Abstract
Objective: To evaluate the effect of haptotherapy on severe fear of childbirth in pregnant women.
Design: Randomized controlled trial.
Setting: Community midwifery practices and a teaching hospital in the Netherlands.
Population or Sample: Primi- and multigravida, suffering from severe fear of childbirth (N = 134).
Methods: Haptotherapy, psycho-education via Internet and care as usual were randomly assigned at 20–24 weeks of gestation and the effects were compared at 36 weeks of gestation and 6 weeks and 6 months postpartum. Repeated measurements ANOVA were carried out on the basis of intention to treat. Since there were crossovers from psycho-education via Internet and care as usual to haptotherapy, the analysis was repeated according to the as treated principle.
Main outcome measures: Fear of childbirth score at the Wijma Delivery Expectancy/Experience Questionnaire.
Results: In the intention to treat analysis, only the haptotherapy group showed a significant decrease of fear of childbirth, F(2,99) = 3.321, p = .040. In the as treated analysis, the haptotherapy group showed a greater reduction in fear of childbirth than the other two groups, F(3,83) = 6.717, p < .001.
Conclusion: Haptotherapy appears to be more effective in reducing fear of childbirth than psycho-education via Internet and care as usual.
Introduction
Approximately 10% of pregnant women suffer from severe fear of childbirth [Citation1–7]. The etiology of fear of childbirth is likely to be multifactorial and may be related to a more general anxiety proneness, as well as to specific fears [Citation8–16]. Women with severe fear of childbirth and their newborns are at increased risk of various complications, such as pre-term birth [Citation17,Citation18], gestational hypertension and pre-eclampsia [Citation19], emergency cesarean section [Citation20], extra use of pain medication during birth [Citation21,Citation22], low birthweight [Citation23], prolonged birth and trauma anxiety [Citation24], increased risk of postpartum post-traumatic stress and depression [Citation24] and, later-on, emotional and behavioral problems of the child [Citation23].
Several studies have evaluated interventions designed to reduce fear of childbirth [Citation25]. Saisto et al. studied group psycho-education consisting of information and discussion of previous obstetric experiences, current feelings and misconceptions [Citation26]. Salmelo-Aro studied group psycho-education consisting six sessions during pregnancy and one after childbirth [Citation27]. Rouhe et al. compared group psycho-education including relaxation exercises with conventional care [Citation28,Citation29]. Toohill et al. and Fenwick et al. studied individual psycho-education by telephone in women with moderate to severe fear of childbirth [Citation30,Citation31]. Nieminen et al. performed a feasibility study for an Internet-delivered therapist-supported self-help program according to cognitive behavior therapy [Citation32]. These studies all reported a decrease of fear of childbirth and showed a reduction in cesarean birth, interventions and psychosocial factors. However, they provide little information about long term clinically meaningful psychological health outcomes.
Attempts to decrease fear of childbirth in pregnant women are not always successful. For instance, Ryding et al. found that new mothers who had consulted specially trained midwives because of fear of childbirth during pregnancy afterward reported a more frightening experience of birth and more frequent symptoms of post-traumatic stress related to birth than women in the comparison group [Citation33]. Moreover, in a study among pregnant women with a DSM-IV anxiety diagnosis, Verbeek et al. found that the mean birth weight was over 275 g lower and the mean gestational age almost a week shorter in a cognitive behavioral therapy group than in their care as usual group [Citation34].
During the past decade, clinical experience has suggested that fear of childbirth might be effectively reduced by means of haptotherapy [Citation35]. The haptotherapy exercises have been designed to create a change in the woman’s perception of her pregnancy and to promote a more positive attitude towards pregnancy and childbirth. In addition, through haptotherapy, the pregnant woman may improve her readiness for the upcoming labor process, which in turn, is expected to result in a decrease of her fear of childbirth [Citation25,Citation35].
To evaluate the effect of haptotherapy on fear of childbirth, we compared haptotherapy with psycho-education via the Internet and care as usual as control conditions in a randomized controlled study. The main research question was as follows: (1) Do pregnant women with severe fear of childbirth after haptotherapy have a lower fear of childbirth than women who received psycho-education via Internet or care as usual? The secondary research questions were as follows: (2) Do women with severe fear of childbirth who received haptotherapy have a better mental wellbeing during pregnancy and postpartum than women who received Internet-psycho-education or care as usual and (3) Do they have fewer medical interventions during birth?
