Abstract
The cervical area of teeth is the most unpredictable region for durable adhesive bonding. This study evaluated the adhesion potential of resin cement to coronal and cervical/root structures with a focus on enamel, dentin and cementum using etch-and-rinse and self-etch adhesive systems. Anterior teeth (N = 60) were randomly divided into six groups for adhesion tests: (a) unprepared enamel (UE), (b) ground enamel (GE), (c) mid-coronal dentin (D), (d) cervical enamel 2 mm above cementoenamel junction (CE), (e) cementoenamel junction (CEJ), and (f) root cementum (RC). Enamel and dentin surfaces were conditioned using either an etch-and-rinse (Syntac Classic-SY) or self-etch (Clearfil S3 Bond Plus-CS3) adhesive system. Resin cement (Variolink Esthetic) was adhered to the different substrates using polyethylene molds and photo-polymerized. Bonded specimens were stored in water for 24 h at 37 °C. Microshear tests (µSBT) were conducted in a Universal Testing Machine (1 mm/min) and failure types were analyzed after debonding. Data were analyzed using two-way ANOVA and t-test (alpha = 0.05). While substrate type (p < 0.001) and adhesive system (p < 0.001) significantly affected the bond results, interaction terms were not significant (p = 0.063). Within SY adhesive system, adhesion to all substrates were not significant ranging between (8.07 ± 2.39–6.80 ± 4.60) (p > 0.05), except for CEJ (5.19 ± 1.39) and RC (4.08 ± 1.13). With the CS3 adhesive system, all groups presented non-significant results (4.15 ± 1.35–6.04 + 2.38) (p > 0.05), except for D (3.57 ± 1.84) and RC (3.21 ± 1.13) (p < 0.05). µSBT values for D (7.19 ± 2.31) and RC (4.08 ± 1.13) were significantly higher for SY compared to that of CS3 (3.57 ± 1.84–3.21 ± 1.13, respectively) (p < 0.05).
Introduction
For many decades, the treatment of choice for the unaesthetic anterior teeth were based on preparation of the teeth for full coverage crowns, which resulted in a large amount of loss of healthy tooth substance which is irreversible. Furthermore, tooth preparation can have adverse effects on the pulp and the periodontal tissues [Citation1]. With the advances in the field of adhesive dentistry, the treatment spectrum for reconstructions was broadened and direct or indirect resin composite restorations and ceramic veneers have become successful options to restore the anterior teeth due to caries, trauma or optical reasons [Citation1,Citation2].
A veneer is a thin porcelain shell, which is bonded to a minimally prepared tooth surface through dental adhesives and luting composites. This minimally invasive treatment relies on the ability of resin composites adhere to the tooth [Citation3]. Amongst other invasive treatment options, for the long-term retention of porcelain veneers, a strong and stable bond between the luting composite and the tooth is essential [Citation3]. However, clinical trials show a deterioration of the bond at the margins of porcelain veneers and particularly at the cervical regions of the anterior tooth [Citation4–7]. Such debonding could yield to not only optical but also other problems such as secondary caries, post-operative sensitivity and plaque accumulation [Citation8–10]. Also, especially the treatment of periodontal diseases can result in gingival recessions and exposed root surfaces in the anterior tooth area, which is for many patients is the reason to seek treatment with veneers. The differences in tooth structure at different locations significantly dictate the adhesion of resin-based materials. For instance, morphological structure of dental enamel at the cervical enamel border, cementoenamel junction (CEJ), significantly differs from that of incisal enamel. The enamel prism exhibits frequently a disturbed arrangement in the cervical region whereas on the coronal part they present a more organized morphology [Citation11–15]. Such structural characteristics of cervical enamel affect the bonding of restorative materials [Citation11–15]. The CEJ is a complex area where different hard tissues of the tooth come together, namely enamel overlapped by cementum; enamel and cementum edge-to-edge; a gap, revealing a strip of exposed dentin; and cementum overlapped by enamel [Citation16,Citation17]. The distribution of the hard tissues found at the CEJ is unpredictable and irregular in all individual teeth as well as within the same tooth [Citation17,Citation18]. Therefore, abrasion of CEJ due to aggressive toothbrushing, biofilm or acidic dietary may result in wear or defects at variable levels in individuals in this region. The root portion of the teeth on the other hand, consists of root cementum and root dentin onto which veneers are bonded in gingival recession cases. The cementum around the CEJ is acellular and afibrillar cementum. It is a non-homogenous matrix composed of multiple calcified layers without collagen fibers [Citation19]. The coronal two-thirds of the root surface is typically covered by a thin layer of acellular extrinsic fibre cementum [Citation19] which consists of short collagenous fibers that are fixed in the dentinal matrix and run perpendicularly to the root surface [Citation20].
