Abstract
Introduction: Turner syndrome (TS) is associated with subfertility and infertility. Nevertheless, an increasing number of women become pregnant through oocyte donation. The wish to conceive may be negatively influenced by the fear of cardiovascular complications. The aim was to investigate the wish to conceive and the concerns about cardiovascular complications during pregnancy in women with TS.
Methods: The patient association for TS invited all members of ≥18 years old (n = 344) to complete a specifically developed, disease-specific questionnaire, including questions about fertility, wish to conceive, attempts and concerns. Results were compared with previously published results of this questionnaire in women with congenital heart disease.
Results: The questionnaire was completed by 89 women (median age 30.1 years, Q1–Q3 = 22.9–39.4). Of them, 51% had 45, X0-monosomy and 38% had ≥1 cardiac abnormality. Seventeen women (19%) had attempted to become pregnant and 12 of them succeeded to become pregnant. Women who had not undertaken attempts to conceive (81%), considered themselves mainly too young or had no partner. Of the total sample, 58% were concerned about the influence of pregnancy on their cardiovascular status. This was higher (75%) in the sample of women with TS and cardiac abnormalities, than in women with congenital heart disease from a previously published cohort (21%), (p < .001). There were no differences in concerns about pregnancy complications between women with TS who respectively had or had not attempted to become pregnant.
Discussion: Women with TS, especially those with cardiac abnormalities, show serious concerns about the risks pregnancy may have. Patients should be timely counseled and specifically asked about their concerns. Psychosocial care should be provided when necessary.
Introduction
Turner syndrome (TS) is caused by a partial or total monosomy of the X-chromosome. One in 2000 live born girls is affected [Citation1,Citation2]. TS is characterized by short stature, webbed neck and gonadal dysgenesis. The phenotype varies considerably and some women have barely dysmorphic features. Awareness of TS from several disciplines has increased in the past decades and in the Netherlands it resulted in a multidisciplinary approach which is now part of standard care [Citation3]. Cardiac or aortic abnormalities are present in 30–40% of women with TS [Citation1,Citation4,Citation5]. Pregnancy in women with TS is an important challenge due to the gonadal dysgenesis, which may lead to premature ovarian failure. Only a small minority of women with TS is able to conceive spontaneously. Nevertheless, since oocyte donation became available, pregnancy became possible for a larger group of these women. The risk of complications during pregnancy in women with TS is suggested to be increased, in particular the risk of aortic dissection [Citation6]. Pregnancy is assumed to decrease the integrity of the aortic wall [Citation7]. The loss of structure may have deleterious consequences in women with an aortic syndrome and associated preexistent wall abnormalities. Several reports have described aortic dissection during pregnancy in patients with TS [Citation8,Citation9]. It is important to address this when counseling these women. So far, it is unknown how many women with TS are hesitant to become pregnant due to their knowledge about this specific cardiovascular risk during pregnancy.
The wish to conceive and concerns regarding pregnancy are rather unexplored and neglected field. Whether one wants to have children or not and concerns in this domain, are crucial subjects in a woman’s life. The surplus value of this study is that by gaining more specific knowledge on essential themes, counseling of women with TS can be attuned more to these women’s wishes.
Since the past two decades the possibility to conceive increased and evolved in this group of women, the present study aims to investigate how many women with TS have a wish to conceive and how many actually undertake attempts to conceive. Also, the concerns and fear for cardiovascular complications during pregnancy are assessed.
Methods
This is a cross-sectional observational study organized together with the Dutch patients association for women with TS (“Turner Contact Nederland”). All adult women with TS, who were the members of the association, were approached by the association in November 2014. After giving informed consent, participants received a questionnaire. The medical status of all participants was checked to retrieve data on karyotype, cardiac abnormalities and conception or pregnancy outcomes. Institutional review board approval was obtained (MEC-2014–457). The study was conducted according to the Declaration of Helsinki (version October 2013).
