ABSTRACT
Background
Stroke is a major cause of death and disability worldwide and presents a significant burden on healthcare systems. This retrospective study aims to analyze the characteristics and outcomes of stroke patients admitted to Hamad General Hospital (HGH) stroke service in Qatar from January 2014 to July 2022.
Methods
The medical records of 15,859 patients admitted during the study period were analyzed. The data collected included patient demographics, stroke types, admission location, procedures performed, mortality rates, and other clinical characteristics.
Results
Of the total cohort, 70.9% were diagnosed with a stroke, and 29.1% were diagnosed with stroke mimics. Of the stroke patients, 85.3% had an ischemic stroke, and 14.7% had a hemorrhagic stroke. Male patients below 65 years old (80.2%) and of South Asian ethnicity (44.6%) were the most affected. The mortality rate was 4.6%, significantly higher for hemorrhagic stroke than ischemic stroke (12.6% vs. 3.2%). Female patients had a higher stroke-related mortality rate than male patients (6.8% vs. 4%). The thrombolysis rate was 9.5%, and the thrombectomy rate was 3.4% of the ischemic stroke cohort. The mean door-to-needle time for thrombolysis was 61.2 minutes, and the mean door-to-groin time for thrombectomy was 170 minutes. Stroke outcomes were good, with 59.3% of patients having favorable outcomes upon discharge (mRS ≤2), which improved to 68.2% 90 days after discharge.
Conclusion
This study provides valuable insights into stroke characteristics and outcomes in Qatar. The findings suggest that stroke mortality rates are low, and favorable long-term disability outcomes are achievable. However, the study identified a higher stroke-related mortality rate among female patients and areas for improvement in thrombolysis and thrombectomy time.
Introduction
According to the 2022 Global Stroke Fact Sheet released by the World Stroke Organization (WSO), stroke is a major cause of mortality and morbidity worldwide, ranking second as a cause of death and third as a cause of death and disability combined. Unfortunately, the lifetime risk of experiencing a stroke has risen by 50% over the past 17 years, with an estimated 1 in 4 people expected to suffer from this condition during their lifetime [Citation1]. Furthermore, recent reports suggest that there is a growing stroke pandemic, with stroke incidence increasing by 70%, deaths due to stroke by 43%, stroke prevalence by 102%, and Disability Adjusted Life Years (DALY) by 143% [Citation2,Citation3].
Jaberinezhad and colleagues have reported that the burden of stroke in the Middle East and North Africa (MENA) region has decreased over the past 30 years, following a global trend. However, the decline has been less steep. The researchers found that there were more than 7 million prevalent stroke cases in the MENA region in 2019, with 312.2 thousand deaths, resulting in an age-standardized rate of 87.7 (78.2–97.6) per 100,000 population and 7.9 million Disability Adjusted Life Years (DALYs), with an age-standardized rate of 1826.2 (1635.3–2026.2) [Citation4].
Qatar is a wealthy peninsula on the Northeastern border of the Arabian Peninsula, with a native Qatari population comprising only 15% of the total population [Citation5]. However, despite the country’s affluence, Qatar faces significant public health challenges, such as a high prevalence of obesity, diabetes mellitus (DM), and cardiovascular disease [Citation6]. In 2020, Qatar ranked 15th globally for obesity, with more than 35% of the population affected by this condition. Additionally, around 16% of the population was diagnosed with DM in 2013 [Citation7]. Despite these concerning statistics, Qatar has a relatively low stroke incidence rate of 58 per 100,000 people, significantly lower than the MENA region’s rate, which reaches 250 per 100,000 people [Citation8,Citation9]. Qatar has a significant population of expatriates, primarily from the Indian subcontinent, who are of working age, and this may explain the relatively lower mean age of stroke patients in Qatar compared to the global average [Citation5,Citation10]. However, the mean age of Qatari stroke patients is higher than that of other stroke patients in Qatar [Citation11,Citation12]. Notably, women in Qatar tend to have higher mortality and disability rates than men, which may be attributed to their older age at presentation and the higher prevalence of co-existing comorbidities, such as atrial fibrillation (AF) and obesity [Citation13–15].
This descriptive study aims to provide insight into the stroke burden in Qatar by interrogating the national stroke registry to gather information on the country’s demographics, clinical features, management, and outcomes of stroke cases. By shedding light on these critical aspects, this study can improve Qatar’s stroke prevention, treatment, and management strategies.
Materials and methods
This study aims to provide an overview of stroke disease in Qatar. We conducted a retrospective analysis at Hamad Medical Corporation (HMC), Qatar’s principal Health care provider. The Hamad General Hospital (HGH), the country’s main tertiary hospital, offers specialized stroke services under the umbrella of the Neuroscience Institute and maintains the stroke registry. This center covers more than 90% of all stroke admissions in Qatar. The registry provides a comprehensive insight into the incidence and management of stroke disease in Qatar.
Data were extracted from the stroke registry at HGH, covering the period from the registry’s inception in January 2014 to July 2022. The data included all adult patients aged ≥18 years who were admitted to HGH with stroke as a primary diagnosis, including cases of IS, transient ischemic attack, ICH, and stroke mimics. In total 15,859 patients were included in the study, all of whom visited the hospital with stroke symptoms and received specialized stroke care. It is worth noting that mimic inclusion in the registry started in 2016. All pertinent risk factors, including existing health conditions and smoking history, were ascertained during the patient’s hospitalization, and verified by stroke registry personnel through accessing electronic medical records.
Extracted variables
The extracted variables included patients’ demographics, nationality, stroke risk factors, and stroke severity classified by the National Institute of Health Stroke Score (NIHSS) as minor stroke (≤4), moderate stroke [Citation5–15], and severe stroke (≥16), stroke etiology was determined using the Trial of Org 10,172 in Acute Stroke Treatment (TOAST) classification [Citation16], and stroke outcomes were measured using the modified Rankin Score (mRS) at discharge and 90 days post-discharge. Favorable outcomes were defined as an mRS of ≤ 2 [Citation5,Citation17].
The patients were categorized based on their declared nationality into three groups: the Middle East and North Africa (MENA) region, which was defined by the United Nations International Children’s Emergency Fund (UNICEF); South Asia and South East Asia, which were subdivided according to the United Nations geo-scheme; and the remaining nationalities were categorized as ‘other’ [Citation11]. and summarize all the variables included in the study.
