Abstract
Objective
The aim of this study was to explore the “Birth Attitude Profile Scale (BAPS)” in a selected sample of women with fear of birth. Another aim was to develop profiles of women according to their birth attitudes and levels of childbirth fear in relation to background characteristics.
Methods
A secondary analysis of data collected in two different samples of women with fear of birth. Data were collected by a questionnaire in gestational week 36 and background data from mid-pregnancy. A principal component analysis and a cluster analysis were performed of the combined sample of 195 women.
Results
The principal component analysis revealed four domains of the BAPS: “personal impact, birth as a natural event, freedom of choice and safety concerns”. When adding the fear of birth scale, two clusters were identified: one with strong attitudes and lower fear, labeled “self-determiners”; and one with no strong attitudes but high levels of fear, labeled “fearful.” Women in the “Fearful” cluster more often reported previous and current mental health problems, which were the main difference between the clusters.
Conclusion
The BAPS instrument seems to be useful in identifying birth attitudes in women with fear of birth and could be a basis for discussions and birth planning during pregnancy. Mental health problems were the main difference in cluster membership; therefore, it is important to ask women with fear of childbirth about physical, mental and social aspects of health. In addition, a qualitative approach using techniques such as focus groups or interviews is needed to explore how women come to form their attitudes and beliefs about birth.
Introduction
Women’s attitudes to childbirth might influence their perceptions of pregnancy and birth, which is an important factor to consider when promoting women-centered care. One of the foundations in women-centered care is to investigate whether women adhere to a belief that birth is a natural or a medical event [Citation1], as this could influence the level of intervention during birth. Women’s willingness to accept an intervention, when asked in the antenatal period, increases the odds of receiving an intervention [Citation2].
Women with fear of birth are more exposed to birth interventions [Citation3]. Fear of birth affects 14% of pregnant women worldwide [Citation4]. Various attempts to treat fear of birth have been investigated, such as counseling with midwives [Citation5], group psycho education [Citation6], telephone support [Citation7], cognitive behavioral therapy [Citation8,Citation9], continuous Labor support [Citation10] and continuity with a known midwife [Citation11].
Cesarean sections are more frequent in women with fear of birth [Citation12,Citation13], and women who delivered by cesarean section more often report negative birth experiences [Citation3,Citation14], including when they preferred and subsequently received a cesarean section [Citation15]. Long-term follow ups have shown that negative birth experiences are still present after one year [Citation14,Citation16]. In addition, a poorer perception of quality of care has been reported in women with childbirth fear [Citation17].
In a population-based study of women’s attitudes to birth, using the “Birth Attitude Profile Scale (BAPS)”, Haines et al. [Citation18] identified four subscales in the instrument. Women from Sweden and Australia were compared, and Swedish women were more likely to score higher on the subscales “personal impact and birth as a natural event” compared to women from Australia [Citation18]. Following this study of birth attitudes, Haines et al. [Citation18] added level of fear to the four subscales [Citation19] using the “Fear of Birth Scale (FOBS)” [Citation20,Citation21] and identified three profiles of women following a cluster analysis [Citation19]. The three profiles were labeled “self-determiners, take it as it comes and Fearful”. The “self-determiners” group was characterized by seeing birth as a natural event. These women were not afraid of giving birth, but they were concerned about the personal impacts of birth. Women in this cluster were less likely to have a high level of education. They preferred and were more likely to have a vaginal birth. Women belonging to the cluster labeled “take it as it comes” were also not afraid of birth. They had no strong views about pregnancy or mode of birth, but they were more likely to have an elective cesarean section [Citation19].
The last cluster labeled “fearful” consisted of women with high fear and concerns about personal impacts and safety, and they did not see birth as a natural event. While these fearful women did not favor women’s choices in general, they were more likely to prefer an elective cesarean section. They reported a more negative self-rated mental health during pregnancy, and they had more often been treated with counseling due to fear of birth. Elective cesarean sections were more common in this group, and if they went into Labor, they were more likely to use an epidural and report more intense pain. Finally, they reported a more negative birth experience compared to women in the other clusters [Citation19].
