Abstract
Purpose
This study examined experiences during the cessation of fertility treatment due to the COVID-19 pandemic, including levels of mental health, coping strategies used to manage uncertainty about treatment due to the pandemic, sources of support, and predictors of mental health.
Methods
One hundred and seventy-five participants in the UK completed an online survey.
Results
Half of the participants experienced clinical levels of anxiety and/or depression, and 20% reported suicidal feelings as a result of the uncertainty about treatment due to the pandemic. Support from friends, family and online forums were reported by more than half of participants, but support from fertility clinics or counsellors were reported by less than one quarter. The strategy used most frequently to cope with the uncertainty about treatment due to the pandemic was self-distraction, and this predicted reduced depression. However, self-blame, behavioral disengagement and venting predicted increased depression and self-blame, behavioral disengagement, and denial predicted increased anxiety.
Conclusions
Fertility clinic communication and psychological support, such as counselling, which had substantially reduced during treatment cessation, could include some focus on personal coping, including what to avoid. Psychological support is likely to be more important now than ever. Despite resumption of treatment, the impacts of the period of cessation and of COVID-19 are likely to continue to reverberate.
Introduction
As a result of the COVID-19 pandemic, fertility clinics across the world closed. In the UK, treatment ceased in April 2020, affecting the estimated 55,000 patients in the UK already receiving treatment [Citation1] and those due to start treatment, which may have impacted their chances of becoming a parent. For example, Smith et al. [Citation2] and Bhattacharya et al. [Citation3] found that delays to starting treatment reduced chances of conception leading to a live birth, especially in older women. The already fragile mental health of women and men undergoing fertility treatment [Citation4] was also compounded by the cessation of treatment [Citation5–11]. For example, Lawson et al. [Citation9] reported rates of clinical levels of anxiety and depression of 73% and 78%, respectively, although Barra et al. [Citation7] reported respective rates of only 11% and 13% following cessation of treatment. Barra et al. [Citation7] and Tokgoz et al. [Citation6] found factors such as age and decreased ovarian reserve predicted poorer mental health.
In the UK, Boivin et al. [Citation12] found that experiences of clinic closures included feelings that the attainability of parenthood was threatened, especially for those who felt this was their last chance. There was uncertainty about the impact on fertility and chances of treatment success, and ability to access treatment, especially funded treatment in the future. These feelings heightened levels of distress that were already experienced as a result of fertility issues, although only a few participants reported deep feelings of depression or suicidal ideation.
A key issue is how those impacted by the cessation of treatment managed the uncertainty and distress. For example, what coping strategies did they use and how did this impact their mental health? Lawson et al. [Citation9] reported that coping through seeking emotional and informational support, and self-blame and avoidance predicted greater distress due to treatment cancelation. Gordon and Balsom [Citation8] found that using avoidance to cope with fertility issues predicted worse mental health and optimism predicted better mental health as a result of treatment cessation. However, these studies identified few coping strategies linked to better mental health and they did not ask specifically about coping with the cessation of treatment. In the UK, Boivin et al. [Citation12] found that strategies used included thought-management, getting mentally and physically ready for when treatment resumes, seeking social support, and information gathering to keep up-to-date. Similarly, Tippett [Citation13] found increased use of online forums/groups during the pandemic but support from counsellors and clinics was least often reported.
However, research using a validated coping measure to explore coping with the uncertainties due to treatment cessation is lacking, as is research examining relationships between coping and clinical measures of mental health, especially in the UK. Research looking at the full range of coping strategies is needed to identify what may be helpful, as well as detrimental, to mental health. Therefore, the present study examined levels of mental health (anxiety and depression) and whether strategies used to cope with uncertainty about treatment due to the pandemic predicted mental health, all assessed using validated measures during the first national lockdown in the UK. The study also reports: (1) emotional distress responses related to uncertainty about treatment due to the pandemic, (2) coping strategies used to manage this uncertainty, (3) sources of support utilized and (4) treatment-related worries as a result of the pandemic.
Materials and methods
Following University Psychology Research Ethics Committee approval, the link to an online survey was posted on the website of Fertility Network UK and data were collected in June 2020. One hundred and seventy-five women who had been impacted by the cessation of treatment provided consent to participate and fully completed the anonymous survey. A response rate cannot be calculated as it is not possible to know how many people saw the survey link.
