Abstract
Introduction: Demoralization is a relatively neglected issue in which low morale and poor coping result from a stressor such as familial cancer risk. Female BRCA1/2 mutation carriers are highly susceptible for developing breast and ovarian cancer. The aim of this study was to evaluate demoralization in oophorectomized BRCA1/2 mutation carriers and its relation to quality of life.
Methods: This cross-sectional study examined 288 oophorectomized BRCA1/2 mutation carriers using the following standardized self-report measures: Demoralization Scale, EORTC Quality of Life Questionnaire-C30, State-Trait Anxiety Inventory and the Cancer Worry Scale.
Results: The mean score on the Demoralization Scale was 17.8 (SD 14.0). A clinically significant level of demoralization, defined as a score ≥30, was found in 45 BRCA1/2 mutation carriers (16%). Being highly demoralized was associated with a significantly lower quality of life, and higher levels of physical problems, anxiety and cancer worries. No demographic or clinical factors could predict higher levels of demoralization.
Conclusions: Our findings established that a clear proportion of oophorectomized BRCA1/2 mutation carriers experience demoralization impacting on their well-being. Further research is needed to explore the natural trajectory of demoralization and the resultant need for support in these women.
Introduction
Evidence grows showing that demoralization is a relevant factor influencing psychological well-being in patients with cancer and other medical diseases [Citation1,Citation2]. Demoralization, as described by Frank [Citation3], is experienced as a persistent inability to cope, together with feelings of helplessness, hopelessness, meaninglessness, subjective incompetence and diminished self-esteem. It is the burden of disease or suffering from a specific condition which highly determines the need for professional support, advocating for measures to assess the well-being of individual patients [Citation4].
Women with a germline mutation in one of the two breast cancer genes (BRCA1 and BRCA2) are at high risk for developing breast and ovarian cancer, 40–80% and 18–60%, respectively [Citation5–7]. To handle these high risks, female BRCA1/2 mutation carriers have to make decisions about risk-reducing strategies potentially affecting both physical and psychological well-being.
Options for breast cancer risk reduction consist of intensive surveillance or risk-reducing mastectomy (RRM), with the latter substantially reducing the breast cancer risk, but survival benefits are not yet confirmed [Citation8,Citation9]. Because of the absence of effective screening for ovarian cancer combined with its poor prognosis [Citation10], risk-reducing salpingo-oophorectomy (RRSO) is strongly recommended to all BRCA1/2 mutation carriers around the age of 40 years [Citation11]. RRSO highly reduces the risk of ovarian cancer [Citation12,Citation13], although a residual risk of peritoneal cancer (1–4%) remains [Citation14,Citation15]. Adverse effects of premature surgical menopause include short-term (e.g. vasomotor symptoms, sexual dysfunction) and possible long-term effects (e.g. osteoporosis, cardiovascular disease), which may not be fully alleviated by hormone replacement therapy (HRT) [Citation16–21].
Besides physical consequences, aspects of psychological distress are studied in BRCA1/2 mutation carriers. After risk-reducing surgery, health-related quality of life in BRCA1/2 mutation carriers is unaffected or only briefly diminished, and general and cancer-specific distress are decreased [Citation22–27]. The level of depressive symptoms and general anxiety have been low and seem to be unaffected by RRSO [Citation22,Citation23,Citation28].
In addition to physical and psychological functioning, existential well-being is an important determinant of quality of life [Citation29]. Demoralization, as described by Clarke and Kissane [Citation30], is a clearly defined syndrome of existential distress occurring in patients suffering from physical and psychiatric illness, including ones that threaten life or integrity of being. Hopelessness, the hallmark of demoralization, is associated with poor outcomes in illness [Citation30–32], and seems to be associated with a significantly increased risk of relapse or death at 5 and 10 years after early-stage breast cancer [Citation33,Citation34]. In cancer patients, demoralization is negatively associated with quality of life, and positively related to depression, anxiety and physical problems. Demoralization is not associated with cancer-related factors such as time since diagnosis, stage of disease and type of treatment [Citation2].
