ABSTRACT
Punctoplasty is a common procedure in the management of punctal stenosis and was first described by Sir William Bowman in 1853. Several types of punctoplasty are described, and include 1-snip, 2-snip, triangular 3-snip, rectangular 3-snip and 4-snip procedures. The understanding of the anatomy and physiology of the punctum has greatly improved in the last decade aided by electron microscopic and molecular techniques. The use of minimally invasive modalities for primary cases is on the rise with successful preservation of the physiological functions of the punctum and canaliculus. The paper reviews the current anatomical and physiological evidence to present an alternative perspective. Given our evolving understanding, it may be time to debate the practice of performing routine punctoplasty.
I. Historical perspectives
Punctal stenosis causing epiphora is a common lacrimal disorder that has been addressed surgically for at least 168 years; punctoplasty was first described by Sir William Bowman in 1853.Citation1,Citation2 Bowman’s description was that of a single snip procedure, involving slitting the canaliculus. This technique was reiterated by Arlit in 1874.Citation2 Hoffman, in 1904 was one of the earliest to suggest a three-snip procedure.Citation3 Graves in 1926 criticized the three-snip procedure and proposed his technique of posterior ampullotomy using Critchett’s grooved probe.Citation4 Graves believed that unlike Bowman’s method, his technique did not alter the capillary action of the canaliculi. Thomas in 1951 refined it to the modern 3-snip procedure, which was suggested to him by his colleague David Hardie.Citation5 The procedure saw further refinement by Viers in 1955.Citation6 However, Jones in 1962 reintroduced the modern 1-snip and heavily criticized the 3-snip procedures as unphysiological.Citation7 For recurrent or refractory cases and canaliculitis, Jones proposed a 2-snip procedure with a small horizontal arm medially without removing part of the punctum or ampulla. The arguments by Jones were counteracted by Viers and Cassady, separately.Citation7 In 1967, Hughes and Maris proposed a punch punctoplasty that involved targeting the ampulla, which was re-popularized by Edelstein and Reiss in 1992 using the ‘Reiss punch.Citation8,Citation9 To enhance the success of the 1-snip, Dolin and Hecht in 1986 proposed a suturing technique to keep the freshened edges of 1-snip procedure separated.Citation10 Offutt and Cowen in 1993 proposed their technique of microsurgical punctoplasty, which involved externalization of the vertical canaliculus.Citation3 The same year, Lam and Tessler proposed adjunctive use of mitomycin C with a 3-snip punctoplasty in a patient who failed a 1-snip procedure earlier.Citation11 The classical triangular 3-snip punctoplasty remained the most popular technique of punctoplasty for decades. In 2009, Chak and Irvine proposed their technique of a rectangular 3-snip punctoplasty as a more physiological procedure.Citation12 Kim et al. in 2012 proposed a 4-snip punctoplasty in cases of severe punctal stenosis. Their approach modified the 3-snip rectangular technique to include a portion of the horizontal canaliculus.Citation13 The debate continues as to which punctoplasty procedure is the best or, indeed, is punctoplasty the best solution for punctal stenosis?
II. Current knowledge of the anatomy and physiology of the punctum: considerations against performing punctoplasty
The punctum is an anatomical structure representing the beginning of the lacrimal drainage system. It lies on a fibrous mound, the ‘lacrimal papilla.’ Although routinely believed to measure 0.2–0.4 mm, there are wide variations in its dimensions, which are influenced by several factors such as age, gender, race, and ethnicity.Citation14,Citation15 Studies assessing the natural evolution of punctal parameters from the 1st to 8th decade in a normal population have shown differences between genders as well as between the upper and lower puncta.Citation16 From childhood to old age, typical changes have been documented in size, punctal papilla, density of peri-punctal fibrous layers, peri-punctal vascularity, and the white punctal zones.Citation16
The lacrimal punctum is surrounded by a dense ring of fibrous tissue that provides support and integrity to the punctum and facilitates its functions. The muscle of Riolan was earlier believed to pass through the tarsal plate along with the dense fibrous tissue to insert into the lateral aspect of the punctum and vertical canaliculus.Citation17 In a detailed cadaveric study in 2011, Kakizaki et alCitation18 demonstrated the lacrimal punctum and the vertical canaliculus to be a part of the tarsal plate. This partly validated Whitnall’sCitation19 earlier work and that of others.Citation20 They further demonstrated that the fibrous tissue and muscle of Riolan surround the punctum and the vertical canaliculus both medially and laterally.Citation21 Ultrastructural mapping of a normal punctum revealed a well-defined elevated junction between the inner punctal surface and the beginning of the vertical canaliculus. The mucosa on either side of the junction was distinct with rugae distal to the junction.Citation22 Each of these areas are believed to be anatomically and functionally distinct.
