ABSTRACT
Self-care support is a key cornerstone of treatment for patients with a cardiovascular disease. The success of any supportive intervention requires adaptation to the distinct needs of individuals. This requirement also applies to eHealth interventions. This study investigates how experts from multiple fields of science assess the potential success of different eHealth design strategies when matched to key self-care needs. An online vignette survey experiment was conducted. Nine vignettes representing different combinations of self-care needs (maintenance, monitoring, management) and eHealth persuasive design strategies (primary task support, dialogue support, social support) were evaluated. In total, 118 experts from 18 different countries participated in the survey. Their evaluations show primary task support as a promising design strategy across all self-care needs. In contrast, dialogue support and social support showed more promise for specific self-care needs. Above all, according to experts, the success of design strategies could be enhanced by (i) personalising the pacing of the intervention and (ii) tailoring the information to the literacy and culture of the person. Adding to that, self-care support should distinctly (iii) support the three self-care needs, be (iv) patient-centered, (v) support the collaboration with caregivers, and (vi) be aligned to the life goals and values of individuals.
1. Introduction
Cardiovascular disease (CVD) adds an alarming burden to health care systems worldwide (Roth, Johnson, and Abajobir Citation2017). A key cornerstone of treatment that can lessen such burden is to support the self-care goals and behaviours of patients (Riegel, Moser, and Buck Citation2017). To effectively support self-care, a strategy must consider the distinct needs of the individual, their most relevant goals, and key behaviours (Harvey, Dopson, and McManus Citation2015; Tadas and Coyle Citation2020). For example, the needs of a patient with a stable condition might center on the goal of improving general health and well-being to minimise risks, which can be achieved through the performance of healthy behaviours such as going for a short walk every morning.
The present study investigates how the design of technology-based interventions can be tailored to better support the varying self-care needs of patients. The approach of using technology to support health, well-being, and health care is better known by the concept of electronic health or eHealth (van Gemert-Pijnen, Kip, and Kelders Citation2018). The study proposed different eHealth design strategies to support distinct theory-based self-care needs, and asked individuals, with diverse professional backgrounds and expertise, to evaluate their potential success (e.g. cardiologists, psychologists, and technology designers). The study follows the premise that multidisciplinary expert stakeholders play key roles in the process of eHealth development. In that regard, the present study aimed to take a ‘holistic’ view of eHealth development to capture many of the influencing factors that determine the success of eHealth (e.g. human, technological, and contextual factors) (van Gemert-Pijnen, Nijland, and van Limburg Citation2011). Therefore, the views of experts were studied to better understand their diverse views and approaches to eHealth design when it comes to self-care support. To elaborate on this approach, the following sections introduce two overarching themes that inspired this study.
1.1. Designing eHealth for self-care with theory
To better understand the needs of patients, it is important to understand self-care as a complex process involving multiple goals and behaviours. This paper uses the term self-care instead of self-management, self-regulation, or other related terms, adhering to the propositions of the Middle-Range Theory of Self-Care of Chronic Illness (Matarese, Lommi, and De Marinis Citation2018; Riegel, Jaarsma, and Lee Citation2019b; Riegel, Jaarsma, and Stromberg Citation2012). This theory posits that self-care entails key processes of health maintenance (e.g. to take a short walk every day), monitoring (e.g. to routinely measure blood pressure), and management (e.g. to decide if a perceived symptom is a reason to call the health care provider) (Riegel, Jaarsma, and Stromberg Citation2012). This theory outlines the complexity of self-care because it explains how it can be influenced by multiple, reciprocally interacting factors such as the experience, motivation, and cultural beliefs of the patient (Riegel, Jaarsma, and Lee Citation2019). The use of theory in self-care studies also contributes to the accumulation and curation of knowledge, thus facilitating progress towards the identification of the most promising components for self-care support (Cornet, Daley, and Cavalcanti Citation2020; Jaarsma, Strömberg, and Dunbar Citation2020; Riegel, Dunbar, and Fitzsimons Citation2019; Toukhsati, Jaarsma, and Babu Citation2019).
The complexity of the individual self-care process makes it important to identify what support strategies work best, for whom, and why (Jaarsma, Strömberg, and Dunbar Citation2020; Riegel, Dunbar, and Fitzsimons Citation2019; Hekler, Michie, and Pavel Citation2016). The present study specifically investigates strategies that are embedded in eHealth design to support the self-care of patients with a CVD. There is already a lot of accumulated evidence that eHealth can support self-care of chronic conditions, including all types of CVD (Riegel, Moser, and Buck Citation2017; Greenwood, Gee, and Fatkin Citation2017; Hanlon, Daines, and Campbell Citation2017; Kebapci, Ozkaynak, and Lareau Citation2020; Kim and Lee Citation2017; Villarreal and Berbey-Alvarez Citation2020). All in all, the promise of eHealth seems to rest on its ability to support patients while they are at their homes and communities. For instance, smartphone-based applications that seek to remotely support self-care of patients with heart failure or hypertension have been found to be feasible, acceptable, and effective interventions (Cajita, Hodgson, and Budhathoki Citation2017; Chandler, Sox, and Kellam Citation2019; Foster Citation2018; Triantafyllidis, Kondylakis, and Votis Citation2019; Woods, Duff, and Roehrer Citation2019; Chantler, Paton, and Velardo Citation2016).
To effectively support self-care, an eHealth technology can integrate multiple design strategies. The challenge of designing for self-care arises because multiple agents and their roles must be considered (e.g. patients, family members, informal caregivers, and health care professionals) (Cornet, Daley, and Cavalcanti Citation2020). To put an example, design strategies can direct what type of content (e.g. information about the disease) and mode of presentation is employed (e.g. text or videos). Technology design models such as the Persuasive Systems Design (PSD) model can be used to select supportive design strategies (Oinas-Kukkonen and Harjumaa Citation2009). The PSD model categorises design strategies that aim to increase a system’s persuasiveness, meaning how much it can motivate its users to reach their goals (Oinas-Kukkonen and Harjumaa Citation2009). For instance, patients who need to improve their general health and aim to do so by increasing physical activity could be supported by a planner to schedule daily exercise sessions (an example of what the PSD model calls primary task support). Alternatively, the same patients with the same need could be supported through the delivery of motivational messages to their phones (an example of what the PSD model calls dialogue support). Finally, the same patients could also be supported via the enrolment in an online support group with other individuals that share similar goals (an example of what the PSD model calls social support).
In practice, persuasive design strategies can be operationalised in many different ways in an eHealth technology. For instance, they can be tailored to target key psycho-behavioural determinants that potentially increase eHealth effectiveness (e.g. targeting an individual’s motivation to change) (Oyebode, Ndulue, and Mulchandani Citation2021; van Velsen, Broekhuis, and Jansen-Kosterink Citation2019). In studies of persuasive design, strategies have targeted specific determinants using theoretical frameworks such as self-determination theory (van Velsen, Broekhuis, and Jansen-Kosterink Citation2019) or the ARCS motivation model (Oyebode, Ndulue, and Mulchandani Citation2021). In a similar way, it is plausible that different strategies could also have varying effects on the distinct processes of self-care that are proposed by the Middle-Range Theory of Self-Care of Chronic Illness (e.g. the same factor could act as a facilitator or a barrier, depending on the person, the need, and the context) (Harvey, Dopson, and McManus Citation2015; Tadas and Coyle Citation2020). Moreover, research has suggested that persuasive design strategies such as goal-setting, suggestions, or reminders are key components of eHealth interventions that aim to promote healthy lifestyles (Lentferink, Oldenhuis, and de Groot Citation2017). However, in the context of CVD, no studies have yet explored how specific eHealth (persuasive) design strategies should actually be operationalised and tailored to the diverse and dynamic self-care processes to achieve optimal support.
1.2. Studying the tailoring of eHealth design through vignette survey experiments
Several approaches that can be used to inform, guide, or operationalise the tailoring of eHealth design to the patients’ characteristics can be identified in scientific publications. For instance, the use of theoretical models to inform or justify design choices, the creation of ‘representative’ user profiles to guide or reflect upon the design work, or the development of data-driven adaptive features to operationalise tailoring during implementation (Cruz-Martínez, Sieverink, and Wesselink Citation2018; Haldane, Koh, and Srivastava Citation2019; Mawson, Nasr, and Parker Citation2016; Wais-Zechmann, Gattol, and Neureiter Citation2018; Wildeboer, Kelders, and van Gemert-Pijnen Citation2016). However, in the specific case of tailoring for CVD self-care, this type of information is still often lacking or left unclear in published reports. Case in point, a recent review of eHealth interventions within this scope showed that the vast majority of theoretical models used to inform their design was not suitable to capture all relevant factors (e.g. developers did not consider technology-driven models) (Cruz-Martínez, Wentzel, and Asbjørnsen Citation2020). In general, detailed descriptions of the guiding design approaches was lacking, making it difficult to identify what type of knowledge informed, guided, or was used somehow to tailor an intervention (Cruz-Martínez, Wentzel, and Asbjørnsen Citation2020). As noted before, the approaches that expert stakeholders adopt to inform, guide, or operationalise eHealth design matters because their choices can end up determining the success of an intervention. Thus, here lies a gap in the case of CVD self-care, because previous works have not directly studied how or why specific eHealth design strategies could be successful at supporting some self-care needs, while being less promising for others.