Table 1. The annual Qatar population census 1950–2024.
Table 2. Summary of variable – comparison between ischemic and hemorrhagic cohorts.
Data analysis
A descriptive analysis was carried out to provide a comprehensive overview of stroke in Qatar to achieve the study’s objectives. Additionally, relevant univariate analyses, including the Chi-square test of association, independent t-test, and one-way ANOVA, were conducted to explore the relationship between selected variables and identify future research potentials. All presented p-values were two-tailed, and a p-value less than 0.05 was considered statistically significant with a confidence level of 95%. It was ensured that all statistical key assumptions about each test were respected. IBM SPSS version 29 was used for data analysis.
Ethical considerations
The Institutional Review Board at Hamad Medical Corporation approved the study with reference number (MRC-01-22-594). This work utilized secondary data that are available in the stroke registry at HMC- stroke service. Therefore, no patient’s consent was required.
Results
Between January 2014 and July 2022, a total of 15,859 patients with suspected stroke conditions visited HGH, with males comprising 74.8% of the patient population. Most patients (80.2%) were under age 65, with a mean age of 53.5 ± 14.17 and an interquartile range (IQR 20). Female patients had a significantly higher mean age than male patients (56.63 ± 16 years vs. 52.43 ± 13.3 years, p-value <0.05). Regarding ethnicity, 44.6% of patients were of South Asian ethnicity, while 41.4% were from the MENA region. Qatari patients represented 19.4% of all stroke patients and 47% of patients from the MENA cohort.
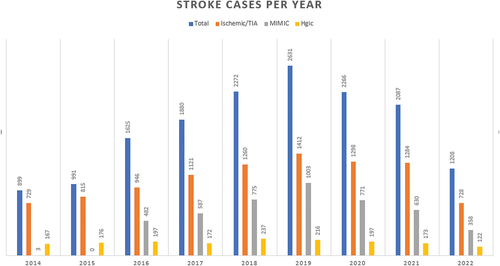
Among the patients 11,250 patients (70.9%) were diagnosed with stroke, while 4,609 patients (29.1%) were diagnosed with stroke mimics. Of the 11,250 stroke patients, 9,593 patients (85.3%) were diagnosed with IS, and 1,657 patients (14.7%) were diagnosed with ICH. The year 2019 had the highest number of registered stroke cases in Qatar, with 2,631 cases admitted to the hospital, out of which 1,412 cases were diagnosed with IS, 216 patients with ICH, and the remaining 1,003 patients were diagnosed with stroke mimics. The number of cases gradually declined in the following three years, with 2,266 cases in 2020 and 2,087 cases in 2021, as shown in . shows the annual Qatar population census 1950–2024 [Citation18].
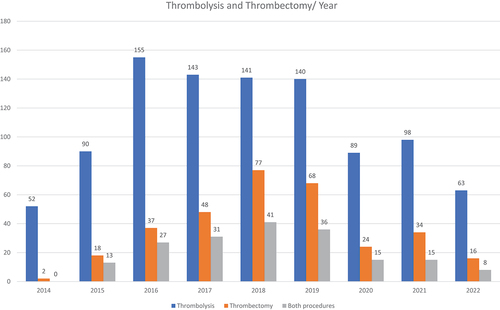
A total of 971 stroke patients, comprising 6.1% of all stroke patients, underwent thrombolysis during the study period. Among these, 913 (94%) were diagnosed with IS, while 58 (6%) were diagnosed with stroke mimics. Furthermore, 324 patients (2% of all stroke patients and 3.4% of IS patients) underwent thrombectomy. Among these patients, 186 underwent both procedures, with 185 (99.5%) having an IS diagnosis. The number of thrombolysis/thrombectomy procedures per year is illustrated in .
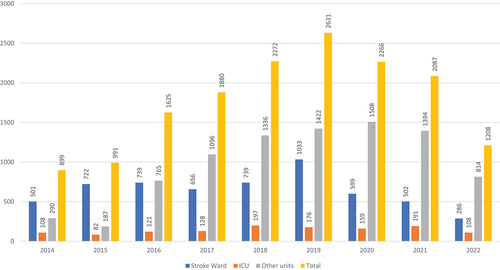
depicts the average annual admission of 1762 stroke patients to the stroke service. Among these patients, 39.4% were admitted to the stroke unit, 8.3% were admitted to critical care, and 52.12% were admitted to other units. Over the nine years from 2014 to 2022, the proportion of patients admitted to other units has gradually increased from 32% to 67.4%, while the proportion of patients admitted to the stroke unit has declined from 52.7% to 23.7%.
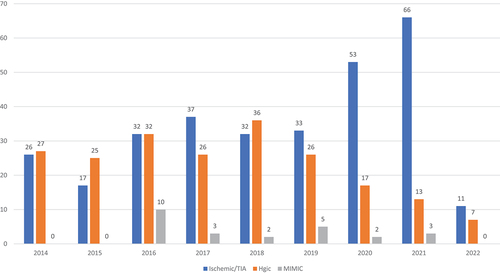
The overall mortality rate for stroke patients between 2014 and 2022 was 3.4%. The ICH had a significantly higher mortality rate than IS (12.6% vs. 3.2%), while the mortality rate for stroke mimics was 0.5%, p-value <0.05. Crucially, a significant correlation was found between the severity of stroke upon admission, as measured by the NIHSS, and overall mortality rates. Specifically, the average NIHSS score for patients who passed away within 90 days of stroke onset was notably higher compared to those who survived beyond the 90-day post-stroke diagnosis (13 vs. 4), p-value <0.05. Additionally, the average NIHSS score for patients who experienced unfavorable outcomes according to the mRS 90 days after discharge was significantly greater than for those reporting favorable outcomes at the same interval (11 vs. 3), again with a p-value <0.05, underscoring the importance of stroke severity as a predictor of long-term recovery. displays the mortality rate per year for each diagnosis. Notably, female patients had a higher mortality rate (4.1%) compared to male patients (3.2%), with an odds ratio of 1.3 (95% CI: 1.06–1.55) and p-value <0.05.