The pars lacrimalis of musculus orbicularis oculi (lacrimal portion of the orbicularis oculi muscle) or tensor tarsi, was first noted by the French anatomist Jacques-Francois-Marie Duverney in 1745 and later by Rosenmüller in 1805. Although eponymously called the ‘Horner’s muscle’ after its description by William E. Horner in 1822, it has been proposed to be renamed as Horner-Duverney’s muscle.Citation23,Citation24 Recent electron microscopy and 3D histology have demonstrated that at its insertion, the Horner-Duverney’s (HD) muscle continues to encircle the lacrimal punctum and the vertical canaliculus without a separate ‘muscle of Riolan’ ( and ).Citation24 However, the arrangement at the lacrimal punctum constitutes both circular and vertical muscle fibers that partly extend into the peri-punctal area in a scissoring pattern (). This scissoring pattern gets exaggerated around the vertical canaliculus and becomes denser and more parallel as it continues around the horizontal canaliculus.Citation24 The density of the connective tissue regularly alters along the entire course of the muscle. The HD muscle demonstrated a typical equal distribution of type I and type IIb fibers and showed a dense sensory, adrenergic and cholinergic innervation.Citation24
Figure 1. Schematic illustration of the Horner-Duverney’s muscle: Note the criss-cross pattern of the muscle arrangement encircling the punctum and vertical canaliculus.
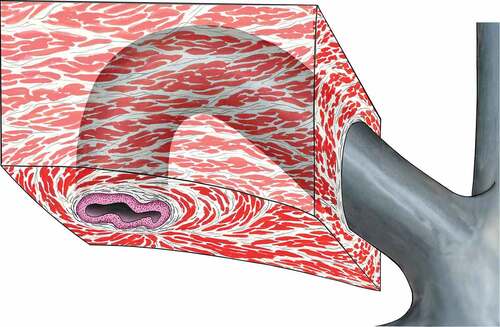
Figure 2. Three-dimensional volume rendered image of the punctum. Note the continuation of Horner-Duverney’s muscle right up to the punctum (yellow arrow) in an extensive criss-cross manner. Also note the dense connective tissue (grey area).

In the context of this current anatomical understanding, punctoplasty is likely to alter the anatomy to potentially impact the physiological functions of the proximal lacrimal drainage pathways. There are six arguments for believing so. Firstly, the tough fibrous ring supports the driving force that creates a negative pressure within the canaliculi and provides the structural buttress needed to maintain the desired punctal position in the lacus lacrimalis. All kinds of incisional punctoplasty procedures violate this fibrous ring to varying degrees. Secondly, as shown recently, the HD muscle continues to insert as high as the punctum, and any irreversible violation of the punctum integrity would logically impact the driving force for propagating tear drainage. Thirdly, there is fundamental evidence now to suggest that the crisscross pattern of the HD muscle at the punctum is responsible for punctal occlusion during eyelid closure. The mechanism is akin to fish-mouth closure (). Punctoplasty would potentially have functional consequences on the loss of punctal occlusion during eyelid closure. Fourth, a 3 or 4-snip punctoplasty would cause irreversible loss of a part of the well-defined puncto-canalicular junction and distinct mucosa on either side of it. Fifth, a 3 or 4-snip punctoplasty may potentially cause varying degrees of neural denervation in a critical area with subsequent functional implications. Neural innervation disturbances as seen in paralytic epiphora, partly support such an argument. Lastly, an incisional punctoplasty may potentially disrupt several natural age-related punctal changes that may be desirable in an aging individual with concurrent dry eye.
