Abstract
Andersen’s Behavioural Model of Health Service Use (ABMHSU) is a multilevel model that helps understand the factors influencing health service access and utilisation. This framework is a widely used model for health service use in general, as well as in immigrant populations and vulnerable populations. ABMHSU, in this project, provided a framework to explain how the mental health nurses’ cultural competence can influence the Victorian CALD community members’ mental health care access and utilisation. A unique model of ABMHSU in the current multiple-method project provided a theoretical framework for examining the factors associated with people from the CALD community accessing mental health services in an Australian context to answer the research questions. The key findings of the research were discussed with reference to the extant literature and with triangulation of research results with the ABMHSU in the context of Victoria. The researchers argue that even though predisposing, enabling, and need factors are necessary to determine whether a person is selected for expert care for mental health issues, these factors alone are insufficient. Ongoing research is essential to ascertain the potential of mental health nurses’ cultural competence education and cultural responsiveness in addressing the mental health service access and utilisation of the heterogeneous CALD communities. Additional research is advocated to identify the supplementary factors, as there is a dearth of research exploring the potential of ABMHSU worldwide.
Introduction
Several researchers have extensively studied the relationship between globalisation and international migration and have examined the various dimensions and impacts of this phenomenon worldwide (Hossin, Citation2020; Petersen & Schramm, Citation2017; Renzaho, Citation2016). Research from Australia and overseas has highlighted that the migrant, refugee, and asylum seeker population universally are at high risk of mental health issues (Gleeson et al., Citation2020; Kirmayer et al., Citation2014; Minas, Citation2018; Rousseau & Frounfelker, Citation2019). However, several researchers have evidence that people with culturally and linguistically diverse backgrounds (CALD) are uneasy about seeking help from mental health services in their host countries despite the prevalence of mental health issues (Cross & Singh, Citation2012; Forrest, Citation2018; Rooney et al., Citation2014; Torres Stone et al., Citation2020). Victoria is one of Australia’s most multicultural states; its multicultural population grows yearly (Australian Bureau of Statistics, Citation2023). Hence, it is vital to explore the contextual factors that affect the CALD community’s access to and utilisation of mental health services in Victoria. Simultaneously, conducting studies based on a model that addresses most aspects of healthcare utilisation is valuable. These studies allow a nuanced understanding of the factors influencing CALD community healthcare access and utilisation. These understandings provide a foundation for informed decision-making and policy development to reduce health disparities. Andersen’s behavioural model of Health Service Use (Andersen et al., Citation2007) has been recognised as a multilevel model that helps to understand the factors influencing health service access and utilisation. This framework is a widely used model for health service use in general and immigrant populations and vulnerable populations like the elderly, refugees and asylum seekers, and homeless people (Yang & Hwang, Citation2016). In addition, Andersen’s model can be adapted to present the concepts that reflect mental health service use factors. Therefore, this model is applicable worldwide to explore issues related to mental health service access and utilisation. In this project, ABMHSU provided a framework to explain Victorian CALD community members’ health care access and utilisation and nurses’ cultural competence. For this research project, the term ‘CALD’ is defined as:
….[a]population [defined] mainly by country of birth, language spoken at home, English proficiency, or other characteristics (including the year of arrival in Australia), parents’ country of birth, and religious affiliations (Australian Institute of Health & Welfare, Citation2018).
This paper explains how a larger multiple-method study analysed the factors affecting the healthcare utilisation of the CALD community using Andersen’s Behavioural Model of Health Service Use. The key findings of the research were discussed with reference to the extant literature and with triangulation of research results with the ABMHSU in the context of Victoria.
The model
The health service utilisation of diverse populations has been explored using numerous models of care. These models not only elucidate but also predict the factors influencing health service utilisation (Khatri & Assefa, Citation2022; Shukla et al., Citation2020). In addition, within various disciplines, numerous models have been developed to investigate, predict, and project the intentions and behaviours of individuals in the utilisation of health care services. Healthcare utilisation refers to people using the healthcare system to prevent and cure health problems. This process also includes promoting health maintenance and well-being or gaining information about one’s health status and prognosis (Awoke et al., Citation2017). A need-based health care system objectively meets an individual’s needs from health professionals and predicts the demands of an individual. The healthcare system’s overuse, underuse and misuse can be avoided if this interface is successful. Otherwise, there is a possibility of compromising an individual’s health and burdening the health care system. Various contextual and individual factors determine the use of the health care system. Therefore, it is essential to consider the non-use of healthcare services to avoid the healthcare system’s overuse, underuse, and misuse (Lederle et al., Citation2021).