To bridge the aforementioned gap, it is important to identify how eHealth could be tailored to ensure an optimal match between different types of design features and the dynamic self-care needs of patients with a CVD. For example, to identify what influencing factors could be the most relevant for a patient with an outstanding maintenance need, and then select the eHealth design features that could best support them. To pursue that goal, one could consider developing contrasting versions of a particular eHealth intervention, then deliver each version to a suitable amount of individuals, and finally observe their outcomes before making an informed decision for the best tailoring approach. However, that could be a highly inefficient way to meet the goal, as it would take time and resources to develop and test multiple designs of the same intervention. Alternatively, to study the potential effect of eHealth design strategies on distinct self-care needs, and to go beyond what can be found in the literature, the present study proposes to form a multidisciplinary panel of experts that can directly tackle the gap and pursue the main goal (e.g. experts such as cardiologists, nurses, technology designers, or psychologists who conduct research on eHealth or use it in their professional practice to treat CVD).
Certainly, it must be noted that the views of experts can only provide a partial view on the matter, as it leaves out the perspectives of patients. However, the present work adopts a holistic view of eHealth that seeks to explore the views of all key stakeholders who are involved in the process of design and development (van Gemert-Pijnen, Nijland, and van Limburg Citation2011). For that reason, the study holds the premise that systematically assessing the views of experts on the tailoring of eHealth design for self-care is a feasible and relevant step that can begin to bridge the observed gap in the published literature at the crossroads of self-care, CVD, and eHealth (Cruz-Martínez, Wentzel, and Asbjørnsen Citation2020). That is, because published literature does not always clarify how eHealth researchers and developers underpin their design choices (e.g. in theory, empirical studies, or intuition). Nevertheless, expert stakeholders play important roles in determining how supportive strategies are matched to the needs of individuals in the target population. Thus, studying their views and decisions could provide a deeper understanding of how eHealth design can be tailored to best support self-care.
Importantly, when a panel of experts is involved, it is necessary to collect and analyse data in such a way that it derives valid and structured conclusions, rather than just a collection of multiple and diverse opinions. To this end, a vignette survey experiment was proposed as a suitable method. Vignettes are short, systematically varied descriptions of situations or persons (Atzmüller and Steiner Citation2010). In a vignette experiment, respondents are confronted with vignettes that are composed of a (randomised) combination of different factors (which is why they are also called factorial survey experiments) (Atzmüller and Steiner Citation2010; Auspurg and Hinz Citation2015). The experimental approach aims to identify how each factor might causally affect individual responses to the contextualised, hypothetical settings depicted in the vignettes (Atzmüller and Steiner Citation2010). The vignettes can be presented to respondents within the survey in many different forms, for example using keywords, narrative text, pictures, audio, or videos (Atzmüller and Steiner Citation2010). The vignettes can also provide rich qualitative data because they generate reactions to stimuli that seeks to closely resemble realistic situations (Jackson, Harrison, and Swinburn Citation2015). In short, this study proposes that a vignette survey experimental approach can facilitate the collection of key, contextualised information from experts, which will advance knowledge of how distinct eHealth design strategies can better match specific self-care needs of patients with a CVD.
1.3. Aim
The present study aims to investigate how experts from multiple fields of science (such as medicine, psychology, or technology design) assess the potential success of eHealth design strategies when matched to the specific processes of self-care maintenance, monitoring, and management. The multidisciplinary perspective is important to capture various dimensions of factors that are often missed by discipline-specific studies. The results of the study will provide practical knowledge on which eHealth design strategies are potentially more effective than others, and why. This practical knowledge will be used in future studies to design and test prototypes that are tailored to specific needs, relevant goals, and key behaviours. The main research questions of the study are:
What eHealth design strategies are most promising (i.e. perceived to be successful), according to the views of experts, to support distinct self-care needs of patients with a CVD?
According to the views of experts, what factors can explain the high or low promise (i.e. perceived success) of eHealth design strategies to support distinct self-care needs of patients with a CVD?
To assess the external validity of the results, an additional question was also of interest: how realistic are the cases depicted in the vignettes, according to experts from multiple fields of science? An advantage of vignette survey experiments is precisely that they aim to balance both internal and external validity (Auspurg and Hinz Citation2015). Although it is not a main study question, providing an answer to it could help to establish the generalisability of the results.
2. Materials and methods
2.1. Study design
An online vignette survey experiment was conducted (Auspurg and Hinz Citation2015). The survey collected both quantitative and qualitative data in parallel. Data were analysed separately at first but brought together at the discussion level to bridge all key findings of the study (Creswell and Clark Citation2017; Fetters, Curry, and Creswell Citation2013).
2.2. Experimental factors and design
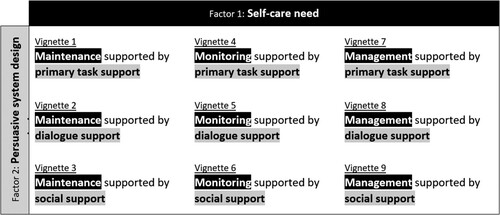
To answer the research questions, a factorial experimental design was used in order to establish how single factors and their levels, as depicted and systematically varied in the vignettes, causally affected individual responses (Atzmüller and Steiner Citation2010). It must be emphasised that, in contrast to typical experiments of interventions in health care, vignette experiments use short, systematically varied descriptions of situations or persons (called vignettes) to elicit the beliefs, attitudes, or behaviours of respondents with respect to the scenarios presented within the survey (Steiner, Atzmüller, and Su Citation2017). Following that rationale, the factorial design of the present study included two factors, self-care needs and eHealth design strategies, with three levels each.
The factor levels defining distinct self-care needs were based on the Middle-Range Theory of Self-Care of Chronic Illness (Riegel, Jaarsma, and Stromberg Citation2012). The three levels were: maintenance, defined as the performance of behaviours to improve well-being, preserve health, or to maintain physical and emotional stability; monitoring, defined as the process of routine, vigilant body monitoring, surveillance, or ‘body listening’; and management, defined as the evaluation of changes in physical and emotional signs and symptoms to determine if action is needed (Riegel, Jaarsma, and Stromberg Citation2012).
The factor levels defining different eHealth design strategies were based on the PSD model and previous studies on eHealth design (Oinas-Kukkonen and Harjumaa Citation2009). The three levels used were: primary task support, defined as a persuasive design strategy that directly supports the user in carrying out a primary task; dialogue support, defined as a persuasive design strategy that implements computer–human dialogue in a manner that helps the user move towards the goal or target behaviour; and social support, defined as a persuasive design strategy that seeks to motivate the user by leveraging social influence (Oinas-Kukkonen and Harjumaa Citation2009). These levels were chosen based on previous studies of eHealth design (van Velsen, Broekhuis, and Jansen-Kosterink Citation2019; Lentferink, Oldenhuis, and de Groot Citation2017; Asbjørnsen, Wentzel, and Smedsrød Citation2020) and because in the PSD model they are broad, easily distinguishable categories that can include more specific principles to persuade users into behaviour change. For example, differentiating the previously defined categories could be easier and more relevant than differentiating ‘reminders’ from ‘suggestions’, both of which are specific principles placed under the dialogue support category.
The factorial design resulting from the combination of these factors and levels delivers a population of 9 different vignettes (3 × 3 or 32). presents an overview of the nine vignettes, and in the next section presents an example of a vignette design and structure, as it appeared in the survey. For easier comparison, Appendix 1 presents a full list of key study definitions that are also described throughout the paper. Moreover, Appendix 2 provides the full textual summaries of each vignette factor level.
2.3. Vignette design
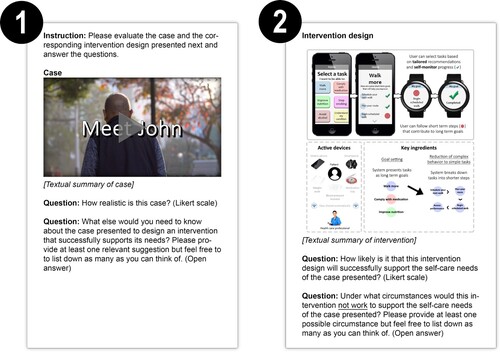
To provide valid answers to the research questions, each vignette in must accurately describe a hypothetical scenario aligned to the corresponding combination of factors. To accomplish that, in each vignette the self-care need was represented with a short video that described the situation and self-care needs of an individual with a CVD (left in ). To complement the vignette, the persuasive design strategy was represented by a visual mock-up of an eHealth intervention (right in ).
Specific cardiovascular conditions were used to make each case more realistic and contextualised. For that, three different conditions were selected to represent each self-care need (left in ). Coronary heart disease was selected for the maintenance need, hypertension for the monitoring need, and heart failure for the management need. An overview of CVD self-care studies shows that these three conditions demand engagement in all self-care needs (Riegel, Moser, and Buck Citation2017).