Concepts of demoralization or existential distress have hardly had any attention in research in BRCA1/2 mutation carriers of whom a substantial part may become breast cancer survivors at some point in their lives. BRCA1/2 mutation carriers are generally exposed to various overwhelming circumstances concerning health and family matters. The majority will be able to cope with existential challenges in the context of being a BRCA1/2 mutation carrier, and they may react with personal growth and a heightened sense of meaning and purpose in life [Citation35]. At the other end of the spectrum of responses to existential challenges, helplessness, hopelessness, confusion, low morale and pessimism might occur when patients feel they have failed their own or others’ expectations for coping with these life events, and then they may become demoralized [Citation30].
Demoralization might be a harbinger of clinical depression, exist co-morbidly with it or occur quite independently of depression [Citation2]. Depression is particularly characterized by anhedonia, the diminished ability to experience pleasure; whereas, demoralization is marked by low morale, pessimism and helplessness, without affecting the ability to enjoy the present moment [Citation30,Citation36]. Differentiation between demoralization and depression is of clinical importance in guiding the choice of appropriate therapy [Citation30,Citation37,Citation38].
The aim of this study was to evaluate the level of demoralization in oophorectomized BRCA1/2 mutation carriers and to test our hypothesis that higher levels of demoralization would be related to lower quality of life.
Methods
Participants and procedure
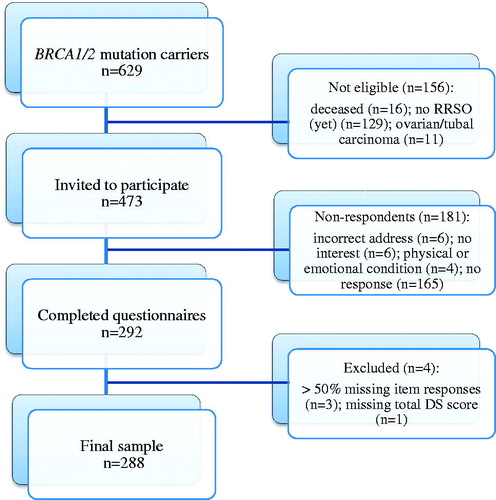
We performed a cross-sectional observational study of BRCA1/2 mutation carriers who underwent RRSO using validated questionnaires to assess demoralization, quality of life, general and specific anxiety. A total of 629 BRCA1/2 mutation carriers were identified at the Department of Obstetrics and Gynaecology of Radboud university medical center, Nijmegen, the Netherlands. All these BRCA1/2 mutation carriers were counseled at the Familial Cancer Clinic organizing integrated care for BRCA1/2 mutation carriers within the context of a multidisciplinary team including all professionals involved in prevention and management of breast and ovarian cancer (clinical geneticists, gynecologic oncologists, medical oncologists, (plastic) surgeons, pathologists, radiologists and social workers). During counseling by the gynecologic oncologists, BRCA1/2 mutation carriers were told about their estimated lifetime risk of ovarian cancer, RRSO as only evidence-based approach to reduce ovarian cancer risk, recommended age for RRSO, the effect of RRSO on ovarian cancer risk and menopause and possibility of HRT use. Of all identified women, 156 were excluded for not having an RRSO yet (n = 129), being deceased (n = 16) or diagnosed with ovarian cancer (n = 11). In total, 473 BRCA1/2 mutation carriers were eligible for participation and underwent an RRSO between November 1995 and May 2011 (), and were informed by letter about the aim and content of the study in June 2011. When consenting to participate, they were invited to fill in a digital questionnaire. Participation was strictly voluntary and the survey was confidential and anonymous. Questionnaires contained demographic and clinical information (age, parity, highest level of education, type of BRCA mutation, date of BRCA mutation analysis, date of RRSO, HRT use, hysterectomy, history of breast cancer, family history of breast and/or ovarian cancer and RRM). This study was not subject to the Dutch “Medical Research Involving Human Subjects Act” meaning no ethical approval was needed from the institutional review board of the Radboud university medical center.