In a randomized controlled trial of women with fear of birth, randomized to internet-based cognitive therapy or counseling with midwives, five clusters of the sample were identified using a variety of psychological variables (pain catastrophizing scale (PCS), injection and phobia scale, hospital anxiety and depression scale (HADS), the Edinburgh postnatal depression scale (EPDS) and post traumatic symptom scale (PTSD)) [Citation9]. Ten percent had severe symptoms of psychological morbidity, 13% presented with blood and injection phobia, 19% reported symptoms of depression and anxiety, 31% scored low on most variables and 28% had relatively high scores of anxiety and depressive symptoms, post-traumatic stress and pain catastrophizing. These findings suggest that women with fear of birth comprise a heterogeneous group.
Problem area
Fear of birth is quite common, but there is no evidence for the best treatment. Previous studies have shown that women with fear of birth are not homogeneous concerning psychological characteristics, but there is still a lack of knowledge regarding their attitudes. The aim of this study was, therefore, to test the BAPS in a selected sample of women with fear of birth. Another aim was to develop profiles of women according to their attitudes regarding birth and their levels of childbirth fear in relation to background characteristics.
Material and methods
Design
This is a secondary analysis of a combined sample of women with fear of birth who completed a similar questionnaire in gestational week 36 and background data from mid pregnancy.
Setting
The studies were conducted in Sweden at one university hospital and three referral hospitals. All women were enrolled in antenatal care in their community, following the national program [Citation22]. Women are usually cared for by the same midwife during approximately nine antenatal visits, and during an uncomplicated pregnancy, there are no visits to a physician. All hospitals in Sweden offer counseling for fear of birth [Citation5]. In some antenatal clinics, women are offered a screening procedure for fear of birth, and in other clinics, women self-report to the midwife and are subsequently referred to counseling teams when needed.
Sample
The combined sample consisted of (A) 118/258 women participating in a randomized controlled trial comparing internet-based cognitive therapy and counseling with midwives (standard care), and who responded to the BAPS and (B) 77 women participating in an experimental study who were offered counseling with midwives; in addition, when possible, the counseling midwife provided intrapartum care.
Recruitment of participants
For sample A, the recruitment was done stepwise. First, all women who came for a routine ultrasound examination during gestational weeks 17–19 who mastered the Swedish language filled out a screening questionnaire including FOBS [Citation19,Citation20]. Those who scored 60 or above on FOBS were contacted by telephone by a research midwife and asked if they were willing to participate in the study. If they consented to participate, login details to the internet portal were sent out. All questionnaires were completed in the internet portal. After completing background data, women were randomized either to internet-based cognitive therapy or counseling with midwives. Details of the process are presented elsewhere [Citation23]. For sample B, women were referred to the counseling team by the antenatal midwife, after screening with FOBS or self-reported fear of birth. They received oral and written information about the study, and if they consented to participate, they filled out the first of three questionnaires, with background data in mid pregnancy [Citation11].
Data collection
Data were collected by a questionnaire distributed in gestational week 36 and combined with the background data collected in mid pregnancy. Women in sample A completed the questionnaire online and women in sample B in print. Background data included age, parity, marital status, level of education, country of birth, birth preference, negative experience of healthcare and history of mental health problems. Women’s emotional wellbeing was assessed using the HADS [Citation24] and the EDPS [Citation25]. Fear of birth was assessed twice, in mid pregnancy and in gestational week 36, using FOBS [Citation19,Citation20].
In the questionnaire completed in gestational week 36, the BAPS was used [Citation18]. It contains 12 personal and four general attitudes toward birth and the items were preceded by a prompt “I would like a birth that…” These attitudinal items (included in the BAPS) were subjected to an audit in the UK in 2001 about cesarean sections [Citation1]. All statements were assessed on a six-point scale ranging from “strongly agree” to “have not thought about it”.
Analysis
Following the procedure reported by Haines et al. [Citation18] in a population-based study, the analysis started with a principal component analysis to explore the underlying dimensions of the 16 items. The factorability of the data was confirmed with a Kaiser-Meyer-Olkin value that exceeded the recommended value of 0.6 [Citation26] and Bartlett’s test of sphericity [Citation27].