In health services research, the ABMHSU is a respected model for healthcare service access and utilisation (Tesfaye et al., Citation2018; Travers et al., Citation2020; Willet et al., Citation2018). ABMHSU is a product of the National Health Survey in the USA. This model has undergone many revisions and additions. These were to respond to evolving issues in health policy and health services delivery, input from the researchers, critiques of the earlier model versions, and new developments and research in various health disciplines. However, the revisions have not altered the model’s fundamental notions and relationships. Additionally, the ABMHSU has been reiterated several times (Andersen et al., Citation2007; Babitsch et al., Citation2012; Lederle et al., Citation2021).
According to Andersen et al. (Citation2014), the model suggests the significant components of contextual characteristics are divided in the same way as individual characteristics determining access: (a) Existing conditions that predispose people to use or not use services even though the conditions are not directly accountable for the use (b) Enabling conditions that facilitate or hinder the use of services and (c) need or conditions that ordinary people or health care service providers identify as requiring medical management. Andersen’s model emphasises contextual factors in acknowledging the importance of community, the structure and process of providing care and the realities of a managed care environment. Nevertheless, the model’s ultimate focus stays on individuals’ health behaviour, especially the use and resulting outcomes regarding their health, satisfaction with the services and quality of life. Andersen et al. (Citation2014) explain each model’s significant component as shown in .
Table 1. Summarises the various characteristics under each component of ABMHSU and provides examples to illustrate each point.
The model is expected to assist in realising that the perceived need helps us better understand the healthcare-seeking process of the individual and their adherence to a medical regimen (Gu & Dupre, Citation2021). Andersen et al. (Citation2014) hypothesised that the predisposing, enabling and need factors would have differential capacities to explain use, depending on the nature of the examined service. For instance, in response to a severe condition, hospital service use would be mainly described by need and demographic characteristics. On the other hand, service access to chronic conditions (such as dental services) would be more likely to be explained by social conditions, health beliefs, enabling resources and severity of symptoms (Lederle et al., Citation2021). Still, the ultimate aim of improved access is to reduce the individual’s perceived needs.
How is Andersen’s model relevant to the current study?
Even though mental health system reforms have been working on enhancing mental health services to be equitable, accessible, and inclusive of the diversity of Australians, gaps remain in health care access and disparities in terms of mental health treatment (Burgess et al., Citation2002; Forrest, Citation2018; Torres Stone et al., Citation2020). It is vital to explore the contextual factors that affect the access and utilisation of mental health services by culturally and linguistically diverse communities across Australia. Additionally, many researchers have recommended improving mental health professionals’ knowledge of cultural responsiveness and mental health service provision to reduce health discrepancies (Betancourt et al., Citation2014; Jongen et al., Citation2018; Oikarainen et al., Citation2019; Truong et al., Citation2014). As demonstrated by Aguiar et al. (Citation2012), McDonough et al. (Citation2013), Owiti et al. (Citation2014), Kverno (Citation2016), and Santhanam-Martin et al. (Citation2017), this, consecutively, will enhance CALD community access to mental health services. The current project examined and analysed this strategy in detail using multiple methodologies. ABMHSU was the theoretical framework for this project.
Methodology
After obtaining the final ethics approval from xxx University, Australia, the three-phased multiple-method project. During Phase 1, this project conducted telephone interviews with people from CALD communities in Victoria to examine their experience with health care, especially mental health services and an online survey for Mental Health Nurse (MHN) participants working in the mental health service department of a metropolitan hospital to do the gap analysis. A modified Cultural Competence Assessment instrument (CCA) (Schim et al., Citation2003; Citation2007) was used as the survey instrument to measure the cultural diversity experience, cultural competence behaviours and cultural awareness and sensitivity. Based on the Phase 1 results, an education package for MHNs was prepared and rolled out along with a post-intervention survey for MHNs during Phase 2. Phase 3 of the project evaluated the effectiveness of the education package using results from a 3-month post-intervention survey and semi-structured interviews with MHNs. (The details of the project phases are not provided in this paper).