The survey covered sociodemographic (age, gender, relationship status and ethnicity) and COVID-19 related information, including whether they or a close friend/family member had been diagnosed with COVID-19, and their current employment status (not working pre-COVID-19, working outside the home, remote working, furloughed and lost job). It covered treatment information such as how long they had been trying to conceive, whether it was NHS or private, whether it was in the UK or abroad, number of previous treatment cycles, and at what stage treatment was cancelled (waiting for treatment to begin, start date cancelled and cancelled mid-cycle).
The survey assessed mental health in the past few weeks using the Generalized Anxiety Disorder Scale (GAD-7) [Citation14] and the Patient Health Questionnaire (PHQ-9) [Citation15]. Responses on both scales range from 0 (not at all) to 3 (nearly every day) and items on each scale are summed with higher scores indicating greater severity (GAD-7 α = 0.92, PHQ-9 α = 0.87). GAD-7 scores range from 0 to 21 and a score of 10 or above is considered to show clinical levels of anxiety. PHQ-9 scores range from 0 to 27 and a score of 10 or above is considered to show clinical levels of depression. Participants were also asked whether they had received support or not in relation to fertility and treatment pre-pandemic and if they had received support or not during the pandemic from their GP, fertility specialist, other clinic staff, support group, fertility organization, online forums, counsellor, friends and family.
Next, participants were asked to what extent they had experienced 18 emotional distress responses as a result of the uncertainty about treatment due to the pandemic, such as suicidal feelings, depression, frustration and anger [Citation4]. Response options range from 1 (“not at all”) to 5 (“all of the time”). Items were summed so scores range from 18 to 90 with higher scores indicating more distress. They were also asked how they had coped with this uncertainty using the brief Coping Orientations to Problems Experienced (brief-COPE) [Citation16]. This comprises 28 items assessing 14 different coping strategies, such as denial, planning, acceptance and emotional support, with responses ranging from 1 (“I haven’t been doing this at all”) to 4 (“I have been doing this a lot”). Scores on each of the 14 coping subscales range from 2 to 8 with higher scores indicating greater use of a coping strategy. Reliability of the subscales ranged from α = 0.60 to α = 0.97. Finally, participants were asked about treatment-related worries as a result of the pandemic such as time running out, lack of fertility support and communication and catching COVID-19 delaying progress.
Statistical analyses
Using SPSS (SPSS Inc., Chicago, IL), descriptive statistics were generated for all variables. ANOVA was used to examine group differences where one variable was categorical and the other continuous. Pearson’s correlations were used to determine the relationship between two continuous variables. Finally, multiple linear regression analyses were used to examine the predictors of mental health. Statistical significance was set at p < 0.05..
Results
Participant and treatment characteristics
The participants were women with an average age of 34 (SD = 3.90), 92% described themselves as white, 93% were in a heterosexual relationship (5% were in a lesbian relationship and 2% were single). Eighty-seven percent had not had COVID-19 and 72% had not known a close friend or family member with COVID-19. Since the start of the pandemic, 32% were working outside home, 48% were working at home, 10% were furloughed, 5% had lost their income or their job and 5% were not employed before.
Participants had on average been trying to conceive for three years (SD= 1.78). When treatment was ceased due to the pandemic, 20% were waiting for treatment to begin, 44% had a start date that was canceled and 36% were mid-cycle. Sixty-nine percent were due to have/having NHS funded treatment, 94% planned to have/were having treatment in the UK and for all participants this was IVF.
Mental health
The mean level of depression was 8.93 (SD= 5.47); 22% experienced moderate depression, 12% moderately severe and 5% severe. The mean level of anxiety was 8.74 (SD= 5.58); 22% experienced moderate anxiety and 18% severe. This means that 39% of participants experienced depression and 41% experienced anxiety at levels (i.e. a score of 10+) where psychological or pharmacological treatment should be considered. A total of 50% of the sample experienced anxiety and/or depression at this level.
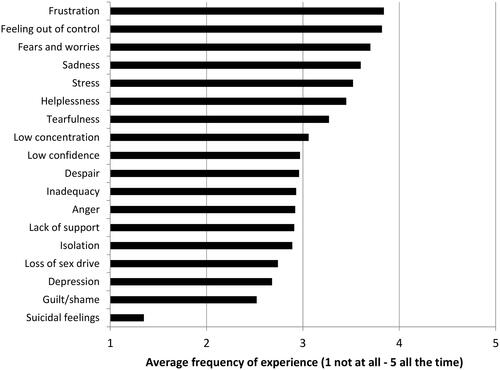
Emotional impacts
shows the frequency with which various emotional impacts were experienced as a result of uncertainty about treatment due to the pandemic. The emotions experienced the most were frustration, feeling out of control, fears and worries, and sadness, whereas suicidal feelings were experienced the least but 20% still experienced suicidal feelings at least “occasionally”.