Data
A validated questionnaire about concerns and fear for potential pregnancy complications in this specific group is lacking. Hence, we based our questionnaire as much as possible on an existing questionnaire for patients with congenital heart disease, with published data [Citation10]. Questions are presented in the results section. The karyotypes were subdivided into the seven groups commonly used in the literature [Citation11]: monosomy, mosaic, isochromosomes, deletions, polyploidy, ring chromosomes and Y material.
Statistical analysis
Age, karyotypes and cardiac abnormalities are described. Concerns and fears were analyzed for age groups, karyotypes and presence versus absence of cardiac abnormalities. We compared women younger than 25 years of age with women over 25, because we hypothesized that the younger group may have been influenced by the rapid increase in the Netherlands of well organized and multidisciplinary care and the availability of oocyte donation in the past 10 years in particular. Continues variables were checked for normality and presented as mean with standard deviation, or as median with first and third quartile (Q1–Q3). Categorical variables are presented as frequencies and percentages, and compared using chi-squared tests providing a p value. The p values smaller than .05 was considered significant. The Bonferroni method was used to correct for multiple hypothesis testing, for each subgroup (corrected α = .05/n, with n= number of hypotheses tested). All analyses were performed using SPSS version 21.0 (IBM Corp., Armonk, NY).
Results
Of the total 344 women with TS invited for this study, 104 women (30%) responded and gave informed consent. The questionnaire was completed by 89 women (86%). Median age was 30.1 years (Q1–Q3 = 22.9–39.4; range 18.0–65.7 years). Patient characteristics including bicuspid aortic valve, aortic dilatation and coarctation are presented in . One or more of these anomalies were presented in 28 women (37.8%). Nine women had other cardiac abnormalities: partial anomalous pulmonary venous return (n = 4), abnormal origin of the right subclavian artery (n = 2), corrected persistent arterial duct (n = 1), right descending aorta and persistent left superior vena cava (n = 1), dextroposition (n = 1).
Table 1. Patient characteristics.
Fertility and wish to conceive
The majority of the responders had been told by their physician that they probably needed oocyte donation to conceive (). Seventeen women (19.1%) were told they were infertile (median age of 22.6 years, Q1–Q3: 19.6–46.6, range: 18.5–62.6). Eleven patients did not know their fertility status (median age of 22.1 years, Q1–Q3: 19.1–41.3, range: 18.0–65.7).
Table 2. Fertility.
Seventeen patients (19.1%) had attempted to become pregnant. The reason for not trying to get pregnant in the remaining 72 patients, as shown in , was in the majority their young age and the fact that they felt a child would not (yet) fit into their lives. Patients that reported their young age as a reason for not trying to get pregnant (n = 28), had a median age of 21.1 years (Q1–Q3: 19.0–22.9, range 18.0–26.4). Three patients (3.4%) did not have a wish for a child at all.
Table 3. Pregnancy attempts.
Of the 17 women, who had attempted to become pregnant, 14 women had been treated with assisted reproductive therapies. Five women failed to become pregnant, of whom two were still trying to get pregnant. Eventually, 12 women became at least once pregnant, which resulted in seven miscarriages before 20 weeks, one therapeutic abortion because of anencephaly, and eight live births. Preconception cardiac screening was performed in 12 of the 17 women; two patients had not been screened (in one of them it was 20 years ago) and in three patients TS had not been diagnosed at the time of their first attempt to conceive.
Concerns regarding pregnancy and cardiac complications
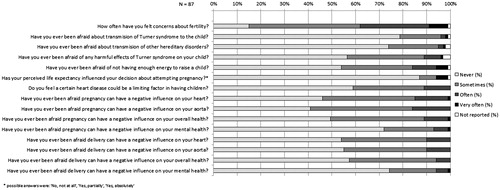
The results of the concerns questionnaire were available for 87 patients and are shown in : more than half of the patients had concerns about the influence of pregnancy or delivery on their cardiovascular status. shows the presence of concerns in TS women with cardiac abnormalities compared to those without. There were no significant differences in the concerns of women with and without pregnancy attempts. Women younger than 25 years of age (n = 31) seemed to have more concerns about the heredity of TS (36% versus 13%, p = .013), but less concerns about not having enough energy for raising a child (29% versus 55%, p = .022) and fewer concerns about a negative influence of pregnancy on their mental health (13% versus 36%, p = .023). After correction for multiple hypothesis testing (p < .0033 considered significant), none of these results were significantly different. No significant differences were found in the answers to the questionnaire between patients with (n = 37) versus without monosomy (n = 34).