Findings
The findings from the TI with CALD community members identified multiple barriers to and a lack of understanding of mental health services. These barriers included cultural beliefs about mental health issues, previous experiences with mental health services, stigma, labelling discrimination, language barriers, issues with interpreters, mental health service access issues, and lack of quality time with GPs and other health care professionals (Radhamony et al., Citation2023). The Phase 1 results of the project indicated the educational gaps of MHNs in assisting the CALD community in accessing and utilising mental health services. An online education package, ‘Acknowledging Diversity’, was developed and implemented in Phase 2 to assist the MHNs in improving their knowledge, attitude, and behaviour while caring for the CALD community.
MHNs rated their baseline knowledge, behaviour, and attitude highly on the baseline survey but were less confident on follow-up surveys. MHNs reported that the education package was a refresher for them and assisted them in becoming more self-aware. MHN's attitude to the challenges of caring for CALD consumers showed they were willing to learn about CD and flexible in achieving cultural congruence. Individual and system issues were identified as barriers to CC care. MHNs emphasised the need for more resources for CALD communities and reported that they were partially aware of the full range of services available for CALD communities. The Phase 3 online survey results showed no statistically significant change in the cultural competence behaviours and cultural awareness and sensitivity of the MHNs across the three phases.
The results from all phases were triangulated to answer the research questions. The project results suggested that the education package effectively improved MHNs’ cultural competence behaviours, cultural awareness, and sensitivity, even though the results were not statistically significant. The present study supports previous studies that established that education could improve MHNs’ knowledge, and the need for continuous education and training of mental health professionals in providing culturally congruent care to CALD communities has been widely recognised. The overall findings of the study indicated the need to improve the experiences of the CALD community within health facilities and through the empowerment of health professionals. MH illiteracy (lack of knowledge of MH issues and available MH services) was found to be a barrier for the CALD community accessing and utilising MH services (Radhamony et al., Citation2023).
A unique model of ABMHSU in the current project provided a theoretical framework for examining the factors associated with CALD community access to mental health services to answer the research questions. The current research findings on mental health care access and utilisation by the CALD communities were explained using the ABMHSU. The inter-relationships among the results of each phase of the study were determined using ABMHSU. Moreover, to our knowledge, no previous study in Australia has analysed the variables in the multidimensional ABMHSU for CALD community mental health service access and utilisation.
Discussion
Andersen’s Behavioural Model of Health Service Use (ABMHSU) is mainly used in research to examine healthcare in general without focusing on specific diseases. However, many studies have focused on specific care settings, such as nursing and mental health services. Additionally, ABMHSU has been adapted and utilised extensively in many studies investigating health services for diverse populations (Babitsch et al., Citation2012; Chen et al., Citation2016; Lengerke et al., Citation2014; Woolfenden et al., Citation2015).
The ABMHSU was used as a guiding framework, and the study did not aim to test the model. This multiple-method project considered qualitative and quantitative methods for analysing and recording detailed descriptions and complex mental healthcare service utilisation issues. ABMHSU informed an examination of mental health service utilisation. The impact of predisposing, enabling and need factors to utilise mental health services among the CALD community members were analysed. Health disparities exist among CALD communities in Victoria regarding mental health service access and utilisation, and improving the knowledge of mental health professionals regarding cultural responsiveness was one of the suggested strategies to improve the situation (Radhamony et al., Citation2021).
Factors affecting utilisation are cultural, socio-demographic, access-related issues, and institutional factors such as lack of awareness of services and previous service use experience (Centre for Multicultural Youth, Citation2014; Colucci et al., Citation2015; Radhamony et al., Citation2023). The project outcomes illustrated how the practices around mental health service utilisation are the product of interplay between many different factors at the consumer, health provider and health system levels. ABMHSU provides a framework for this project by conceptualising the enabling, predisposing and need factors. Following these three factors, the outcomes of this project suggest that mental health service utilisation could be significantly improved (in the study focus) by modifying the CALD characteristics in line with ABMHSU.
This project analysed conceptual characteristics consistent with the ABMHSU () and examined the CALD characteristics conclusively. Utilising the ABMHSU, the current study considered the contextual variables for the people from the CALD community in Victoria as:
Figure 1. Adapting ABMHSU to explain the current research project.
Source: Adapted from Andersen, R., Davidson, P., & Sebastian, E. (2014). Improving Access to Care in Kominski Changing the US Health Care System. In (pp. 33–68).