On the other hand, a mock-up was created to contextualise the presentation of key components for an eHealth intervention (right in ). Mock-ups are a way to provide medium-fidelity representations of a design, and can complement other forms of description such as text or diagrams (Burns Citation2018). A smartphone app was chosen as the mode of delivery because it is often used in eHealth interventions that combine monitoring and coaching to promote healthier lifestyles, and several examples were known by the research team from periodic literature searches and a systematic review of eHealth interventions for CVD (Cruz-Martínez, Wentzel, and Asbjørnsen Citation2020; Cruz-Martínez, Noort, and Asbjørnsen Citation2019). In short, the mock-up mimicked a smartphone app, its interface and presented a visualisation of active technological devices and its key ingredients. To make sure the depictions of the self-care needs or design strategies were clear, each vignette was iteratively revised with input from researchers of the department of Psychology, Health and Technology of the University of Twente, who were not involved in the study.
2.4. Survey design
To answer both research questions, it was important to obtain sufficient assessments for all vignettes. However, principally to make it less burdensome and repetitive for respondents, the nine vignettes were divided into three different survey blocks. Dividing the survey into equally sized blocks (also called sets or decks) is a common technique of vignette survey experiments (Auspurg and Hinz Citation2015). The survey was created using the Qualtrics software (Qualtrics, Provo, Utah, U.S.A.), and divided in three blocks. Earlier versions of the survey were also pilot tested with researchers not involved in the study. Appendix 3 provides additional descriptions of each survey section and its content.
In accordance with the experimental approach, each respondent was randomised to one of the three different blocks. However, each block displayed the cases representing the self-care needs in the same order: first the maintenance need, then the monitoring need, and finally the management need. The main difference therefore was that each block presented a different mock-up of an eHealth design strategy as a solution to each case. The order was based on the propositions of the Middle-Range Theory of Self-Care of Chronic Illness, mainly by the argument that patients must lay a foundation on self-care maintenance first, and later build expertise in self-care monitoring and management (Riegel, Jaarsma, and Lee Citation2019; Riegel, Jaarsma, and Stromberg Citation2012). Such theory-based order was preferred over total randomisation of vignettes across respondents, primarily because respondents could have been instinctively confused by the order in which vignettes are presented, or became highly aware of the aim of the study by having to rate two or more vignettes with repeated self-care needs or eHealth design strategies. Supporting this choice was evidence that shows order effects of vignettes are minimised when vignettes have a certain level of complexity (e.g. by video presentation rather than just a short text) (Auspurg and Jäckle Citation2017).
As can be observed in , for each vignette respondents were first presented with the self-care case video. They were then asked about how realistic the cases seemed to them. For that, they could answer via a 5-point Likert scale, ranging from ‘Extremely unrealistic’ to ‘Extremely realistic’. This was followed with an open-ended question asking about aspects of importance to design an intervention that successfully supports the case’s needs. In this way, respondents were primed to think about their own expertise and experience before presenting a mock-up. Next, respondents were presented with a mock-up and were asked about the likeliness to succeed of the eHealth intervention design to support the case’s self-care need. Respondents could also answer via a 5-point Likert scale, ranging from ‘Extremely unlikely’ to ‘Extremely likely’. After providing this rating, respondents were finally asked an open-ended question about the circumstances under which according to them the intervention would not work to support the self-care needs of the case presented.
2.5. Sample size and recruitment
The recruitment objective was to collect a minimum of 30 responses per vignette from experts and to randomise to each survey block to achieve balanced groups. Based on that objective, a minimum sample size of 100 participants was determined. Between January and April of 2020, 752 experts were invited to participate via e-mail. The list of potential participants was created by searching scientific publications, professional networking platforms (e.g. LinkedIn and ResearchGate), and websites of relevant institutions (e.g. directories of universities, medical associations, or research centers). Snowball sampling was also used, prompting those first invited to refer other experts. The survey was only accessible to individuals who received an invitation link via e-mail by the main researcher (RCM). In the case of referrals, their expertise and experience were checked before sending an invitation to participate. On top of that, the exit questions asked background information and an e-mail for a potential follow-up.
Although it was not possible to certify with a hundred percent confidence who was sitting behind the screen responding to the questions, the aforementioned steps were considered to provide sufficient confidence in the identity, expertise, and experience of the respondents (i.e. the pre-screening, the individual invitation links, and the exit questions). As a selection criterion, expertise was defined as having cross-disciplinary or domain-specific knowledge in one of the key topics of the survey, which could include but not be limited to medical, behavioural, computer and informational systems engineering, design, human-technology interaction, human factors and ergonomics, and business or innovation. In addition, experience was defined as having led, participated, or consulted in projects of relevance to the topics of the survey. The projects could be related to academia, health care institutions, private industry, or policy-making. Ethical approval was obtained from the ethical committee of the Faculty of Behavioural, Management and Social sciences of the University of Twente (request number 191396).
2.6. Data analysis
2.6.1. Quantitative data
To answer the first research question, about the identification of the most promising eHealth design strategies to support specific self-care needs, it was hypothesised that vignette factor levels (the specific need or the design being presented) would have significant effects on the ratings, mainly by interactions between each other (e.g. that for the same case, different designs have higher or lower chances to be rated higher in the success scale). Quantitative data were entered into SPSS version 26 (IBM Corp., Armonk, New York, U.S.A.). Descriptive statistics (e.g. percentage distributions) and generalised linear mixed modeling (GLMM) were used due to the ordinal measurement level of the outcome variables and the hierarchical structure of the data (Garson Citation2013; Heck, Thomas, and Tabata Citation2013). The dependent variables were the realism and success ratings given to the vignettes, while the independent variables were the vignette factors being rated. As an external validity check, the realism of each case presented was first examined. For this, it was expected that realism ratings would not differ between cases. For the GLMM of the success ratings, the five-point scale was collapsed into three categories because both the ‘Extremely unlikely’ and ‘Extremely likely’ categories had low counts (six, and three, respectively). For the GLMM of the realism ratings, the five-point scale was collapsed into four categories because the ‘Extremely unrealistic’ category had only three counts in total.
2.6.2. Qualitative data
To answer the second research question, about the possible reasons argued by experts for the (lack of) perceived success of eHealth design strategies, qualitative data were analysed by RCM and JW with the thematic analysis method (Braun and Clarke Citation2006). The thematic analysis could provide support to the answers of the first research question (e.g. why a strategy was seen as promising) or provide expanding or contrasting evidence (e.g. arguments for the potential of strategies despite being perceived as ‘less successful’). To conduct the analysis, the data were exported to a Microsoft Excel 2016 workbook. The analysis consisted of four steps: (1) inductive pilot coding; (2) codebook-driven coding; (3) analysis and revision of coding results; and (4) searching and reviewing for themes.
The inductive coding pilot was performed independently by two reviewers (RCM and JW) on a small set of data extracts (i.e. individual responses to open-ended questions), to become familiarised with the data. Next, RCM considered the results of the pilot and then proceeded to code all of the data to create an initial codebook, iteratively revising code labels and descriptions. The codebook resulting from RCM’s full-data coding was then used independently by JW, who could still suggest new codes or make notes when necessary. Once all data had been independently coded by both researchers using the codebook, RCM analysed the results and suggested revisions according to the levels of agreement reached. For instance, the highest priority of data extracts to revise were those with no agreements between reviewers despite multiple codes being proposed by one or both. A sub-set of these revisions were checked and approved by JW. At this stage it was judged that the qualitative data set had been analysed thoroughly and additional full dual-reviewing was not deemed necessary. To finalise, RCM searched, reviewed, and defined the themes, receiving feedback from JW and JGP. The most salient codes by frequency and interpreted significance per vignette (case by design combinations) were taken as the basis for most themes.
3. Results
3.1. Characteristics of respondents
Out of the 752 invited experts, 118 completed the survey (15.7% response rate). Respondents were from 18 countries in total. The Netherlands (38.3%), the United Kingdom (10.3%) and the United States (8.4%) were the most common countries of origin. Most respondents categorised themselves as a ‘researcher’ (66.1%), rather than a ‘developer or implementer’ or a ‘health care professional or provider’. presents an overview of the respondents’ expertise. Appendix 4 provides more details about the respondents’ characteristics.
Table 1. Overview of respondents’ expertise.
3.2. Quantitative results
In total, 329 ratings were collected about both the success and realism of vignettes. The goal was to collect three ratings per participant but 7.1% responses were missing (25 out of 354).
3.3. Perceived success of eHealth design strategies
In answer to the first research question, about the identification of the most promising eHealth design strategies, the results show that some combinations of cases and designs did differ with each other. presents all percentage distributions of the success ratings per vignette. shows some noticeable differences in the ratings across vignettes. For instance, primary task support was more frequently rated as ‘very likely’ to succeed for both monitoring (V4) and management (V7) needs. Similarly, dialogue support for a monitoring need (V5) was the highest rated combination. In contrast, the social support strategy was more frequently rated as ‘very unlikely’ to succeed for both monitoring (V6) and management (V9) needs. Dialogue support for a management need (V8) was also more frequently rated the same way. Interestingly, what also shows is that a large amount of experts settled for the ‘somewhat likely’ response option when rating the potential success of eHealth design strategies (from 48.6% for V8 up to 81.1% for V3).