Ischemic stroke (IS) in Qatar
Demographic characteristics
Throughout 2014 to 2022, a total of 9593 patients with IS were admitted to the HGH stroke service, with males accounting for 79% and females 21% of the cohort. Among these patients, the largest ethnic group was South Asian, making up 49.2% of the cohort, followed by MENA at 38%. Qatari patients represented 17.9% of all IS cases. Most patients (39.1%) were between 51 and 65 years old, with a mean age of 54.6 ± 13.5 (IQR 18). The mean age of female patients was significantly higher (60 ± 15.5 years) than that of male patients (53.2 ± 12.5 years) with a small independent sample effect size (i.e. Cohen’s d of −0.3 and 95% CI: −0.334:-0.26) and a p-value <0.05.
Risk factors
Regarding the risk factors, 67% of patients had a Body Mass Index (BMI) greater than 25, indicating they were overweight, obese, or extremely obese. Furthermore, 55% of patients were diabetic, 70% had hypertension (HTN), 45.7% had dyslipidemia, 12% had coronary artery disease (CAD), and 5% had a history of AF. Additionally, 23% of patients who suffered from IS were tobacco users.
Etiology and clinical features
Over 68% of patients had minor strokes, whereas 7.1% had severe strokes, according to the NIHSS. The mean NIHSS was 4.6 ± 5.7 (IQR 5). The most prevalent IS TOAST classification subtype in Qatar was SVD (31%), followed by a Stroke of Undetermined Origin (SUO) (22%).
Acute interventions and complications
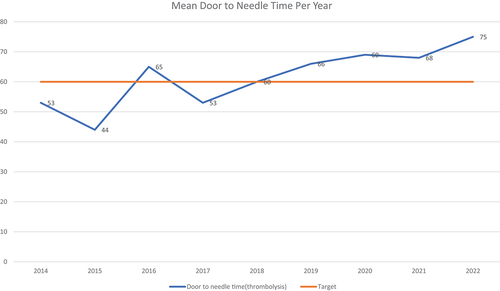
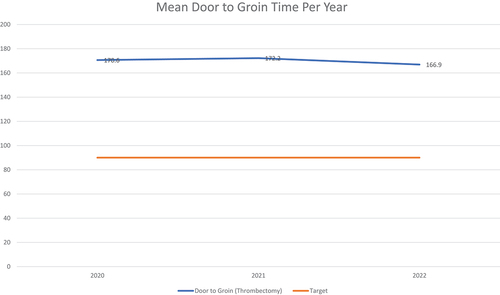
Of the 9593 patients, 913 (9.5%) underwent thrombolysis, and 322 (3.4%) underwent thrombectomy. Additionally, 185 patients (2%) underwent both procedures. The main etiological category receiving thrombolysis was Large Vessel Disease (LVD) stroke, accounting for 31.9% of cases, followed by Small Vessel Disease (SVD) stroke at 25.3%. The mean door-to-needle time for thrombolysis was 61.2 minutes ±38.5 (IQR 39), slightly higher than the international benchmark of 60 minutes [Citation19], as shown in . Similarly, the mean door-to-groin time for thrombectomy was 169.9 minutes, greater than the international benchmark of 90 minutes [Citation20], as demonstrated in .
Significantly, 1.2% (58 out of 4609) of patients with stroke mimics received thrombolysis. Identifying mimics in emergency settings is challenging due to their symptoms often closely resembling those of a stroke [Citation21]. Research indicates that the percentage of mimics treated with thrombolysis varies between 2% and 15% [Citation22–24]. Generally, thrombolysis is deemed safe for mimics. In our study, none of the 58 patients treated exhibited post-thrombolysis bleeding, an outcome that compares favorably with the typically reported rates of 0% to 1.2% [Citation22].
In terms of procedural complications, 56 out of 913 patients who underwent thrombolysis experienced post-procedure bleeding (6.1%), while 28 patients (3%) experienced post-procedure intracranial hemorrhage.
Outcomes
The study found that 3.4% of patients (326 patients) developed in-hospital pneumonia, while 2.1% (202 patients) developed in-hospital urinary tract infections (UTI). Only 10 cases of radiologically confirmed deep vein thrombosis (DVT) were reported during the acute hospital stay. Regarding patient outcomes, the mean modified Rankin Scale (mRS) score at discharge was 1.75 ± 1.8 (IQR 3), indicating favorable stroke outcomes for most patients. However, the mean mRS score improved to 1.4 ± 1.8 (IQR 3) 90 days after discharge, suggesting that many patients could recover some functions. Notably, a considerable proportion of patients (2146/22.4%) did not attend their 90-day follow-up appointments, which may have impacted the accuracy of these results. The study also examined mortality rates among patients with IS and found that 307 patients (3.2%) had died. Most of these deaths occurred among patients diagnosed with Stroke of Undetermined Origin (SUO) (36.5%) or Large Vessel Disease (LVD) (22.8%).
Our analysis revealed a significant correlation between the initial stroke severity, as measured by the NIHSS, and ischemic stroke outcomes. Patients presenting with severe strokes (NIHSS ≥16) exhibited a notably higher mortality rate of 23%, compared to 4% for moderate strokes (NIHSS 5–15) and a mere 0.1% for mild strokes (NIHSS <5), with a p-value <0.05. Similarly, the likelihood of unfavorable outcomes, as indicated by the modified Rankin Scale (mRS) at 90 days post-discharge, was markedly elevated in patients with severe strokes, with 83% demonstrating unfavorable mRS scores compared to 47% for moderate strokes and 14.5% for mild strokes, again with a p-value <0.05. These findings shed light on the critical importance of early identification and intervention for severe stroke cases to mitigate adverse outcomes and improve patient prognosis.
It is important to put emphasis on the significant impact of stroke severity at presentation on patient outcomes, including 90-day mRS and mortality rates, even among individuals undergoing thrombolysis and thrombectomy. Our analysis revealed compelling disparities: 45% of patients who underwent thrombolysis exhibited unfavorable 90-day mRS scores, compared to only 23% of those who did not undergo the procedure, with a statistically significant p-value <0.05. Similarly, among patients undergoing thrombectomy, 54% had unfavorable 90-day mRS scores, compared to 24% of those who did not undergo thrombectomy, also with a p-value <0.05. These disparities may be attributed to the higher presenting National Institutes of Health Stroke Scale (NIHSS) severity scores among patients who underwent thrombolysis [Citation10] and thrombectomy [Citation14], as opposed to those who did not undergo these interventions; 3 and 3.5, respectively. Furthermore, regarding mortality rates, our findings indicate that 3.8% and 5.6% of patients who underwent thrombolysis and thrombectomy, respectively, experienced mortality, compared to 2.2% and 2.3% among those who did not undergo these procedures, with a p-value <0.05. It is plausible that the presenting stroke severity contributes to these observed differences.