The microstructure and properties of dentin are determinants of adhesive procedures in restorative dentistry [Citation21]. Dentin consists of dentin tubules that run from the dentin-enamel junction (DEJ) to the pulpal coronal dentin, and from cementum-dentin junction to the pulp canal in the root [Citation22]. Not only in different parts of the tooth various forms of dentin exists but also physiological aging or disease processes can result in different forms of dentin. Root dentin for instance has a lower density of dentin tubules than coronal dentin. Such factors could influence the adhesion capacity of resin-based materials [Citation23,Citation24].
In addition to the anatomic and morphological variations on the tooth substrate, the adhesive system plays also an important role on the level of adhesion achieved. Adhesion promoters build a hybrid layer on the dental substrate as a result of resin component impregnating the enamel and dentin microstructure [Citation25]. In dentistry, the adhesive resin types can be classified into two main subgroups: etch-and-rinse and self-etch systems. Etch-and-rinse systems use a separate phosphoric acid before the application of the primer and adhesive solution which is a two- or three-step procedure. Self-etch systems, on the other hand, are based on acidic monomers that demineralize and impregnate the tooth substrates simultaneously. Such adhesives are available as one- or two-step systems [Citation26]. Recent data show similar results between adhesion potential of etch-and-rinse and self-etch systems where the latter could be easier to apply in bonding to root regions of the teeth as they require no etching and rinsing procedures.
The objective of this study, therefore, was to evaluate the adhesion potential of resin cement to coronal and cervical/root dental structures with a focus on enamel, dentin, cementoenamel junction and root cementum using total etch and self-etch adhesive systems. The null hypotheses tested were that bond strength results would be significantly affected neither by the tooth substrate and the adhesive material.
Materials and methods
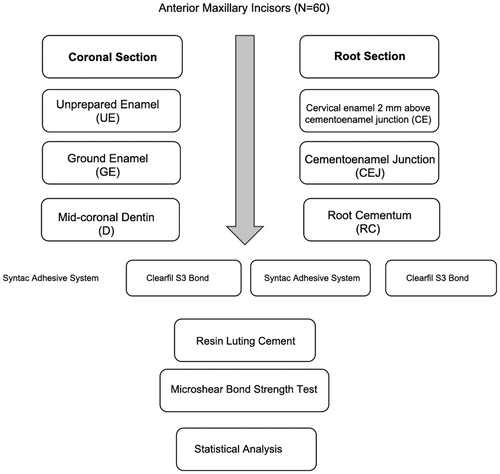
The brands, types, manufacturers and chemical compositions of the materials used in this study are listed in . Distribution of experimental groups based on the substrate type and test methods and sequence of experimental procedures are presented in .
Table 1. Brands, chemical compositions, manufacturers and batch numbers of the materials used in this study.
Specimen preparation
For this study, extracted human anterior incisor teeth (N = 60) with intact cementoenamel junction (CEJ) were collected. After tissue remnants were removed with a scaler (M23, Deppeler SA, Rolle, Switzerland) and stored in an aqueous solution of 0.2% chloramine trihydrate for no longer than 6 months prior to testing. All teeth used in the present study were extracted for reasons unrelated to this project. Written informed consent for research purpose of the extracted teeth was obtained by all donors prior to extraction according to the directives set by the National Federal Council. Ethical guidelines were strictly followed and irreversible anonymization was performed in accordance with State and Federal Law [Citation27–29].
The teeth were initially embedded plastic moulds (Scandiquick, Scandia, Hagen, Germany) with auto-polymerized polymethylmethacrylate using an acrylic resin (Duralay, Reliance, Illinois, USA) with their bonding surfaces exposed. They were then randomly divided into six groups for adhesion tests. On each tooth the coronal and cervical/root segments were selected for bonding regions. The groups consisted of (a) unprepared enamel (UE), (b) ground enamel (GE), (c) mid-coronal dentin (D), (d) cervical enamel 2 mm above cementoenamel junction (CE), (e) cementoenamel junction (CEJ), and (f) root cementum (RC).
For the cervical region, an area of 5 mm × 5 mm was selected for the test group. The area comprised a 2 mm-wide band of cervical enamel (CEJ) and a 2 mm-wide band of cervical root surface (CR). For the coronal control group, an area of 5 mm × 5 mm from the coronal middle third was selected. For group GE, enamel was removed (Isomet, Buehler Ltd., Lake Bluff, IL, USA) under water-cooling until flat dentin surfaces were achieved.