Figure 2. Concerns about pregnancy in Turner patients with cardiac abnormalities compared to Turner patients without cardiac abnormalities. *p values of significance after Bonferroni’s correction: p=.00333
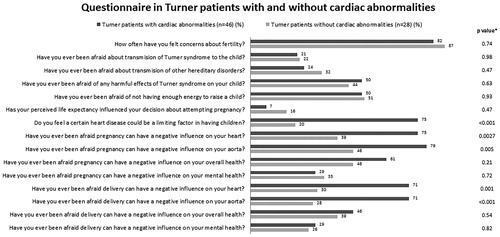
shows the results of the comparison of the questionnaires of the TS women with cardiac abnormalities in our cohort with the questionnaires of another cohort of women with congenital heart disease [Citation10]. The table shows that women with TS and cardiac abnormalities had more concerns than women with congenital heart disease regarding pregnancy risks, also related to the possible negative influence on their heart (75% versus 21%, p < .001).
Table 4. Concerns about pregnancy in Turner patients (with cardiac abnormalities) compared to other patients with congenital heart disease.
Discussion
In this study, we explored the wish to conceive and the concerns of cardiovascular complications during pregnancy in women with TS. Pregnancy had been attempted by 19.1% of all women, while only 3.4% had no wish for a child at all. More than half of all women with TS have or have had concerns about the influence of a potential pregnancy on their cardiovascular health. In women with TS and cardiac abnormalities this percentage was as high as 75%. Women with TS and cardiac abnormalities also had much more concerns regarding pregnancy and possible complications, than women with congenital heart disease.
Cardiovascular risks of reproductive therapy and Turner’s syndrome
Awareness of cardiovascular pregnancy risks in women with TS has evolved since 2003, when a study reported an estimated 2% risk of maternal mortality [Citation6] in pregnancy after oocyte donation. This percentage, however, was based on equivocal extrapolation of data. In the following 10 years, several papers were published containing retrospective data on pregnancy complications reporting aortic dissection rates during pregnancy of 0% (0/9[Citation12]; 0/13[Citation13]; and 0/18[Citation14]), 0.8% (1/122[Citation9]) and 2.2% (2/93[Citation8]). Most of these patients conceived through oocyte donation. In a national study that might have partially overlapped with one of these studies, one aortic dissection was found in 202 pregnancies (0.5%), where the majority conceived spontaneously [Citation15]. Outside pregnancy, the presence of aortic dilatation, a bicuspid aortic valve and hypertension are risk factors for aortic dissection in women with TS [Citation16]. However, also in the absence of these factors and with a normal diameter of the aorta, dissection has been reported. Hence, women with TS without aortic dilatation still need to be informed about these risks: not only about the risk of dissection but also about other pregnancy complications, like hypertension and early onset preeclampsia. A large Scandinavian study has shown the substantial risk of hypertensive complications during pregnancy in women with TS, who conceived by oocyte donation [Citation9]. In 35% of these patients, pregnancy induced hypertension or preeclampsia occurred, which might be both related to TS and oocyte donation.
Since cardiac screening of women with TS prior to conception is advocated by the European Society of Cardiology guidelines [Citation17], several studies have reported on the number of preconceptionally screened patients, which ranged from 37.6% to 48.7% [Citation6,Citation8,Citation9]. Apart from those that received the diagnosis of TS after pregnancy attempts or pregnancy, cardiac screening was performed in almost all women who attempted pregnancy in our cohort, except for one patient who delivered in 2009 and one patient who tried to become pregnant in the nineties.