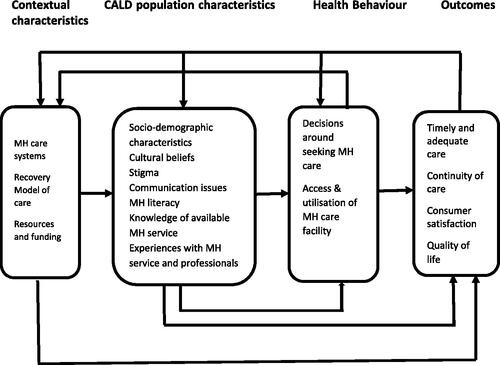
Mental health care systems: Various levels of mental health care systems exist in Victoria, such as primary, secondary, and tertiary levels, to meet the MH needs of the population.
Recovery Model of Care: The recovery model is a holistic, person-centred approach to mental health care currently followed in the Victorian mental health care system. The model is based on the notion that it is possible to recover from a mental health condition, and the most effective recovery is patient-centred.
Resources and funding: The national mental health plans and strategies and the allocated funding for mental health care, government, and stakeholder interventions in Victoria to cater to the diverse population’s cultural needs.
In line with the individual characteristics in the ABMHSU, the variables considered in the current study are:
Socio-demographic characteristics, cultural beliefs, stigma, language barriers and communication issues, MH literacy, knowledge of available mental health services and experiences with mental health services and professionals. These factors were identified in the interviews with the CALD community members and were discussed earlier in this article.
As per the ABMHSU, health behaviours can be influenced by contextual and individual characteristics. So, the variables considered in the health behaviours of the CALD participants are decisions around seeking MH care, access, and utilisation of MH services. The outcome factors considered for the CALD community in the current study were timely and adequate care for mental health issues and continuity of care. These factors can lead to consumer satisfaction and improved quality of life.
explains the ABMHSU model in relation to the current project results related to the CALD community that are pliable for modification. The integration of the study findings is visually represented and mapped onto the components of the ABMHSU in . In the context of Victoria, the government’s and stakeholders’ interventions to enhance people from the CALD community accessing and utilising MH services are explained using the predisposing, enabling, and need factors.
The telephone interview (TI) results with the CALD community members highlighted the predisposing factors such as socio-demographic characteristics, cultural beliefs, stigma, knowledge of available MH services, and experiences with MH services and professionals. Hence, in a Victorian context, the government and stakeholders could target these factors to abate the underutilisation of MH care services. In addition, the TIs assisted in identifying the CALD community members’ understanding, needs, and experiences with MH services and developing innovative ideas for enhancing the CALD community’s understanding and utilisation of the services (Radhamony et al., Citation2023).
Similarly, the enabling factors include implementing MH policies for equitable access, funding for more CALD-appropriate MH services, and availability of cultural portfolio holders and interpreters in the organisation. However, the most significant enabling factor is improving the knowledge of MH professionals, including MHNs (identified from the literature review, online surveys, and SSIs in the current study). These factors can also enhance CALD community access and utilisation of MH services in Victoria. Therefore, the ABMHSU contemplated the enabling variables at the contextual and individual levels to measure the potential access to services. The need factors included the symptoms related to MH issues or disability and improved CALD community understanding of MH services as potential areas of intervention. ABMHSU considers that predisposing factors, social characteristics, and health beliefs can influence the perceived and evaluated needs of the individual. Simultaneously, perceived needs such as awareness of one’s mental health issues and comorbidities can lead to the decision to seek MH care or to disregard the care.
As illustrated in , the interventions for the predisposing factors for the CALD community resulted in improved CALD MH literacy, enabling factors resulted in improved culturally competent behaviours (CCB) and cultural awareness and sensitivity (CAS) of MHNs (due to cultural competence education), and interventions for need factors lead to the provision of culturally congruent MH care. These modified factors (CALD MH literacy, improved CCB and CAS of MHNs and culturally congruent care) can interrelate and facilitate the achievement of enhanced CALD community access to MH services, leading to the recovery goals of care. Consequently, there will be consumer satisfaction and improved quality of life (Andersen et al., Citation2007; Citation2011; Citation2014).
Figure 2. Modifiable population characteristics of ABMHSU for CALD communities in Victoria.
Source: Model adapted from: (Tesfaye et al., Citation2018).