The teeth were then randomly divided into two subgroups where enamel and dentin surfaces were conditioned using either an etch-and-rinse (Syntac Classic, Ivoclar Vivadent, Schaan, Liechtenstein-SY) or one-bottle self-etch (Clearfil S3 Bond Plus, Kuraray, Tokyo, Japan-CS3) adhesive system.
Adhesive procedures
Subgroup SY: Following application of 35% phosphoric acid gel for 30 s on the enamel and 15 s on the dentin/root, etchant gel was removed with water spray for 10 s and the specimens were dried with an air syringe for 5 s. Primer (Syntac Primer, Ivoclar Vivadent) was applied on dentin rubbing gently with a microbrush against the tooth surface for 15 s. Before applying the adhesive, the surface was gently dried with an air syringe. Subsequently, the adhesive was applied for 10 s and dried again with air syringe. Finally, a thin layer of adhesive resin (Heliobond) was applied for 10 s and air-thinned. This was then photo-polymerized for 15 s with a polymerization lamp (Bluephase G2, Ivoclar Vivadent) at 1100mW/cm2 intensity from a constant distance of 2 mm from the surface. The output of the polymerization unit was verified by a radiometer (Demetron LC, SDS Kerr, Orange, CA, USA).
Subgroup CS3: Adhesive was applied with a microbrush for 10 s to the tooth surface. Thereafter, the specimen was gently air-thinned for 5 s and photo-polymerized for 10 s with a polymerization lamp (Bluephase G2) as described in group SY.
One calibrated operator carried out adhesive procedures throughout the experiments. After conditioning the surfaces with the different adhesive systems, transparent polytetrafluoroethylene (Teflon) molds (DuPont, Saint-Gobain, France) (inner surface area: 1 mm2, height: 4 mm) were placed perpendicularly to the substrate surface and filled with resin luting cement (Variolink Esthetic LC, Ivoclar Vivadent). Finally, the composite was photo-polymerized for 30 s from 5 directions. Oxygen inhibiting gel (Oxyguard, Kuraray, Tokyo, Japan) was applied at the bonded margins and rinsed with copious water after 1 min [Citation30].
Storage conditions
The specimens were stored in an incubator (Binder GmbH, Tuttlingen, Germany) in distilled water at 37 °C for 24 h and then subjected to bond tests.
Micro-shear test
For the micro-shear bond (µSBT) test, the specimens were mounted in the jig of the Universal Testing Machine (Zwick ROELL Z2.5 MA 18-1-3/7, Ulm, Germany) and the shear force was applied using a shearing blade to the adhesive interface until failure occurred. The load was applied to the adhesive interface, as close as possible to the surface of the substrate at a crosshead speed of 0.5 mm/min and the stress-strain curve was analyzed with the software program (TestXpert, Zwick ROELL, Ulm, Germany). The maximum load (N) was converted into megapascal (MPa) by dividing it by the bonding surface area of the resin cements.
Microscopic evaluation and failure type analysis
After adhesion tests, debonded specimen surfaces were analysed for failure types using an optical microscope (Zeiss MC 80 DX, Jena, Germany) at x50 magnification.
Statistical analysis
According to the two-group Satterthwaite t-test (SPSS Software V.20, Chicago, IL, USA) with a 0.05 two-sided significance level, a sample size of 15 in each experimental group was calculated to provide more than 80% power to detect a difference of 2 MPa between mean values. The statistical analysis was executed using the statistical software R (R Foundation for Statistical Computing, Vienna, Austria), including the software package Ggplot2 (Version 2016, Springer-Verlag, New York, USA). Before statistical evaluation, data were logarithmically transformed in order not to violate the ANOVA assumptions. Subsequently, a two-way analysis of variance (ANOVA) was used where the bond strength was the dependent variable and substrates types (6 levels: UE, GE, D, CE, CEJ, RC) and the bonding systems (2 levels: SY, CS3) as the independent variables. Multiple comparisons were analysed using Holm`s test. P values less than 0.05 were considered to be statistically significant in all tests.
Results
While substrate type (p < 0.001) and adhesive system (p < 0.001) significantly affected the bond results, interaction terms were not significant (p = 0.063) ().
Table 2. The mean bond strength values (MPa ± standard deviations) of µSBT.
Within SY adhesive system, adhesion to all substrates were not significant ranging between (8.07 ± 2.39–6.80 ± 4.60) (p > 0.05) except for CEJ (5.19 ± 1.39) and RC (4.08 ± 1.13) ().
