Abstract
Pulmonary aspiration is a potentially lethal perioperative complication related to gastric size and contents. Several perioperative factors are believed to increase gastric size, while others are less studied. This prospective observational study aimed to investigate the effect of preoperative anxiety and hormone-induced ovarian stimulation on gastric size examined by gastric ultrasound. We recruited 49 female patients undergoing hormone-induced ovarian stimulation and oocyte retrieval for in vitro fertilization at Rabin Medical Centre, Petah Tikva, Israel. Preoperatively, women ranked their anxiety level using a verbal numeric anxiety score (VNS). In addition, we recorded the extent of ovarian stimulation and measured the antral cross-sectional area (CSA) using gastric ultrasound. There was no substantial correlation between preoperative VNS anxiety and antral CSA (p = .697). Moreover, the number of follicles, blood estradiol, and progesterone levels did not correlate with antral CSA (p = .590, p = .104, and p = .511, respectively). In conclusion, neither preoperative anxiety nor extensive ovarian stimulation affects gastric size in fasting healthy patients. However, further studies are warranted in this area to define these findings better. Trial registration: Clinicaltrials.gov, identifier: NCT04833530
Introduction
Background
Pulmonary aspiration is one of the most serious risks of general anesthesia and has been reported in as many as one in 4000 cases [Citation1]. Predisposing factors include enlarged gastric antrum size and contents, increased regurgitating tendency, and laryngeal incompetence [Citation2]. Therefore, preoperative fasting guidelines were introduced to minimize the risk of aspiration [Citation3,Citation4]. However, it has been found that aspiration can occur even in fasted patients.
Due to the disastrous consequences of pulmonary aspiration, much research has focused on identifying which patients are at risk for enlarged gastric antrum size.
Anxiety may increase gastric size because it predisposes to nausea and vomiting [Citation5]. In addition, several studies have shown that gastric emptying in healthy females can be affected by fluctuations in ovarian sex hormones, with decreased gastric emptying reported with high estrogen levels [Citation6].
Gastric ultrasound is an emerging point of care tool that provides bedside information [Citation7]. It is increasing in popularity and has been included in recent subspecialty guidelines [Citation8–11]. Gastric antrum size is evaluated by measuring the gastric antral cross-sectional area (CSA).
In vitro fertilization (IVF) is a standard method in infertility treatment that often requires general anesthesia for oocyte retrieval. In addition, these procedures are associated with iatrogenic-induced hormonal changes. Therefore, women who underwent IVF may experience increased emotional distress, including stress and anxiety [Citation12].
Study objectives
We designed this study to assess various factors influencing gastric antrum size in women undergoing oocyte retrieval. The primary outcome was the effect of preoperative anxiety on the antral CSA. The secondary outcome was the effect of ovarian stimulation on the antral CSA.
We hypothesized that increased preoperative anxiety level and extended ovarian stimulation would increase gastric antrum size.
Materials and methods
Ethics
Ethical approval for this study (RMC 21-0010) was provided by the Institutional Review Board of Rabin Medical Center (Chairperson Prof. Ran Tur-Kaspa) on 21 March 2021. The study was registered with the U.S. National Institutes of Health (ClinicalTrials.gov; Identifier: NCT04833530). All included patients gave informed written consent.
Study design
Prospective observational study.
Settings
We consecutively recruited women between 7 April 2021 and 9 August 2021. The study was performed in a tertiary medical center (Rabin Medical Center-Beilinson Hospital, Petah Tikva, Israel).
Participants
Women undergoing general anesthesia for oocyte retrieval, aged ≥18 years, ASA physical status of I or II.
Exclusion criteria were: patient refusal, morbid obesity (body mass index ≥40 kg/m2), diabetes mellitus, depressive and anxiety disorders, regular antidepressant medications, and a history of bariatric surgeries.
Study protocol and variables
Anxiety
Upon enrollment, participants were asked to fill out a verbal numeric anxiety score (VNS) to rank their anxiety level on a scale from 0 to 10 (i.e. 0: no anxiety, 10: highest anxiety). This measurement was validated [Citation13] and used in three previous studies in our institution measuring preoperative anxiety [Citation14–16].