*CCB – cultural Competence Behaviours, *CAS – Cultural Awareness and Sensitivity.
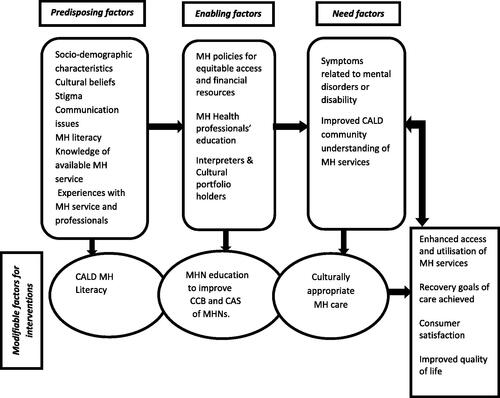
Thus, using the ABMHSU, the current study attempted to explain the contextual and individual characteristics determining the CALD community’s access and utilisation of mental health services in Victoria. These factors include the ‘existing conditions’ that predispose people to use or neglect mental health services even though these conditions are not directly responsible for the use. Similarly, ‘Enabling conditions’ that facilitate or impede the use of service and the ‘need factors’ that lay people from CALD community or health care providers recognise as requiring mental health service (Andersen, Citation1995, Citation2008; Andersen et al., CitationCitation2007, Citation2011, Citation2014). However, Dhingra et al. (Citation2010) propose that public MH services should consider health service utilisation as socially patterned and not just individual behaviour. The researchers argue that even though predisposing, enabling and need factors are principal in determining whether a person perceives professional care for mental or emotional problems, these factors alone are insufficient.
Strengths and limitations of this study
This study used the ABMHSU as the theoretical framework and explored the possibilities of the model in explaining the mental health service use of the CALD community in Victoria. Furthermore, this study is the first in Australia to analyse the variables in the multidimensional ABMHSU for CALD community mental health service access and utilisation. Similar to the Lederle et al. (Citation2021) study, ABMHSU could identify and explain the factors affecting CALD community access and utilisation in the context of Victoria from its qualitative and quantitative components’ findings of the current study. Future research related to access and utilisation of the CALD community to MH services should include ABMHSU and explore its potential.
Implications to practice
The findings from the current project have implications for health services, mental health nursing practice, mental health nursing education and research. In addition, the current study findings have important implications for mental health care delivery, with MHNs identified as fundamental to the planning, coordination and referral to services and supports. Future research on consumer outcomes and measures of equity, as well as the effectiveness and efficiency of the service outcomes, are needed to inform future policy and organisation of mental health services for the CALD population. Future research on access and utilisation of the CALD community to MH services should include ABMHSU and explore its potential, as this model is adaptable for CALD research worldwide. More detailed research examining health and healthcare disparities refines what is known while adding new findings related to several variables that this study had not investigated.
Conclusion
Thus, using the ABMHSU, the current study attempted to suggest the modifiable factors as proposed by the results of the qualitative and quantitative components of the study to improve MH care utilisation by the CALD community in Victoria. This multi-method project has used the ABMHSU as the theoretical framework and explored the possibilities of the model explaining the mental health service use of the CALD communities. The mental health service use of CALD communities in Victoria is associated with the need factors being the most potent predictor after we accounted for the predisposing, enabling and need factors. However, these needs are determined by several factors, such as mental health literacy, cultural beliefs, and knowledge about mental health services. There is a gap in research regarding the analysis of the variables of multidimensional ABMHSU. To fill this gap, researchers may explore cultural factors, language barriers, socioeconomic conditions, and other pertinent variables that could impact the access and utilisation of mental health services by CALD communities. These investigations may provide a comprehensive understanding of the complex dynamics influencing mental health care outcomes in these populations. Likewise, the implementation and evaluation of the national mental health and well-being policies are warranted as the CALD community in Victoria expands.
Further research is essential to ascertain the potential of MHNs’ cultural competence education and cultural responsiveness in addressing the mental health service access and utilisation of CALD communities. Additionally, research is advocated to identify the supplementary factors as there is a dearth of research globally exploring the potential of ABMHSU in the context of the CALD community accessing and utilising mental health services worldwide. These investigations will provide valuable insights into the unique challenges and opportunities present within this context.
Authors’ contributions
RR conducted the study and wrote and developed the manuscript. WC, LT and BB critically reviewed the manuscript. All authors approved the final manuscript, confirmed they met the authorship criteria and agreed with its content.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Federation University, Australia (Project Number - A20-024, Date of Approval: 30 September 2020).