III. Current knowledge of pathophysiology and treatment of punctal stenosis: considerations against performing punctoplasty
Punctal stenosis is a common disorder of the proximal lacrimal pathway and constitutes 3–17% of all lacrimal drainage disorders in large epidemiology studies.Citation25,Citation26 Recent ultrastructural studies have shown widespread fibrosis and inflammation, which may be severe in 30% of cases.Citation27 Extensive and irregular laying of collagen cross-bundles with mononuclear inflammatory infiltration of the bundles and inter- and intracellular edema in the vicinity of fibroblast has been demonstrated.Citation27
Punctal stenosis remains the main indication for punctoplasty, the outcomes of which vary in part based upon the precise procedure. Anatomical and functional success varies between 31.2%-96.2% and 18.7–93.3%.Citation11–13,Citation28–34 Assessment of punctoplasty outcomes is complex owing to the lack of a standard definition of punctal stenosis, a large range of punctal size in the normal population, several variations in surgical techniques, different stages of the disease, and poor data on adjunctive modalities. Although significant dysfunctions were reported in short-term, long-term functional epiphora and other defects from performing punctoplasties remain unclear. Reported complications following punctoplasty include fibrosis, restenosis, and stent extrusions. These are more likely in the scenario of eyelid cicatricial changes. Given the presence of inflammation and fibrosis associated with punctal stenosis, it is not unreasonable to expect this to increase in response to an incisional insult following punctoplasty. Whilst several steps may be taken to either reduce or manage these complications, it may be preferable to consider an ounce of prevention over a pound of cure.Citation35
IV. Punctoplasty in canaliculitis
A combination of punctoplasty and canaliculotomy is commonly used in the management of infective canaliculitis. While the clinical outcomes in terms of resolution of infection are excellent compared to those of medical management alone, persistence or recurrence occurs in 33–100%.Citation36,Citation37 However, the functional consequences of punctoplasty and canaliculotomy have not been studied in detail.Citation36–40 The combination of incision of the punctum as well as the canaliculus would potentially have a cumulative detrimental impact upon the physiology of the lacrimal pump and capillary action of the canaliculus beyond that of each individually. Lacrimal pump dysfunction, canalicular fibrosis and fistula formation are documented complications.Citation41–44 This has prompted the increased use of punctum-sparing canaliculotomy techniques such as focal canaliculotomy or non-incisional canalicular curettage with encouraging outcomes.Citation41–44
V. Alternative modalities to incisional punctoplasty
Non-incisional modalities are being increasingly investigated and practiced in the management of punctal stenosis. They include simple mechanical punctal dilatation, perforated punctal plugs, punctal dilatation with mini-monoka or bicanalicular stents, and balloon punctoplasty.Citation45,Citation46 The use of stents is well-established now as an alternative modality to incisional punctoplasty and has been found to be simple, safe, equally effective as snip punctoplasties, and minimally invasive with preservation of the punctal anatomy and lacrimal pump functions.Citation46–49 Stents also have the potential advantage of simultaneously addressing associated canalicular stenosis. Quality of life assessment has demonstrated monoka stents to be very effective (93% anatomical and functional success) in managing primary punctal stenosis.Citation50 The use of balloon punctoplasty is recently being investigated as an alternate option.Citation51,Citation52 Although initial results appear promising, well-designed studies are underway to assess their utility in the management of primary punctal stenosis.
VI. Conclusion
The paper reviews the current anatomical and physiological evidence to present an alternate perspective on routine punctoplasty. In light of the evidence discussed, the authors propose that while punctoplasty can continue to be performed for recurrent or recalcitrant cases of punctal stenosis and canaliculitis, the indications for a 3-snip or 4-snip-punctoplasty be critically analyzed for routine punctoplasty. The use of minimally invasive modalities for primary cases is on the rise with successful preservation of the physiological functions of the punctum and canaliculus. We still do not have a detailed understanding of punctal and canalicular functions. A better understanding would translate to better patient management in the future. To quote Dr Lester. T. Jones, “Only too often we seem willing to attack a normal structure instead of the abnormal one that is the cause of the disease. This is certainly true of the ‘three-snip’ operation. The surgeon apparently had assumed that if one ‘three-snip operation’ works so well on a single canaliculus, two would work twice as well. Perhaps we should call this the ‘six-snip’ operation. This patient with the four crippled canaliculi, now wants me to cure his epiphora. Gentlemen, how would any of you like to be in my predicament?”Citation7 Given our evolving understanding of the anatomy and physiology of the punctum and canaliculus, it may be time to debate the performance of routine punctoplasty. It may be preferable to consider an ounce of prevention over a pound of cure.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Additional information
Funding
References
- Ali MJ. Lacrimal disorders and surgery: historical perspectives. Int Ophthalmol. 2014;34(6):1309–1313. doi:10.1007/s10792-014-0003-0.