Ovarian stimulation
All participants underwent ovarian stimulation for IVF utilizing a short antagonist protocol. The follicle stimulation hormone dose was set according to individual clinical parameters, and oocyte maturation was triggered using human chorionic gonadotropin (Ovitrelle®, Merck Serono, Weiterstadt, Germany) 250 μg, combined with gonadotropin-releasing hormone agonist (Decapeptyl®, Ferring, Kiel, Germany) 0.2 mg, administered 36–38 h prior to the oocyte retrieval procedure.
Gastric ultrasound
A preoperative gastric ultrasound examination was performed in the operating room using a SonoSite EDGE portable ultrasound machine (SonoSite, Inc., Bothell, WA, fitted with a 5–2 MHz probe). The examination was performed in the supine position in the operating room to measure the antral CSA, as described per standard protocol [Citation17].
An example of a sonogram with the relevant anatomic landmarks and antral CSA measurements is shown in .
Figure 1. Preoperative gastric sonogram. The sonogram shows a sagittal scan of an empty gastric antrum. L: liver; A: gastric antrum; SMA: superior mesenteric artery; Ao: aorta.

In addition, we performed an ultrasound images quality score to rank images quality from 1 to 3 (i.e. 1: poor, 2: average and 3: good image quality), as described in a previous study [Citation18].
Data collection
We collect the following data: demographics (i.e. age, height, weight and BMI); medical history (i.e. comorbidities, concomitant medications, smoking status and history of PONV or motion sickness); perioperative data (i.e. preoperative VNS anxiety, the duration of the procedure, postoperative VAS pain score, nausea and vomiting); gynecological profile and the extent of the ovarian stimulation (i.e. indication for IVF, number of the current cycle, length of ovarian stimulation, number of follicles > 14 mm, number of oocytes retrieved, and the blood levels of estradiol and progesterone prior to triggering of oocyte maturation); and gastric ultrasound parameters (i.e. preoperative antral CSA, and image quality score).
Bias
The investigators who performed the gastric ultrasound examinations were blinded to the VNS anxiety score and the extent of the ovarian stimulation.
Study size
No studies have been performed on the relationship between anxiety and antral CSA. A moderate correlation coefficient of 0.4 was considered of clinical importance to justify the sample size calculation [Citation19].
Therefore, a correlation coefficient of 0.4, with an alpha level of 0.05 and power of 80%, was used to calculate the required sample size using the “pwr” package in R (R Foundation for Statistical Computing, Vienna, Austria), yielding the need of 46 participants. With an expected attrition rate of 30%, a sample of 60 participants was planned for recruitment.
Statistical methods
Before the performance of linear regression models, statistical assumptions (i.e. linearity, independence) were tested. Spearman’s rank correlation coefficients and linear regression models were generated. Nonlinear relationships were assessed visually and using loess-smoothing.
The dependent variable was the antral CSA, while other variables were independent.
All the continuous variables were tested for normality of distribution using histograms and Q-Q plots. Due to nonnormality, variables are presented as median [IQR]. All statistical analyses have been performed in R (R Foundation for Statistical Computing, Vienna, Austria) and IBM SPSS® Statistics version 22 (IBM Corp., Armonk, NY).
Results
We screened 77 patients, and we included 49 participants after the exclusion. The enrollment flow diagram is presented in . In addition, patient characteristics and perioperative data are listed in .
Figure 2. The enrollment flow diagram. GA: general anesthesia; LMA: laryngeal mask airway; US: ultrasound.
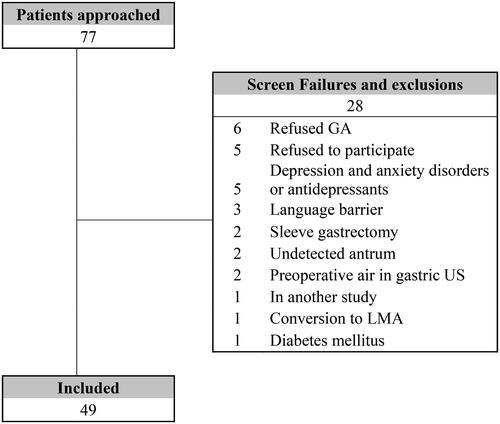
Table 1. Patient characteristics and perioperative data.
Primary outcome
The median VNS anxiety score level was 4 [IQR 1–6]. There was no substantial correlation between preoperative VNS anxiety score level and antral CSA (r = 0.057, p = .697). Moreover, linear regression with preoperative VNS anxiety score level as the independent and antral CSA as the dependent variable also did not result in a good model (p-value of β coefficient .216, and R2 = 0.012). Results of a multivariable linear regression model taking patient related factors into account are presented in . Higher age was significantly associated with a decreased antral CSA.