Acknowledgement
The authors are grateful to the Federation University, Australia, for supporting the research and Austin Health for facilitating the data collection. We would also like to thank all study participants.
Disclosure statement of funding
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Aguiar, M. I. F. d., Lima, H. d P., Braga, V. A. B., Aquino, P. d S., Pinheiro, A. K. B., & Ximenes, L. B. (2012). Nurse competencies for health promotion in the mental health context. Acta Paulista de Enfermagem, 25(spe2), 157–163. https://doi.org/10.1590/S0103-21002012000900025
- Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36(1), 1–10.
- Andersen, R. M. (2008). National health surveys and the behavioral model of health services use. Medical Care, 46(7), 647–653.
- Andersen, R. M., Davidson, P. L., & Baumeister, S. E. (2007). Improving access to care in America. Changing the US health care system: key issues in health services policy and management (3a. ed., pp. 3–31). Jossey-Bass.
- Andersen, R. M., Rice, T. H., & Kominski, G. F. (2011). Changing the US health care system, CafeScribe: Key issues in health services policy and management. John Wiley & Sons.
- Andersen, R., Davidson, P., & Sebastian, E. (2014). Improving access to care in Kominski changing the US health care system. pp. 33–68. https://www.semanticscholar.org/paper/Improving-Access-to-Care-in-America%3A-Individual-and-Andersen-Davidson/1219ae558b20775ff8f4821eee84445d540c4b4c
- Australian Bureau of Statistics. (2023). Australian demographic statistics. https://www.abs.gov.au/ausstats/[email protected]/0/D56C4A3E41586764CA2581A70015893E?Opendocument
- Australian Institute of Health and Welfare. (2018). Australia’s health 2018 (AUS 221). AIHW.
- Awoke, M. A., Negin, J., Moller, J., Farell, P., Yawson, A. E., Biritwum, R. B., & Kowal, P. (2017). Predictors of public and private healthcare utilization and associated health system responsiveness among older adults in Ghana. Global Health Action, 10(1), 1301723. https://doi.org/10.1080/16549716.2017.1301723
- Babitsch, B., Gohl, D., & Von Lengerke, T. (2012). Re-revisiting Andersen’s behavioral model of health services use: A systematic review of studies from 1998-20. GMS Psycho-Social-Medicine, 9, 11.
- Betancourt, J. R., Corbett, J., & Bondaryk, M. R. (2014). Addressing disparities and achieving equity: Cultural competence, ethics, and health-care transformation. Chest, 145(1), 143–148. https://www.ncbi.nlm.nih.gov/pubmed/24394825
- Burgess, P., Pirkis, J., Buckingham, B., Eagar, K., & Eckstein, G. (2002). Mental health needs and expenditure in Australia. Mental Health and Special Programs Branch. https://www.researchgate.net/publication/43493726_Mental_Health_Needs_and_Expenditure_in_Australia
- Centre for Multicultural Youth. (2014). Mind Matters - The mental health and wellbeing of young people from diverse cultural backgrounds. https://www.cmy.net.au/resource/mind-matters-the-mental-health-and-wellbeing-of-young-people-from-diverse-cultural-backgrounds/
- Chen, J., Vargas-Bustamante, A., Mortensen, K., & Ortega, A. N. (2016). Racial and ethnic disparities in health care access and utilization under the Affordable Care Act. Medical Care, 54(2), 140–146. https://doi.org/10.1097/MLR.0000000000000467
- Colucci, E., Minas, H., Szwarc, J., Guerra, C., & Paxton, G. (2015). In or out? Barriers and facilitators to refugee-background young people accessing mental health services. Transcultural Psychiatry, 52(6), 766–790. Retrieved Dec from, https://www.ncbi.nlm.nih.gov/pubmed/25731986
- Cross, W., & Singh, C. (2012). Dual vulnerabilities: Mental illness in a culturally and linguistically diverse society. Contemporary Nurse, 42(2), 156–166. https://www.ncbi.nlm.nih.gov/pubmed/23181368
- Dhingra, S. S., Zack, M., Strine, T., Pearson, W. S., & Balluz, L. (2010). Determining prevalence and correlates of psychiatric treatment with Andersen’s behavioral model of health services use. Psychiatric Services (Washington, D.C.), 61(5), 524–528. https://doi.org/10.1176/ps.2010.61.5.524
- Forrest, S. (2018). Review of Cultural and Linguistic Diversity (CaLD) Data Collection Practices in the WA Health System. Department of Health, Western Australia.