Figure 2. Box plot graphic showing the logarithmic microshear bond strength (µSBT) (MPa) to coronal and root sections of teeth using Syntac Adhesive (SY) and Clearfil S3 Bond (CS3) adhesive systems. See for group abbreviations.
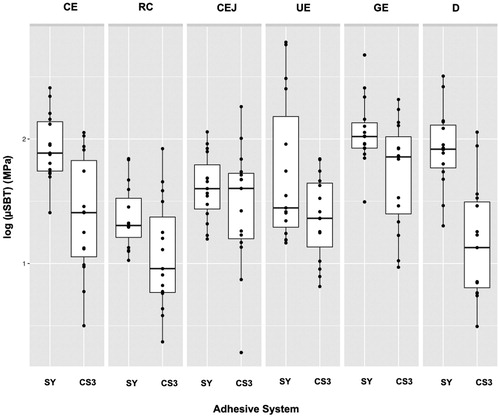
With the CS3 adhesive system, all groups presented non-significant results (4.15 ± 1.35–6.04 + 2.38) (p > 0.05), except for D (3.57 ± 1.84) and RC (3.21 ± 1.13) (p < 0.05).
µSBT values for D (7.19 ± 2.31) and RC (4.08 ± 1.13) were significantly higher for SY compared to that of CS3 (3.57 ± 1.84–3.21 ± 1.13, respectively) (p < 0.05).
Both unprepared (UE) and prepared (GE) substrates did not show significant differences with both SY and CS3 adhesive systems (p > 0.05).
No cohesive failures in the substrate were observed in any of the specimens.
Discussion
This study was undertaken in order to evaluate the adhesion of resin luting cement to unprepared, prepared enamel, dentin, cervical enamel, cementoenamel junction and root cementum on cervical area of the tooth using etch-and-rinse and self-etch adhesive systems. Based on the results of this study, since both the adhesive system and substrate type affected the results, the null hypotheses tested could be rejected.
In order to measure the bond strength values between an adhesives and tooth substrates, a number of methods have been suggested such as macro-, micro-shear macro or micro-tensile tests. Regardless of the test methodology, however, it is crucial that the bonding interface should be the most stressed region. Previous studies using stress distribution analyses have reported that some of the bond strength tests do not appropriately stress the interfacial zone [Citation30,Citation31]. Shear tests have been criticized for the development of non-homogeneous stress distributions at the bonded interface, inducing either underestimation or misinterpretation of the results, as the failure often starts in one of the substrates and not solely at the adhesive zone [Citation30,Citation31]. Conventional tensile tests also present some limitations, such as the difficulty of specimen alignment and the tendency for heterogeneous stress distribution at the adhesive interface. On the other hand, when specimens are aligned correctly, the microtensile test shows more homogeneous distribution of stress, and thereby more sensitive comparison or evaluation of bond performances [Citation32]. However, minute deviations in specimen alignment in the jig may cause increased bond strength due to shear component being introduced during deboning bonded joints [Citation32]. Overall, adhesion-related studies in dentistry, bonded surface areas range from 3 mm2 to 1 mm2 in macro- and micro-test methods, respectively [Citation33]. Due to the reduced bonded area and more homogeneous distribution of stresses, micro-test methods are suggested in adhesion tests [Citation30].
In this study, the area of interest, namely coronal and cervical regions of the tooth constitute a very small area of the tooth that could not allow for macro-shear or macrotensile test methods. Moreover, in contrast to the µTBS test, µSBT, does not require any slicing of the substrate prior to testing which may lead to pre-test failures simply due to vibrations during cutting specimens. It also has to be noted that the type of test chosen should be able to address the research question to be answered.
The clinical success of veneers depends on many factors such as tooth preparation, tooth surface, type of dental adhesives used and type and thickness of ceramic or composite materials [Citation1,Citation3]. A strong adhesion between the luting composite and the tooth surface is essential in order to avoid marginal gaps. It is well-established knowledge that the strongest bond strength of resin composite could be achieved on the enamel. However, especially in the cervical one third, the enamel layer is very thin and after veneer preparation, it is very likely that the dentin is exposed or a combination of enamel and dentin is present in this region [Citation34]. The same problem exists in teeth with gingival recessions where veneers are bonded on the cervical margin extending to the root surface depending on the level of recession in order to achieve aesthetic results.