Method
Design
Between April 2012 and June 2015, pregnant women were recruited through 35 Dutch community midwifery practices, gynecologists at a teaching hospital and the project’s website. Women who provided informed consent received a login code by email and were requested to digitally complete the Wijma Delivery Expectancy/Experience Questionnaire (W-DEQ). Inclusion criteria for the intervention study were singleton pregnancy, age ≥ 18 years and a W-DEQ score ≥ 85, i.e., suffering from severe fear of childbirth [Citation36]. Exclusion criteria were multiple pregnancies and a history of psychotic episodes. The participants were randomly [Citation37] assigned to (1) haptotherapy, (2) psycho-education via the Internet or (3) care as usual.
Interventions
Haptotherapy
In the Netherlands, pregnant women recognized with severe fear of childbirth would ordinarily visit a psychologist or psychiatrist. However, these women can also directly contact a certified healthcare haptotherapist who is specialized in the treatment of pregnant women with severe fear of childbirth. Haptotherapy claims to facilitate the development of specific skills changing the cognitive appraisal of giving birth and labeling childbirth as a more normal and positive life event, which may ultimately lower fear of childbirth. This intervention, described in detail by Klabbers et al. [Citation35], consists of training participants in a combination of skills, which are taught in eight 1 h sessions between gestational week 20 and 36. Preferably, the partner of the pregnant woman also attends every session and participates actively in several exercises [Citation38].
Psycho-education via the Internet
Psycho-education via the Internet consisted of eight modules (and a brief test) during a period of 8 weeks between gestational week 20 and 36, providing information about the normal course of pregnancy, labor and birth [Citation39]. Participants also could ask questions about their own situation.
Care as usual
Care as usual was conducted according to the standards of the Royal Dutch Organization of Midwives (KNOV) [Citation40] and the Dutch Organization of Obstetrics and Gynaecology (NVOG) [Citation41].
Although healthcare-haptotherapists who are working in primary healthcare in the Netherlands are directly accessible to the public without the necessary intervention of a GP or specialist, haptotherapy was not available as part of care as usual. Some of the participants, who had been allocated to the psycho-education via Internet group or the care as usual group, however, were aware of the other treatment arms and violated the protocol by switching to haptotherapy. These participants were considered as crossovers.
Measures
Fear of childbirth was measured using the W-DEQ [Citation9,Citation36], with 33 items on a 6-point Likert scale ranging from ‘not at all’ (=0) to ‘extremely’ (=5). Internal consistency and split-half reliability of the W-DEQ is 0.87. A W-DEQ score of ≥ 85 is considered to signify severe fear of childbirth [Citation36]. In the current study, at T1, the Cronbach’s α was 0.95. Distress, anxiety, depression and somatization were assessed using the Four Dimensional Symptom Questionnaire (4DSQ) [Citation44]. This measure contains 50 psychological and psychosomatic symptoms according to DSM-IV [Citation45]. In the present study, at T1, Cronbach’s α was 0.94. Social support – as a potential confounder – was measured by the Social Support Questionnaire (SSQ) [Citation46], with a Cronbach’s α of 0.92. Post-Traumatic Stress Disorder (PTSD) following childbirth was measured by the Traumatic Event Scale (TES) [Citation24]. This measure comprises all the DSM-IV symptoms and criteria of PTSD [Citation45] (Cronbach’s α= 0.88). We additionally collected information about baseline characteristics, birth complications and medical interventions [Citation35].
Procedure
The questionnaires were sent by e-mail on four occasions: admission to the study at 20–24 weeks of gestation (T1), 36 weeks of gestation (T2), 6 weeks postpartum (T3) and 6 months postpartum (T4). The project had a secured Internet environment to facilitate the completion of the online questionnaires.
After the approval of the Dutch Medical Ethics Review Committee (ABR number: NL34900.008.11), the original protocol was modified as follows: (1) Pregnant women initially received the information letter, in which they were asked to participate, in week 8–12 of gestation. Given the low response rates, following the recommendation of the participating midwives: (1) the baseline was brought forward to week 20–24 of gestation; (2) after 8 months, the inclusion criterion ‘primigravida’ was expanded with ‘multigravida’; (3) after 8 months of study, we started a special research website through which pregnant women could also sign up directly to participate in our study.
Statistical analyses
Intention to treat analyses
To evaluate the effects of haptotherapy on fear of childbirth, we compared the W-DEQ means of the haptotherapy group at T2 with the means of the psycho-education via Internet and care as usual groups, using repeated measures analysis of variance (ANOVA), followed by two planned pair-wise comparisons to test pair-wise group mean differences (i.e., haptotherapy treatment versus care as usual, and haptotherapy versus psycho-education via Internet). The experiment-wise Type I error rate was set at 5% level. For the post-hoc comparisons, we used a Bonferroni-corrected alpha of 0.05/2 = 0.025 for each single comparison. To exclude the influence of birth, we focused on the first two measurements, i.e., (T1) at 20 weeks of gestation, and (T2) 36 weeks of gestation, directly after the intervention.