Measures
The Dutch version of the Demoralization Scale (DS) is a 24-item self-report, validated questionnaire, developed to assess demoralization across cognitive, emotional, motivational and social dimensions [Citation31,Citation39]. Respondents report the frequency of each item over the last two weeks on a five-point Likert scale ranging from 0 (“never”) to 4 (“all the time”). The DS has five subscales describing loss of meaning and purpose (5 items), dysphoria (5 items), disheartenment (6 items), helplessness (4 items) and sense of failure (4 items). In this study, the DS had a Cronbach’s alpha of 0.95; for the subscales it ranged between 0.78 and 0.89. A total score may range from 0 to 96, and higher scores indicate more demoralization. The cutoff scores ≥30 and ≥36 were used to indicate moderate and high demoralization, respectively [Citation31,Citation35,Citation40]. The DS is able to differentiate a subset of patients who are demoralized and yet not clinically depressed [Citation1,Citation2].
The European Organization for Research and Treatment of Cancer (EORTC) developed a valid and reliable instrument measuring the quality of life of cancer patients: the Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30) (Dutch version 3) [Citation41,Citation42]. The EORTC QLQ-C30 is composed of both multi-item scales and single-item measures including five functional scales (physical, role, emotional, cognitive, social), three symptoms scales (fatigue, pain, nausea/vomiting), a global health status scale and six single items (dyspnoea, insomnia, appetite loss, constipation, diarrhea, financial difficulties), all concerning the past week. All of the scales range in score from 0 to 100. Higher scores in the global health status and functioning scales and lower scores in the symptom scale indicate better quality of life.
General anxiety was assessed using the Dutch version of the Spielberger State-Trait Anxiety Inventory (STAI) [Citation43,Citation44]. It contains two separate 20-item subscales that measure state anxiety (present anxiety) and trait anxiety (anxiety in general as a personality trait). The global score for each form is calculated as the sum of the 20 items ranging from 20 to 80. Higher scores indicate more severe anxiety.
To assess patients’ worries about the remaining risk of peritoneal cancer in the previous month, the Dutch version of the 8-item Cancer Worry Scale (CWS) was used. The CWS was originally designed as a six-item scale to measure worry about cancer recurrence and the impact of worry on daily functioning [Citation45,Citation46]. Douma et al. [Citation47] added two general items to address worries about family members and future surgery (items 7 and 8). We specifically asked for the fear of the remaining risk of peritoneal cancer (items 1–6) instead of cancer in general, and thereby we left the fear of (recurrent) breast cancer out of consideration. Scores range from 8 to 32. In breast cancer survivors, a cutoff score of 13 (low) versus 14 (high) seemed optimal to detect severe levels of fear [Citation48].
Statistical analysis
We computed the sum scores of the validated questionnaires as indicated. We handled the less than 1% missing data of the DS by imputing items from multi-item scales: subscales were calculated if at least half of the items from that subscale were completed. Means and percentages were used to describe baseline characteristics and all measured psychological variables. We tested the distribution of the data for normality using Kolmogorov–Smirnov. The DS was categorized into three groups (low <30; moderate 30–35; high >35) [Citation31,Citation35,Citation40]. Correlations were used to test associations between the three levels of demoralization and other psychological and physical problems. Univariate logistic analysis was used to identify demographic and clinical factors associated with high demoralization. Statistical analysis was performed using SPSS software version 20.0 (SPSS Inc., Chicago, IL). A two-sided p values <.05 was considered statistically significant.
Results
Participants
In total 473 women were invited to participate, of who 292 (62%) completed the questionnaire. Data from four women were excluded because in three cases more than 50% of item responses were missing, and in one case the total DS score could not be calculated because of missing values. The final study sample consisted of 288 BRCA1/2 mutation carriers (). Characteristics of all participants are listed in . Of the excluded women for not having an RRSO (yet), 120 of 129 (93%) were under or at the recommended age of RRSO.
Table 1. Demographic and clinical characteristics of the respondents (n = 288).
Demoralization and psychological factors
The results for demoralization, quality of life, anxiety and worries about future peritoneal cancer are reported in . A clinically relevant level of demoralization was found in 45 BRCA1/2 mutation carriers (16%); 15 women were moderately demoralized (5.2%) and 30 women were highly demoralized (10.4%).