Fertility and counseling
Fertility issues and TS are closely connected, and the majority of women in our cohort do seem to be informed about their situation. However, 12.4% of (mainly younger, median age 22 years) patients did not know whether they are fertile or not. In a previous study, nondisclosure or partial disclosure of the TS diagnosis or associated infertility appeared to be a common strategy of physicians toward their patients, mostly in consensus with the patient’s parents [Citation18]. Withholding such important information may induce fear, isolation and depression [Citation18,Citation19]. However, in recent research it seemed that mainly parents of very young children had barriers to communicate about fertility [Citation20]. Overprotective parents of the child with an (cardiac) anomaly influences the evolvement of body image and self-esteem, and parents should be guided in how to communicate with their child about reproductive matters [Citation21].
Patients with sex development disorders were previously reported to have difficulties with social interaction and impaired cognition, fewer experiences with sexual relationships and lack of initiative to finding a partner [Citation22,Citation23,Citation24]. Talking about these subjects may help to lower the thresholds for entering a relationship. Also, early puberty induction may optimize their psychosocial development [Citation25,Citation26]. When fertility is discussed, a patient should also be informed about her risks of pregnancy complications. Timing of this additional information should not be delayed to adult age. Although adolescents with TS are generally older when they become sexually active [Citation27], the age of onset of sexual intercourse decreases in the general population, and this may also happen in young patients with TS. In patients with congenital heart disease the (perceived) level of information regarding sexual activities and pregnancy seems to be deficient [Citation10]. In Marfan syndrome, where the risk of aortic dissection during pregnancy is much better documented, women reported not having started a family partly because of the chances for an affected child, but also because of worries for personal health in 30% of the study cohort [Citation28]. An increase in consciousness in reproductive decision-making was reported, similarly to some other genetic counseling populations. The authors do emphasize that this may also bring induce an undesired increased psychological burden.
Education about fertility and cardiovascular risks in women with TS by cardiologists and gynecologists should be adequately timed, and when necessary follow-up by a psychologist should be offered.
Anxiety and pregnancy
The women in this study seem to have much more concerns about pregnancy and delivery risks, particularly when they have a cardiac abnormality, than women with congenital heart disease assessed by the same questionnaire. The female patients in the reference cohort were older (median age 39) than in our study cohort, which could partly explain the fact that patients were less worried about pregnancy complications. Women were older and hence, might remember fewer concerns. However, comparing patients younger than 25 years to those older than 25, revealed no significant differences. Also, fertility is less of an issue in women without TS, which should be taken into account when interpreting our results.
It remains unknown if the difference between the two cohorts is due to information provided during counseling, or if this is associated with an underlying anxiety disorder or symptoms, which are known to be more common in women with TS [Citation1]. Furthermore, a previous study described that women with congenital heart disease who thought they were unable to bear a child, often had expressions of self-hate and a feeling of inadequacy as women [Citation21]. Regardless of the underlying cause, during pregnancy, stress symptoms have shown to be associated with adverse pregnancy outcomes [Citation29,Citation30,Citation31]. Thus, the presence of anxiety symptoms does warrant extra psychosocial care.
Clinical implications
Young women with TS, should be adequately informed about fertility issues, but also about the risks of pregnancy, irrespective of conceiving by spontaneous conception or oocyte donation [Citation32,Citation33,Citation34]. After full disclosure of risks, women should be offered not only psychosocial support regarding subfertility or infertility, but also regarding fear or concerns of pregnancy complications since this might influence their pregnancy outcome as well.
Limitations and future perspectives
Since a validated questionnaire about this topic was not available from literature, we derived questions from a questionnaire already used in a cohort study of women with congenital heart disease [Citation10]. We added questions focusing on the aorta and also on mental health. The questions were based on literature and clinical experience of experts in this field (JR;EU). However, since this is the first study using this questionnaire, future studies are needed to replicate our findings.