In the present study, two different adhesive systems were tested, namely a 3-step etch-and-rinse (SY) system and a self-etch adhesive (CS3). The adhesive systems used showed a significant influence on the µSBS results. Mean values for SY were overall on the tested tooth substrates were higher than those achieved with CS3. The μSBT especially on coronal dentin (D) and root cementum (RC) were significantly higher than that with CS3, whereas on other substrates the results were lower with CS3 but not significant to that of SY. The non-significant difference between the two adhesive systems on the enamel containing coronal region could be due to the presence of enamel on to which micromechanical retention could be achieved that in turn compensates for the chemical adhesion achieved with the adhesive systems tested. The advantage of utilizing phosphoric acid etching in etch-and-rinse systems particularly for D and RC appears to be still advantageous over the self-etch versions. Self-etch adhesives become increasingly popular due to the reduction of chair-side time and the reduced technique sensitivity [Citation35].
The bond strength of self-etch adhesives to coronal enamel is controversially discussed in the literature. While some reported lower bond strength for self-etch adhesives [Citation36–38], others observed no difference between the bond strength of self-etch and etch-and-rinse adhesives to coronal enamel [Citation39–41]. From the structural perspective, the morphology of cervical enamel is different to that of the coronal enamel. In the cervical region towards the root, enamel demonstrates a thicker aprismatic structure [Citation11,Citation12,Citation14]. After etching, resin tags on the cervical enamel are shorter than those on the coronal enamel [Citation14]. This could be the reason for lower bond strength results in cervical enamel which is in line with previous studies, where also etch-and-rinse adhesives were used [Citation15,Citation41]. Shimada et al. [Citation15] on the other hand, found no significant difference between the bond strength of resin materials to cervical enamel using a two-step self-etch or a one-step etch-and-rinse adhesive but these results were not compared to etch-and-rinse adhesives. Therefore, the superiority of the data compared to etch-and-rinse adhesives cannot be stated.
Adhesion to enamel is typically achieved after etching enamel with H3PO4 that creates a highly micro-retentive surface that is easily wetted by hydrophobic resin-based adhesives [Citation42]. The adhesive resin then penetrates the etched surface through capillary action and subsequent polymerization of the resin facilitates micromechanical adhesion. Most commercially available enamel etching agents have a concentration ranging between 30% and 40%. When the concentration is less, the dicalcium phosphate dihydrate precipitates in the enamel surface becomes very difficult to remove by rinsing [Citation42]. While for orthodontic applications, enamel tissue removal is not needed when bonding brackets, in reconstructive dentistry, minimal room has to be created for the material that eventually necessitates the removal of surface enamel using mechanical methods such as the use of diamond burs, disks or air-borne particle abrasion. The next step after micromechanical roughening of the enamel is the application of the adhesive resin where the conditioned surface provides the foundation for better wettability of the adhesive resin and the following resin composite [Citation43,Citation44]. In minimally invasive dentistry, some applications such as sectional veneers could be also bonded to unground enamel. For this reason, in this study, both unground and ground enamel was studied. Although not significant with both adhesive systems, the ground enamel (GE) tend to present higher results which need to be investigated in a larger sample. Enamel is a crystalline substance that consists of hydroxyapatite arranged in prisms that comprises 96 wt% inorganic matter, 0.4–0.8 wt% organic matter such as proteins, lipids, carbohydrates or lactate and 3.2–3.6 wt% water [Citation42] and the histological structure of these hydroxyapatite crystals of enamel in cross section is hexagonal. From lateral perspective, they present small rods, of which each is built out of about 100 crystals [Citation43]. However, they may also appear as prisms and in the centre of the prisms, the crystals are placed parallel to the longitudinal axis and in the outer parts in almost 90° inclination [Citation43]. This change in direction gives the prisms a honeycomb shape structure and the interprismatic areas consist of more loosely packed and randomly oriented crystals surrounded by a higher quantity of water and inorganic matter. Thus, enamel microstructure is in fact not a homogeneous structure and anatomical variations could be observed on enamel surface also sometimes due to the presence of aprismatic enamel layer [Citation44]. The removal of this layer allows for better capillary reaction within the created etch prisms [Citation45].
In general, in adhesive dentistry, adhesion values to enamel are considered as gold standard as the etched enamel surface provides excellent micromechanical retention. The results obtained in this study on enamel are in line with those reported in orthodontics but lower than those of other studies (21.6 ± 5.8–29.2 ± 7.3 MPa) in combination with other resin composites [Citation30,Citation33,Citation35,Citation45]. In this study, adhesion procedures were performed on anterior teeth and not complying with ISO/TS 11405 specifications where the buccal dentin of molars are advised to be used as a substrate [Citation30]. Although caution was practiced aligning the enamel surface as parallel as possible, the convexity of the enamel surface could have caused early deflexion of the resin and thereby detachment from enamel surface which is an inherent problem in adhesion tests on un prepared enamel. On the other hand, on flat surfaces such as ground enamel and dentin, the obtained results were in line with previous studies when SBT (8 ± 3.7) or TBT (2.6 ± 1.4–5.08 ± 3.69) tests were used [Citation30,Citation33,Citation35,Citation45].