Table 2. Demoralization, quality of life and anxiety.
The mean score on global health status in oophorectomized BRCA1/2 mutation carriers was 76.3 (SD 17.6). Overall, the specific quality of life measured by the five functioning scales was high, and symptoms were low, in particular, the global level of emotional functioning did not suggest concern for clinical depression.
Worries about peritoneal cancer were generally low in BRCA1/2 mutation carriers. Especially, specific worries about residual risk of peritoneal cancer (items 1–6) were low (6.8 (SD 1.6)); 65% of the women had no worries about this risk at all, and only six women (2%) reported (very) frequent worries. General worries (items 7 and 8) about risk of cancer in their family or potential need for (additional) surgery in the future were reported in a substantial part of the BRCA1/2 mutation carriers, 32% and 10%, respectively. When using the cutoff score from the literature to detect severe levels of fear of recurrence [Citation48], in our study 12% of the BRCA1/2 mutation carriers reported severe levels of worries about peritoneal cancer.
Demoralization associated with psychological, clinical and demographic factors
Oophorectomized BRCA1/2 mutation carriers who were highly demoralized had a significantly lower global health status (Spearman’s rho (rs) = −0.459, p < .001), and scored worse on all functioning dimensions (). Regarding the item about feeling depressed within the EORTC QLQ-C30, a high correlation with demoralization was found (rs = −0.580, p < 0.001). Both general anxiety and cancer worry were positively related to demoralization. Higher levels of demoralization were also associated with more physical problems, especially fatigue and insomnia (rs = 0.338 and rs = 0.349, both p < .001). Furthermore, a correlation was found between financial difficulties and demoralization (rs = 0.327, p < .001) (). No demographic or clinical factors were associated with moderate to high demoralization using univariate logistic analysis; and therefore no multivariate logistic regression was performed ().
Table 3. Correlations between demoralization and psychological and physical variables.
Table 4. Univariate logistic analysis for moderate to high demoralization (DS ≥30) by demographic and clinical factors.
Discussion
Overall, low levels of demoralization were found in oophorectomized BRCA1/2 mutation carriers; although, for a substantial minority (16%) clinically relevant levels of demoralization occurred. Being demoralized was significantly associated with lower quality of life and higher levels of general and cancer-specific anxiety.
The levels of demoralization in oophorectomized BRCA1/2 mutation carriers were lower than found in a systematic review of cancer patients in general [Citation2]. Unfortunately, data on demoralization in the general population are lacking; only one Dutch study on demoralization in opioid-dependent patients used a community-based sample and cancer patients as reference groups, reporting a slightly higher level of demoralization in the community-based sample than in our study [Citation39].
In mainly Italian studies, demoralization has been assessed by a categorical measurement, the Diagnostic Criteria for Psychosomatic Research (DCPR) [Citation49] reporting demoralization in 20–34% of the patients with different medical diseases [Citation50–54]. Comparing this structured interview with the DS, the DS appears to be more clinically useful as it is likely that demoralization exists on a continuum ranging from what would be a normal response to one that would be characterized as dysfunctional. In addition, the most recent edition of the DSM, the DSM-V [Citation55], acknowledges the limitations of categorical diagnosis and has shifted the conceptualization of some disorders to a dimensional focus.
Concentrating on the clinical significance of demoralization, different thresholds have been utilized to quantify meaningful presence of demoralization [Citation2,Citation31,Citation35,Citation40]. For our study, we used the cutoff scores for moderate demoralization (30–35) and high demoralization (≥36), derived from studies by Kissane et al. [Citation31] and Vehling et al. [Citation35,Citation40]. Moderate and high levels of demoralization in cancer patients were observed in 8–11% and 9–17%, respectively [Citation35,Citation40,Citation56] which is higher than our results.
Overall, we found normal to high levels of general and specific quality of life, and low levels of anxiety. Our results are in accordance with studies on the impact of RRSO on quality of life and anxiety, reporting normal levels and no changes after RRSO, although further comparisons seems difficult due to small samples and different study populations, designs and questionnaires [Citation22,Citation23,Citation57,Citation58,Citation59,Citation60].