Hemorrhagic stroke (ICH) in qatar
Demographic characteristics
A total of 1657 patients with ICH were admitted during the study period, with 83.2% male. Most patients were of South Asian ethnicity (53.4%), followed by patients from the Middle Eastern and North African (MENA) region (25.4%). The mean age of patients with ICH was 50.9 ± 13.1 (IQR 17), and 33.4% were between 41 and 51 years old. Female patients had a significantly higher mean age than male patients (55.9 vs. 49.8, p < 0.05).
Clinical features and risk factors
Patients with ICH typically present with severe symptoms, with 72.5% presenting to the hospital with moderate symptoms, resulting in a mean NIHSS of 11.9 ± 8.7 (IQR 16). Additionally, most patients (62%) had a BMI greater than 25, with 6% of those being classified as extremely obese. The risk factor profile differed from IS, with a higher rate of HTN (83%) and lower rates of DM (34%), dyslipidemia (28%), and AF (3%). Furthermore, 10.4% of the patients were current tobacco users.
Outcomes
In terms of in-hospital complications, a significant proportion of patients with ICH developed complications such as in-hospital pneumonia (15.6%) and UTI (9.7%). Unfortunately, stroke outcomes were poor, with most patients (69.4%) experiencing unfavorable modified Rankin Scale (mRS) scores (>2) at the time of hospital discharge, with a mean score of 3.4 ± 1.9 (IQR 3). Even 90 days after discharge, a substantial proportion of patients (44.8%) still had unfavorable mRS scores, with a mean score of 2.97 ± 2.2 (IQR 4), which means that a significant percentage of the patients continued to suffer longer-term moderate to severe disability. It is also concerning that around 24.1% of patients missed their 90-day follow-up appointment, potentially impacting the accuracy of these results. The mortality rate for ICH was 12.6%, and there was a statistically significant association with sex, p-value <0.05, with higher mortality rates observed in females than in males 28% vs. 19% with odds ratio 1.5 (95% CI, 1.3–1.7). Notably, Qatari nationals had the highest mortality rate among patients with ICH, with 17.9%, compared to a 12.3% mortality rate among other ethnicities with an odds ratio of 1.5 and p-value <0.05.
Our analysis revealed a significant correlation between the initial stroke severity, as measured by the NIHSS, and hemorrhagic stroke outcomes. Patients presenting with severe strokes (NIHSS ≥16) exhibited a notably higher mortality rate of 29%, compared to 4% for moderate strokes (NIHSS 5–15) and a 4% for mild strokes (NIHSS <5), with a p-value <0.05. Similarly, the likelihood of unfavorable outcomes, as indicated by the modified Rankin Scale (mRS) at 90 days post-discharge, was markedly elevated in patients with severe strokes, with 89% demonstrating unfavorable mRS scores compared to 55% for moderate strokes and 21% for mild strokes, again with a p-value <0.05. These findings shed light on the critical importance of early identification and intervention for severe stroke cases to mitigate adverse outcomes and improve patient prognosis.
Comparison between ischemic and hemorrhagic stroke
Demographic characteristics
Of the stroke patients in the study, 85.3% were diagnosed with IS, while 14.7% had ICH. A statistically significant association was observed between sex and stroke type, p-value <0.05. Specifically, 15.3% of males were diagnosed with ICH, compared to 12.3% of females (odds ratio of 1.24), while 84.7% of males had an IS, compared to 87.7% of females (odds ratio of 1.04).
The study found that patients with IS had a significantly higher mean age of 54.6 years, compared to patients with ICH who had a mean age of 50.9 years, p-value <0.05 with a small sample effect size (Cohen’s d = 0.3 and 95% CI: 0.24–0.34).
Of note, Southeast Asian patients were found to be more prone to ICH compared to other ethnicities. Specifically, 27.9% of Southeast Asian patients were admitted with ICH compared to 15.8% of South Asian patients and approximately 10% of all other ethnicities. Furthermore, it is obvious that the impact of hemorrhagic stroke on the 90-day prognosis is worse than that of ischemic stroke.
Importantly, our analysis revealed that across all severity groups, the proportion of patients experiencing unfavorable outcomes, as measured by the modified Rankin Scale (mRS) at 90 days post-discharge, was higher in hemorrhagic stroke compared to ischemic stroke. Specifically, for mild strokes, the percentage of patients with unfavorable mRS scores was 21% in hemorrhagic stroke versus 14.5% in ischemic stroke. Similarly, for moderate strokes, the percentages were 55% and 47% respectively, and for severe strokes, they were 89% and 83% respectively, with a p-value <0.05. Additionally, we observed a higher mortality rate in hemorrhagic stroke compared to ischemic stroke, with 4% versus 0.1% for mild strokes, and 29% versus 23% for severe strokes, with a p-value <0.05. However, there was no significant difference in mortality rates between hemorrhagic and ischemic stroke for moderate strokes, with both groups experiencing a 4% mortality rate. These findings feature the distinct impact of hemorrhagic stroke on patient outcomes across severity levels compared to ischemic stroke.
Clinical features
Furthermore, patients with ICH tended to present with more severe symptoms, as measured by the NIHSS. The mean NIHSS for IS patients was 4.6 ± 5.7 with a median of 3, whereas patients with ICH had a mean NIHSS of 11.99 ± 8.7 and a median of 11 with a p-value <0.05.
Risk factors
Noteworthy, there was a significant association between BMI and stroke type, with ICH being more prevalent in underweight patients, 29.8% compared to 14.2% of patients with normal weight and 13.8% of patients in other weight categories with a p-value of 0.05.
Stroke risk factors show significantly different prevalence in the two cohorts with DM, dyslipidemia, CAD, AF, and current tobacco use are more prevalent in the IS cohort compared to the ICH cohort (55% vs. 34%),(45.7% vs. 28%),(12% vs. 6%), (5.2% vs 2.9%), and (23.2% vs 4%) respectively with a p-value <0.05. In the ICH cohort, HTN was more prevalent than in the IS cohort (83.3% vs. 70.3%), p-value <0.05.