Figure 3. Percentage distribution of the success ratings per vignette (case x persuasive design strategy).
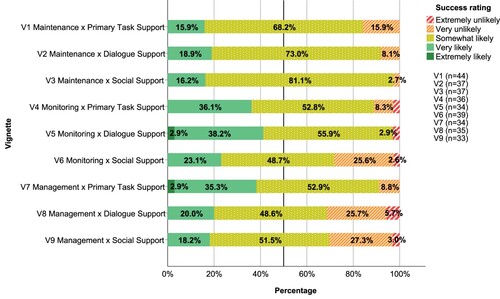
presents an overview of the GLMM output of success ratings. shows that some combinations of cases and designs did significantly differ with each other (F = 3.22; p = .013). Specifically, reveals that, when compared to primary task support, social support was significantly less likely to be successful at supporting monitoring needs (OR = .167; 95% CI .035–.801; p = .025). Similarly, both dialogue (OR = .147; 95% CI .028–.769; p = .023) and social support (OR = .114; 95% CI .024–.540; p = .006) were significantly less likely to be successful at supporting management needs.
Table 2. Fixed coefficients in GLMM of success ratings.
3.3.1. Realism of the self-care cases
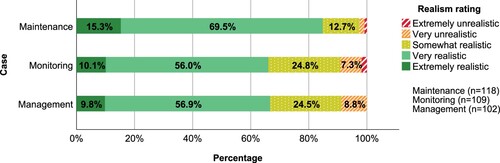
The self-care cases depicted in the vignettes were expected to be assessed as highly realistic by experts. However, the results show that this was not always the case. presents the percentage distribution of the realism ratings of cases and visualises how much, in comparison to the maintenance case, the monitoring and management cases were less frequently rated as being ‘very’ or ‘extremely’ realistic.
The observed difference was statistically significant (F = 13.79; p = .000), as can be confirmed by the GLMM output of realism ratings shown in . Specifically, the monitoring (OR = .338; 95% CI .195–.586; p = .000) and management (OR = .325; 95% CI .205–.516; p = .000) case were significantly perceived to be less realistic when compared to the maintenance case.
Table 3. Fixed coefficients in GLMM of realism ratings.
3.4. Qualitative results
In answer to the second research question, about the arguments provided by experts to judge the potential (lack of) success of eHealth design strategies, the patterns of the qualitative data emphasised multiple approaches towards eHealth tailoring. At large, experts proposed how to tackle the multidimensional factors that can influence the potential success of design strategies for self-care support. Six major themes were identified:
Unraveling complexity to achieve patient-centeredness.
Addressing complexity by adjusting the pacing and simplicity of eHealth interventions.
Supporting persons and their circumstances, not just as patients.
Supporting collaboration between the patient and the health care team.
Targeting key objectives with eHealth support.
Fitting eHealth into self-care routines.
3.4.1. Unraveling complexity to achieve patient-centeredness
According to experts, the success of any design strategy depended heavily on first conducting a holistic, thorough, patient-centered assessment. However, the list of influencing factors could be extensive, multidimensional, and naturally unknown to the health care provider or intervention designer. In practice, experts advised to collaboratively analyse key factors with the patient before considering any potential solutions. The primacy of patient-centeredness was well described by the following quote:
To ensure the optimal personalization of the intervention [we would seek to collect] baseline data around the subjects physical condition, mental health and current relevant behaviors, their attitudes to behavior change and willingness to change, or to optimize each of the various behaviors and the barriers to those changes (i.e. how easy it is to improve behavior or reach optimal behavior for each indicator). (eHealth developer with expertise on computer and informational systems engineering and neuroscience)
Recurring views from experts suggested that the highest level of complexity in such an assessment comes with factors that are highly intertwined with each other. For instance, what was often referred to as the ‘social context and environment’ can be composed of several factors. The next quote exemplifies this for the maintenance case:
What is John’s family situation? Who makes the decisions on what to buy from the store? Who makes the foods John eats? Should the whole family be included in the intervention? Does John have any other conditions that we should be aware of? What is the education level of John? What kind of terminology should be used for him? In what kind of environment does John live in? Is it possible for him to, for example, take a walk in the neighborhood or to go to a forest for a walk? (eHealth researcher with expertise on communication science)
Other important multifactorial aspects to consider were about the availability of technology, its acceptability as a potential solution to self-care needs, and finally, the capability of the patient to actually use it for that purpose. Similarly, the patient’s own previous experience in self-care was complex because it could englobe both favourable and unfavourable beliefs or attitudes towards intervention components.
3.4.2. Addressing complexity by adjusting the pacing and simplicity of eHealth interventions
According to experts, the success of design strategies goes beyond simply matching problem A with solution B. What matters the most is to address the problem in the simplest, most meaningful way. To do this, experts highlighted the importance of attuning the pacing of the intervention to what better fits each patient according to their experiences, abilities, or attitudes. This idea is outlined by the next quote:
It comes down to what kind of patient is in front of you. In case of our own mHealth [mobile health] intervention, I can say that the majority of patients is cooperating without an issue. They learn about their disease and via that route, they manage to both improve their lifestyle and ask better questions to the physician. However, there are many patients who need (technology) support. This cannot be disregarded when starting an mHealth intervention. (eHealth implementer with expertise on medicine)
Experts emphasised that pacing does not apply only to the ability of using technology, but extends to the patient’s physical or mental state and current knowledge or skills in self-care. Therefore, tailoring also requires adaptation to the patient’s informational, learning, or reflective needs. This refers to what patients need to know, how they can better get to learn it, and how they prefer to reflect about it. For example, the following two experts envisioned two different directions in the provision of information for the management case:
I am not sure whether it is advantageous to know all side effects of medication. I know from experience that patients get very afraid about those side effects, leading to negative emotions, which in turn can affect the desired positive outcome of the intervention. (eHealth researcher with expertise on communication science, human-media interaction, and psychology)
I think a personal plan involves more than text messages can solve. An online ‘workbook' with questions and assignments that help George to deal with his lack of knowledge on symptoms and guidelines and solutions for the necessary adjustments could be an extra intervention, and again with the guidance needed. (eHealth researcher with expertise on health sciences, nursing, and philosophy)
3.4.3. Supporting persons and their circumstances, not just as patients
According to experts, despite the wide range of potential design strategies that can be considered, the starting point in offering support is clear: start where the patient chooses. In other words, when supporting self-care: prioritise the person over the patient. The next quote exemplifies this approach for the maintenance case:
What are concrete goals in regard of daily life which are hindered by his illness? For example, related to career, leisure, social interactions, etc. In my view, to be successful in goal achievement, these personal goals should be the starting point and determine what should be John’s medical and functional goals and subsequently the self-care tasks/activities John should perform to achieve these goals (medical and personal). For example, John wants to go on a world-trip. This requires John to be in relative good health, which can be achieved through performing self-care activities X, Y and Z. (eHealth researcher with expertise on human-media interaction)
Several experts reasoned that this approach to promote self-care must leverage on a person’s intrinsic motivation. Nevertheless, some experts also warned that behaviour change is not just about motivation. To help the person achieve their life goals, experts emphasised that all design strategies must be aware of the context or the person’s circumstances:
I think simplification of the complex behavior is a good way to support self-care. However, one also needs to consider external factors as these are very much context dependent. For example, John, as an old man, may find it difficult and inconvenient to take a walk when it is raining outside. Hence, when breaking down the tasks into shorter steps, the system should be aware of the context. (eHealth researcher with expertise on human-media interaction)
3.4.4. Supporting collaboration between the patient and the health care team
In the view of experts, the most successful strategies are those that facilitate (rather than seek to replace) the collaboration between a person and the health care team. However, experts in this study did not just prefer warm over cold care, but also emphasised that what is necessary is to provide health care professionals the right tools to support the self-care process. This challenge is noted by the following quote:
How are the data to be presented to the health care professional? Our research showed sharing is an important motivator but professionals do not want a constant stream of raw data and will not participate unless the data has been intelligently presented and transferred to them in a way that is congruent with other data such as hospital letters. I.e. they do not like having to log on to a website. (eHealth researcher with expertise on health sciences and nursing)
Design strategies that skip over the process of collaboration could overwhelm patients, especially for the interpretation of symptoms and the decisions about how and when to take action. On the other hand, several experts made the point that collaboration must still be driven by patient-centeredness. The following quote highlights again this important requirement:
It is pretty clear in this case scenario what healthcare professionals think that the patient should do, and why. What I completely miss in this case scenario is the patient’s own intrinsic motivation. I therefore also miss any tool and/or strategy to explore and strengthen that intrinsic motivation. (Expert on preventive cardiology)
3.4.5. Targeting key objectives with eHealth support
According to experts, while health care providers are indispensable, eHealth does have things to offer for self-care support. One of the key objectives that eHealth can help with is to increase the patient’s health literacy. Bridging the knowledge-behaviour gap was a key challenge, as it could be for the maintenance case (e.g. understanding information about condition, medication, long-term effects). Another important objective for eHealth is to support the habituation to monitoring signals and symptoms. This is outlined for the monitoring case in the following quote:
Why not let technology work as it already does? The APIs [application programming interfaces] in the mobile systems take in the measurements automatically from internet-capable devices such as scales and blood pressure monitors and the system could simply show the ongoing trend and maybe the latest reading and show if there is a gap (e.g. if the user did not step on scales this week). (eHealth researcher with expertise on human factors and ergonomics, and psychology)
Beyond simply monitoring, experts also highlighted the importance of the provision of feedback, and its potential challenges. Three key objectives that eHealth design strategies could help with were identified in this area: to increase awareness, to facilitate sense-making, and to support emotional control (e.g. over anxiety or fear). Both primary task support and dialogue support were often endorsed as suitable persuasive strategies that could be applied to fulfill these objectives.