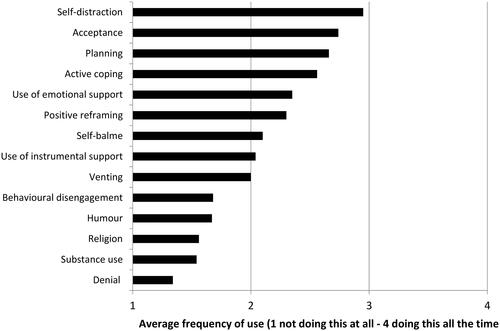
Coping utilized
shows on average the frequency with which various strategies were used to cope with uncertainty about treatment due to the pandemic. The strategies used the most were self-distraction, acceptance and planning.
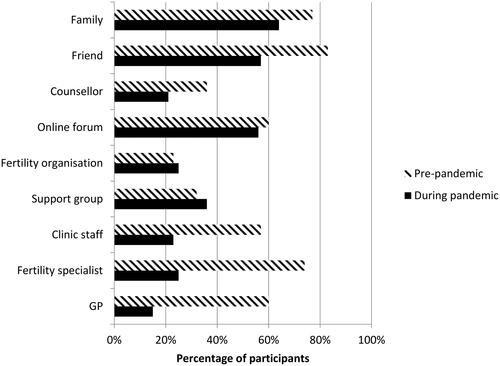
Support utilized
shows the levels of fertility-related support received from various sources pre-pandemic and during the pandemic. Support from the GP (15%), fertility specialist (24%) and clinic staff (23%) were most reduced during the pandemic. Support from a counsellor (21%) was also reduced but this was one of the least used forms of support pre-pandemic. Support from fertility organizations (36%), support groups (25%) and online forums (56%) remained relatively unchanged.
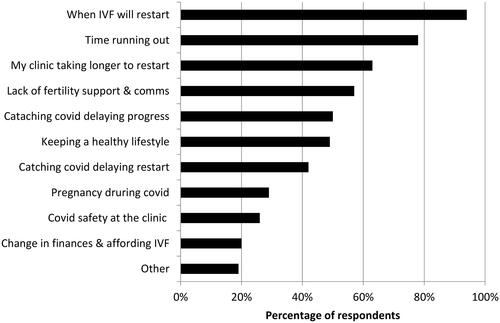
Worries
shows that for nearly all participants, the biggest treatment-related worry due to the pandemic was when treatment would resume, followed by feeling that time was running out. ‘Other’ worries not listed here include longer waiting times when treatment resumes (due to e.g. others being prioritized), the NHS no longer funding their treatment, and other aspects of life changing during the cessation of treatment that will make it more difficult to resume treatment.
Associations between coping and mental health
ANOVAs showed there were no significant differences in levels of anxiety or depression between participants who were waiting to start treatment, those for whom the start date was cancelled and those for whom treatment was cancelled. However, shows some significant correlations. Depression and anxiety were positively correlated with coping using denial, substance use, behavioral disengagement and self-blame, so these strategies were not good for mental health. Depression and anxiety were negatively correlated with coping using acceptance, and depression was negatively correlated with active coping and positive reframing, so these strategies were good for mental health. Depression and anxiety were not correlated with age, years spent trying to conceive or number of previous cycles of treatment.
Table 1. Variables significantly correlated with depression or anxiety.
As correlation analysis showed a number of relationships between coping and mental health, multiple linear regression analysis including the 14 coping subscales was conducted. This showed that coping using behavioral disengagement (β = 0.27, p < 0.001), venting (β = 0.20, p < 0.05) and self-blame (β = 0.40, p < 0.001) predicted increased depression, whereas coping using self-distraction (β = −0.18, p < 0.01) predicted reduced depression. Fifty-one percent of the variance was explained (F = 10.62, p < 0.001). Another regression analysis showed that coping using behavioral disengagement (β = 0.29, p < 0.001), denial (β = 0.21, p < 0.01) and self-blame (β = 0.32, p < 0.001) predicted increased anxiety. Forty-seven percent of the variance was explained (F = 9.07, p < 0.001).