- Gleeson, C., Frost, R., Sherwood, L., Shevlin, M., Hyland, P., Halpin, R., Murphy, J., & Silove, D. (2020). Post-migration factors and mental health outcomes in asylum-seeking and refugee populations: A systematic review. European Journal of Psychotraumatology, 11(1), 1793567. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7717836/pdf/ZEPT_11_1793567.pdf
- Gu, D., & Dupre, M. E.. (Eds). (2021). Encyclopedia of gerontology and population aging. Springer International Publishing.
- Hossin, M. Z. (2020). International migration and health: It is time to go beyond conventional theoretical frameworks. BMJ Global Health, 5(2), e001938. https://doi.org/10.1136/bmjgh-2019-001938
- Jongen, C., McCalman, J., & Bainbridge, R. (2018). Health workforce cultural competency interventions: A systematic scoping review. BMC Health Services Research, 18(1), 232. https://www.ncbi.nlm.nih.gov/pubmed/29609614
- Khatri, R. B., & Assefa, Y. (2022). Access to health services among culturally and linguistically diverse populations in the Australian universal health care system: Issues and challenges. BMC Public Health, 22(1), 880. https://www.ncbi.nlm.nih.gov/pubmed/35505307
- Kirmayer, L. J., Guzder, J., & Rousseau, C., editors. (2014). Cultural consultation: Encountering the other in mental health care. Springer.
- Kverno, K. (2016). Promoting access through integrated mental health care education. The Open Nursing Journal, 10(1), 73–77. https://doi.org/10.2174/187443460160101073
- Lederle, M., Tempes, J., & Bitzer, E. M. (2021). Application of Andersen’s behavioural model of health services use: A scoping review with a focus on qualitative health services research. BMJ Open, 11(5), e045018. https://www.ncbi.nlm.nih.gov/pubmed/33952550
- Lengerke, T. v., Gohl, D., & Babitsch, B. (2014). Re-revisiting the behavioral model of health care utilization by Andersen: A review on theoretical advances and perspectives. In T. v. Lengerke, D. Gohl, B. Babitsch, & C. Janssen (Eds.), Health care utilization in Germany: Theory, methodology, and results (pp. 11–28). Springer.
- McDonough, S., Chopra, P., Tuncer, C., Schumacher, B., & Bhat, R. (2013). Enhancing cultural responsiveness: The development of a pilot transcultural secondary consultation program. Australasian Psychiatry: Bulletin of Royal Australian and New Zealand College of Psychiatrists, 21(5), 494–498. https://www.ncbi.nlm.nih.gov/pubmed/23996791
- Minas, H. (2018). Mental health in multicultural australia. (B. D. Moussaoui, & Ventriglio A, Eds.) Springer. https://link.springer.com/content/pdf/10.1007/978-981-10-0750-7_10-1.pdf
- Oikarainen, A., Mikkonen, K., Kenny, A., Tomietto, M., Tuomikoski, A.-M., Meriläinen, M., Miettunen, J., & Kääriäinen, M. (2019). Educational interventions designed to develop nurses’ cultural competence: A systematic review. International Journal of Nursing Studies, 98, 75–86. https://www.ncbi.nlm.nih.gov/pubmed/31319338
- Owiti, J. A., Ajaz, A., Ascoli, M., de Jongh, B., Palinski, A., & Bhui, K. S. (2014). Cultural consultation as a model for training multidisciplinary mental healthcare professionals in cultural competence skills: Preliminary results. Journal of Psychiatric and Mental Health Nursing, 21(9), 814–826. https://doi.org/10.1111/jpm.12124
- Petersen, A. R., & Schramm, M. (2017). (Post-)Migration in the age of globalisation: New challenges to imagination and representation. Journal of Aesthetics & Culture, 9(2), 1–12. https://doi.org/10.1080/20004214.2017.1356178
- Radhamony, R., Cross, W. M., & Townsin, L. (2021). Nursing education to enhance culturally and linguistically diverse (CALD) community access to mental health services: A scoping review. Issues in Mental Health Nursing, 42(11), 1048–1063.