In-hospital complications
ICH patients had significantly higher rates of in-hospital complications compared to patients with IS. 15.6% of patients with ICH had in-hospital pneumonia compared to 3.4% in patients with IS, p-value <0.05. Similarly, 9.7% of the patients with ICH had in-hospital UTI compared to only 2.1% for IS patients, with a p-value <0.05. This increased risk of in-hospital complications in ICH patients could be associated with their significantly longer hospital Length of Stay (LOS), which is 11 ± 11.5 days and a median of 7.4 compared to the mean LOS of 5.2 ± 8 days and a median of 3.3 for IS patients, p-value <0.05). The overall mean LOS for all stroke patients is 6 ± 8.9 days and a median of 3.7.
Outcomes
ICH patients have poorer prognoses, longer-term associated disabilities, and higher mortality compared to IS patients. 69.4% of ICH patients were discharged with unfavorable mRS (>2) compared to 35.8% of IS patients discharged with mRS > 2. At 90-day follow-up, the proportion of IS patients who were presented with unfavorable mRS reduced to 27.2%. In comparison, the percentage of ICH patients who were presented after 90 days with unfavorable mRS was 59%, p-value <0.05. Finally, the overall stroke mortality rate, considering both ischemic and ICH, was 4.6%. Notably, the mortality rate in ICH was significantly higher than IS’s (12.6% vs. 3.2%), p-value <0.05.
Discussion
The study provides a comprehensive overview of the state of stroke patients in Qatar from 2014 to 2022, comparing ischemic and hemorrhagic strokes in terms of patient demographics, risk factors, clinical features, outcomes, and prognosis. Improving chronic conditions management is a strategic priority in Qatar’s national health strategy for 2018–2022 [Citation25], and stroke services have received significant attention as a result. The number of stroke patients admitted to HMC has increased significantly from 2014 to 2019. However, a decline for two consecutive years after 2019 has been witnessed, attributed to the COVID-19 pandemic that hit the world in late 2019 and Qatar in early 2020. Akhtar and colleagues reported a significant decline in stroke admission rates in Qatar from September 2019 to May 2020, with fewer admissions for functional MIMIC conditions, possibly due to concerns about contracting COVID-19 [Citation26].
Over the past nine years, the demand for stroke services in Qatar has increased, but the service’s capacity has not grown at the same pace. This explains why the proportion of patients admitted to units other than stroke units increased from 39% in 2014 to 67% in 2022. To address this issue, enhancing the capacity of the stroke service may be necessary to meet the demand. Given that admission to a stroke unit is recognized as an intervention that enhances patient outcomes, it’s especially important to consider this factor in treatment planning and evaluation [Citation27].
Consistent with previous literature, sex is a significant factor affecting stroke outcomes in Qatar [Citation13,Citation28–31]. While male patients tend to present with more severe stroke symptoms, female patients are at higher risk for unfavorable outcomes; specifically, over 31% of male patients present to the hospital with moderate to severe symptoms, as measured by the NIHSS, compared to 24% of female patients. It is important to note that Qatar has many expatriates, many of whom are young males. The mean age of female stroke patients was significantly higher than that of males, at 57 vs. 52 years, respectively. Moreover, the mortality rate for female patients was higher than that of males, at 4.1% vs. 3.2%, respectively, and the rate of unfavorable outcomes 90 days after hospital discharge was also higher in female patients, at 36% vs. 28% for males. Besides the higher age at the onset, it was found that female patients had a higher prevalence of AF (7.1% vs. 3.6% for males, p-value <0.05), a higher percentage above normal BMI (73.5% vs. 66.1% for males, p-value <0.05%), and a higher prevalence of DM (50% vs. 48% for males, p-value <0.05%). These findings are consistent with previous work conducted in Qatar [Citation13] and highlight the need for more focus on preventive measures and lifestyle adjustments for the female population. Moreover, in the decade after menopause, women’s risk of stroke approximately doubles [Citation32]. According to Welten and colleagues, there is a significant inverse relationship between the risk of total ischemic stroke and the age of menopause [Citation33]. Given that the average age of menopause in Qatar is 48 years [Citation34], which is relatively lower than the average of 130 countries of 50 years, women in Qatar face a greater risk for stroke in general and ischemic stroke in particular. Yet, the specific effects of menopause on stroke outcomes remain uncertain and warrant further investigation. Preliminary evidence from one study indicates a potential increase in fatal strokes among women who experience menopause earlier [Citation35].
According to Jallow et al. [Citation8], Qatar has a low overall mortality rate. However, examining the relationship between ethnicity and outcomes is important to better understand mortality and develop targeted prevention measures. The highest mortality rate among patients with IS seen in Qatari patients, with a rate of 5.5%, compared to 4% in the rest of the MENA region, 2.2% in South Asian patients, 2.2% in Southeast Asian patients, and 3.1% in patients of other ethnicities (p-value 0.05). Similarly, the mortality rate among patients with ICH is highest in the Qatari population, with a rate of 17.9%, compared to 14.6%, 11.2%, 11.7%, and 11.5% in the MENA, South Asian, Southeast Asian, and other ethnicities, respectively, consistent with previous research [Citation8]. Qatari patients also reported the highest percentage of unfavorable mRS scores (>2) at 90 days after stroke, with a rate of 41.2%, compared to 27.2%, 27.5%, 27.4%, and 22% for MENA, South Asian, Southeast Asian, and other ethnicities, respectively. Upon secondary analysis, Qatari patients were found to have a significantly higher prevalence of risk factors than other ethnic groups. Specifically, Qatari patients have a higher prevalence of DM: 67.3% vs. 43.9%, HTN; 73.5% vs. 64.2%, dyslipidemia; 49.5% vs. 39.3%, AF; 8.2% vs. 3.6%, obesity; 75.3% vs. 66.2%, and CAD; 18.1% vs. 9.3%, p-value <0.05. These findings suggest that targeted prevention measures and interventions are needed to address the higher mortality and unfavorable outcomes among Qatari stroke patients.
The rate of thrombolysis (9.3%) as an acute intervention in Qatar is within international rates and remarkably close to that of highly developed countries. As reported by Mikulik et al., the rate of thrombolysis ranges from < 4% in developing countries to 10% [Citation36]. Similarly, the proportion of IS patients who get access to thrombectomy is estimated internationally to be 2.8% [Citation37]. In Qatar, the rate is around 3.2%, which is higher than the international rate. This is related to the country’s policy where care is free for all [Citation38].