To our knowledge, worries about residual risk of peritoneal cancer after RRSO have not been studied previously; we found low levels of fear of residual risk of peritoneal cancer. Twelve percent of all BRCA1/2 mutation carriers had a severe level of worries, which is lower compared to earlier studies showing that about 20% of the women still had significant ovarian cancer-specific worries after RRSO [Citation22,Citation58,Citation59]. Most of the reported worries in our study were about risk of cancer in family members and future surgery. Possible explanations for low worries about peritoneal cancer could be that women were not (well) informed about the residual risk, could not remember the given information, or concluded that the residual risk of 1–4% is small, and not worth worrying about.
We found a strong negative association between demoralization and health-related quality of life. Anxiety, depression and cancer worries were highly related to demoralization. The relationships between quality of life, depression and anxiety to demoralization were consistently confirmed in the literature on cancer patients, and mixed results were reported for age, education and cancer site [Citation2]. Uniformly, no association was found between demoralization and time since diagnosis, stage of disease and type of treatment [Citation2]. In our sample, no association was found for age, parity, education level, history of breast cancer, HRT use after RRSO, family history and RRM.
Presumably, many physicians will meet demoralized patients, and the confusion with depressed patients is easily made when not being familiar with the concept of demoralization. When a threat occurs that we need to cope with, we normally sustain our morale. If disappointment or a mild or fleeting level of demoralization occurs, we help with encouragement and support. But once moderate or severe demoralization occurs, clinicians can do a lot to help assuage this distress and impairment. In addition, Clarke and Kissane [Citation30] stated that helping a demoralized person is the role of every health professional and is achieved most importantly through a relationship characterized by empathic resonance, combined with good physical care and symptomatic relief. It may be helpful for physicians to familiarize themselves with the concept of demoralization to better inform and support BRCA1/2 mutation carriers who exhibit symptoms of demoralization.
Highly demoralized persons could benefit from specialist support. Different styles of psychotherapy may usefully address specific problems in a demoralized patient, including brief bed-side therapy and meaning-centered psychotherapy [Citation37,Citation38,Citation61]. Strong support is provided for the efficacy of meaning-centered psychotherapy for hopelessness, as a hallmark of demoralization, in advanced cancer patients [Citation61–63]. We are waiting for results of a randomized controlled trial started on this concept in cancer survivors [Citation64]. Furthermore, differentiation between depression and demoralization is relevant in the treatment setting [Citation65–67]: antidepressant medication helps patients who have depression/melancholia but by itself does little to relieve demoralization, while psychotherapy is helpful in demoralized patients, but has limited effects for patients who have entrenched anhedonia [Citation38].
Qualitative research could be useful to explore in-depth the experiences of BRCA1/2 mutation carriers with demoralization. Further longitudinal research could provide insight in the natural trajectory of demoralization in BRCA1/2 mutation carriers and its relation to the specific events allied to being a BRCA1/2 mutation carrier.
To our knowledge, we are the first to describe the concept of demoralization in oophorectomized BRCA1/2 mutation carriers. The large sample size is a strength of our study. Important limitations of our study are the cross-sectional design, and the lack of controls. The presence of demoralization will change over time; however, our study gives no insight into this. Unfortunately, we did not measure depression with a validated depression scale to explore its comorbidity with or differentiation from demoralization, which should be assessed in further research.
In conclusion, demoralization is low in oophorectomized BRCA1/2 mutation carriers; although a substantial minority has clinically relevant levels of demoralization. Demoralization is highly associated with lower quality of life, and higher anxiety. Detecting demoralization in BRCA1/2 mutation carriers could be useful because these women face different stressful circumstances related to being a BRCA1/2 mutation carrier, potentially arousing existential distress. Identifying highly demoralized BRCA1/2 mutation carriers gives the opportunity to offer appropriate treatment to contribute to a better quality of life.
Hopelessness is the hallmark of demoralization.