Applying Jacobson and Truax’s criteria, we defined a decrease of a W-DEQ score of minimally 16 points to <85 as a clinically significant change [Citation47]. For the secondary research questions, we ran a series of multiple regression analyses with the predictors W-DEQ and Social Support at T1. As dependent variables, we used the changes in distress, depression, somatization and anxiety between T1 and T2, and postpartum PTSD symptoms at T3. The kind of intervention (haptotherapy, psycho-education via Internet or care as usual) was also used as a predictor.
Power analysis
Concerning the primary research question, we performed an a-priori power analysis with GPower3.0 [Citation48]. For the planned pair-wise comparisons, to detect medium or larger effects (i.e., Cohen’s d ≥ 0.5 [Citation49]) with at least 80% power and a Bonferroni corrected alpha of 0.025, a minimal sample size of 64 in each group was needed.
Effect of treatment as received
In case of non-adherence to assigned treatment and crossing over between treatments, we additionally compared W-DEQ scores, at post-test, using groups defined by the treatment as received (as treated analysis) [Citation50]. To gauge possible confounding, we compared the baseline characteristics of the as treated groups.
Results
Sample characteristics
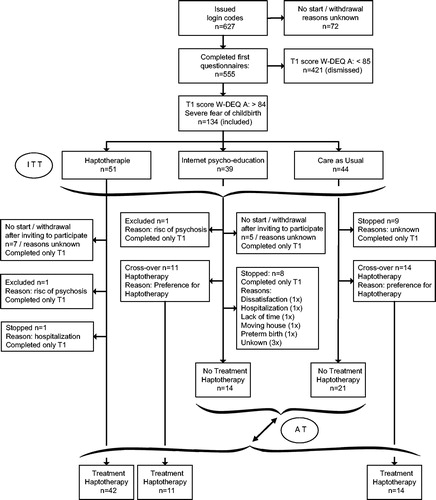
After 3 years, recruitment numbers showed a sharp decline and we decided to end the data collection. Consequently, we did not reach the predetermined number of inclusions. At T1, data were obtained from 555 respondents (see for the full details). The inclusion criterion of severe fear of childbirth was met by 134 women (24.2%), who were randomized (haptotherapy: n = 51; psycho-education via Internet: n = 39; care as usual: n = 44).
Not all participants adhered to the intervention to which they were assigned. Eleven assigned to the psycho-education via Internet group switched to the haptotherapy group on their own initiative, as did 14 who had been assigned to the care as usual group. Also, 32 participants dropped out (haptotherapy: n = 9; psycho-education via Internet: n = 14, care as usual: n = 9: see ).
Baseline characteristics
shows the baseline characteristics and measurements of the three groups haptotherapy, psycho-education via Internet and care as usual as assigned intention to treat and as treated. Baseline levels of W-DEQ, 4DSQ and social support did not statistically differ between the groups.
Table 1. Baseline Characteristics and Measurements.
Effect of haptotherapy
Intention to treat analysis
Repeated measures ANOVA showed a significant interaction effect of fear of childbirth for T1 and T2 in the three groups, F(2,99) = 3.321, p = .040, implying that the average change between T1 and T2 differs among groups. Post-hoc comparisons revealed a larger decrease of fear of childbirth for the haptotherapy group than for the other two groups: haptotherapy versus psycho-education via Internet (mean difference in change −8.75: p = .250) and haptotherapy versus care as usual (mean difference in change −11.09, p = .049).
A repeated measures ANOVA without the crossovers also showed a significant change of fear of childbirth from T1 to T2 in the three groups, F(2,74) = 9.255, p < .001 and post-hoc comparisons demonstrated a larger decrease of fear of childbirth for those who were assigned to the haptotherapy condition than for the other two groups; haptotherapy versus psycho-education via Internet (mean difference in change −17.07: p = .016) and haptotherapy versus care as usual (mean difference in change −20.0, p = .001).
displays the profiles of fear of childbirth scores across T1–T4 for the three groups. In all three groups, from pre to postpartum, the fear of childbirth further decreased to T3 and did not change from T3 to T4.