Thrombolysis is an effective treatment option for stroke patients, as it can significantly improve prognosis and reduce disability. However, its success is highly time-dependent, so the mean door-to-needle time (DNT) is particularly important [Citation39]. The recommended DNT is 60 minutes [Citation19]. In Qatar, the DNT has increased significantly from 53 minutes in 2014 to 75 minutes in mid-2022, with 4 consecutive years above the recommended mean DNT. Besides the impact of the COVID-19 pandemic on the health system performance, this increase in the DNT could be due to the mismatch between the rising demand for thrombolysis, driven by an increased patient load, and the available healthcare resources. This is a critical area for improvement, and measures must be taken to ensure that patients receive thrombolysis treatment as soon as possible to enhance their outcomes. Literature shed light on some initiatives that helped reduce the DNT, such as registering the patients as unknown to save the time of formalities, STAT stroke protocol, and administering the thrombolytic agent in the CT suite [Citation40].
Similarly, the door-to-groin time (DGT) for thrombectomy is also essential for patient outcomes and disability, with a target of less than 90 minutes [Citation20]. Data from Qatar is only available from 2020, with a mean DGT ranging from 170 to 172 minutes. This highlights another area for improvement, where patient outcomes and disability can be improved by reducing the DGT time. Therefore, it is essential to implement measures to reduce DGT times to ensure that stroke patients receive timely and effective treatment to achieve optimal outcomes. Previous literature emphasized the importance of designing an effective workflow and implementing the role of the stroke nurse, which helps identify patients who require thrombectomy [Citation41]. Others suggested implementing the Ventura Emergent Large Vessel Occlusion Score (VES) protocol, which significantly improved the DGT [Citation42].
Consistent with previous studies in regional and international settings, IS is the most common type of stroke in Qatar. However, ICH is associated with more severe outcomes, which may be due to the severity of presenting symptoms. The mean NIHSS score, which measures stroke severity, is significantly higher in patients with ICH than those with IS (11.9 vs. 4.6, p-value <0.05) [Citation4,Citation43,Citation44]. These findings highlight the importance of prompt recognition and appropriate management of ICH to improve patient outcomes in Qatar.
The in-hospital complications rate in Qatar’s stroke services is low. Notably, only 10 patients (approximately 0.005%) developed deep vein thrombosis (DVT) or pulmonary embolism, which is significantly lower than the reported rates internationally, ranging from 3–9% following acute stroke [Citation45]. Similarly, only 66 patients (approximately 0.04%) developed hospital-acquired pressure injury (HAPI) during the study period, which is significantly lower than the reported rates in other tertiary care centers, ranging from 3.3% to 8.3% [Citation46,Citation47]. These findings suggest that effective preventive measures for venous thromboembolism and skin breakdown are being implemented in Qatar’s stroke services in addition to the presence of the younger population and the prevalence of lacunar strokes and milder stroke severity in general, which may be other contributing factors.
Furthermore, Qatar scored a significantly low rate of 4% for hospital-acquired pneumonia compared to the 14.3% reported in a recent systematic review and meta-analysis of 64 studies, including 639,953 patients [Citation48]. In addition, the hospital-acquired urinary tract infection rate was only 2.3%. In comparison, a meta-analysis that included 13,513 patients in 16 studies reported an incidence rate of UTI in patients with stroke reaching up to 19% [Citation49]. These findings reflect the effective implementation of infection control measures in Qatar’s stroke services, resulting in a lower incidence of hospital-acquired infections than in other centers.
Comparing Qatar’s stroke data with international registries is crucial for identifying global and regional trends in stroke management and outcomes. This enables the adaptation of successful prevention strategies, improving patient care by learning from diverse healthcare approaches and addressing the challenge of sustaining long-term medication adherence. In China, a study in 1913 of minor ischemic stroke patients revealed high one-year rates of stroke recurrence, disability, and death [Citation50]. Risk factors included hypertension and atrial fibrillation. Triple therapy reduced death rates, yet only half continued prevention medications after a year, stressing the need for sustained secondary prevention strategies to improve outcomes. Another study from China revealed that among 4643 acute ischemic stroke patients eligible for DVT prophylaxis, adherence was only 59.6%, with a median hospital rate of 57.8% [Citation50]. Factors like atrial fibrillation history, rehabilitation evaluation, and care in eastern or central regions increased prophylaxis use. Conversely, older age, higher NIHSS scores, and larger hospital sizes were associated with lower adherence rates, highlighting significant variability and areas for improvement in DVT prevention practices.
It is important to note that a significant amount of data regarding the 90-day disability assessment is missing due to the loss of 90-day follow-up. This issue is particularly pronounced among certain ethnicities, with 7.4% of Qatari patients and those of Middle Eastern and North African descent missing their 90-day follow-up compared to 16.5%, 10.8%, and 11.4% in South Asian, Southeast Asian, and other ethnic groups, respectively. The lack of complete data on the 90-day follow-up appointments may negatively impact the accuracy of stroke outcomes in Qatar and our knowledge of the true prognosis for these patients.
The findings of this study offer invaluable insights poised to make a substantial impact on stroke prevention and treatment strategies in Qatar. By meticulously delineating the demographic profiles and prognosis of stroke patients, healthcare providers gain nuanced understanding essential for tailoring prevention initiatives to the needs of specific at-risk groups, such as females and individuals of South Asian descent. Moreover, insights into prevailing practices and impediments in stroke management, notably delays in thrombolysis and thrombectomy procedures, pave the way for targeted interventions aimed at enhancing the promptness and efficacy of acute stroke care delivery. Furthermore, the study underscores the imperative for heightened stroke awareness campaigns directed at both the general public and healthcare practitioners. These initiatives hold the potential to foster early recognition of stroke symptoms and facilitate swift access to medical interventions. By translating these findings into actionable strategies, policymakers and healthcare stakeholders can collaboratively strive towards alleviating the burden of stroke in Qatar, thus fostering improved patient outcomes and quality of life.