The initial response rate was quite low, which is probably related to the fact that people were approached through a nonmedical institution by airmail, so not in person, and first had to give their consent before questionnaires were sent. Since, we do not have data from nonresponders, we do not know to what extent a potential selection bias may have influenced our results. Overall, the age of women in our cohort was quite low, given the fact that all age categories are represented within the patient society. The topic of research is probably most appealing for women of young age who are considering their options of starting a family. Although this might induce a selection bias, the risk of recall bias is subsequently lower.
Finally, we did not report the medical fertility status, as opposed to the perception about fertility of women with TS in our cohort. It would be interesting to know whether there is a discrepancy between fertility and perceived fertility.
Conclusion
In this cohort, half of the women with TS currently or previously experienced fears and concerns about cardiac or aortic complications during pregnancy. This holds particularly for women with a cardiac abnormality. Information about these risks should be given, and psychosocial support during fertility and pregnancy counseling should be provided without restraint.
TS is often characterized by infertility.
An increasing number of women with TS can conceive through oocyte donation.
They have an increased risk of cardiovascular complications and potentially of aortic dissection during pregnancy.
Current knowledge on the subject:
Women with TS appeared to have considerable concerns about the influence of pregnancy on their heart and aorta.
This was even more pronounced in women with TS and cardiac abnormalities who showed much more concerns than other women with congenital heart disease.
Women should be adequately informed about the cardiovascular risks during pregnancy, but also screened for the need of additional psychological support to deal with these risks.
What this study adds:
Acknowledgements
We would like to thank the board of the Dutch Association of Turner Patients for their support in approaching Turner women in this study and their help in conducting the questionnaire.
Disclosure statement
The authors report no conflicts of interest.
References
- Sybert VP, McCauley E. Turner's syndrome. N Engl J Med 2004;351:1227–38.
- Stochholm K, Juul S, Juel K, et al. Prevalence, incidence, diagnostic delay, and mortality in Turner syndrome. J Clin Endocrinol Metab 2006;91:3897–902.
- Nederlands-Vlaams Multidisciplnair netwerk Turner Syndroom. Klinische richtlijn Turner Syndroom. The Netherlands, 2012.
- Gotzsche CO, Krag-Olsen B, Nielsen J, et al. Prevalence of cardiovascular malformations and association with karyotypes in Turner's syndrome. Arch Dis Child 1994;71:433–6.
- Mortensen KH, Erlandsen M, Andersen NH, Gravholt CH. Prediction of aortic dilation in Turner syndrome: enhancing the use of serial cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2013;15:47.
- Karnis MF, Zimon AE, Lalwani SI, et al. Risk of death in pregnancy achieved through oocyte donation in patients with Turner syndrome: a national survey. Fertil Steril 2003;80:498–501.
- Manalo-Estrella P, Barker AE. Histopathologic findings in human aortic media associated with pregnancy. Arch Pathol 1967;83:336–41.
- Chevalier N, Letur H, Lelannou D, et al. French Study Group for Oocyte D. Materno-fetal cardiovascular complications in Turner syndrome after oocyte donation: insufficient prepregnancy screening and pregnancy follow-up are associated with poor outcome. J Clin Endocrinol Metab 2011;96:E260–7.
- Hagman A, Loft A, Wennerholm UB, et al. Obstetric and neonatal outcome after oocyte donation in 106 women with Turner syndrome: a Nordic cohort study. Hum Reprod 2013;28:1598–609.
- Opic P, Roos-Hesselink JW, Cuypers JA, et al. Sexual functioning is impaired in adults with congenital heart disease. Int J Cardiol 2013;168:3872–7.
- Mortensen KH, Andersen NH, Gravholt CH. Cardiovascular phenotype in Turner syndrome-integrating cardiology, genetics, and endocrinology. Endocr Rev 2012;33:677–714.
- Bodri D, Vernaeve V, Figueras F, et al. Oocyte donation in patients with Turner's syndrome: a successful technique but with an accompanying high risk of hypertensive disorders during pregnancy. Hum Reprod 2006;21:829–32.
- Hadnott TN, Gould HN, Gharib AM, Bondy CA. Outcomes of spontaneous and assisted pregnancies in Turner syndrome: the US National Institutes of Health experience. Fertil Steril 2011;95:2251–6.