Figure 2. Means of fear of childbirth (W-DEQ score) across four measurement occasions. T1: 20–24 weeks of gestation, T2: 36 weeks of gestation, T3: 6 weeks postpartum, and T4: 6 months postpartum. (a) Intention to treat analysis (ITT). 1: Haptotherapy (HT), 2: Psycho-education via the Internet (INT), 3: Care as usual (CAU), 4: Cut off score 85. (b) As treated analysis (AT). A: Haptotherapy including Cross-overs (HT + CRO), B: Combined no-HT groups (INT + CAU), C: Cut off score 85.
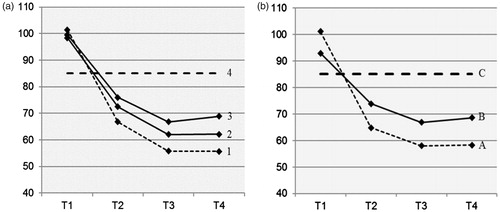
The mean fear of childbirth score of the haptotherapy group shows a (non-significant) trend to remain the lowest in comparison to psycho-education via Internet and care as usual [F(6,164) = 1.616, p = .146; see also .
As-treated analysis
shows the profiles of fear of childbirth across T1–T4 in an As treated analysis of women who actually obtained haptotherapy and those who obtained either psycho-education via Internet or care as usual. At T2, average fear of childbirth was lower in the haptotherapy group than in the combined no-haptotherapy groups (psycho-education via Internet and care as usual). Repeated measures ANOVA showed an interaction effect across all four measurement occasions, F(3,83) = 6.717, p < .001 and on fear of childbirth for T1 and T2, F(1,100) = 27.092, p < .001 (haptotherapy group mean W-DEQ score −35.49, no-haptotherapy −15.89, haptotherapy versus no-haptotherapy mean difference in change score −19.6, p = <.01). Cohens d: haptotherapy = 2.4 and no-haptotherapy = 0.8, meaning haptotherapy more effectively reduced fear of childbirth than no-haptotherapy ().
According to As treated analysis, the percentages of women with a reliable and clinically significant change of fear of childbirth between T1 and T2 (i.e., a decrease of the W-DEQ score ≥ 16 + a W-DEQ score < 85 at T2), in the haptotherapy group (haptotherapy + crossovers) versus the no-haptotherapy groups together (psycho-education via Internet + care as usual) were 75% and 51% respectively (Z = 2.36, p < .01).
Secondary data analyses
Regression analysis revealed no significant differences in the adjusted means of the TES-scores at T3 between the intention to treat groups when controlling for fear of childbirth and social support at T1, F(2,88) = 2.945, p = .058. Intention to treat uniquely accounted for 5.9% of the total variance. However, post-hoc comparisons of the adjusted means suggested a significant difference between haptotherapy and care as usual, t(88) = −2.257, p = .026. We may notice that in the case of three groups, no Bonferroni correction is needed to maintain the experiment-wise alpha at the 5% level [Citation51]. We should also notice that caution should be exercised with interpretation of the post-hoc test because the assumption of homogeneity did not hold. As the smallest within-group variance was for the largest group, the p values tend to be little too low (i.e., the test is too liberal). But given that the p values of .026 is considerably smaller than the nominal level of .05, the conclusion that the effect exist seems robust even though the test is liberal. Regarding the as treated analysis, shows the results of the regression analysis for the secondary outcomes (4DSQ). The dependent variables are the changes between T1 and T2 (i.e., T2–T1), with negative change scores reflecting improvement. The intervention had a significant effect on changes in 4DSQ-scores, controlled for fear of childbirth and social support at T1. The haptotherapy group showed a larger improvement on average than the no-haptotherapy groups. The haptotherapeutic intervention uniquely accounted for 4.9–9.8% of the variance in change scores. Social support also was significantly associated with change in depression (), meaning that more social support results in fewer depression symptoms. No statistically significant correlation was found between social support and change in fear of childbirth for the haptotherapy group (r = 0.024, n = 67, p = .844); nor for the no-haptotherapy group (r = 0.244, n = 35, p = .200).
Table 2. Results of multiple regressions using AT analyzes with FOC and social support at T1 and the intervention as predictors, and the 4DSQ-scale T1–T2 change scores as dependent variables.
Applying the cutoff values of the 4DSQ [Citation52], in the haptotherapy group (n=67) the percentages of women with high distress and depression 4DSQ-scores decreased, between T1 and T2, from 22.4% to 3.0% (p = .001) and from 16.4% to 6.0% (p = .039), respectively. In contrast, in the combined no-haptotherapy groups (psycho-education via Internet + care as usual) (n = 35), the percentages of pregnant women with severe distress symptoms (14.3%) and depression symptoms (5.7%) did not change significantly.
No significant differences between intervention groups were observed concerning somatization, medical interventions, duration of pregnancy or birthweight.