3.4.6. Fitting eHealth into self-care routines
According to experts, overcomplicated and unnecessary design strategies would only hinder eHealth’s uptake and fit in a person’s life. However, doing this required more than just simplicity. Remarkably, several experts called for eHealth to be empathic, reassuring, and empowering. In this regard, several experts suggested that eHealth design strategies must be personalised to reflect a person’s internal narrative of his/her condition, for example by offering tailored messages. The following quote gives an example of this approach:
Jane’s main problem is fear of [the consequences of her] condition and of information that might likely tell her that her condition is not improving. She needs to be empowered by the technology, not disabled by it. Technology is not always positive, unless […] the interpretation of results is very easy and clear, [which might not occur] particularly if [the] technology breaks or is unreliable. (eHealth researcher with expertise on health sciences and psychology)
Experts in this study also endorsed tailored prompts to incentivise engagement and progress in self-care. The next quote outlines this method for the maintenance case:
Leaving the selection of the tasks to the patient may promote selection bias towards the easiest task for that particular patient. One possible example is the patient selecting the ‘walk more' goal and never selecting ‘stop smoking'. Maybe forcing less preferred tasks from time to time could be more effective towards more relevant changes in the patient’s lifestyle. (eHealth researcher with expertise on computer and informational systems engineering)
4. Discussion
The present study pursued the goal of understanding how to best tailor eHealth for self-care support by matching design strategies with the distinct needs of patients with a CVD. The goal was operationalised as two main research questions, which can be simplified as what works? And why does it work? When it comes to self-care support through eHealth.
The first research question sought to identify, from the view of experts, the most promising eHealth design strategies that can support specific self-care needs (i.e. under what context is a strategy most promising?). The results showed that primary task support was seen as a promising design strategy across different self-care needs. In contrast to that, while dialogue support was also promising for maintenance and monitoring needs, it was perceived to be less promising when supporting a management need. Moreover and notably, social support was perceived to be most promising only when supporting a maintenance self-care need. To characterise these findings, it must be noted that a large amount of experts settled for the ‘somewhat likely’ response option when rating the potential success of eHealth designs (see ). That observation highlights the importance of the answer obtained for the second research question of this study.
The second research question sought to integrate the arguments from experts about the potential success of eHealth design strategies when matched to specific self-care needs (i.e. why would a strategy work or not under that specific context?). The results relating to this question were represented by six major themes. These themes showed in general how the multidimensional, complex nature of self-care presents a remarkable challenge for eHealth design. In the following sections, the findings of the study are discussed along with related literature.
4.1. Promising eHealth design strategies to support distinct self-care needs
4.1.1. Primary task support
As remarked above, the results suggest that primary task support could be a promising eHealth design strategy across different self-care needs of patients with a CVD. In light of the themes of the qualitative data, the promise of this strategy seems to rest on the potential simplification of the various tasks across different self-care goals (maintenance, monitoring, and management). Experts suggested how different operationalisation of primary task support could match the varying behaviours across the theory-based self-care processes. For example, by setting personally meaningful goals for self-care maintenance (e.g. to support engagement in physical activity), facilitating self-care monitoring through automatic measurements (e.g. to support symptoms monitoring), or lowering the threshold of communication with the health care team for self-care management (e.g. to support collaboration with clinicians).
Research from the perspective of end users supports the large and promising applicability of primary task support strategies that was noted by experts involved in the present study. For instance, research on how eHealth can support long-term weight control has shown that end users could benefit from direct support to their self-regulation skills (Asbjørnsen, Wentzel, and Smedsrød Citation2020). Adding to that, primary task support principles within the PSD model such as ‘reduction’ (e.g. stepped, short-term goals) or ‘personalization’ (e.g. self-set goals) have been recognised as necessary components that can help achieve health outcomes (Lentferink, Oldenhuis, and de Groot Citation2017). Likewise, literature with a clinical perspective argues that these types of components could also help promote the underlying principle that there must be a shared responsibility between health care providers and patients (Tadas and Coyle Citation2020; Riegel, Jaarsma, and Lee Citation2019). In the present study, respondents with clinical expertise often emphasised the important balance between giving the patient the initiative while at the same time not leaving them completely alone in the process. In contrast to that, respondents with technical backgrounds rather emphasised the potential of eHealth to simplify or automatise tasks that could decrease the burden to the patient.
4.1.2. Dialogue support
In turn, the dialogue support design strategy was seen as promising for maintenance and monitoring needs (or at least as much as primary task support), but less so for a management need. According to several experts, the most salient barrier for the success of dialogue support was actually the fragility of the person depicted in the management case, and not the design itself. For some experts this combination was even unrealistic because someone like George (the fictional person depicted in the management case) would not be left alone or even ‘trusted’ with only technology to manage his own condition. Therefore, dialogue support seemed to be frequently judged by experts to be inadequate when the case at hand showed a dire need for more direct help and guidance to ensure the safety of the patient. These views made evident that another important objective for eHealth support was to minimise risks and contribute to ensure the patient’s safety.
The aforementioned insights aligns with research that has shown end users do appreciate dialogue support strategies such as receiving suggestions or reminders, as they could help them build confidence or motivation towards their goals (Oyebode, Ndulue, and Mulchandani Citation2021). Furthermore, related literature also supports the important requirement – noted repeatedly by experts involved in the present study – that communications must be timely, context-aware, and customisable by end users (Vo, Auroy, and Sarradon-Eck Citation2019). In that sense, the arguments in favour of dialogue support put forward by experts echoed the importance of underlying principles that eHealth developers and implementers should consider when aiming to support self-care. For example, on the principle of patient-centeredness, which under this context meant to ensure that communications from the technology stay relevant to the patients’ preferences and personal circumstances (e.g. literacy level and culture).
4.1.3. Social support
In the case of the social support design strategy, its merit was strikingly judged by many experts to be lower for the monitoring and management needs (when compared to the maintenance need). First, it might not be surprising that this strategy fits well with maintenance needs, as the importance of social support has been identified in self-care studies (Fivecoat, Sayers, and Riegel Citation2018; Won and Son Citation2016). Furthermore, there is evidence that individuals appreciate eHealth design strategies that aim to motivate them through social competition or compliments that they receive from others through digital means (van Velsen, Broekhuis, and Jansen-Kosterink Citation2019). However, those works have not distinguished between self-care processes as done by the present study (i.e. to identify if the aforementioned benefits apply to self-care monitoring and management tasks).
The results of the present study in fact suggest that the proposed operationalisation of the social support design strategy, as a chat function to facilitate peer support, was the main reason for the lower promise to support both the monitoring and management needs. For example, for the monitoring need, experts found it difficult to conceive how social support could promote or facilitate the corresponding behaviours such as to routinely measure blood pressure. Moreover, experts reasoned that this strategy entailed too many pitfalls when it came to support management needs. For example, potential risks caused by misinformation or lack of supervision over interactions between patients. Research on social support has supported the ambiguity of this type of strategy as signaled by the present study. For instance, social support has been noted to act as both an important facilitator or barrier for the adoption of self-care solutions (Harvey, Dopson, and McManus Citation2015). Extending on that, a meta-review of qualitative studies with patients supports the view that such strategies might only be appreciated by specific sub-groups (e.g. younger individuals) or work under specific circumstances (e.g. when there is social isolation) (Vo, Auroy, and Sarradon-Eck Citation2019).
4.2. Tailoring eHealth design to the self-care needs of cardiovascular diseases
Largely, for many of the multidisciplinary experts involved in this study the optimal eHealth design includes but goes beyond simply selecting a specific design strategy to support a targeted need. Instead, experts offered multiple recommendations through which eHealth could be optimally tailored to best support the complex and dynamic self-care processes in a way that accounts for the many influencing factors (see the qualitative data themes). The most outstanding optimisation strategies collected by the present study are summarised in as a visual joint-display of both quantitative and qualitative insights. The figure outlines examples of how eHealth design can be optimised to match distinct self-care needs. It centers on instances where eHealth (persuasive) design strategies were found to be most or least promising, according to the assessments of multidisciplinary experts.
Figure 5. Optimisation of eHealth persuasive design strategies to support self-care of patients with cardiovascular diseases, according to the views of experts.