- Radhamony, R., Cross, W. M., Townsin, L., & Banik, B. (2023). Perspectives of culturally and linguistically diverse (CALD) community members regarding mental health services: A qualitative analysis. Journal of Psychiatric and Mental Health Nursing, 30(4), 850–864. https://doi.org/10.1111/jpm.12919
- Renzaho, A. M. (2016). Globalisation, migration and health: Challenges and opportunities. Imperial College Press.
- Rooney, R., Wright, B., & O’Neil, K. (2014). Issues faced by carers of people with a mental illness from culturally and linguistically diverse backgrounds: Carers’ and practitioners’ perceptions. Australian e-Journal for the Advancement of Mental Health, 5(2), 132–144. https://doi.org/10.5172/jamh.5.2.132
- Rousseau, C., & Frounfelker, R. L. (2019). Mental health needs and services for migrants: An overview for primary care providers. Journal of Travel Medicine, 26(2), 1–8. https://www.ncbi.nlm.nih.gov/pubmed/30561687
- Santhanam-Martin, R., Fraser, N., Jenkins, A., & Tuncer, C. (2017). Evaluation of cultural responsiveness using a transcultural secondary consultation model. Transcultural Psychiatry, 54(4), 488–501. https://www.ncbi.nlm.nih.gov/pubmed/28776452
- Schim, S. M., Doorenbos, A. Z., Miller, J., & Benkert, R. (2003). Development of a cultural competence assessment instrument. Journal of Nursing Measurement, 11(1), 29–40. https://www.ncbi.nlm.nih.gov/pubmed/15132010
- Schim, S. M., Doorenbos, A., Benkert, R., & Miller, J. (2007). Culturally congruent care: Putting the puzzle together. Journal of Transcultural Nursing, 18(2), 103–110. https://www.ncbi.nlm.nih.gov/pubmed/17416711
- Shukla, N., Pradhan, B., Dikshit, A., Chakraborty, S., & Alamri, A. M. (2020). A review of models used for investigating barriers to healthcare access in Australia. International Journal of Environmental Research and Public Health, 17(11), 4087. https://doi.org/10.3390/ijerph17114087
- Tesfaye, G., Chojenta, C., Smith, R., & Loxton, D. (2018). Application of the Andersen-Newman model of health care utilization to understand antenatal care use in Kersa District, Eastern Ethiopia. PLos One, 13(12), e0208729. https://doi.org/10.1371/journal.pone.0208729
- Torres Stone, R. A., Cardemil, E. V., Keefe, K., Bik, P., Dyer, Z., & Clark, K. E. (2020). A community mental health needs assessment of a racially and ethnically diverse population in New England: Narratives from community stakeholders. Community Mental Health Journal, 56(5), 947–958. https://www.ncbi.nlm.nih.gov/pubmed/32006294
- Travers, J. L., Hirschman, K. B., & Naylor, M. D. (2020). Adapting Andersen’s expanded behavioral model of health services use to include older adults receiving long-term services and supports. BMC Geriatrics, 20(1), 58. https://www.ncbi.nlm.nih.gov/pubmed/32059643
- Truong, M., Paradies, Y., & Priest, N. (2014). Interventions to improve cultural competency in healthcare: A systematic review of reviews. BMC Health Services Research, 14(1), 99. https://bmchealthservres.biomedcentral.com/track/pdf/10.1186/1472-6963-14-99
- Willet, M., Dorstyn, D., Due, C., & Li, W. (2018). Applying Andersen’s model to explain service use and quality of life among Australian caregivers of children with autism spectrum disorder. Journal of Developmental and Physical Disabilities, 30(3), 339–354. https://doi.org/10.1007/s10882-018-9589-x
- Woolfenden, S., Posada, N., Krchnakova, R., Crawford, J., Gilbert, J., Jursik, B., Sarkozy, V., Perkins, D., & Kemp, L. (2015). Equitable access to developmental surveillance and early intervention–understanding the barriers for children from culturally and linguistically diverse (CALD) backgrounds. Health Expect, 18(6), 3286–3301. Retrieved Dec, from, https://www.ncbi.nlm.nih.gov/pubmed/25510182
- Yang, P. Q., & Hwang, S. H. (2016). Explaining immigrant health service utilization. SAGE Open, 6(2), 215824401664813. https://doi.org/10.1177/2158244016648137