Discussion
The aim of this study was to evaluate the effect of haptotherapy on fear of childbirth by comparing haptotherapy with psycho-education via Internet and care as usual as control conditions in a randomized controlled study. In comparison to psycho-education via Internet and care as usual, haptotherapy had a stronger positive effect on the mental wellbeing of the mother. During pregnancy, prenatal distress symptoms and prenatal depressive symptoms were lower in the haptotherapy group, and postpartum participants in the haptotherapy group also had less fear of childbirth and fewer PTSD symptoms. Fewer PTSD symptoms postpartum suggest that women in the haptotherapy group experienced childbirth as less traumatic than the women in the no-haptotherapy groups, perhaps because they were better able to mentally handle birth. In contrast, no differences were observed concerning somatization, medical interventions, duration of pregnancy, birthweight and gestational age. This indicates that haptotherapy had no negative side effects on birthweight or gestational age.
A considerable number of participants switched from a no-haptotherapy treatment to the treatment condition haptotherapy. According to Marcus and Gibson [Citation53], such switching can cause intention to treat results to poorly indicate the efficacy of the treatment. Therefore, we carried out an additional as treated analysis, which revealed a more pronounced decrease of fear of childbirth in the haptotherapy group as compared with the psycho-education via Internet- and care as usual groups. This analysis also revealed a substantially higher percentage of women showing a clinically significant change in the haptotherapy group than in the two no-haptotherapy groups combined.
This is the first study to examine haptotherapy as treatment for severe fear of childbirth, which precludes a comparison with previous studies. Comparisons with other studies are also problematic because of the use of different W-DEQ cutoff scores to define fear of childbirth and differences in population groups [Citation25]. For example, Rouhe et al. [Citation28,Citation29] used a W-DEQ score ≥ 100, whereas Toolhill et al. [Citation30] used a W-DEQ score ≥ 66. Only Nieminen et al. [Citation32] also used a W-DEQ score ≥ 85, as was recommended by the developers of the W-DEQ [Citation54]. International consensus about the cutoff score to define severe fear of childbirth would make it much easier to compare outcomes of RCT’s.
In the present study, the percentage of pregnant women with a W-DEQ score >85 was 24.2%. A recent systematic review [Citation55] has shown the worldwide prevalence in developed countries is 14%. However, there might be populations with significantly higher prevalences of fear of childbirth, and Dutch women may be one of those populations. An alternative obvious explanation may be that this study in particular attracted the attention of high fear women.
According to Ugarriza et al. [Citation56] and Chojenta et al. [Citation57], a lack of social support is associated with postpartum depression, which is consistent with our findings that more social support results in fewer antepartum and postpartum depression symptoms. However, in the haptotherapy group and the no-haptotherapy group as well, we found no association between social support and fear of childbirth. One may argue, that the haptotherapeutic sessions, comprising of eight episodes together with the partner, may well lead to experience of additional attention and feelings of support by both the therapist and the woman’s partner. This experience might add to feelings of being socially supported and may be of influence in the results. However, although perceived social support decreases feelings of depression, it did not show to reduce fear of childbirth.
Proposed mechanism
HT has been designed to gradually shape the mind-set and teach the pregnant woman to become more confident about her ability to deliver the baby vaginally. It is plausible that increasing the woman’s self-reliance and self-confidence results in reduction of fear of childbirth [Citation35].
Limitations
Based on power analysis, we had fewer participants than planned due to difficulty with recruitment and amended the protocol to improve this. We also had a considerable number of crossovers: 11 participants in the ‘psycho-education via Internet’ group and 14 participants in the ‘care as usual’ group chose to switch to haptotherapy, which impacted our planned analysis. Nevertheless, we were able to demonstrate statistically and clinically significant differences in favor of haptotherapy. One of the reasons for the many crossovers might have been that the participants knew about the possibility of haptotherapy and actively opted for it.
The participating midwifery practices did not adequately represent practices in general but were more motivated than others to improve the care for women with severe fear of childbirth. Therefore, their care as usual might have been more supportive than in the average midwifery practices, which have less experience in dealing with women with severe fear of childbirth. Consequently, they likely also attract more pregnant women with special needs, as was reflected in the high percentage of women with severe fear of childbirth.
Strengths
The crossovers were not planned by protocol, but were also followed in our study. Whereas the crossovers in some way must be regarded as a major weakness of the study, this particular characteristic simultaneously renders the study less artificial and gives it a high ecological validity. Apparently, both the psycho-education via Internet group and the care as usual group comprised many pregnant women with strong views about the treatment they wanted. Currently, in clinical practice, empowerment is a hot issue and patients increasingly make their own choices and select the specific treatment they feel most comfortable with, rather than passively accepting whatever treatment the health provider proposes. Furthermore, we respected the women’s choice for specific antenatal guidance, which also contributed to the high ecological validity.