Unlike enamel, dentin consists only of about 68% inorganic hydroxyapatite where the rest is mostly organic collagen fibers. The primary bonding mechanism to dentin is primarily diffusion based and depends highly on hybridization or infiltration of resin within the exposed collagen fiber scaffold. Thus, true chemical bonding to dentin is fairly unlikely since the functional groups of monomers have only a weak affinity to the hydroxyapatite-depleted collagen [Citation46]. In this study, significantly higher results obtained D, using SY adhesive system could be related to the composition of primer and adhesive. In this system, Syntac Primer, a mild maleic acid is applied on dentin and subsequently dentin was rehydrated with adhesive resin (Syntac Adhesive) that is water-based. The lower pH could have contributed to this difference where similar observations were made in previous studies [Citation30,Citation47,Citation48]. Meta-analysis in the field of adhesion in dentistry signified that depending on the test method employed and the variation in chemical compositions, bond strength of resin based materials to dentin vary between 9 and 45.3 MPa [Citation49]. Unfortunately, to date, limited number of studies compared several test methods in one study or used enamel as a control substrate when testing dentin adhesives [Citation30,Citation49].
As for CEJ or RC regions, the adhesion achieved in these zones have more clinical implications in that microleakage experienced clinically as a consequence of the deterioration of the bond at the margins of the porcelain veneers, especially in the cervical region, the longevity could decrease [Citation5–7]. For veneer preparation, it is recommended to maintain the preparation completely in enamel to reach an optimal bonding [Citation50,Citation51]. However, it is almost impossible not to have enamel-dentin and in some cases CEJ and RC as a substrate after tooth preparation.
RC in the cervical area belongs to acellular extrinsic fiber cementum composed of Sharpey fibers where the overall degree of mineralization is about 45–60%. Cementum contains about 50% organic matrix and predominantly Type I collagen [Citation52]. The present study found significantly lower bond strength on RC than on GE with both adhesive systems. Okada et al. also found lower µSBS to cementum than to dentin using different self-etch adhesive systems. The mentioned study showed that after etching with phosphoric acid gel, the cementum surface presented a spongier morphology with a higher density of collagen fibrils network compared to etched dentin [Citation5]. The etch zone was deeper in cementum than in coronal dentin [Citation53]. The presence of thick and coarse collagen bundles in the etched RC may result in some water left which might have hampered the penetration of resin monomer into the intact zone [Citation54] resulting in lower bond strength compared to coronal structure.
In this study, testing procedures were simplified since interest was on a single anatomic zone. Adhesion of the while veneer covering the complex of enamel-dentin-root cementum assembly could be further investigated. Hydrolytic degradation was not involved in this study since it would not be possible age the coronal and cervical area separately. Furthermore, due to the very small surface area after debonding, since no cohesive substrate failures were observed no further failure analysis was made which could be considered as a limitation of the study. Nevertheless, clinical studies should report on problems associated with debonding or marginal problems in the CEJ and root regions when minimally invasive veneer applications are indicated and anatomical regional differences when bonding such reconstructions should be taken into consideration to increase the longevity of such indications.
Conclusions
From this study, the following could be concluded:
Adhesion of resin luting cement tested to both the coronal enamel and dentin substrates were affected by the etch-and-rinse and self-etch adhesive systems.
Regardless of the adhesive system employed, adhesion to root cementum presented the lowest results.
While adhesion to cementoenemal junction was lower with the etch and rinse system, the results were less favourable on dentin with the self-etch system.
Etch-and-rinse adhesive system tested demonstrated higher µSBT values for dentin and root cementum compared to that of self-etch system.
Clinical relevance
When bonding reconstruction, it could be stated that adhesion to cervical root cementum is less favourable compared to the adhesion to cementoenamel junction and coronal enamel and/or dentin. Overall, the etch-and-rinse-based adhesive system results in better adhesion and especially on coronal dentin compared to self-etch adhesive tested.
Acknowledgment
The authors acknowledge Mr. A. Trottmann, University of Zürich, Center for Dental and Oral Medicine, Zürich, Switzerland, for his assistance with the specimen preparations.
Disclosure statement
The authors did not have any commercial interest in any of the materials used in this study.