- Caesar RH, McNab AA. A brief history of punctoplasty: the 3-snip revisited. Eye (Lond). 2005;19(1):16–18. doi:10.1038/sj.eye.6701415.
- Offutt WN 4th, Cowen DE. Stenotic puncta: microsurgical punctoplasty. Ophthalmic Plast Reconstr Surg. 1993;9(3):201–205. doi:10.1097/00002341-199309000-00006.
- Graves B. Making a new lacrimal punctum. Am J Ophthalmol. 1926;9:675–677. doi:10.1016/S0002-9394(26)90482-0.
- Thomas JB. A modification of Graves’ operation for epiphora due to stenosis of the lacrimal punctum. Br J Ophthalmol. 1951;35(5):306. doi:10.1136/bjo.35.5.306.
- Viers ER. Disorders of the canaliculus. The Lacrimal System. Grune & Stratton, New York; 1955:46–47.
- Jones LT. The cure of epiphora due to canalicular disorders, trauma and surgical failures on the lacrimal passages. Trans Am Acad Ophthalmol Otolaryngol. 1962;66:506–524.
- Hughes WL, Maris CS. A clip procedure for stenosis and eversion of the lacrimal punctum. Trans Am Acad Ophthalmol Otolaryngol. 1967;71:653–655.
- Edelstein J, Reiss G. The wedge punctoplasty for treatment of punctal stenosis. Ophthalmic Surg. 1992;23:818–821.
- Dolin SL, Hecht SD. The punctum pucker procedure for stenosis of the lacrimal punctum. Arch Ophthalmol. 1986;104(7):1086–1087. doi:10.1001/archopht.1986.01050190144055.
- Lam S, Tessler HH. Mitomycin as adjunct therapy in correcting iatrogenic punctal stenosis. Ophthalmic Surg. 1993;24:123–124.
- Chak M, Irvine F. Rectangular 3-snip punctoplasty outcomes: preservation of the lacrimal pump in punctoplasty surgery. Ophthalmic Plast Reconstr Surg. 2009;25(2):134–135. doi:10.1097/IOP.0b013e3181994062.
- Kim SE, Lee SJ, Lee SY, Yoon JS. Outcomes of 4-snip punctoplasty for severe punctal stenosis: measurement of tear meniscus height by optical coherence tomography. Am J Ophthalmol. 2012;153(4):769–773. doi:10.1016/j.ajo.2011.09.026.
- Carter KD, Nelson CC, Martonyi CL. Size variation of the lacrimal punctum in adults. Ophthalmic Plast Reconstr Surg. 1988;4(4):231–233. doi:10.1097/00002341-198804040-00006.
- Kamal S, Ali MJ, Ali MH, Naik MN. Fourier domain optical coherence tomography with 3D and En face imaging of the punctum and vertical canaliculus: a step toward establishing a normative database. Ophthalmic Plast Reconstr Surg. 2016;32(3):170–273. doi:10.1097/IOP.0000000000000396.
- Bothra N, Saini P, Ali MJ. 2022. Age- related changes in the lacrimal punctum morphology in a normal population: punctum update (PUP) study - paper 1. Ophthalmic Plast Reconstr Surg. Accepted.
- Wulc AE, Dryden RM, Khatchaturian T. Where is the gray line? Arch Ophthalmol. 1987;105(8):1092–1098. doi:10.1001/archopht.1987.01060080094035.
- Takahashi Y, Kakizaki H, Nakano T, Asamoto K, Ichinose A, Iwaki M. Anatomy of the vertical lacrimal canaliculus and lacrimal punctum: a macroscopic study. Ophthalmic Plast Reconstr Surg. 2011;27(5):384–386. doi:10.1097/IOP.0b013e318219a54b.
- Whitnall SE. The Anatomy of the Human Orbit and Accessory Organs of Vision. 2nd ed. London: Oxford University Press Inc; 1932:133–134.