The number of factors to retain was guided by Kaiser’s criterion [Citation26] of eigenvalues over 1, inspection of the screen plot [Citation28] and by a parallel analysis [Citation29]. Only factors exceeding 0.40 were retained. Total scores were then calculated for each retained subscale, with high scores indicated strong agreement. The internal consistency was measured using Cronbach alpha coefficients [Citation30].
In the next step, a cluster analysis was conducted on responses to the BAPS and the level of fear, as determined by the FOBS in mid pregnancy [Citation19,Citation20]. Thereafter, a Kappa-mean cluster analysis was applied to z-score transformed responses to each of the four BAPS subscales and the FOBS scores [Citation31]. Background characteristics of the clusters were then compared. The software Statistical Package of Social science (SPSS, version 23, Chicago, IL) was used in the analysis.
The study was approved by the Research Ethics Committee at the Regional Ethical Review Board in Uppsala, Sweden (no. 2013/209 and 2016/058).
Results
In total, 195 women with fear of birth were included in the study (118 from the randomized controlled trial and 77 from the experimental study). Their background characteristics are presented in . The majority were aged 25–35 years, living with a partner and of Swedish origin. Just of half of the sample presented with a high level of education, and similar proportions of primiparas and multiparas participated. In all, 63% reported previous negative experiences of healthcare, and just over half had a history of mental health problems. More than half of the participants scored higher than eight on HADS-anxiety and 15% on HADS-depression. In addition, 27% scored 13 or more on EPDS. When asked about birth preference, Citation36% preferred a cesarean section. The mean level of FOBS was 72.68 (18.31) in mid pregnancy and 56.05 (24.51) in late pregnancy and there was no statistically significant difference between samples A and B.
Table 1. Study sample.
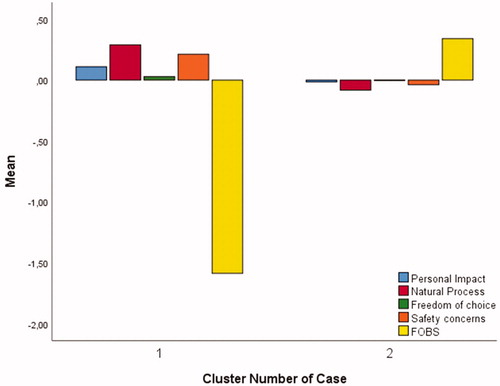
Principal component analysis with oblimin rotation was conducted on the 12 personal and four general attitudes to birth. The factorability of the data was confirmed with a Kaiser-Meyer-Oklin value of 0.65 and a highly significant Bartlett’s test of sphericity (p = 0.001). One of the attitudes, “doctors should decide if a woman should have a caesarean section under any circumstances”, loaded inconsistently in the model. Therefore, the structure was explored with this item removed. Using Catell’s screen test, four components were retained for further investigation. This was supported by the results from the parallel analysis, which showed four components with eigenvalues exceeding the corresponding criterion values for a randomly generated data matrix of the same size. Total scores were calculated for each component by adding together the item scores loading above 0.4 on each component. The internal consistency of each subscale was assessed using Cronbach’s Alpha. The components were given descriptive subscale labels following the results from Haines et al. [Citation17]: “personal impact of birth” (mean score = 28.12, standard deviation (SD) = 4.7, Cronbach’s α = 0.77), “birth as natural event” (mean score= 11.4, SD = 2.61, Cronbach’s α = 0.66), “freedom of choice” (mean score = 5.4, SD = 1.9, Cronbach’s α = 0.59) and “safety concerns” (mean score = 13.9, SD = 1.2, Cronbach’s α = 0.63). shows the results from the principal component analysis, with the factor loading for each dimension of the BAPS. shows the two clusters that were identified based on the women’s level of agreement on the BAPS subscales and their level of fear on the FOBS. From the z-transformed scores it was seen that Cluster 1 was characterized by women with lower fear and stronger agreements on the attitudes relating to the personal impact of birth, safety concerns, the natural process of birth and freedom of choice. Cluster 2 showed a group that scored low on all domains of the BAPS scale but scored high on the FOBS. Majority of participants belonged to Cluster 2.