Recommendations for future research
One of the reasons why it might have been difficult to recruit enough women might be that the W-DEQ comprises of 33 items, which is rather lengthy. In order to compare the outcomes to previous studies – for future research on interventions which aim to decrease fear of childbirth – we recommend that everyone uses the same questionnaire, such as the W-DEQ. For clinical use however, there is need for a shortened questionnaire. In this respect, the two-item Fear of Birth Scale (FOBS) has been tested against the W-DEQ as a ‘gold standard’ and seems to be promising for clinical use [Citation58]. Therefore, in future research, it is recommended to use both questionnaires: W-DEQ for comparison with other studies and FOBS for validation in clinical settings. Furthermore, further research is needed to explore the proposed working mechanism of haptotherapy in reducing fear of childbirth.
Conclusion
We demonstrated positive effects of haptotherapy on fear of childbirth, both in comparison to care as usual and psycho-education via Internet. Haptotherapy additionally improved several aspects of the wellbeing of the mother, such as prenatal distress and depressive symptoms, as well as postpartum fear of childbirth and PTSD symptoms. No differential effects were observed in somatization, medical interventions or duration of pregnancy. Haptotherapy seems a promising intervention for pregnant women suffering from fear of childbirth.
Ethics approval
This trial has been approved by the Dutch Medical Ethics Review Committee and is registered under ABR number: NL34900.008.11. Clinical trial registration: Dutch Trial Register, NTR3339.
Acknowledgements
The authors wish to thank DJ Pot for his support as confidential physician, as well as all the involved obstetricians, practice assistants and gynecologists who recruited pregnant women. We acknowledge K. Nieminen and K. Wijma for accessibility and the translation into Dutch of their text ‘Information om graviditet och förlossning för föderskor’ from their CBT program for childbirth anxiety [Citation39]. We also thank all the participating healthcare haptotherapists for their treatment of pregnant women with severe fear of childbirth, and, last but not least, all the participating pregnant women and their partners.
Disclosure statement
The authors declare that they have no competing interests.
Funding
This research received a grant from the Dutch Association of Haptotherapists (Dutch: Vereniging van Haptotherapeuten [Citation59] and the Dutch Working Group on Psychosomatic Obstetrics and Gynaecology (Dutch: Werkgroep Psychosomatische Obstetrie en Gynaecologie) [Citation60]. The funders have neither participated in the investigation, nor in the writing of the paper.
References
- Zar M, Wijma K, Wijma B. Pre- and postpartum fear of childbirth in nulliparous and parous women. Scand J Behav Ther. 2001;30:75–84.
- Kjærgaard H, Wijma K, Dykes A-K, et al. Fear of childbirth in obstetrically low-risk nulliparous in Sweden and Denmark. J Reprod Infant Psychol. 2008;26:340–350.
- Spice K, Jones SL, Hadjistavroulos HD, et al. Prenatal fear of childbirth and anxiety sensitivity. J Psychosom Obstet Gynaecol. 2009;30:168–174.
- Nieminen K, Stephansson O, Ryding EA. Women’s fear of childbirth and preference for caesarean section – a cross-sectional study at various stages of pregnancy in Sweden. Acta Obstet Gynecol Scand. 2009;88:807–813.
- Adams SS, Eberhard-Gran M, Eskild A. Fear of childbirth and duration of labour: a study of 2206 women with intended vaginal delivery. Br J Obstet Gynaecol. 2012;119:1239–1246.
- Nordeng H, Hansen C, Garthus-Niegel S, et al. Fear of childbirth, mental health, and medication use during pregnancy. Arch Womens Ment Health. 2012;15:203–209.
- Storksen HT, Eberhard-Gran M, Garthus-Niegel S, et al. Fear of childbirth; the relation to anxiety and depression. Acta Obstet Gynecol Scand. 2012;91:237–242.
- Zar M, Wijma K, Wijma B. Relation between anxiety disorders and fear of childbirth during late pregnancy. Clin Psychol Psychother. 2002;9:122–130.
- Wijma K, Wijma B. A woman afraid to deliver – how to manage childbirth anxiety, Chapter 1. In: Paarlberg KM, van de Wiel, H.B.M., editor. Biopsychosocial obstetrics and gynaecology. Switzerland: Springer International Publishing; 2017.