- Lipham WJ, Tawfik HA, Dutton JJ. A histologic analysis and three-dimensional reconstruction of the muscle of Riolan. Ophthalmic Plast Reconstr Surg. 2002;18(2):93–98. doi:10.1097/00002341-200203000-00002.
- Kakizaki H, Takahashi Y, Iwaki M, Nakano T, Asamoto K, Ikeda H, et al. Punctal and canalicular anatomy: implications for canalicular occlusion in severe dry eye. Am J Ophthalmol. 2012;153(2):229–237. doi:10.1016/j.ajo.2011.07.010.
- Ali MJ, Baig F, Lakshman M, Naik MN. Scanning electron microscopic features of the external and internal surfaces of normal adult lacrimal drainage system. Ophthalmic Plast Reconstr Surg. 2015;31(5):414–417. doi:10.1097/IOP.0000000000000489.
- Ali MJ, Paulsen F. Horner’s muscle or Horner-Duverney’s muscle. Ophthalmic Plast Reconstr Surg. 2020;36(2):208. doi:10.1097/IOP.0000000000001574.
- Ali MJ, Zetzsche M, Scholz M, Hahn D, Gaffling S, Heichel J, et al. New insights into the lacrimal pump. Ocul Surf. 2020;18(4):689–698. doi:10.1016/j.jtos.2020.07.013.
- Viso E, Rodríguez-Ares MT, Gude F. Prevalence and associations of external punctal stenosis in a general population in Spain. Cornea. 2012;31(11):1240–1245. doi:10.1097/ICO.0b013e31823f8eca.
- Das AV, Rath S, Naik MN, Ali MJ. The incidence of lacrimal drainage disorders across a tertiary eye care network: customization of an indigenously developed electronic medical record system-eyeSmart. Ophthalmic Plast Reconstr Surg. 2019;35(4):354–356. doi:10.1097/IOP.0000000000001257.
- Ali MJ, Mishra DK, Baig F, Lakshman M, Naik MN. Punctal stenosis: histopathology, immunology, and electron microscopic features-a step toward unraveling the mysterious etiopathogenesis. Ophthalmic Plast Reconstr Surg. 2015;31(2):98–102. doi:10.1097/IOP.0000000000000204.
- Kashkouli MB, Beigi B, Astbury N. Acquired external punctal stenosis: surgical management and long-term follow-up. Orbit. 2005;24:73–78. doi:10.1080/01676830490916055.
- Chalvatzis NT, Tzamalis AK, Mavrikakis I, Tsinopoulos I, Dimitrakos S. Self retaining bicanaliculus stents as an adjunct to 3-snip punctoplasty in the management of upper lacrimal duct stenosis: a comparison to standard 3-snip procedure. Ophthal Plast Reconstr Surg. 2013;29(2):123–127. doi:10.1097/IOP.0b013e31827f5a10.
- Ali MJ, Ayyar A, Naik MN. Outcomes of rectangular 3-snip punctoplsaty in acquired punctal stenosis: is there a need to be minimally invasive? Eye. 2015;29(4):515–518. doi:10.1038/eye.2014.342.
- Murdock J, Lee WW, Zatezalo CC, Ballin A. Three-snip punctoplasty outcome rates and follow up treatments. Orbit. 2015;34(3):160–163. doi:10.3109/01676830.2015.1014513.
- Shahid H, Sandhu A, Keenan T, Pearson A. Factors affecting outcome of punctoplasty surgery: a review of 205 cases. Br J Ophthalmol. 2008;92:1689–1692. doi:10.1136/bjo.2008.140681.
- Wong ES, Li EY, Yuen HK. Long-term outcomes of punch punctoplasty with Kelly punch and review of literature. Eye (Lond). 2017;31:560–565.
- Cao X, Hu ZZ, Wu Y, Song Y, Liu QH. Rectangular 3-snip punctoplasty versus punch punctoplasty with silicone intubation for acquired external punctal stenosis: a prospective randomized comparative study. Int J Ophthalmol. 2021;14(6):849–854. doi:10.18240/ijo.2021.06.09.
- Franklin B, Sparks J. In ‘The Works of Benjamin Franklin’ 1840;1:134.
- Kaliki S, Ali MJ, Honavar SG, Chandrasekhar G, Naik MN. Primary canaliculitis: clinical features, microbiological profile, and management outcome. Ophthalmic Plast Reconstr Surg. 2012;28(5):355–360. doi:10.1097/IOP.0b013e31825fb0cd.