Table 2. Pattern and structure matrix of four factor Principal Component Analysis solution with oblimin rotation of birth attitudes.
shows background factors in relation to cluster membership. There was no difference in the women’s socio-demographic background, previous experiences with healthcare or birth preference. Women in Cluster 2 differed from women in Cluster 1 by being more likely to have a history of mental health problems. They were also more likely to present with depressive symptoms (EPDS) and anxiety.
Table 3. Cluster membership in relation to background characteristics.
Discussion
The main findings of this study are that the BAPS instrument seems to be useful for women identified with fear of birth, as similar subscales were identified as in the original study [Citation18]. When adding FOBS, two clusters appeared that showed different characteristics of cluster membership with a strong impact of fear and mental health problems.
The PCA showed the same loadings as the previous population-based study by Haines et al. [Citation18], with one exception. In the present study, women valued a birth that allowed the best start for breastfeeding and was included in the subscale “birth as a natural event”. This item loaded inconsistently in the population-based study [Citation18]. Similarly, to that study, the item “doctors should always decide about cesarean sections” was omitted in the present study. The similarities in factor loading suggest that BAPS could be useful, not only for women in general but also for women with fear of birth. The subscales may also prove useful in a clinical setting as a tool to start a discussion and better understand women’s attitudes and what concerns they might have regarding birth particularly. This information can be used to tailor appropriate interventions with individual women to pinpoint their concerns.
Discussing attitudes in such a way is fairly similar to that of group counseling for fear of birth provided in an Australian hospital [Citation7]. In such group sessions, women brought up certain areas for discussion regarding issues they were afraid of or worried about, and these areas were discussed with peers and professionals in the group. Such reflective discussions showed a significant reduction in levels of fear of birth.
Another way to deal with women’s fear has been shown in a Norwegian study, when counseling midwives adopted an attitude to empower and encouraging women to face their fears and cope with Labor instead of an attitude supporting women’s autonomy in their choice to have a cesarean section. When challenging the women’s attitudes, changes in birth preferences also occurred [Citation32].
The cluster analysis in the present study generated two distinct clusters. These clusters are fairly similar to those identified by Haines et al. [Citation19] The exception was their “take it as it comes” profile was not identified in the present study. It is possible that the inclusion of Australian women in the Haines study accounted for some of this explanation, where the national cesarean section rates are almost doubled, compared to Sweden. In that study, the distribution of cluster participation showed that 35% of Australian women belonged to the “take it as it comes” profile. The corresponding figures for the Swedish sample was 25%. On the other hand, Swedish women were more likely to align with the “self-determiner” cluster (42 vs. 32%) [Citation19]. Another explanation could be that women with fear of birth often report valid reasons behind their fears and attitudes, especially if they prefer a birth by cesarean section. As such, they do not “take it as it comes” [Citation3].
The variables that differed between the two clusters were all related to mental health problems, in that the women either had a history of mental illness, ongoing depressive symptoms or anxiety. Co-morbidity is common in women with fear of birth [Citation33] and women might need treatment for their mental problems, as mental health problems could affect the health of both mother and baby [Citation34], as well as prenatal attachment [Citation35], for a long period after birth [Citation34,Citation36].
Cluster 1 was smaller with quite strong attitudes and lower levels of fear, while Cluster 2 showed no strong attitudes but high fear. Fear seems to override the attitudes. It is very interesting that although all women in the study were identified with fear of birth in early pregnancy, it seems that, for some women, the fear was reduced from recruitment to mid pregnancy and for the majority further reduced by the time point when they completed the BAPS instrument, e.g. in gestational week 36. Previous population-based studies [Citation21,Citation37] and randomized controlled trials [Citation23] have shown that the level of fear decreases at the end of pregnancy for most women, regardless of treatment for fear of birth. Persistent fear in late pregnancy might be attributed to circumstances such as mental health problems, as shown in the present study. It is, therefore, important to follow up the women’s levels of fear as well as their mental health [Citation34,Citation36].