- Melender HL. Experiences of fears associated with pregnancy and childbirth: a study of 329 pregnant women. Birth. 2002;29:101–111.
- Saisto T, Salmela-Aro K, Halmesmäk IE. Psychosocial characteristics of women and their partners fearing vaginal childbirth. Br J Obstet Gynaecol 2001;108:492–498.
- Saisto T, Halmesmäk IE. Fear of childbirth: a neglected dilemma. Acta Obstet Gynecol Scand. 2003;82:201–304.
- Sjögren B. Reasons for anxiety about childbirth in 100 pregnant women. J Psychosom Obstet Gynaecol. 1997;18:266–272.
- Ruble DN, Brooks-Gunn J, Fleming AS, et al. Transition to motherhood and the self: measurement, stability, and change. J Pers Soc Psychol. 1990;58:450–463.
- Hofberg K, Brockington I. Tokophobia: an unreasoning dread of childbirth. A series of 26 cases. Br J Psychiatry. 2000;176:83–85.
- Sjögren B, Thomassen P. Obstetric outcome in 100 women with severe anxiety over childbirth. Acta Obstet Gynecol Scand. 1997;76:948–952.
- Hedegaard M, Brink Henriksen T, Sabroe S, et al. Psychological distress in pregnancy and preterm delivery. Br Med J 1993;307:234–239.
- Dole N, Savitz DA, Hertz-Picciotto I, et al. Maternal stress and preterm birth. Am J Epidemiol. 2002;157:14–24.
- Kurki T, Hiilesmaa V, Raitasalo R, et al. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet Gynecol. 1995;95:487–490.
- Ryding EL, Wijma B, Wijma K, et al. Fear of childbirth during pregnancy may increase the risk of emergency caesarean section. Acta Obstet Gynecol Scand. 1998;77:542–547.
- Alehagen S, Wijma K, Lundberg U, et al. Fear, pain and stress hormones during childbirth. J Psychosom Obstet Gynaecol. 2005;26:153–165.
- Andersson L, Sundstrom-Poromaa I, Wulff M, et al. Implications of antenatal depression and anxiety for obstetric outcome. Obstet Gynecol. 2004;104:467–476.
- De Bruijn TCE. Tied to mommy’s womb? Prenatal maternal stress, postnatal parental interaction style and child development. Unpublished PhD thesis. Faculty of Social and Behavorial Science, University of Tilburg, Tilburg, The Netherlands; 2010.
- Söderquist J, Wijma B, Thorbert G, et al. Risk factors in pregnancy for post-traumatic stress and depression after childbirth. BJOG. 2009;116:672–680.
- Klabbers GA, Van Bakel HJA, Van den Heuvel MA, et al. Severe fear of childbirth: its features, assessment, prevalence, determinants, consequences and possible treatments. Psychol Top. 2016;25:107–127.
- Saisto T, Salmela-Aro K, Nurmi JE, et al. A randomized controlled trial of intervention in fear of childbirth. Obstet Gynecol. 2001;98:820–826.
- Salmela-Aro K, Read S, Rouhe H, et al. Promoting positive motherhood among nulliparous pregnant women with an intense fear of childbirth: RCT intervention. J Health Psychol. 2012;17:520–534.
- Rouhe H, Salmela-Aro K, Tolvanen R, et al. Obstetric outcome after intervention for severe fear of childbirth in nulliparous women – randomised trial. BJOG Int J Obst Gynaecol. 2012;120:75–84.
- Rouhe H, Salmela-Aro K, Tolvanen R, et al. Group psychoeducation with relaxation for severe fear of childbirth improves maternal adjustment and childbirth experience – a randomised controlled trial. J Pschosom Obstet Gynecol. 2015;36:1–9.
- Toohill J, Fenwick J, Gamble J, et al. A randomized controlled trial of a psycho-education intervention by midwives in reducing childbirth fear in pregnant women. Birth. 2014;41:384–394.
- Fenwick J, Toohill J, Gamble J, et al. Effects of a midwife psycho-education intervention to reduce childbirth fear on women’s birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth. 2015;15:284.
- Nieminen K, Andersson G, Wijma B, et al. Treatment of nulliparous women with severe fear of childbirth via the Internet: a feasibility study. J Psychosom Obstet Gynaecol. 2016;37:37–43.
- Ryding EL, Persson A, Onell C, et al. An Evaluation of midwives’ counseling of pregnant women in fear of childbirth. Acta Obstet Gynecol Scand. 2003;82:10–17.
- Verbeek T, Bockting CLH, Meijer JL, et al. Psychological treatment of antenatal depression and anxiety: effects on obstetric outcomes. Eur Psychiatry. 2015;30:993.