Conclusion and future directions
Stroke is a preventable disease that significantly challenges the well-being and economy of nations globally. Qatar has a unique advantage in having a well-established stroke registry that captures stroke activities nationwide. Encouraging scholars to study the burden of stroke in Qatar can shed light on the specific characteristics of the population, helping to devise relevant and effective preventive measures and improve stroke management and treatment outcomes. While the incidence and mortality rates of stroke are low in Qatar, this study provides invaluable information to initiate more epidemiological studies that enhance our understanding of the disease and its prevention. There is an opportunity to establish prevention programs tailored to sex and ethnicity, which have been shown to have a considerable influence on disease outcomes. By leveraging this unique advantage, Qatar can continue to improve stroke prevention, management, and outcomes and contribute to the global effort to combat this preventable disease.
Statement of ethics
The Medical Research Center of Hamad Medical Corporation IRB approved this project (MRC-01-22-594). The research was carried out in compliance with the ethical principles outlined in the Helsinki Declaration of 1964 and its subsequent modifications and related ethical norms. The IRB waived the need for informed consent at the Medical Research Center of Hamad Medical Corporation.
Author contributions
Conceptualization: AAA, YI
Formal analysis: AAA
AAA, YI, AJN, AMO, NA: Data Curation, Methodology, Writing – original draft, Writing – review & editing
All authors read and approved the final manuscript.
Acknowledgments
Open Access funding provided by the Qatar National Library.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request and subject to appropriate ethical approvals.
Additional information
Funding
References
- Feigin V, Brainin M, Norrving B, et al. World stroke organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18–29. doi: 10.1177/17474930211065917
- World Health Organization. World stroke day. 2022 [2023 Mar 28]. Available from World Stroke Day 2022 (who.int).
- Steinmetz JD, Seeher KM, Schiess N, et al. Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet Neurol. 2024;23(4):344–381. doi: 10.1016/S1474-4422(24)00038-3
- Jaberinezhad M, Farhoudi M, Nejadghaderi S, et al. The burden of stroke and its attributable risk factors in the Middle East and North Africa region, 1990–2019. Sci Rep. 2022;12(1):2700. doi: 10.1038/s41598-022-06418-x
- Imam Y, Kamran S, Saqqur M, et al. Stroke In the adult Qatari population (Q-stroke) a hospital-based retrospective cohort study. PLoS One. 2020;15(9):e0238865. doi: 10.1371/journal.pone.0238865
- Alhyas L, McKay A, Balasanthiran A, et al. Prevalences of overweight, obesity, hyperglycaemia, hypertension and dyslipidaemia in the gulf: Systematic review. JRSM Short Rep. 2011;2(7):55. doi: 10.1258/shorts.2011.011019
- World Stroke Organization. Stroke in the Qatari Population. 2020 [cited 2023 Mar]. Available from: https://www.world-stroke.org/news-and-blog/blogs/stroke-in-the-qatari-population#:~:text=86%25%20of%20strokes%20that%20occur,females%20of%20hypertension%20and%20diabetes
- Jallow E, Al Hail H, Han T, et al. Current status of stroke in Qatar: Including data from the BRAINS study. JRSM Cardiovasc Dis. 2019;8:2048004019869160. doi: 10.1177/2048004019869160
- El-Hajj M, Salameh P, Rachidi S, et al. The epidemiology of stroke in the Middle East. Eur Stroke J. 2016;1(3):180–198. doi: 10.1177/2396987316654338
- Gulli G, Rutten-Jacobs L, Kalra L, et al. Differences in the distribution of stroke subtypes in a UK black stroke population – final results from the South London ethnicity and stroke study. BMC Med. 2016;14(1):77. doi: 10.1186/s12916-016-0618-2
- Imam Y, Kamran S, Akhtar N, et al. Incidence, clinical features and outcomes of atrial fibrillation and stroke in Qatar. Int J Stroke. 2020;15(1):85–89. doi: 10.1177/1747493019830577
- Abujaber AA, Imam Y, Albalkhi I, et al. Utilizing machine learning to facilitate the early diagnosis of posterior circulation stroke. BMC Neurol. 2024;24(1):1–12. doi: 10.1186/s12883-024-03638-8
- Akhtar N, Kate M, Kamran S, et al. Sex-specific differences in short-term and long-term outcomes in acute stroke patients from qatar. Eur Neurol. 2020;83(2):154–161. doi: 10.1159/000507193
- Sposato L, Brown D. Sex differences in the use of therapeutic resources and stroke outcomes in 5 randomized trials. Neurology. 2019;93(24):1025–1027. doi: 10.1212/WNL.0000000000008610
- Phan H, Blizzard C, Reeves M, et al. Factors contributing to sex differences in functional outcomes and participation after stroke. Neurology. 2018;90(22):e1945–e53. doi: 10.1212/WNL.0000000000005602
- Adams H, Bendixen B, Kappelle L, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. doi: 10.1161/01.STR.24.1.35
- Banks J, Marotta C. Outcomes validity and reliability of the modified Rankin Scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007;38(3):1091–1096. doi: 10.1161/01.STR.0000258355.23810.c6
- macrotrends.net. Qatar Population 1950-2024. 2024 [ Available from: https://www.macrotrends.net/countries/QAT/qatar/population
- Fonarow G, Zhao X, Smith E, et al. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA. 2014;311(16):1632–1640. doi: 10.1001/jama.2014.3203
- Rangel I, Palmisciano P, Vanderhye V, et al. Optimizing Door-to-Groin Puncture Time: The Mayo Clinic Experience. Mayo Clinic Proc Innovations Qual Outcomes. 2022;6(4):327–336. doi: 10.1016/j.mayocpiqo.2022.05.009
- Tsivgoulis G, Zand R, Katsanos AH, et al. Safety of intravenous thrombolysis in stroke mimics: prospective 5-year study and comprehensive meta-analysis. Stroke. 2015;46(5):1281–1287. doi: 10.1161/STROKEAHA.115.009012