Discussion
This study found that half of the participants had clinical levels of anxiety and/or depression. It is possible to compare this to research in other countries that used the same measures (PHQ-9 and GAD-7). For example, this is less than the 73% and 78% (anxiety and depression) reported in the USA [Citation9], but more than the 11% and 13% reported in Italy [Citation7]. However, levels of poor mental health were higher than in the population of people experiencing fertility issues pre-pandemic [Citation17] and higher than in the general population both pre-pandemic and during the pandemic [Citation18]. Furthermore, shows that suicidal feelings as a result of uncertainty about treatment due to the pandemic were reported by 20% of participants. This is less than the 42% who reported these feelings as a result of fertility issues pre-pandemic [Citation4], but is still substantial.
Unlike previous research [Citation6,Citation7], factors such as number of treatment cycles were not associated with mental health. Some research has suggested that personal resources are more important than demographic and fertility-related factors [Citation10]. Coping strategies may be considered personal resources. This study found that using self-blame, behavioral disengagement, venting and denial to cope with uncertainty about treatment due to the pandemic predicted worse mental health. Gordon and Balsom [Citation8] and Lawson et al. [Citation9] also found that avoidant coping was related to worse mental health. In the present study using self-distraction, which is also considered avoidant coping, predicted better mental health, and shows that this was the strategy participants reported using most frequently. Problem-focused, rather than avoidant coping, is often considered the most adaptive form of coping [Citation19], although this works best when the source of stress is controllable, which the pandemic and treatment cessation were not. shows that two problem-focused strategies (planning and active coping) were among the most commonly used. One could argue that using such strategies, even though they were not linked to better mental health, would be healthier than using ones that may do harm such as behavioral disengagement and self-blame. Therefore, promoting problem-focused coping, in addition to self-distraction, could be helpful. Boivin et al. [Citation12] found that getting physically ready for the resumption of treatment and information gathering were often used.
Reports of fertility-related support () showed that support from the GP, fertility specialist and clinic staff had all substantially reduced and were received by less than one quarter of participants. While Boivin et al. [Citation12] and Tippett [Citation13] note some reports of clinic initiatives during the pandemic, experiencing a lack of communication and support was more common. Twenty-one percent reporting support from a counsellor in the present study is still more than the 5% reported by Tippett [Citation13]. However, this is less than the pre-pandemic 45% reported by Payne et al. [Citation4]. Thus while prioritization of health service resources due to the pandemic is, of course, understandable, clinics should offer more psychological support, especially as there is evidence that psychological intervention is associated with higher pregnancy rates [Citation20]. Such support could include some focus on coping strategies that may help, such as self-distraction, and those to avoid, such as self-blame, and future research could examine the impact of this support on mental health. A whole clinic approach may be advisable whereby all staff are able to detect and address patients’ behavioral, emotional and cognitive needs and refer them for counselling where appropriate [Citation21]. This could be part of the patient support policy that clinics are required by the HFEA to have in place. The HFEA also requires that patients are offered counselling. However, this only needs to be “offered” and only for certain types of treatment, which may belie the significant mental health impacts of fertility challenges and the importance of psychological support, so HFEA policy could be reconsidered.
While shows that the most common worries about fertility treatment and the pandemic were when it would restart and time running out, worries about the future of fertility treatment were also common, such as the impact of catching COVID-19. Other concerns included longer waiting lists, other patients being prioritized and no longer being able to access funding, supporting [Citation12] and [Citation22]. This suggests that, despite resumption of treatment, the impacts of the treatment cessation reported in this study are likely to continue to reverberate for a long time, and future research should continue to monitor this.
While other research has examined mental health during the cessation of treatment, and some has included coping, to our knowledge, this is the only study to specifically examine coping with the cessation of treatment using validated measures of both coping and mental health, and to look at this in the UK, where research has primarily been more qualitative in nature. These are strengths of the study. There are also some limitations. The sample is lacking in diversity in terms of ethnicity and sexual orientation, and no men responded, thus limiting the generalizability of the findings. Future fertility research should consider methods to reach a more diverse range of participants so all experiences are captured. The small, self-selected sample also means findings should be interpreted with caution. For example, it is possible that those who chose to respond had worse mental health or were more in need of support. Finally, it is not known if people had preexisting mental health issues prior to the cessation of treatment or prior to experiencing fertility issues, and as this was a cross-sectional survey, we cannot unpick the causal direction of relationships.