- Alvaro Mercadal B, Imbert R, Demeestere I, et al. Pregnancy outcome after oocyte donation in patients with Turner's syndrome and partial X monosomy. Hum Reprod 2011;26:2061–8.
- Hagman A, Kallen K, Barrenas ML, et al. Obstetric outcomes in women with Turner karyotype. J Clin Endocrinol Metab 2011;96:3475–82.
- Carlson M, Airhart N, Lopez L, Silberbach M. Moderate aortic enlargement and bicuspid aortic valve are associated with aortic dissection in Turner syndrome: report of the International Turner syndrome aortic dissection registry. Circulation 2012;126:2220–6.
- Regitz-Zagrosek V, Lundqvist CB, Borghi C, et al. CPG ECPG. ESC guidelines on the management of cardiovascular diseases during pregnancy The task force on the management of cardiovascular diseases during pregnancy of the European Society of Cardiology (ESC). Eur Heart J 2011;32:3147–97.
- Sutton EJ, Young J, McInerney-Leo A, et al. Truth-telling and Turner syndrome: the importance of diagnostic disclosure. J Pediatr 2006;148:102–7.
- Freedman B. The roles and responsibilities of the ethnics consultant. Hagerstown: University Publishing Group; 2000.
- King JE, Plamondon J, Counts D, et al. Barriers in communication and available resources to facilitate conversation about infertility with girls diagnosed with Turner syndrome. J Pediatr Endocrinol Metab 2016;29:185–91.
- Gantt LT. Growing up heartsick: the experiences of young women with congenital heart disease. Health Care Women Int 1992;13:241–8.
- Ediati A, Faradz SM, Juniarto AZ, et al. Emotional and behavioral problems in late-identified Indonesian patients with disorders of sex development. J Psychosom Res 2015;79:76–84.
- Ediati A, Juniarto AZ, Birnie E, et al. Body image and sexuality in Indonesian adults with a disorder of sex development (DSD). J Sex Res 2015;52:15–29.
- Hong DS, Dunkin B, Reiss AL. Psychosocial functioning and social cognitive processing in girls with Turner syndrome. J Dev Behav Pediatr 2011;32:512–20.
- Lagrou K, Froidecoeur C, Verlinde F, et al. Belgian Study Group of Pediatric E. Psychosocial functioning, self-perception and body image and their auxologic correlates in growth hormone and oestrogen-treated young adult women with Turner syndrome. Horm Res 2006;66:277–84.
- Carel JC, Elie C, Ecosse E, et al. Self-esteem and social adjustment in young women with Turner syndrome–influence of pubertal management and sexuality: population-based cohort study. J Clin Endocrinol Metab 2006;91:2972–9.
- Boman UW, Moller A, Albertsson-Wikland K. Psychological aspects of Turner syndrome. J Psychosom Obstet Gynaecol 1998;19:1–18.
- Peters KF, Kong F, Hanslo M, Biesecker BB. Living with Marfan syndrome III. Quality of life and reproductive planning. Clinical Genetics 2002;62:110–20.
- Wadhwa PD, Sandman CA, Porto M, et al. The association between prenatal stress and infant birth weight and gestational age at birth: a prospective investigation. Am J Obstet Gynecol 1993;169:858–65.
- Lobel M, Dunkel-Schetter C, Scrimshaw SC. Prenatal maternal stress and prematurity: a prospective study of socioeconomically disadvantaged women. Health Psychol 1992;11:32–40.
- Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol 1999;18:333–45.
- Udell JA, Lu H, Redelmeier DA. Long-term cardiovascular risk in women prescribed fertility therapy. J Am Coll Cardiol 2013;62:1704–12.
- Roos-Hesselink JW, Johnson MR. Does fertility therapy hamper cardiovascular outcome? J Am Coll Cardiol 2013;62:1713–4.
- Practice Committee of American Society for Reproductive M. Increased maternal cardiovascular mortality associated with pregnancy in women with Turner syndrome. Fertil Steril 2012;97:282–4.