When assessing the BAPS, women in the present study usually had some form of treatment for their fear of birth, a fact that most likely would have affected the level of fear. The counseling service is usually available in the third trimester and provides women with access to tools for managing the fear [Citation38]. Women who were randomized to treatment with internet-based cognitive therapy had weekly assignments to complete from gestational week 25 but were less likely to fulfill the program [Citation23]. We did not, however, find any association between allocation to treatment and cluster membership.
Methodological considerations
The study had several limitations. A strength of this study is its prospective design, which allowed women to express their attitudes during pregnancy, rather than retrospectively after giving birth. The multicenter approach with women from four hospitals, both referral and university hospitals, strengthened the generalizability of the findings.
One limitation is the exclusion of non-Swedish speaking women, as it has been shown that women with foreign backgrounds are more likely to have a strong fear of birth [Citation39,Citation40] and worse mental health [Citation34]. Adding data from two different samples could, of course, impact on the findings. In total, women were recruited from four different hospitals. One hospital recruited women in both studies but on different time spans. Majority of participants in the present study were, therefore, exposed to counseling with midwives. We could not, however, control for the way the counseling was performed. It is known from precious research that the counselor’s way of providing care for women with fear of birth could differ and change the outcome [Citation32]. One strength of the study is the use of a similar questionnaire, which facilitates the merging of the samples available.
Conclusion
The BAPS instrument seems to be useful to identify birth attitudes in women with fear of birth and could be a basis for discussions during pregnancy. Mental health problems were the main difference in cluster membership; thus, it is important to ask women with fear of childbirth about physical, mental and social aspects of health.
In addition, a qualitative approach using techniques such as focus groups or interviews is needed to explore how women come to form their attitudes and beliefs about birth.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Thomas J, Paranjothy S. The National Sentinal Caesarean Section Audit Report. Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit. London: RCOG Press;2001.
- Green JM, Baston HA. Have women become more willing to accept obstetric interventions and does this relate to mode of birth? Data from a prospective study. Birth. 2007;1:6–13.
- Dencker A, Nilsson C, Begley C, et al. Causes and outcomes in studies of fear of childbirth: a systematic review. Women Birth. 2019;32:99–111.
- O’Connell M, Leahy-Warren P, Khashan A, et al. Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2017;96:907–920.
- Larsson B, Karlström A, Rubertsson C, et al. Counseling for childbirth fear- a national survey. Sex Reprod Healthc. 2016;8:82–87.
- Rouhe H, Salmela-Aro K, Toivanen E, et al. Group psychoeducation with relaxation for severe fear of childbirth improves maternal adjustment and childbirth experience- a randomized controlled trial. J Psychosom Obstet Gynecol. 2015;36:1–9.
- Toohill J, Fenwick J, Gamble J, et al. Effects of a midwife psycho-education intervention to reduce childbirth fear on women’s birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth. 2015;30:8.
- Nieminen K, Andersson G, Wijma B, et al. Treatment of nulliparous women with severe fear of childbirth via the internet: a feasibility study. J Psychosom Obstet Gynaecol. 2016;37:37–43.
- Rondung E, Ekdahl J, Rubertsson C, et al. Heterogenity in childbirth fear or anxiety. Scand J Psychol. 2018;59:634–643.
- Sydsjö G, Blomberg M, Palmquist S, et al. Effects of continuous midwifery labour support for women with severe fear of childbirth. BMC Pregnancy Childbirth. 2015;15:115.
- Hildingsson I, Rubertsson C, Karlström A, et al. A known midwife can make a difference for women with fear of childbirth-birth outcome and women’s experience of intrapartum care. Sex Reprod Healthc. 2019;21:33–38.
- Henriksen L, Borgen A, Rislökken J, et al. Fear of birth: prevalence, counselling and method of birth at five obstetrical units in Norway. Women Birth. 2020;33:97–104.
- Waldenström U, Hildingsson I, Ryding E-L. Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG. 2006;113:638–646
- Nilsson C, Lundgren I, Karlström A, et al. Self reported fear of childbirth and its association with birth experience and mode of delivery: a longitudinal population based study. Women Birth. 2012;25:114–121.
- Karlström A, Nystedt A, Hildingsson I. A comparative study of the experience of childbirth between women who preferred and had a caesarean section and women who preferred and had a vaginal birth. Sex Repr Healthc. 2011;2:93–99.
