of Interactive Technologies: Some Lessons From Placeless Documents.” Computer Supported Cooperative Work 12 (4): 465–490. doi: 10.1023/A:1026149119426
- Evangelista, Lorraine S., Kismet D. Rasmusson, Ann S. Laramee, Joan Barr, Susan E. Ammon, Sandra Dunbar, Susan Ziesche, J. Herbert Patterson, and Clyde W. Yancy. 2010. Journal of Cardiac Failure 16 (1): 9–16. doi: 10.1016/j.cardfail.2009.10.026
- Fischer, Gerhard. 1987. “Making Computers More Useful and More Usable.” In Cognitive Engineering in the Design of Human-Computer Interaction and Expert Systems, edited by G. Salvendy, 97–104. Amsterdam: Elsevier.
- Fischer, Gerhard. 2018a. “Exploring Design Trade-Offs for Quality of Life in Human-Centered Design.” Interactions 25 (1): 26–33. doi: 10.1145/3170706
- Fischer, Gerhard. 2018b. “Identifying and Exploring Design Trade-Offs in Human-Centered Design.” Proceedings of International Conference on Advanced Visual Interfaces 2018, article 22, 9 pages.
- Fitzpatrick, Geraldine, and Gunnar Ellingsen. 2013. “A Review of 25 Years of CSCW Research in Healthcare: Contributions, Challenges, and Future Agendas.” Computer Supported Cooperative Work 22: 609–665. doi:10.1007/s10606-012-9168-0.
- Grönvall, Erik, and Nervo Verdezoto. 2013. “Beyond Self-Monitoring: Understanding Non-Functional Aspects of Home-Based Healthcare Technology.” Proceedings of the 2013 ACM International Joint Conference on Pervasive and Ubiquitous Computing (Ubicomp '13), 587–596. New York: ACM.
- Höök, Kristina, and Jonas Löwgren. 2012. “Strong Concepts: Intermediate-Level Knowledge in Interaction Design Research.” ACM Transactions on Human-Computer Interaction 19 (3): 23:1–23:18. Article 23. doi: 10.1145/2362364.2362371
- Magnani, Jared W., Mahasin S. Mujahid, Herbert D. Aronow, Crystal W. Cené, Victoria Vaughan Dickson, Edward Havranek, Lewis B. Morgenstern, Michael K. Paasche-Orlow, Amy Pollak, and Joshua Z. Willey. 2018. “Health Literacy and Cardio-Vascular Disease: Fundamental Relevance to Primary and Secondary Prevention.” Circulation 138 (2): e48–e74. doi:10.1161/CIR.0000000000000579.
- McCurdie, T., S. Tavena, M. Casselman, M. Yeung, C. McDaniel, W. Ho, and J. Cafazzo. 2012. “mHealth Consumer Apps: the Case for User-Centered Design.” Biomedical Instrumentation & Technology 46 (s2): 49–56. doi: 10.2345/0899-8205-46.s2.49
- Megari, Kalliopi. 2013. “Quality of Life in Chronic Disease Patients.” Health Psychology Research 1 (3): e27. doi:10.4081/hpr.2013.e27 doi: 10.4081/hpr.2013.932
- Nunes, Francisco, Tariq Andersen, and Geraldine Fitzpatrick. 2017. “The Agency of Patients and Carers in Medical Care and Self-Care Technologies for Interacting with Doctors.” Health Informatics Journal, Available in OnlineFirst. doi:10.1177/1460458217712054.
- Nunes, Francisco, Nervo Verdezoto, Geraldine Fitzpatrick, Morten Kyng, Erik Grönvall, and Cristiano Storni. 2015. “Self-Care Technologies in HCI: Trends, Tensions and Opportunities.” ACM Transactions on Human-Computer Interaction 22 (6): 33:1–33:45. Article 33. doi: 10.1145/2803173
- Ramachandran, K., N. Husain, R. Maikhuri, S. Seth, A. Vij, M. Kumar, N. Srivastava, D. Prabhakaran, B. Airan, and K. Sinath Reddy. 2007. “Impact of a Comprehensive Telephone-Based Disease Management Programme on Quality-of-Life in Patients with Heart Failure.” The National Medical Journal of India 20 (2): 67–73.
- Richard, Angela A., and Kimberly Shea. 2011. “Delineation of Self-Care and Associated Concepts.” Journal of Nursing Scholarship 43 (3): 255–264.
- Rittel, Horst W.J., and Melvin M. Webber. 1973. “Dilemmas in a General Theory of Planning.” Policy Sciences 4 (2): 155–169. doi: 10.1007/BF01405730
- Rost, Mattias, John Rooksby, Alexandra Weilenmann, Thomas Hillman, Pål Dobrin, and Juan Ye. 2016. “Mobile Wellbeing.” Proceedings of the 9th Nordic Conference on Human-Computer Interaction (NordiCHI '16). Article 137, 3 pages.
- Schulman-Green, Dena, Sarah Jaser, Faith Martin, Angelo Alonzo, Margaret Grey, Ruth McCorkle, Nancy S. Redeker, Nancy Reynolds, Robin Whittemore. 2012. “Processes of Self-Management in Chronic Illness.” Journal of Nursing Scholarship 44 (2), 136–144. doi: 10.1111/j.1547-5069.2012.01444.x
- Skinstad, Thor Jarle J., and Babak A. Farshchian. 2016. “Empowerment or Concealed Compliance? A Review of Literature on Mobile ICT Solutions for Patient Empowerment.” Proceedings of the 9th International Conference on Pervasive Technologies Related to Assistive Environments (PETRA '16), Corfu, Greece, June 29–July 1, 2016.