- Klabbers GA, Wijma K, Paarlberg KM, et al. Treatment of severe fear of childbirth with haptotherapy, a multicentre randomized controlled trial. BMC Complement Altern Med. 2014;14:385.
- Zar M, Wijma K, Wijma B. Evaluation of the Wijma Delivery Expectancy/Experience (W-DEQ) as a diagnostic test for disabling fear of childbirth. In: Zar M, editor. Diagnostic aspects of fear of childbirth. Volume Fifth Article, edn. Linköping: Linköping University; 2001.
- Random Integer Generator; 2012. Available from: http://www.random.org/integers
- Guideline Haptotherapy in case of Fear of Childbirth. Dutch: Richtlijn Haptotherapie bij Bevallingsangst; 2017. Available from: http://bevallingsangst.nl/Richtlijn%20Haptotherapie%20bij%20Bevallingsangst.pdf
- Nieminen K, Wijma K. Information om graviditet och förlossning för förstföderskor; en kurs i åtta moduler. Linköping, Sweden: Intern rapport Unit of Medical Psychology, Linköping University; 2011.
- Royal Dutch Organization of Midwives; 2017. Available from: www.knov.nl
- Dutch Organization of Obstetrics and Gynaecology; 2017. Available from: www.nvog.nl
- Prenatale verloskundige begeleiding; 2017. Available from: http://www.knov.nl/fms/file/knov.nl/knov_downloads/791/file/KNOV-Standaard%20Prenatale%20verloskundige%20begeleiding.pdf?download_category=overig
- Basis prenatale zorg; 2017. Available from: https://richtlijnendatabase.nl/richtlijn/basis_prenatale_zorg/basis_prenatale_zorg_-_startpagina.html
- Terluin B, Van Marwijk HWJ, Adèr HJ, et al. The Four-Dimensional Symptom Questionnaire (4DSQ): a validation study of a multidimensional self-report questionnaire to assess distress, depression, anxiety and somatization. BMC Psychiatry. 2006;6:1–20.
- American-Psychiatric-Association: Diagnostic and statistical manual of mental disorders (DSM-IV). Washington, DC: American Psychiatric Association; 1994.
- Sarason IG, Sarason BR, Shearln EN, et al. A brief measure of social support: practical and theoretical implications. J Soc Pers Relationsh. 1987;4:497–510.
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–19.
- Faul F, Erdfelder E, Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral and medical sciences. Behav Res Methods. 2006;39:175–191.
- Cohen J. Statistical power for the behavioral sciences. 2nd ed. New York, NY: Taylor & Francis Group; 1988.
- Armijo-Olivo S, Warren S, Magee D. Intention to treat analysis, compliance, drop-outs and how to deal with missing data in clinical research: a review. Phys Ther Rev. 2009;14:36–49.
- Maxwell SE, Delaney HD. Designing experiments and analyzing data: a model comparison perspective, 2nd ed. New York: NY: Psychology Press; 2004.
- Tebbe B, Terluin B, Koelewijn JM. Assessing psychological health in midwifery practice: a validation study of the Four-Dimensional Symptom Questionnaire (4DSQ), a Dutch primary care instrument. Midwifery 2014;29:608–615.
- Marcus SM, Gibbons RD. Estimating the efficacy of receiving treatment in randomized clinical trials with noncompliance. Health Serv Outcomes Res Methodol. 2001:2:247–258.
- Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. 1998;19:84–97.
- O’Connell MA, Leahy-Warren P, Khashan AS, et al. Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynaecol Scand. 2017;96:907–920.
- Ugarriza D, Brown S, Chang-Martinez C. Anglo-American mothers and the prevention of postpartum depression. Issues Ment Health Nurs. 2007;28:781–798.
- Chojenta C, Loxton D, Lucke J. How do previous mental health, social support, and stressful life events contribute to postnatal depression in a representative sample of Australian women? J Midwifery Women’s Health. 2012;57:145–150.
- Haines HM, Pallant JF, Fenwick J, et al. Identifying women who are afraid of giving birth: a comparison of the fear of birth scale with the W-DEQ-A in a large Australian cohort. Sex Reprod Healthc. 2015;6:204–210.
- Association of Haptotherapists. Dutch: Vereniging van Haptotherapeuten; 2017. Available from: http://www.haptotherapeuten-vvh.nl
- Working Group on Psychosomatic Obstetrics and Gynaecology. Dutch: Werkgroep Psychosomatische Obstetrie en Gynaecologie; 2017. Available from: http://wpog.nl