Table 2. Multivariable linear regression model including patient-related factors.
Secondary outcome
The IVF cycle data are listed in . The number of follicles, pre trigger estradiol (pmol/L) and progesterone (nmol/L) levels did not correlate with antral CSA (r = –0.079, p = .590; r = –0.096, p = .511; and r = –0.235, p = .104, respectively). Moreover, univariable linear regression with the number of follicles, estradiol (pmol/L) and progesterone (nmol/L) levels as independent variables and antral CSA as the dependent variable also showed no association between these variables and preoperative antral CSA (p values of β coefficients all >.1, and R2 all <0.015).
Table 3. IVF cycle data.
In contrast, the number of oocytes retrieved showed a weak correlation with antral CSA (r = –0.316, p = .027). However, a univariable linear regression model with the number of oocytes as an independent variable and antral CSA as the dependent variable did not result in a good linear model (p-value of β coefficient in linear regression .444, and R2 = 0.013). Therefore, there is likely no association between the number of oocytes and preoperative antral CSA.
Discussion
Pulmonary aspiration is a severe complication associated with morbidity and mortality [Citation1], and its risk has been linked to gastric antrum size [Citation2]. Currently, there are a few factors that have been identified as contributing to an increase in gastric antrum size, such as delayed gastric emptying and gastroparesis in diabetes mellitus [Citation20]. While other perioperative variables, such as preoperative anxiety level and the extent of ovarian stimulation, have received less attention in the literature in specific populations.
IVF is a standard procedure in the gynecological arena, in which female patients with a tendency to anxiety, as well as those under hormonally induced ovarian stimulation, undergo a relatively stressful procedure under general anesthesia [Citation12]. Additionally, the stimulated ovaries’ steroid hormones secreted at supraphysiological levels directly affect vascular permeability and gastrointestinal mobility [Citation6].
Preoperative anxiety is related to increased anesthetic requirements, augmented pain during the postoperative period, and an elevated incidence of nausea and vomiting [Citation14,Citation15,Citation21,Citation22]. Nevertheless, no data were found on the association between anxiety and gastric size.
We thought it would affect gastric emptying and consequently increase antral CSA. However, our study results showed no substantial correlation between preoperative anxiety level and antral CSA. In fact, none of the patients experienced postoperative vomiting, but the lack of vomiting may have been due to propofol’s antiemetic effect. This result may suggest that anxiety, although causing nausea, does not affect gastric emptying in a way that standard fasting guidelines cannot overcome.
Concerning the extent of ovarian stimulation, evidence from the literature suggests that fluctuations in ovarian sex hormone levels affect gastric emptying, mainly when estrogen levels are high [Citation6]. However, no data were found regarding the association between the number of follicles aspirated or oocytes retrieved and antral CSA. Surprisingly, neither estradiol and progesterone levels nor the number of follicles aspirated demonstrated a significant correlation with antral CSA. In contrast, the number of oocytes retrieved exhibited a modest correlation with preoperative antral CSA, but this did not result statistically in a satisfactory linear model. Thus, our study results showed no association between stimulated ovaries and preoperative antral CSA following recommended fasting guidelines. Furthermore, considering that the number of aspirated oocytes is associated with the cumulative outcome of the oocyte aspiration [Citation23], the results from this study demonstrate that a more extensive ovarian stimulation aimed to recruit and retrieve a higher number of oocytes is not associated with a higher degree of increased preoperative gastric size.
Strengths and limitations
There are two notable strengths in this study. First, in order to enhance internal validity and quality control, before the study began, the investigators performing gastric ultrasound examinations completed a training program that included dedicated teaching and a portfolio of live scans assessed by one of the investigators with expertise in gastric ultrasound (C.A.), who also reviewed and verified all measurements before beginning statistical analysis. Second, the gastric ultrasound examiners were blinded to the preoperative VNS anxiety score and the level of ovarian stimulation.
We need to consider two limitations. First, the dynamic nature of the organ is an inherent limitation of any research utilizing gastric ultrasound. Despite following a strict ultrasound scanning protocol, the peristaltic contractions may have added an element of variability between successive measurements. Second, the study selected population was homogenous, with no known risk factors for perioperative aspiration, since all the patients were admitted for elective cases while fasting for at least 6 h. A more heterogeneous group with higher risk factors for perioperative aspiration may yield different results.