References
- Peumans M, Van Meerbeek B, Lambrechts P, et al. Porcelain veneers: a review of the literature. J Dent. 2000;28(3):163–177.
- Hikita K, Van Meerbeek B, De Munck J, et al. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater. 2007;23(1):71–80.
- Peumans M, Van Meerbeek B, Yoshida Y, et al. Porcelain veneers bonded to tooth structure: an ultra-morphological FE-SEM examination of the adhesive interface. Dent Mater. 1999;15(2):105–119.
- Calamia JR. Clinical evaluation of etched porcelain veneers. Am J Dent. 1989;2(1):9–15.
- Christensen GJ, Christensen RP. Clinical observations of porcelain veneers: a three-year report. J Esthet Dent. 1991;3(5):174–179.
- Walls AW. The use of adhesively retained all-porcelain veneers during the management of fractured and worn anterior teeth: part 2. Clinical results after 5 years of follow-up. Br Dent J. 1995;178(9):337–340. 6
- Peumans M, Van Meerbeek B, Lambrechts P, et al. Five-year clinical performance of porcelain veneers. Quintessence Int. 1998;29(4):211–221.
- Cox CF, Felton D, Bergenholtz G. Histopathological response of infected cavities treated with Gluma and Scotchbond dentin bonding agents. Am J Dent. 1988;1:189–194.
- Alani AH, Toh CG. Detection of microleakage around dental restorations: a review. Oper Dent. 1997;22(4):173–185.
- HekimoǧLu C, Anil N, Yalçin E. A microleakage study of ceramic laminate veneers by autoradiography: effect of incisal edge preparation. J Oral Rehabil. 2004;31(3):265–269.
- Silverstone LM, Saxton CA, Dogon IL, et al. Variation in the pattern of acid etching of human dental enamel examined by scanning electron microscopy. Caries Res. 1975;9(5):373–387.
- Arakawa Y, Takahashi Y, Sebata M. The effect of acid etching on the cervical region of the buccal surface of the human premolar, with special reference to direct bonding techniques. Am J Orthod. 1979;76(2):201–208.
- Denys FR, Retief DH. Variations in enamel etching patterns produced by different concentrations phosphoric acid. J Dent Assoc S Afr. 1982;37(3):185–189.
- Gaspersic D. Micromorphometric analysis of cervical enamel structure of human upper third molars. Arch Oral Biol. 1995;40(5):453–457.
- Shimada Y, Kikushima D, Tagami J. Micro-shear bond strength of resin-bonding systems to cervical enamel. Am J Dent. 2002;15:373–377.
- Neuvald L, Consolaro A. Cementoenamel junction: microscopic analysis and external cervical resorption. J Endod. 2000;26(9):503–508.
- Arambawatta K, Peiris R, Nanayakkara D. Morphology of the cemento-enamel junction in premolar teeth. J Oral Sci. 2009;51(4):623–627.
- Walter C, Kress E, Götz H, et al. The anatomy of non-carious cervical lesions. Clin Oral Investig. 2014;18(1):139–146.
- Schroeder HE. Handbook of microscopic anatomy. Vol. 5.5. Berlin; Heidelberg; New York; Tokyo: Springer; 1986.
- Beertsen W, Van den Bos T. Alkaline phosphatase induces the deposition of calcified layers in relation to dentin: an in vitro study to mimic the formation of afibrillar acellular cementum. J Dent Res. 1991;70(3):176–181.
- Marshall GW, Marshall SJ, Kinney JH, et al. The dentin substrate: structure and properties related to bonding. J Dent. 1997;25(6):441–158.
- Pashley DH. Dynamics of the pulpo-dentin complex. Crit Rev Oral Biol Med. 1996;7(2):104–133.
- Marshall GW. Dentin: microstructure and characterization. Quintessence Int. 1993;24(9):606–617.
- Giannini M, Carvalho RM, Martins LR, et al. The influence of tubule density and area of solid dentin on bond strength of two adhesive systems to dentin. J Adhes Dent. 2001;3:315–324.
- Silva e Souza MH, Carneiro KGK, Lobato MF, et al. Adhesive systems: important aspects related to their composition and clinical use. J Appl Oral Sci. 2010;18(3):207–214.
- Ozer F, Blatz MB. Self-etch and etch-and-rinse adhesive systems in clinical dentistry. Compend Contin Educ Dent. 2013;34(1):12–14.
- Human Research Ordinance (810.301), Art. 30.
- World Medical Association (WMA): Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. 64th WMA General Assembly, Fortaleza, Brazil, October 2013.