- Storni, Cristiano. 2010. “Multiple Forms of Appropriation in Self-Monitoring Technology: Reflections on the Role of Evaluation in Future Self-Care.” International Journal of Human-Computer Interaction 26 (5): 537–561. doi: 10.1080/10447311003720001
- Storni, Cristiano. 2014. “Design Challenges for Ubiquitous and Personal Computing in Chronic Disease Care and Patient Empowerment: a Case Study Rethinking Diabetes Self-Monitoring.” Personal and Ubiquitous Computing 18 (5): 1277–1290. doi: 10.1007/s00779-013-0707-6
- Swan, Melanie. 2009. “Emerging Patient-Driven Health Care Models: An Examination of Health Social Networks, Consumer Personalized Medicine and Quantified Self-Tracking.” International Journal of Environmental Research and Public Health 6 (2): 492–525. doi: 10.3390/ijerph6020492
- Vandenberghe, Bert, Jasper Vanhoof, Roos Voorend, David Geerts and Fabienne Dobbels. 2018. “The ‘Self’ as Barrier for Self-Management Technologies in Healthcare?” Proceedings of 12th International Conference on Pervasive Computing Technologies for Healthcare. (PervasiveHealth 2018).
- World Health Organisation. 1996. Programme on Mental Health. Geneva: World Health Organisation.
- Zhu, Bin, Anders Hedman, and Haibo Li. 2016. “Design digital mindfulness for personal wellbeing.” Proceedings of the 28th Australian Conference on Computer-Human Interaction (OzCHI '16), 626–627.
Appendices
Appendix A: Diary Study (Sample Questions)
A Day in My Life
Describe an average day as detailed as possible. Pay special attention to anything that is related to your heart condition.
Letter
Juul has recently been diagnosed with the same heart condition as you have. His condition is similar to yours when you were diagnosed. Starting from your own experiences, write a letter of advice to Juul to help him deal with this condition and to be prepared for what's lying ahead of him.
Association
Write down as many words that you associate with your heart condition. This can be positive, neutral and negative words. The words may be related to any aspect of your condition, such as physical aspects, social aspects, emotional aspects, aspects related to daily life, or any other aspect you can think of.
Timeline
In the envelope labelled with ‘Timeline’ you will find a sheet of paper with a timeline printed on it, and some coloured stickers.
Mark the most important events in your life by placing a coloured sticker on the timeline. For each event, briefly write next to the sticker what happened, and what the impact of this event was on your life.
Use blue stickers for events related to your heart condition (this could be events like hospitalisations, changes in medication/therapy, major improvements or deteriorations of your condition, etc.)
Use yellow stickers for important events related to your personal life (e.g. special birthdays, family events, a new hobby, …)
Costs & Benefits
You have probably been given lots of advices by your doctors and by other caregivers (e.g. about exercise, a healthy diet, …). We can imagine that it isn’t always easy to follow these advices.
Write a list of costs and benefits on the decision to seriously follow the doctor’s advices.
Appendix B: Interview Protocol
Introductory questions to build rapport
Let me begin by asking some basic questions. Where are you from? Where did you grew up?
What kind of job do or did you have?
Now you live here in … Have you been living here for very long?
Disease management
How do you keep track of everything related to your disease? Monitoring, administration, planning, … Can you show me how you do that?
To what extent do you feel capable to manage your disease properly?
Which parts of keeping track of your disease do you find easy to do? Which are more difficult? Why?
Are there situations or moments when you find it difficult to keep track of your disease? Why? When is this easier to do for you?
Do emergency situations occur to you sometimes? What kind of situations? What do you do in those situations? Can you tell about the last time such a situation occurred? (or, in case no emergency situations have occurred: What could be an emergency situation related to your disease? What would you do in such a situation?)
Can you describe how your lifestyle changed due to your disease (for each change: was this based on a caregiver's advice, or on your own initiative (why?)?)
Take photos of any object that is relevant to your disease or to keeping track of your disease
What causes the patients’ condition to change? How do they make trade-offs (regarding activities they know will impair their condition)? Do they monitor changes in their condition?
Patient characteristics
What do participants do with the technology mapped? (what, how, when, where, …)
Are participants willing to use new technology (or use technology they already use) in another way?
How would you describe the status of your disease at the moment?
Patient experience
Could you describe a recent important event related to your disease (e.g. a hospital admission, new medication, emergency situation, …)
Therapy adherence
What have your caregivers told you to do and not to do? Do you receive any therapy or lifestyle rules?
For each of the advices/rules/therapies: do you always adhere to this? When and why (not)?
Are there any factors that influence whether you adhere to advice, rules, and therapies or not? E.g. your mood, your physical wellbeing, people around you, specific situations? Something else?
Why is it so hard sometimes to keep adhering to advices/rules/therapies? Can you think of anything that would make this easier for you?
How do you try to avoid that you don't adhere to advice you receive? Do you use tricks to help you to adhere to advice/rules/therapies? E.g. ask others to remind you or to follow the same rules?
Social network
Do you know any people with the same disease? What do you share with them? How do you keep in touch with them?
Indicate the role of each important person in the social network map
Has your disease in any way affected your social life? How?
Interaction with caregivers
Indicate role, nature & moment of contact
Expectations towards assistive wearable solutions
Thought experiment: what if invisible little creatures live in our bodies that can measure anything that is going on? What would participants want to know? How would they feel if the data would be sent to their caregivers?
Include mindfulness exercise in diary, ask people during interview how they liked the exercise, whether they would be willing to do similar exercises more often, what they think the effect of such an exercise is?
Do you sometimes plan to do something (e.g. adhere to advice) and end up not doing it? Why does this happen? What do you do when this happens? Do you feel bad about yourself if this happens?
What would be a good way to explain HeartMan to participants and ask them about expectations/attitudes?