Demoralization influences well-being in cancer patients.
Being a female BRCA1/2 mutation carrier has physical and psychological impact.
Current knowledge on the subject
Demoralization is generally low in oophorectomized BRCA1/2 mutation carriers.
One out of six BRCA1/2 mutation carriers are moderately to highly demoralized.
Being demoralized has a negative impact on well-being in BRCA1/2 mutation carriers.
What this study adds
Disclosure statement
N. Hoogerbrugge acts as consultant for Astra Zeneca since June 2014. None of the other authors have conflicts of interest to declare.
References
- Mangelli L, Fava GA, Grandi S, et al. Assessing demoralization and depression in the setting of medical disease. J Clin Psychiatry 2005;66:391–4.
- Robinson S, Kissane DW, Brooker J, Burney S. A systematic review of the demoralization syndrome in individuals with progressive disease and cancer: a decade of research. J Pain Symptom Manage 2015;49:595–610.
- Frank JD. Psychotherapy: the restoration of morale. Am J Psychiatry 1974;131:271–4.
- Thornicroft G, Slade M. New trends in assessing the outcomes of mental health interventions. World Psychiatry 2014;13:118–24.
- Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 2007;25:1329–33.
- King MC, Marks JH, Mandell JB, Group NYBCS. Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 2003;302:643–6.
- Antoniou A, Pharoah PD, Narod S, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 2003;72:1117–30.
- Heemskerk-Gerritsen BA, Menke-Pluijmers MB, Jager A, et al. Substantial breast cancer risk reduction and potential survival benefit after bilateral mastectomy when compared with surveillance in healthy BRCA1 and BRCA2 mutation carriers: a prospective analysis. Ann Oncol 2013;24:2029–35.
- Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol 2004;22:1055–62.
- Hermsen BB, Olivier RI, Verheijen RH, et al. No efficacy of annual gynaecological screening in BRCA1/2 mutation carriers; an observational follow-up study. Br J Cancer 2007;96:1335–42.
- Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst 2009;101:80–7.
- Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA 2010;304:967–75.
- Finch AP, Lubinski J, Moller P, et al. Impact of oophorectomy on cancer incidence and mortality in women with a BRCA1 or BRCA2 mutation. J Clin Oncol 2014;32:1547–53.
- Finch A, Beiner M, Lubinski J, et al. Salpingo-oophorectomy and the risk of ovarian, fallopian tube, and peritoneal cancers in women with a BRCA1 or BRCA2 Mutation. JAMA 2006;296:185–92.
- Dowdy SC, Stefanek M, Hartmann LC. Surgical risk reduction: prophylactic salpingo-oophorectomy and prophylactic mastectomy. Am J Obstet Gynecol 2004;191:1113–23.
- Challberg J, Ashcroft L, Lalloo F, et al. Menopausal symptoms and bone health in women undertaking risk reducing bilateral salpingo-oophorectomy: significant bone health issues in those not taking HRT. Br J Cancer 2011;105:22–7.
- Madalinska JB, van Beurden M, Bleiker EM, et al. The impact of hormone replacement therapy on menopausal symptoms in younger high-risk women after prophylactic salpingo-oophorectomy. J Clin Oncol 2006;24:3576–82.
- Atsma F, Bartelink ML, Grobbee DE, van der Schouw YT. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause (New York, NY) 2006;13:265–79.
- Rocca WA, Grossardt BR, Maraganore DM. The long-term effects of oophorectomy on cognitive and motor aging are age dependent. Neurodegener Dis 2008;5:257–60.
- Svejme O, Ahlborg HG, Nilsson JA, Karlsson MK. Early menopause and risk of osteoporosis, fracture and mortality: a 34-year prospective observational study in 390 women. BJOG 2012;119:810–16.
- Finch A, Metcalfe KA, Chiang JK, et al. The impact of prophylactic salpingo-oophorectomy on menopausal symptoms and sexual function in women who carry a BRCA mutation. Gynecol Oncol 2011;121:163–8.
- Finch A, Metcalfe KA, Chiang J, et al. The impact of prophylactic salpingo-oophorectomy on quality of life and psychological distress in women with a BRCA mutation. Psychooncology 2013;22:212–19.