In conclusion, levels of poor mental health during the cessation of treatment in the UK are a cause for concern. As a result of delays on the chances of conception leading to a live birth, on top of the likelihood of on-going delays now that treatment has resumed, the impacts explored in this study are likely to continue to reverberate. Fertility clinic communication and psychological support, such as counselling, which was lacking during treatment cessation, could include some focus on personal coping, including what to avoid. Psychological support is likely to be more important now than ever.
Disclosure statement
The authors report no conflict of interest.
References
- Human Fertilisation and Embryology Authority. Fertility treatment: trends and figures 2014–2016. London: Human Fertilisation and Embryology Authority; 2018.
- Smith ADAC, Gromski PS, Al Rashid K, et al. Population implications of cessation of IVF during the COVID-19 pandemic. Reprod Biomed Online. 2020;41(3):428–430.
- Bhattacharya S, Maheshwari A, Ratna MB, et al. Prioritizing IVF treatment in the post-COVID 19 era: a predictive modelling study based on UK National Data. Hum Reprod. 2021;36(3):666–675.
- Payne N, Seenan S, van den Akker O. Experiences of involuntary childlessness and treatment in the UK: what has changed in 20 years? Hum Fertil. 2021;24(5):333–340.
- Seifer DB, Petok WD, Agrawal A, et al. Psychological experience and coping strategies of patients in the northeast US delaying care for infertility during the COVID-19 pandemic. Reprod Biol Endocrinol. 2021;19(1):28.
- Tokgoz VY, Kaya Y, Tekin AB. The level of anxiety in infertile women whose ART cycles are postponed due to the COVID-19 outbreak. J Psychosom Obstet Gynaecol. 2020;1–8.
- Barra F, La Rosa VL, Vitale SG, et al. Psychological status of infertile patients who had in vitro fertilization treatment interrupted or postponed due to COVID-19 pandemic: a cross-sectional study. J Psychosom Obstet Gynaecol. 2020;1–8.
- Gordon JL, Balsom AA. The psychological impact of fertility treatment suspensions during the COVID-19 pandemic. PLOS One. 2020;15(9):e0239253.
- Lawson AK, McQueen DB, Swanson AC, et al. Psychological distress and postponed fertility care during the COVID-19 pandemic. J Assist Reprod Genet. 2021;38(2):333–341.
- Ben-Kimhy R, Youngster M, Medina-Artom TR, et al. Fertility patients under COVID-19: attitudes, perceptions, and psychological reactions. Hum Reprod. 2020;35(12):2774–2783.
- Kirubarajan A, Patel P, Tsang J, et al. The psychological impact of the COVID-19 pandemic on fertility care: a qualitative systematic review. Hum Fertil. 2021;1–8.
- Boivin J, Harrison C, Mathur R, et al. Patient experiences of fertility clinic closure during the COVID-19 pandemic: appraisals, coping. Hum Reprod. 2020;35(11):2556–2566.
- Tippett A. Life on pause: an analysis of UK fertility patients’ coping mechanisms after the cancellation of fertility treatment due to COVID-19. J Health Psychol. 2022;27(7):1583–1600.
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
- Carver C. You want to measure coping but your protocolʼs too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100.
- Kiani Z, Simbar M, Hajian S, et al. The prevalence of anxiety symptoms in infertile women: a systematic review and meta-analysis. Fertil Res Pract. 2021;7(1):6.
- Jia R, Ayling K, Chalder T, et al. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open. 2020;10(9):e040620.
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21(3):219–239.
- Frederiksen Y, Farver-Vestergaard I, Skovard NG, et al. Efficacy of psychosocial interventions for psychological and pregnancy outcomes in infertile women and men: a systematic review and meta-analysis. Br Med J Open. 2015;5:e006592.
- Gameiro S, Boivin J, Dancet E, et al. ESHRE guideline: routine psychosocial care in infertility and medically assisted reproduction – a guide for fertility staff. Hum Reprod. 2015;30(11):2476–2485.
- Karavadra B, Stockl A, Balen AH, et al. COVID-19 and fertility services in the United Kingdom: a biphasic qualitative study. Reprod Fertil. 2021;2(1):27–34.