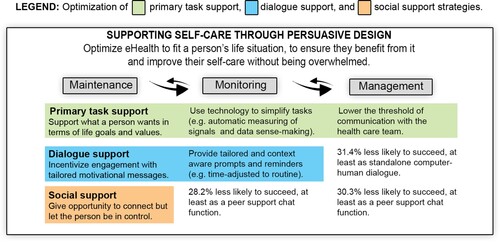
must be considered in light of the six major themes identified in the qualitative data, which provide an underlying context to the numerical ratings given by experts. Mainly, experts in this study highlighted that the key principles of patient-centeredness and the need to support collaboration between the patient and the health care team must always guide the tailoring process. This aligns with research that endorses the importance of patient-centeredness for self-care remote-support (Harst, Lantzsch, and Scheibe Citation2019; Harst, Timpel, and Otto Citation2020) and the collaboration between patients and health care providers (Nordfonn, Morken, and Bru Citation2019). Adding to that, experts pointed to many of the multidimensional factors that can increase the complexity of individual cases and thus hinder the potential success of any eHealth design strategy (e.g. availability of social support, comorbidities, attitudes and beliefs). This multifactorial, complex nature of self-care has been observed in previous works, especially in those that collect the experiences and perspectives of patients with CVD (Vo, Auroy, and Sarradon-Eck Citation2019; Harst, Timpel, and Otto Citation2020; Nordfonn, Morken, and Bru Citation2019).
Notably, several experts argued that an optimal eHealth design must ‘strive for simplicity’, which could be achievable by adjusting the pacing of the intervention and tailoring information to key factors such as literacy and culture (especially for dialogue support). Finally, experts suggested that eHealth is most optimally tailored when it targets problems where technology offers opportunities that other supportive solutions do not. For example, the availability of evidence-based knowledge about CVD and self-care via digital educational materials, the support for habituation to key healthy behaviours via prompts or reminders, or the facilitation of self-awareness and sense-making through self-monitoring and feedback.
4.3. Strengths and limitations
Naturally, this study had its strengths and limitations. One strength is that researchers from multidisciplinary fields of science were actually included. However, a limitation in that respect was that most respondents self-identified as ‘researchers’ rather than ‘developers/implementers’ or ‘health care providers’, which means the views of the latter are underrepresented. Moreover, the general approach of the study to involve only experts and not end users naturally limits its findings to a partial view on the matter. Certainly, neither this nor any single study can provide definitive answers to the question of how to tailor eHealth design strategies for self-care. However, the findings of this study are argued to be important because they display how the diverse views of experts can have an impact in the design of eHealth for self-care. In that regard, while there are multiple publications that collect the experiences and attitudes of patients towards eHealth, how experts use that knowledge to inform eHealth design had been harder to find in the literature.
Regarding the use of vignettes, while their presentation was pre-tested, two patient cases depicted in them were perceived by some experts to be less realistic. For instance, as several experts debated the representativeness of the monitoring case. Although Jane’s case (the patient depicted in that case) was inspired by interventions focusing on titration of medication for patients with uncontrolled hypertension, the vignette did not make this clear (Chandler, Sox, and Kellam Citation2019; Band, Bradbury, and Morton Citation2017). Because of this, the findings of the study must be considered in light of the specific operationalisation of factors used for the vignettes (e.g. the monitoring case presented as a patient with hypertension, or the social support strategy operationalised as a peer support chat function).
Additionally, it could be seen as a limitation that the data were collected through an online survey, making it impossible to be a hundred percent confident of the background of the respondents or their comprehension of the vignettes and survey questions. All of those aspects could have certainly influenced the results, and other methods with different aims could have led to different conclusions (e.g. a consensus-building Delphi study) (Wainwright, Gallagher, and Tompsett Citation2010). Finally, in terms of generalisability, it could be seen as a limitation that the study did not consider other categories or specific principles proposed by the PSD model (e.g. system credibility support such as third-party endorsements) or other promising approaches such as gamification (Radhakrishnan, Baranowski, and Julien Citation2019). However, the context-based evaluations that took place in the present study attempted to be a representation of real-life scenarios, where design choices by eHealth developers must be made in light of the target behaviours, context of use, and many other influencing factors. In short, since the tailoring of eHealth design must always be context-specific, enacting that context is exactly what the present study attempted to achieve with the use of vignettes.
4.4. Future work and opportunities in eHealth design for self-care
The findings of the present study add in to important ongoing discussions about eHealth design and development. While this study centered on the self-care needs as guiding determinants for tailoring, there are many other influencing factors that play a role as facilitators or barriers for self-care. Arguably, some factors such as motivation or social support have been extensively studied, while others such as personal values or cultural practices are influencing dimensions that require further exploration. For instance, there is already a body of knowledge about the roles of personal values among individuals with chronic conditions, but these works have not yet been translated to eHealth applications to self-care (Lim, Berry, and Hartzler Citation2019; Lim, Berry, and Hirsch Citation2017; Berry, Lim, and Hartzler Citation2017). Similarly, the influence of cultural factors has been studied in the specific context of CVD and self-care (Osokpo and Riegel Citation2019), and has been observed in investigations of eHealth persuasive design for other target behaviours, but nevertheless many questions remain (e.g. how to best tailor eHealth to cultural factors) (Orji, Nkwo, and Ajah Citation2021). Understanding how these factors can inform eHealth design could significantly enhance the effectiveness of self-care supportive interventions.
On the broadest view, the present study showed how theory can be used to create and propose potential design solutions (using vignettes) and how to collect not just opinions but contextualised and rich insights from experts with different backgrounds and areas of expertise (using a survey experiment). These contributions are important, because there is an ongoing debate about the usefulness of theory in the design and development of interventions (Hagger and Weed Citation2019). It must be noted that, as used in this study, theory-based vignettes are different from other typical representations such as personas because they focus on distinguishing behavioural patterns or needs and not on representing ‘average’ users (LeRouge, Ma, and Sneha Citation2013). In this regard, the research team will continue to study the use of vignettes as part of focused scenario-based testing for tailored (eHealth) interventions (Cornet, Daley, and Cavalcanti Citation2020).
5. Conclusions
The present study sought to identify the most promising eHealth design strategies that can support distinct self-care needs of individuals with a CVD. In that regard, the integrated views of experts from multiple scientific disciplines characterised primary task support as a promising support strategy for all theory-based self-care needs (maintenance, monitoring, and management). This type of support could be even seen as a prerequisite, as it could not only seek to simplify self-care tasks but also help ensure the safety of patients under the context of remote care. When compared to primary task support, social support was considered by experts to be less likely to succeed in supporting monitoring needs. Similarly, both dialogue and social support were less likely to succeed in supporting patients’ management needs. In practice, the findings of the present study suggest that eHealth design for self-care could benefit from a lean approach (i.e. ‘less is more’). The involvement of experts with diverse backgrounds and areas of expertise displayed various tailoriong approaches to the multidimensional complexity of individual self-care processes. Principally, experts suggested that interventions must be simplified by personalising their pacing to the personal circumstances of each patient (e.g. their knowledge and skills) and by tailoring the information they provide to their preferences (e.g. their literacy and culture). Above all, the results of the study endorse the view that eHealth design must distinctly address all theory-based self-care needs (maintenance, monitoring, and management), while embracing patient-centeredness (i.e. the alignment with the patients’ life personal goals and values) and facilitating the collaboration between patients and caregivers.
Acknowledgements
The authors would like to thank the researchers of the department of Psychology, Health and Technology of the University of Twente who contributed to the development and testing of vignettes and provided feedback on earlier materials and ideas for the study. The authors would also like to thank the expert participants who gave some of their valuable time for the research.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- Asbjørnsen, R. A., J. Wentzel, and M. L. Smedsrød. 2020. “Identifying Persuasive Design Principles and Behavior Change Techniques Supporting End User Values and Needs in eHealth Interventions for Long-Term Weight Loss Maintenance: Qualitative Study.” Journal of Medical Internet Research 22: e22598. doi:10.2196/22598.
- Atzmüller, C., and P. M. Steiner. 2010. “Experimental Vignette Studies in Survey Research.” Methodology: European Journal of Research Methods for the Behavioral and Social Sciences 6: 128–138. doi:10.1027/1614-2241/a000014.
- Auspurg, K., and T. Hinz. 2015. Factorial Survey Experiments. Thousand Oaks: SAGE Publications, Inc.
- Auspurg, K., and A. Jäckle. 2017. “First Equals Most Important? Order Effects in Vignette-Based Measurement.” Sociological Methods & Research 46: 490–539. doi:10.1177/0049124115591016.
- Band, R., K. Bradbury, and K. Morton. 2017. “Intervention Planning for a Digital Intervention for Self-Management of Hypertension: A Theory-, Evidence- and Person-Based Approach.” Implementation Science 12: 1–13. doi:10.1186/s13012-017-0553-4.
- Berry, A. B. L., C. Lim, and A. L. Hartzler. 2017. “Eliciting Values of Patients with Multiple Chronic Conditions: Evaluation of a Patient-centered Framework.” AMIA Annu Symp Proc, 430–439.
- Braun, V., and V. Clarke. 2006. “Using Thematic Analysis in Psychology.” Qualitative Research in Psychology 3: 77–101. doi:10.1191/1478088706qp063oa.
- Burns, C. 2018. Human-Centred Design. EHealth Research, Theory and Development. New York: Routledge.