- Fang CY, Cherry C, Devarajan K, et al. A prospective study of quality of life among women undergoing risk-reducing salpingo-oophorectomy versus gynecologic screening for ovarian cancer. Gynecol Oncol 2009;112:594–600.
- Brandberg Y, Sandelin K, Erikson S, et al. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: a prospective 1-year follow-up study. J Clin Oncol 2008;26:3943–9.
- Gopie JP, Mureau MA, Seynaeve C, et al. Body image issues after bilateral prophylactic mastectomy with breast reconstruction in healthy women at risk for hereditary breast cancer. Fam Cancer 2013;12:479–87.
- den Heijer M, Seynaeve C, Timman R, et al. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: a prospective long-term follow-up study. Eur J Cancer 2012;48:1263–8.
- Bresser PJ, Van Gool AR, Seynaeve C, et al. Who is prone to high levels of distress after prophylactic mastectomy and/or salpingo-ovariectomy? Ann Oncol 2007;18:1641–5.
- Bresser PJ, Seynaeve C, Van Gool AR, et al. The course of distress in women at increased risk of breast and ovarian cancer due to an (identified) genetic susceptibility who opt for prophylactic mastectomy and/or salpingo-oophorectomy. Eur J Cancer 2007;43:95–103.
- Cohen SR, Mount BM, Tomas JJ, Mount LF. Existential well-being is an important determinant of quality of life. Evidence from the McGill Quality of Life Questionnaire. Cancer 1996;77:576–86.
- Clarke DM, Kissane DW. Demoralization: its phenomenology and importance. Aust N Z J Psychiatry 2002;36:733–42.
- Kissane DW, Wein S, Love A, et al. The Demoralization Scale: a report of its development and preliminary validation. J Palliat Care 2004;20:269–76.
- Breitbart W, Rosenfeld B, Pessin H, et al. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA 2000;284:2907–11.
- Watson M, Haviland JS, Greer S, et al. Influence of psychological response on survival in breast cancer: a population-based cohort study. Lancet 1999;354:1331–6.
- Watson M, Homewood J, Haviland J, Bliss JM. Influence of psychological response on breast cancer survival: 10-year follow-up of a population-based cohort. Eur J Cancer 2005;41:1710–14.
- Vehling S, Mehnert A. Symptom burden, loss of dignity, and demoralization in patients with cancer: a mediation model. Psychooncology 2014;23:283–90.
- de Figueiredo JM. Depression and demoralization: phenomenologic differences and research perspectives. Compr Psychiatry 1993;34:308–11.
- Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics 2005;46:109–16.
- Clarke DM, Chapter 7. Depression, demoralization, and psychotherapy in people who are medically ill. In: Alarcon RD, Frank JB, eds. The psychotherapy of hope: the legacy of persuasion and healing. Baltimore: Johns Hopkins University Press; 2012.
- De Jong CAJ, Kisanne DW, Geessink RJ, van der Velden D. Demoralization in opioid dependent patients: a comparative study with cancer patients and community subjects. Open Addict J 2008;1:7–9.
- Vehling S, Lehmann C, Oechsle K, et al. Is advanced cancer associated with demoralization and lower global meaning? The role of tumor stage and physical problems in explaining existential distress in cancer patients. Psychooncology 2012;21:54–63.
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365–76.
- Fayers PM, Aaronson NK, Bjordal K, et al. The EORTC QLQ-C30 scoring manual. 3rd ed. Brussel: European Organisation for Research and Treatment of Cancer; 2001.
- Spielberger CD, Lushene RE, Jacobs GA, Manual for the State-Trait Anxiety Inventory, STAI (Form Y). Palo Alto (CA): Consulting Psychologists Press; 1983.
- van der Ploeg HM. Self-assessment Questionnaire (STAI-DY) – development and validation of Dutch questionnaire to measure anxiety. Tijdschrift Voor Psychiatrie 1982;24:576–88.