- Kim UR, Wadwekar B, Prajna L. Primary canaliculitis: the incidence, clinical features, outcome and long-term epiphora after snip-punctoplasty and curettage. Saudi J Ophthalmol. 2015;29(4):274–277. doi:10.1016/j.sjopt.2015.08.004.
- Vécsei VP, Huber-Spitzy V, Arocker-Mettinger E, Steinkogler FJ. Canaliculitis: difficulties in diagnosis, differential diagnosis and comparison between conservative and surgical treatment. Ophthalmologica. 1994;208(6):314–317. doi:10.1159/000310528.
- Anand S, Hollingworth K, Kumar V, Sandramouli S. Canaliculitis: the incidence of long-term epiphora following canaliculotomy. Orbit. 2004;23(1):19–26. doi:10.1076/orbi.23.1.19.28985.
- Lin SC, Kao SC, Tsai CC, Cheng CY, Kau HC, Hsu WM, et al. Clinical characteristics and factors associated the outcome of lacrimal canaliculitis. Acta Ophthalmol. 2011;89(8):759–763. doi:10.1111/j.1755-3768.2009.01827.x.
- Khu J, Mancini R. Punctum-sparing canaliculotomy for the treatment of canaliculitis. Ophthalmic Plast Reconstr Surg. 2012;28(1):63–65. doi:10.1097/IOP.0b013e318244a367.
- Buttanri IB, Serin D, Akbaba M, Karslioğlu S. Incision-sparing management of canaliculitis. Orbit. 2014;33(5):356–358. doi:10.3109/01676830.2014.907812.
- Law DZ, Goh ES. Incision-sparing management of canaliculitis: an efficacious alternative to surgical management. Can J Ophthalmol. 2017;52(3):258–263. doi:10.1016/j.jcjo.2016.10.013.
- Bothra N, Sharma A, Bansal O, Ali MJ. Punctal dilatation and non-incisional canalicular curettage in the management of infectious canaliculitis. Orbit. 2020;39(6):408–412. doi:10.1080/01676830.2019.1704797.
- Goldberg H, Priel A, Zloto O, Koval T, Varkel L, Ben Simon GJ. Kelly punch punctoplasty vs. simple punctal dilation, both with mini-monoka silicone stent intubation, for punctal stenosis related epiphora. Eye (Lond). 2021;35(2):532–535. doi:10.1038/s41433-020-0891-3.
- Hussain RN, Kanani H, McMullan T. Use of mini-monoka stents for punctal/canalicular stenosis. Br J Ophthalmol. 2012;96(5):671–673. doi:10.1136/bjophthalmol-2011-300670.
- Mathew RG, Olver JM. Mini-monoka made easy: a simple technique for mini-monoka insertion in acquired punctal stenosis. Ophthalmic Plast Reconstr Surg. 2011;27(4):293–294. doi:10.1097/IOP.0b013e31820ccfaf.
- Or L, Zadok D, Hartstein ME. Mini-monoka stenting for patients with perennial allergic conjunctivitis. Orbit. 2019;38(4):285–289. doi:10.1080/01676830.2018.1518465.
- Singh S, Ali MJ, Mohamed A. Comparison of outcomes of 3-snip punctoplasty versus simple punctal dilatation with monocanalicular intubation for acquired punctal stenosis. Ophthalmic Plast Reconstr Surg. 2018;34(4):375–377. doi:10.1097/IOP.0000000000001024.
- Gupta S, Ali MJ, Ali MH, Naik MN. Assessing the outcomes of mini-Monoka stent dilatation for primary punctal stenosis using the lacrimal symptom questionnaire. Indian J Ophthalmol. 2018;66(2):269–271. doi:10.4103/ijo.IJO_799_17.
- Ali MJ, Bothra N. Balloon punctoplasty in punctal stenosis. Orbit. 2021;40(4):346. doi:10.1080/01676830.2020.1776341.
- Sharma A, Pattnaik M, Ali MJ. A rare case of pemetrexed-induced diffuse punctal and canalicular stenosis: management by coronary balloon puncto-canaliculoplasty. Orbit. 2021. Epub. doi:10.1080/01676830.2021.1923042.