- Cajita, M. I., N. A. Hodgson, and C. Budhathoki. 2017. “Intention to Use mHealth in Older Adults With Heart Failure.” The Journal of Cardiovascular Nursing 32: E1–E7. DOI:10.1097/jcn.0000000000000401.
- Chandler, J., L. Sox, and K. Kellam. 2019. “Impact of a Culturally Tailored mHealth Medication Regimen Self-Management Program Upon Blood Pressure among Hypertensive Hispanic Adults.” International Journal of Environmental Research and Public Health 16. doi:10.3390/ijerph16071226.
- Chantler, T., C. Paton, and C. Velardo. 2016. “Creating Connections – The Development of a Mobile-Health Monitoring System for Heart Failure: Qualitative Findings from a Usability Cohort Study.” Digital Health 2. doi:10.1177/2055207616671461.
- Cornet, V. P., C. Daley, and L. H. Cavalcanti. 2020. “Chapter 14 – Design for Self-Care.” In Design for Health, edited by A. Sethumadhavan, and F. Sasangohar, 277–302. London: Academic Press.
- Creswell, J. W., and V. L. P. Clark. 2017. Designing and Conducting Mixed Methods Research. Thousand Oaks: Sage.
- Cruz-Martínez, R. R., P. D. Noort, and R. A. Asbjørnsen. 2019. “Frameworks, Models, and Theories Used in Electronic Health Research and Development to Support Self-Management of Cardiovascular Diseases Through Remote Monitoring Technologies: Protocol for a Metaethnography Review.” Jmir Research Protocols 8: e13334. doi:10.2196/13334.
- Cruz-Martínez, R. R., F. Sieverink, and R. Wesselink. 2018. “Towards Data-Driven Persuasive Coaching in a Heart Failure Telemonitoring Technology.” In Proceedings of the 6th International Workshop on Behavior Change Support Systems co-located with the 13th International Conference on Persuasive Technology (PERSUASIVE 2018), 60–75.
- Cruz-Martínez, R. R., J. Wentzel, and R. A. Asbjørnsen. 2020. “Supporting Self-Management of Cardiovascular Diseases Through Remote Monitoring Technologies: Metaethnography Review of Frameworks, Models, and Theories Used in Research and Development.” Journal of Medical Internet Research 22: e16157. doi:10.2196/16157.
- Fetters, M. D., L. A. Curry, and J. W. Creswell. 2013. “Achieving Integration in Mixed Methods Designs-Principles and Practices.” Health Services Research 48: 2134–2156. doi:10.1111/1475-6773.12117.
- Fivecoat, H. C., S. L. Sayers, and B. Riegel. 2018. “Social Support Predicts Self-Care Confidence in Patients with Heart Failure.” European Journal of Cardiovascular Nursing. doi:10.1177/1474515118762800.
- Foster, M. 2018. “A Mobile Application for Patients With Heart Failure: Theory- and Evidence-Based Design and Testing.” Computers, Informatics, Nursing: CIN 36: 540–549. doi:10.1097/cin.0000000000000465.
- Garson, G. D. 2013. Hierarchical Linear Modeling: Guide and Applications. Thousand Oaks: SAGE Publications, Inc.
- Greenwood, D. A., P. M. Gee, and K. J. Fatkin. 2017. “A Systematic Review of Reviews Evaluating Technology-Enabled Diabetes Self-Management Education and Support.” Journal of Diabetes Science and Technology 11: 1015–1027. doi:10.1177/1932296817713506.
- Hagger, M. S., and M. Weed. 2019. “DEBATE: Do Interventions Based on Behavioral Theory Work in the Real World?” The International Journal of Behavioral Nutrition and Physical Activity 16: 36. doi:10.1186/s12966-019-0795-4.
- Haldane, V., J. J. K. Koh, and A. Srivastava. 2019. “User Preferences and Persona Design for an mHealth Intervention to Support Adherence to Cardiovascular Disease Medication in Singapore: A Multi-Method Study.” Jmir Mhealth and Uhealth 7: e10465. doi:10.2196/10465.
- Hanlon, P., L. Daines, and C. Campbell. 2017. “Telehealth Interventions to Support Self-Management of Long-Term Conditions: A Systematic Metareview of Diabetes, Heart Failure, Asthma, Chronic Obstructive Pulmonary Disease, and Cancer.” Journal of Medical Internet Research 19: e172. doi:10.2196/jmir.6688.
- Harst, L., H. Lantzsch, and M. Scheibe. 2019. “Theories Predicting End-User Acceptance of Telemedicine Use: Systematic Review.” Journal of Medical Internet Research 21: e13117. doi:10.2196/13117.
- Harst, L., P. Timpel, and L. Otto. 2020. “Identifying Barriers in Telemedicine-Supported Integrated Care Research: Scoping Reviews and Qualitative Content Analysis.” Journal of Public Health 28: 583–594. doi:10.1007/s10389-019-01065-5.
- Harvey, J., S. Dopson, and R. J. McManus. 2015. “Factors Influencing the Adoption of Self-Management Solutions: An Interpretive Synthesis of the Literature on Stakeholder Experiences.” Implementation Science: IS 10: 159. doi:10.1186/s13012-015-0350-x.
- Heck, R. H., S. Thomas, and L. Tabata. 2013. Multilevel Modeling of Categorical Outcomes Using IBM SPSS. New York: Routledge Academic.
- Hekler, E. B., S. Michie, and M. Pavel. 2016. “Advancing Models and Theories for Digital Behavior Change Interventions.” American Journal of Preventive Medicine 51: 825–832. doi:10.1016/j.amepre.2016.06.013.
- Jaarsma, T., A. Strömberg, and S. B. Dunbar. 2020. “Self-Care Research: How to Grow the Evidence Base?” International Journal of Nursing Studies 105: 103555. doi:10.1016/j.ijnurstu.2020.103555.
- Jackson, M., P. Harrison, and B. Swinburn. 2015. “Using a Qualitative Vignette to Explore a Complex Public Health Issue.” Qualitative Health Research 25: 1395–1409. doi:10.1177/1049732315570119.
- Kebapci, A., M. Ozkaynak, and S. C. Lareau. 2020. “Effects of eHealth-Based Interventions on Adherence to Components of Cardiac Rehabilitation: A Systematic Review.” The Journal of Cardiovascular Nursing 35: 74–85. doi:10.1097/JCN.0000000000000619.
- Kim, B. Y. B., and J. Lee. 2017. “Smart Devices for Older Adults Managing Chronic Disease: A Scoping Review.” Jmir Mhealth and Uhealth 5. doi:10.2196/mhealth.7141.
- Lentferink, A. J., H. K. Oldenhuis, and M. de Groot. 2017. “Key Components in eHealth Interventions Combining Self-Tracking and Persuasive eCoaching to Promote a Healthier Lifestyle: A Scoping Review.” Journal of Medical Internet Research 19: e277. doi:10.2196/jmir.7288.
- LeRouge, C., J. Ma, and S. Sneha. 2013. “User Profiles and Personas in the Design and Development of Consumer Health Technologies.” International Journal of Medical Informatics 82: E251–E268. doi:10.1016/j.ijmedinf.2011.03.006.
- Lim, C. Y., A. B. L. Berry, and A. L. Hartzler. 2019. “Facilitating Self-reflection about Values and Self-care Among Individuals with Chronic Conditions.” Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. Glasgow, Scotland, UK: Association for Computing Machinery, 655.
- Lim, C. Y., A. B. L. Berry, and T. Hirsch. 2017. “Understanding What is Most Important to Individuals with Multiple Chronic Conditions: A Qualitative Study of Patients’ Perspectives.” Journal of General Internal Medicine 32: 1278–1284. doi:10.1007/s11606-017-4154-3.
- Matarese, M., M. Lommi, and M. G. De Marinis. 2018. “A Systematic Review and Integration of Concept Analyses of Self-Care and Related Concepts.” Journal of Nursing Scholarship. doi:10.1111/jnu.12385.
- Mawson, S., N. Nasr, and J. Parker. 2016. “A Personalized Self-Management Rehabilitation System with an Intelligent Shoe for Stroke Survivors: A Realist Evaluation.” JMIR Rehabilitation and Assistive Technologies 3: e1. doi:10.2196/rehab.5079.
- Nordfonn, O. K., I. M. Morken, and L. E. Bru. 2019. “Patients’ Experience with Heart Failure Treatment and Self-Care – A Qualitative Study Exploring the Burden of Treatment.” Journal of Clinical Nursing 28: 1782–1793. doi:10.1111/jocn.14799.
- Oinas-Kukkonen, H., and M. Harjumaa. 2009. “Persuasive Systems Design: Key Issues, Process Model, and System Features.” Communications of the Association for Information Systems 24: 28.
- Orji, R., M. Nkwo, and I. Ajah. 2021. Design Opportunities for Persuasive Mobile Apps to Support Maternal and Child Healthcare and Help-Seeking Behaviors.
- Osokpo, O., and B. Riegel. 2019. “Cultural Factors Influencing Self-Care by Persons with Cardiovascular Disease: An Integrative Review.” International Journal of Nursing Studies, 103383. doi:10.1016/j.ijnurstu.2019.06.014.