- Hildingsson I, Rubertsson C. Childbirth experience in women randomized to internet based cognitive therapy or midwife counseling. J Psychosom Obstet Gynecol. 2019;1:1–10.
- Haines H, Hildingsson I, Pallant J, et al. The role of women’s attitudinal profiles in satisfaction with the quality of their antenatal and intrapartum care. JOGNN. 2013;42:428–444.
- Haines H, Rubertsson C, Pallant J, et al. Women’s attitudes and beliefs of childbirth and association with birth preference: a comparison of a Swedish and an Australian and Swedish sample in mid-pregnancy. Midwifery. 2012;28:e850–e856.
- Haines H, Rubertsson C, Pallant J, et al. The influence of women’s fear, attitudes and beliefs of childbirth on mode and experience of birth. BMC Pregnancy Childbirth. 2012;12:55.
- Haines H, Pallant J, Karlström A, et al. Cross cultural comparison of levels of child-birth related fear in an Australian and Swedish sample. Midwifery. 2011;27:560–567.
- Hildingsson I, Haines H, Karlström A, et al. Presence and process of fear of birth during pregnancy - findings from a longitudinal cohort study. Women Birth. 2017;30:242–247.
- The Swedish Association of Obstetricians and Gynecologists and the Swedish Association of Midwives. Antenatal care, sexual and reproductive health. Report no 59, updated 2016. Available from: https://www.sfog.se/natupplaga/ARG76web43658b6c2-849e-47ab-99fa-52e8ac993b7d.pdf
- Rondung E, Ternström E, Hildingsson I, et al. Comparing internet-based cognitive behavioral therapy with standard care for women with fear of birth: randomized controlled trial. JMIR Ment Health. 2018;5:e10420.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression- development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–786.
- Kaiser H. An index of factorial simplicity. Psychometrika. 1974;39:31–36.
- Bartlett MS. A note on the multiplying factors for various chi square approximations. J Royal Stat Soc. 1954;16:296–298.
- Cattell RB. The screen test for number of factors. Multivariate Behavioral Res. 1966;1:245–276.
- Horn J. Rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–185.
- Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334.
- Pallant J. SPSS survival manual. 5th ed. Sydney: Allwn & Unwin; 2013.
- Nerum H, Halvorsen L. Does counsellor’s attitude influence change in a request for a caesarean in women with fear of birth? Midwifery. 2010;26:45–52.
- Rubertsson C, Hellstrom J, Cross M, et al. Anxiety in early pregnancy: prevalence and contributing factors. Arch Womens Ment Health. 2014;17:221–228.
- Kingston D, Kehler H, Austin M-P, et al. Trajectories of maternal depressive symptoms during pregnancy and the first 12 months postpartum and child externalizing and internalizing behavior at three years. PLOS One. 2018;13:e0195365.
- Rubertsson C, Pallant J, Sydsjö G, et al. Maternal depressive symptoms have a negative impact on prenatal attachment- findings from a Swedish community sample. J Reprod Infant Psychol. 2015;33:153–164.
- Pietikänen J, Kiviruusu O, Kylliäinen A, et al. Maternal and paternal depressive symptoms and children’s emotional problems at the age of 2 and 5 years: a longitudinal study. J Child Psychol Psychiat. 2020;61:195–204.
- Hildingsson I, Karlström A, Rubertsson C, et al. Women with fear of childbirth might benefit from having a known midwife during labour. Women Birth. 2019;32:58–63.
- Larsson B, Hildingsson I, Rubertsson C, et al. Women’s experience of midwife-led counselling and its influence on childbirth fear: a qualitative study. Women Birth. 2019;32:e88–e94.
- Ternström E, Hildingsson I, Haines H, et al. Higher prevalence of childbirth related fear in foreign born pregnant women- findings from a community sample in Sweden. Midwifery. 2015;31:445–450.
- Taloyan M, Sundquist J, Al-Windi A. The impact of ethnicity and self-reported health on psychological well-being: a comparative study of Kurdish-born and Swedish-born people. Nord J Psychiatr. 2008;62:392–398.