Conclusions
In conclusion, in fasting healthy patients, neither preoperative anxiety nor extensive ovarian stimulation affects gastric size. However, further studies are warranted in this area to characterize these assertions adequately.
Acknowledgements
The authors thank Mrs. Atara Davis for her technical assistance with this manuscript.
Disclosure statement
The authors declare no conflicts of interest.
Additional information
Funding
References
- Lienhart A, Auroy Y, Péquignot F, et al. Survey of anesthesia-related mortality in France. Anesthesiology. 2006;105(6):1087–1097.
- Engelhardt T, Webster NR. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth. 1999;83(3):453–460.
- Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126:376–393.
- Smith I, Kranke P, Murat I, et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2011;28(8):556–569.
- Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992;77(1):162–184.
- Hutson WR, Roehrkasse RL, Wald A. Influence of gender and menopause on gastric emptying and motility. Gastroenterology. 1989;96(1):11–17.
- Perlas A, Arzola C, Van de Putte P. Point-of-care gastric ultrasound and aspiration risk assessment: a narrative review. Can J Anaesth. 2018;65(4):437–448.
- Haskins SC, Bronshteyn Y, Perlas A, et al. American Society of Regional Anesthesia and Pain Medicine expert panel recommendations on point-of-care ultrasound education and training for regional anesthesiologists and pain physicians—part I: clinical indications. Reg Anesth Pain Med. 2021;46(12):1031–1047.
- Haskins SC, Bronshteyn Y, Perlas A, et al. American Society of Regional Anesthesia and Pain Medicine expert panel recommendations on point-of-care ultrasound education and training for regional anesthesiologists and pain physicians—part II: recommendations. Reg Anesth Pain Med. 2021;46(12):1048–1060.
- Meineri M, Arellano R, Bryson G, et al. Canadian recommendations for training and performance in basic perioperative point-of-care ultrasound: recommendations from a Consensus of Canadian Anesthesiology Academic Centres. Can J Anaesth. 2021;68(3):376–386.
- Bronshteyn YS, Anderson TA, Badakhsh O, et al. Diagnostic point-of-care ultrasound: recommendations from an expert panel. J Cardiothorac Vasc Anesth. 2021;36(1):22–29.
- Jain D, Kohli A, Gupta L, et al. Anaesthesia for in vitro fertilisation. Indian J Anaesth. 2009;53(4):408–413.
- Facco E, Stellini E, Bacci C, et al. Validation of Visual Analogue Scale for Anxiety (VAS-A) in preanesthesia evaluation. Minerva Anestesiol. 2013;79(12):1389–1395.
- Orbach-Zinger S, Ginosar Y, Elliston J, et al. Influence of preoperative anxiety on hypotension after spinal anaesthesia in women undergoing caesarean delivery. Br J Anaesth. 2012;109(6):943–949.
- Danon E, Heesen P, Orbach-Zinger S, et al. The effect of preoperative anxiety on phenylephrine dose during cesarean delivery: an open controlled one-arm clinical trial. Acta Anaesthesiol Scand. 2020;64(10):1499–1504.
- Keltz A, Heesen P, Katz D, et al. Intraoperative pain during caesarean delivery: incidence, risk factors and physician perception. Eur J Pain. 2021;26(1):219–226.
- Perlas A, Mitsakakis N, Liu L, et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination. Anesth Analg. 2013;116(2):357–363.
- Zieleskiewicz L, Boghossian MC, Delmas AC, et al. Ultrasonographic measurement of antral area for estimating gastric fluid volume in parturients. Br J Anaesth. 2016;117(2):198–205.
- BMJ. Calculation of the correlation coefficient; 2023. Available from: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-s
- Steinsvik EK, Sangnes DA, Søfteland E, et al. Gastric function in diabetic gastroparesis assessed by ultrasound and scintigraphy. Neurogastroenterol Motil. 2021;34:e14235.
- Van den Bosch JE, Moons KG, Bonsel GJ, et al. Does measurement of preoperative anxiety have added value for predicting postoperative nausea and vomiting? Anesth Analg. 2005;100(5):1525–1532.
- Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg. 1999;89(6):1346–1351.
- Oron G, Ronen M, Hochberg A, et al. Does the outcome of fresh embryo transfer affect the outcome of subsequent thawed embryo transfers from sibling oocytes in patients that utilized all their embryos? Hum Fertil. 2021;25:1–7.