- Oyebode, O., C. Ndulue, and D. Mulchandani. 2021. Tailoring Persuasive and Behaviour Change Systems Based on Stages of Change and Motivation.
- Radhakrishnan, K., T. Baranowski, and C. Julien. 2019. “Role of Digital Games in Self-Management of Cardiovascular Diseases: A Scoping Review.” Games for Health Journal 8: 65–73. doi:10.1089/g4 h.2018.0011.
- Riegel, B., S. B. Dunbar, and D. Fitzsimons. 2019a. “Self-Care Research: Where Are We Now? Where Are We Going?” International Journal of Nursing Studies, 103402. doi:10.1016/j.ijnurstu.2019.103402.
- Riegel, B., T. Jaarsma, and C. S. Lee. 2019b. “Integrating Symptoms into the Middle-Range Theory of Self-Care of Chronic Illness.” Advanced in Nursing Sciences 42: 206–215. doi:10.1097/ans.0000000000000237.
- Riegel, B., T. Jaarsma, and A. Stromberg. 2012. “A Middle-Range Theory of Self-Care of Chronic Illness.” ANS. Advances in Nursing Science 35: 194–204. doi:10.1097/ANS.0b013e318261b1ba.
- Riegel, B., D. K. Moser, and H. G. Buck. 2017. “Self-Care for the Prevention and Management of Cardiovascular Disease and Stroke: A Scientific Statement for Healthcare Professionals from the American Heart Association.” Journal of the American Heart Association 6. doi:10.1161/JAHA.117.006997.
- Roth, G. A., C. Johnson, and A. Abajobir. 2017. “Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015.” Journal of the American College of Cardiology 70: 1–25. doi:10.1016/j.jacc.2017.04.052.
- Steiner, P. M., C. Atzmüller, and D. Su. 2017. “Designing Valid and Reliable Vignette Experiments for Survey Research: A Case Study on the Fair Gender Income Gap.” Journal of Methods and Measurements in the Social Sciences 7: 43. doi:10.2458/v7i2.20321.
- Tadas, S., and D. Coyle. 2020. “Barriers to and Facilitators of Technology in Cardiac Rehabilitation and Self-Management: Systematic Qualitative Grounded Theory Review.” Journal of Medical Internet Research 22: e18025. doi:10.2196/18025.
- Toukhsati, S. R., T. Jaarsma, and A. S. Babu. 2019. “Self-Care Interventions That Reduce Hospital Readmissions in Patients With Heart Failure; Towards the Identification of Change Agents.” Clinical Medicine Insights: Cardiology 13. doi:10.1177/1179546819856855.
- Triantafyllidis, A., H. Kondylakis, and K. Votis. 2019. “Features, Outcomes, and Challenges in Mobile Health Interventions for Patients Living with Chronic Diseases: A Review of Systematic Reviews.” International Journal of Medical Informatics 132: 103984. doi:10.1016/j.ijmedinf.2019.103984.
- van Gemert-Pijnen, L. J., H. Kip, and S. M. Kelders. 2018. Introducing EHealth. EHealth Research, Theory and Development. New York: Routledge.
- van Gemert-Pijnen, J. E., N. Nijland, and M. van Limburg. 2011. “A Holistic Framework to Improve the Uptake and Impact of eHealth Technologies.” Journal of Medical Internet Research 13: e111. doi:10.2196/jmir.1672.
- van Velsen, L., M. Broekhuis, and S. Jansen-Kosterink. 2019. “Tailoring Persuasive Electronic Health Strategies for Older Adults on the Basis of Personal Motivation: Web-Based Survey Study.” Journal of Medical Internet Research 21: 11759. doi:10.2196/11759.
- Villarreal, V., and A. Berbey-Alvarez. 2020. “Evaluation of mHealth Applications Related to Cardiovascular Diseases: a Systematic Review.” Acta informatica Medica 28: 130–137. doi:10.5455/aim.2020.28.130-137.
- Vo, V., L. Auroy, and A. Sarradon-Eck. 2019. “Patients’ Perceptions of mHealth Apps: Meta-Ethnographic Review of Qualitative Studies.” Jmir Mhealth and Uhealth 7: e13817. doi:10.2196/13817.
- Wainwright, P., A. Gallagher, and H. Tompsett. 2010. “The Use of Vignettes Within a Delphi Exercise: A Useful Approach in Empirical Ethics?” Journal of Medical Ethics 36: 656–660. doi:10.1136/jme.2010.036616.
- Wais-Zechmann, B., V. Gattol, and K. Neureiter. 2018. Persuasive Technology to Support Chronic Health Conditions: Investigating the Optimal Persuasive Strategies for Persons with COPD. Cham: Springer International Publishing.
- Wildeboer, G., S. M. Kelders, and J. E. W. C. van Gemert-Pijnen. 2016. “The Relationship Between Persuasive Technology Principles, Adherence and Effect of Web-Based Interventions for Mental Health: A Meta-Analysis.” International Journal of Medical Informatics 96: 71–85. doi:10.1016/j.ijmedinf.2016.04.005.
- Won, M. H., and Y.-J. Son. 2016. “Perceived Social Support and Physical Activity Among Patients With Coronary Artery Disease.” Western Journal of Nursing Research 39: 1606–1623. doi:10.1177/0193945916678374.
- Woods, L. S., J. Duff, and E. Roehrer. 2019. “Patients’ Experiences of Using a Consumer mHealth App for Self-Management of Heart Failure: Mixed-Methods Study.” JMIR Hum Factors 6: e13009. doi:10.2196/13009.
Appendices
Appendix 1. Key study definitions
All of the key terms and concepts that were introduced in the paper are displayed below. These are accompanied by related, narrower or broader terms and definitions that reflect on the study’s understanding of eHealth.
Self-care needs
Self-care: The process of maintaining health through health promoting practices and managing illness, as specified in our prior work. As proposed by the Middle-Range Theory of Self-Care of Chronic Illness, self-care entails three key processes: maintenance, monitoring, and management (Riegel, Jaarsma, and Stromberg Citation2012; Riegel, Jaarsma, and Lee Citation2019).
Maintenance: The performance of behaviours to improve well-being, preserve health, or to maintain physical and emotional stability. The goal of maintenance is to maintain health and prevent symptom exacerbations (Riegel, Jaarsma, and Stromberg Citation2012; Riegel, Jaarsma, and Lee Citation2019).
Monitoring: The process of routine, vigilant body monitoring, surveillance, or ‘body listening’. The goal of monitoring is recognition that a change has occurred (Riegel, Jaarsma, and Stromberg Citation2012; Riegel, Jaarsma, and Lee Citation2019).
Management: The evaluation of changes in physical and emotional signs and symptoms to determine if action is needed. The goal of management is effective treatment of symptoms (Riegel, Jaarsma, and Stromberg Citation2012; Riegel, Jaarsma, and Lee Citation2019).
Persuasive systems design strategies
Persuasive systems: Computerised software or information systems designed to reinforce, change or shape attitudes or behaviours or both without using coercion or deception (Oinas-Kukkonen and Harjumaa Citation2009).
Primary task support: Persuasive design strategy that directly supports the user in carrying out a primary task (Oinas-Kukkonen and Harjumaa Citation2009).
Dialogue support: Persuasive design strategy that implements computer-human dialogue in a manner that helps the user move towards the goal or target behaviour (Oinas-Kukkonen and Harjumaa Citation2009).
Social support: Persuasive design strategy that seeks to motivate the user by leveraging social influence (Oinas-Kukkonen and Harjumaa Citation2009).
System credibility support: Persuasive design strategy that emphasises the expertise behind a system (Oinas-Kukkonen and Harjumaa Citation2009). This strategy was not included in the experiment because it was considered a prerequisite of all interventions (i.e. trust in novel eHealth remote support systems is a known important factor), while the first three categories were considered highly relevant and worth comparing.
Ehealth
eHealth: The use of technology to support health, well-being and health care (van Gemert-Pijnen, Kip, and Kelders Citation2018).
eHealth technology: The actual technological instrument via which health, well-being and health care are supported, often refers to information or communication technologies (van Gemert-Pijnen, Kip, and Kelders Citation2018).
eHealth intervention: An eHealth technology specifically focused on intervening in an existing context by changing behaviour and/or cognitions (van Gemert-Pijnen, Kip, and Kelders Citation2018).
Monitoring technologies: Technologies that allow the user to collect health-related data and often also share the patient’s data with a health care team. Examples of monitoring technologies are internet-enabled blood pressure monitors and weight scales.
Coaching technologies: Technologies that provide feedback, guidance, or recommendations to the patients. Coaching technologies are often designed as web-based, mobile, or wearable apps.
Expert selection criteria
Expertise: Defined as having cross-disciplinary or domain-specific knowledge in one of the key topics of the survey, which could include but not be limited to medical, behavioural, computer and informational sciences, engineering, design, human-technology interaction, human factors and ergonomics, and business or innovation.
Experience: Defined as having led, participated, or consulted in projects of relevance to the topics of the survey. The projects could be related to academia, health care institutions, private industry, or policy-making.