- Lerman C, Daly M, Masny A, Balshem A. Attitudes about genetic testing for breast-ovarian cancer susceptibility. J Clin Oncol 1994;12:843–50.
- Watson M, Duvivier V, Wade Walsh M, et al. Family history of breast cancer: what do women understand and recall about their genetic risk? J Med Genet 1998;35:731–8.
- Douma KFL, Aaronson NK, Vasen HFA, et al. Psychological distress and use of psychosocial support in familial adenomatous polyposis. Psychooncology 2010;19:289–98.
- Custers JA, van den Berg SW, van Laarhoven HW, et al. The cancer worry scale: detecting fear of recurrence in breast cancer survivors. Cancer Nurs 2014;37:E44–50.
- Fava GA, Mangelli L, Ruini C. Assessment of psychological distress in the setting of medical disease. Psychother Psychosom 2001;70:171–5.
- Rafanelli C, Roncuzzi R, Milaneschi Y, et al. Stressful life events, depression and demoralization as risk factors for acute coronary heart disease. Psychother Psychosom 2005;74:179–84.
- Grassi L, Sabato S, Rossi E, et al. Use of the diagnostic criteria for psychosomatic research in oncology. Psychother Psychosom 2005;74:100–7.
- Grandi S, Sirri L, Tossani E, Fava GA. Psychological characterization of demoralization in the setting of heart transplantation. J Clin Psychiatry 2011;72:648–54.
- Porcelli P, De Carne M, Todarello O. Prediction of treatment outcome of patients with functional gastrointestinal disorders by the diagnostic criteria for psychosomatic research. Psychother Psychosom 2004;73:166–73.
- Sonino N, Navarrini C, Ruini C, et al. Persistent psychological distress in patients treated for endocrine disease. Psychother Psychosom 2004;73:78–83.
- American Psychiatric Association. and American Psychiatric Association. DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association, 2013.
- Vehling S, Oechsle K, Koch U, Mehnert A. Receiving palliative treatment moderates the effect of age and gender on demoralization in patients with cancer. PLoS One 2013;8:e59417.
- Touboul C, Uzan C, Ichante JL, et al. Factors associated with altered long-term well-being after prophylactic salpingo-oophorectomy among women at increased hereditary risk for breast and ovarian cancer. Oncologist 2011;16:1250–7.
- Madalinska JB, Hollenstein J, Bleiker E, et al. Quality-of-life effects of prophylactic salpingo-oophorectomy versus gynecologic screening among women at increased risk of hereditary ovarian cancer. J Clin Oncol 2005;23:6890–8.
- Robson M, Hensley M, Barakat R, et al. Quality of life in women at risk for ovarian cancer who have undergone risk-reducing oophorectomy. Gynecol Oncol 2003;89:281–7.
- Elit L, Esplen MJ, Butler K, Narod S. Quality of life and psychosexual adjustment after prophylactic oophorectomy for a family history of ovarian cancer. Fam Cancer 2001;1:149–56.
- Breitbart W, Rosenfeld B, Pessin H, et al. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Oncol 2015;33:749–54.
- Breitbart W, Poppito S, Rosenfeld B, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol 2012;30:1304–9.
- Lethborg C, Schofield P, Kissane D. The advanced cancer patient experience of undertaking meaning and purpose (MaP) therapy. Palliat Support Care 2012;10:177–88.
- van der Spek N, Vos J, van Uden-Kraan CF, et al. Effectiveness and cost-effectiveness of meaning-centered group psychotherapy in cancer survivors: protocol of a randomized controlled trial. BMC Psychiatry 2014;14:22.
- Clarke DM, Mackinnon AJ, Smith GC, et al. Dimensions of psychopathology in the medically ill. A latent trait analysis. Psychosomatics 2000;41:418–25.
- Clarke DM, Smith GC, Dowe DL, McKenzie DP. An empirically derived taxonomy of common distress syndromes in the medically ill. J Psychosom Res 2003;54:323–30.
- Clarke DM, Kissane DW, Trauer T, Smith GC. Demoralization, anhedonia and grief in patients with severe physical illness. World Psychiatry 2005;4:96–105.