- Jacobsen E, Logallo N, Kvistad CE, et al. Characteristics and predictors of stroke mimics in young patients in the norwegian tenecteplase stroke trial (NOR-TEST). BMC Neurol. 2023;23(1):406. doi: 10.1186/s12883-023-03425-x
- Zinkstok SM, Engelter ST, Gensicke H, et al. Safety of thrombolysis in stroke mimics: results from a multicenter cohort study. Stroke. 2013;44(4):1080–1084. doi: 10.1161/STROKEAHA.111.000126
- Keselman B, Cooray C, Vanhooren G, et al. Intravenous thrombolysis in stroke mimics: results from the SITS international stroke thrombolysis register. Eur J Neurol. 2019;26(8):1091–1097. doi: 10.1111/ene.13944
- Ministry of Public Health - Qatar. National Health Strategy. 2018-2022 [ Available from: https://www.moph.gov.qa/english/strategies/National-Health-Strategy-2018-2022/Priority-Populations/Pages/Improved-Health-for-People-with-Multiple-Chronic-Diseases.aspx
- Akhtar N, Al Jerdi S, Mahfoud Z, et al. Impact of COVID-19 pandemic on stroke admissions in qatar. Bmj Neurol Open. 2021;3(1):e000084. doi: 10.1136/bmjno-2020-000084
- Akhtar N, Kamran S, Singh R, et al. Beneficial effects of implementing stroke protocols require establishment of a geographically distinct unit. Stroke. 2015;46(12):3494–3501. doi: 10.1161/STROKEAHA.115.010552
- Khan F, Ibrahim A. Gender differences in risk factors, clinical presentation, and outcome of stroke: A secondary analysis of previous hospital-based study in qatar. Libyan J Med Sci. 2018;2(2):51. doi: 10.4103/LJMS.LJMS_42_17
- Abujaber AA, Alkhawaldeh IM, Imam Y, et al. Predicting 90-day prognosis for patients with stroke: a machine learning approach. Front Neurol. 2023;14:14. doi: 10.3389/fneur.2023.1270767
- Abujaber AA, Albalkhi I, Imam Y, et al. Predicting 90-day prognosis in ischemic stroke patients post thrombolysis using machine learning. J Pers Med. 2023;13(11):1555. doi: 10.3390/jpm13111555
- Abujaber AA, Albalkhi I, Imam Y, et al. Machine learning-based prognostication of mortality in stroke patients. Heliyon. 2024;10(7):e28869. doi: 10.1016/j.heliyon.2024.e28869
- Lisabeth L, Bushnell C. Stroke risk in women: the role of menopause and hormone therapy. Lancet Neurol. 2012;11(1):82–91. doi: 10.1016/S1474-4422(11)70269-1
- Welten S, Onland-Moret NC, Boer JMA, et al. Age at menopause and risk of ischemic and hemorrhagic stroke. Stroke. 2021;52(8):2583–2591. doi: 10.1161/STROKEAHA.120.030558
- Review WP. Age of menopause by country. 2024 [ Available from: https://worldpopulationreview.com/country-rankings/age-of-menopause-by-country
- Z-B H, Z-X L, Zhu F. Age at menarche, age at menopause, reproductive years and risk of fatal stroke occurrence among Chinese women: The Guangzhou biobank cohort study. BMC Women’s Health. 2021;21(1):433. doi: 10.1186/s12905-021-01579-9
- Mikulik R, Bar M, Cernik D, et al. Stroke 2020: implementation goals for intravenous thrombolysis. Eur Stroke J. 2021;6(2):151–159. doi: 10.1177/23969873211007684
- Asif K, Otite F, Desai S, et al. Mechanical Thrombectomy Global Access for Stroke (MT-GLASS): A Mission Thrombectomy (MT-2020 Plus) Study. Circulation. 2023;147(16):1208–1220.
- Ibrahim F, Deleu D, Akhtar N, et al. Burden of stroke in Qatar. J Stroke Cerebrovascular Dis. 2015;24(12):2875–2879. doi: 10.1016/j.jstrokecerebrovasdis.2015.08.024
- Hasnain M, Paul C, Attia J, et al. Door-to-needle time for thrombolysis: a secondary analysis of the TIPS cluster randomised controlled trial. BMJ Open. 2019;9(12):e032482. doi: 10.1136/bmjopen-2019-032482
- Kamal N, Holodinsky J, Stephenson C, et al. Improving door-to-needle times for acute ischemic stroke. Circulation. 2017;10(1):e003242. doi: 10.1161/CIRCOUTCOMES.116.003242
- Uppal A, Rutherford W, Erickson S. Abstract WMP113: Improvement of door-to-groin puncture times in stroke codes. Stroke. 2019; 50(Suppl_1):AWMP113–AWMP.
- Farooqui M, Suriya S, Quadri S, et al. Reduction in door-to-groin puncture time for endovascular treatment in acute ischemic stroke patients with large vessel occlusion. Cureus. 2022;14(8). doi: 10.7759/cureus.28348
- Abd-Allah F, Khedr E, Oraby M, et al. Stroke burden in Egypt: data from five epidemiological studies. Int J Neurosci. 2018;128(8):765–771. doi: 10.1080/00207454.2017.1420068
- Qawasmeh M, Aldabbour B, Momani A, et al. Epidemiology, Risk Factors, and Predictors of Disability in a Cohort of Jordanian Patients with the First Ischemic Stroke. Stroke Res Treat. 2020;2020:1920583. doi: 10.1155/2020/1920583
- Stecker M, Michel K, Antaky K, et al. Risk Factors for DVT/PE in patients with stroke and intracranial hemorrhage. Open Neurol J. 2014;8(1):1–6. doi: 10.2174/1874205X01408010001
- Farid J, Amin R, Sheikh M, et al. Prevalence and prediction of pressure ulcers in admitted stroke patients in a tertiary care hospital. J Tissue Viability. 2022;31(4):768–775. doi: 10.1016/j.jtv.2022.07.010
- Riandini R, Emaliawati E, Prevalence MR. Prevention, and wound care of pressure injury in stroke patients in the neurology ward. Belitung Nurs J. 2018;4(6):581–590. doi: 10.33546/bnj.555
- Kishore A, Vail A, Chamorro A, et al. How is pneumonia diagnosed in clinical stroke research? A systematic review and meta-analysis. Stroke. 2015;46(5):1202–1209. doi: 10.1161/STROKEAHA.114.007843
- Yan T, Liu C, Li Y, et al. Prevalence and predictive factors of urinary tract infection among patients with stroke: A meta-analysis. Am J Infect Control. 2018;46(4):402–409. doi: 10.1016/j.ajic.2017.10.001
- Tan Y, Pan Y, Liu L, et al. One-year outcomes and secondary prevention in patients after acute minor stroke: results from the China national stroke registry. Neurological res. 2017;39(6):484–491. doi: 10.1080/01616412.2017.1322804