- Human Research Act (810.30), Art. 2 and 32, Human Research Ordinance (810.301), Art. 25.
- Bracher L, Özcan M. Adhesion of resin composite to enamel and dentin: a methodological assessment. J Adhes Sci Technol. 2018;32(3):258–271.
- Della Bona A, Van Noort R. Shear vs. tensile bond strength of resin composite bonded to ceramic. J Dent Res. 1995;74(9):1591–1596.
- Betamar N, Cardew G, van Noort R. Influence of specimen designs on the microtensile bond strength to dentin. J Adhes Dent. 2007;9(2):159–168.
- Van Meerbeek B, Peumans M, Poitevin A, et al. Relationship between bond strength tests and clinical outcomes. Dent Mater. 2010;26:100–121.
- Ferrari M, Patroni S, Balleri P. Measurement of enamel thickness in relation to reduction for etched laminate veneers. Int J Periodont Restor Dent. 1992;12:407–413.
- Lührs A-K, Guhr S, Günay H, et al. Shear bond strength of self-adhesive resins compared to resin cements with etch and rinse adhesives to enamel and dentin in vitro. Clin Oral Invest. 2010;14(2):193–199.
- Ibarra G, Vargas MA, Armstrong SR, et al. Microtensile bond strength of self-etching adhesives to ground and unground enamel. J Adhes Dent. 2002;4(2):115–124.
- Kiremitçi A, Yalçin F, Gökalp S. Bonding to enamel and dentin using self-etching adhesive systems. Quintessence Int. 2004;35(5):367–370.
- Pilecki P, Stone DG, Sherriff M, et al. Microtensile bond strengths to enamel of self-etching and one bottle adhesive systems. J Oral Rehabil. 2005;32(7):531–540.
- De Munck J, Van Meerbeek B, Satoshi I, et al. Microtensile bond strengths of one- and two-step self-etch adhesives to bur-cut enamel and dentin. Am J Dent. 2003;16:414–420.
- Perdigão J, Gomes G, Duarte S, et al. Enamel bond strengths of pairs of adhesives from the same manufacturer. Oper Dent. 2005;30:492–499.
- Brackett WW, Ito S, Nishitani Y, et al. The microtensile bond strength of self-etching adhesives to ground enamel. Oper Dent. 2006;31(3):332–337.
- Schwartz RS. Fundamentals of operative dentistry: a contemporary approach. Quintessence books. Chicago: Quintessence Publ; 1996. p. 209.
- Kugel G, Ferrari M. The science of bonding: from first to sixth generation. J Am Dent Assoc. 2000;131(Suppl):20S–25S.
- Joniot SB, Grégoire GL, Auther AM, et al. Three-dimensional optical profilometry analysis of surface states obtained after finishing sequences for three composite resins. Oper Dent. 2000;25(4):311–315.
- Woronko GAJ, St Germain HAJ, Meiers JC. Effect of dentin primer on the shear bond strength between composite resin and enamel. Oper Dent. 1996;21(3):116–121.
- Van Meerbeek B, De Munck J, Yoshida Y, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;3:215–235.
- Leirskar J, Oilo G, Nordbø H. In vitro shear bond strength of two resin composites to dentin with five different dentin adhesives. Quintessence Int. 1998;29(12):787–792.
- Krifka S, Börzsönyi A, Koch A, et al. Bond strength of adhesive systems to dentin and enamel – human vs. bovine primary teeth in vitro. Dent Mater. 2008;24(7):888–894.
- De Munck J, Mine A, Poitevin A, et al. Meta-analytical review of parameters involved in dentin bonding. J Dent Res. 2012;91(4):351–357.
- Gresnigt M, Cune MS, Jansen K, et al. Randomized clinical trial on indirect resin composite and ceramic laminate veneers: up to 10-year findings. J Dent. 2019;86:102–109.
- Gresnigt M, Cune MS, Schuitemaker J, et al. Performance of ceramic laminate veneers with immediate dentine sealing: an 11 year prospective clinical trial. Dent Mater. 2019;35(7):1042–1052.
- Bosshardt DD, Selvig KA. Dental cementum: the dynamic tissue covering of the root. Periodontol 2000. 1997;13:41–75.
- Okada H, Sadr A, Shimada Y, et al. Micro-shear bond strength of current one-step adhesives to cementum and dentin. Am J Dent. 2009;22:259–263.
- Yuan Y, Shimada Y, Ichinose S, et al. Hybridization quality in cervical cementum and superficial dentin using current adhesives. Dent Mater. 2008;24(5):584–593.