Abstract
Aims
To assess arm-muscle strength related to motor function in children with bilateral spastic cerebral palsy, 5–15 years old.
Methods
Muscle strength was measured for shoulder abductors, elbow extensors and flexors, wrist extensors, and grip strength. The children were grouped according to the Manual Ability Classification Scale (MACS).
Results
Forty-two children were included. The majority of the children at MACS levels I–II were within the normal range; shoulder abductors were weakest (mean 60–80% of predicted value), and variation was greatest for wrist extensors.
Children at MACS level II showed lower values than children at level I, with significant differences for shoulder abductors (p=.028) and wrist extensors (p<.001). Differences between the dominant and non-dominant side was greater in children at MACS level II and statistically significant for wrist extensors (p=.024).
Of 15 children tested for grip strength, nine were within the 2 SD range. The three children at MACS level II, all walking with a walker, had a higher mean value than those at MACS level I.
Conclusions
Muscle strength was lower and differences were greater between sides in children at MACS level II. Wrist extensors showed a decreasing trend with age as compared with normal development.
Cerebral palsy (CP) is divided into three subtypes ‒ spastic, dyskinetic, and ataxic ‒ and affects approximately two in 1,000 live-born children in the Western world (Himmelmann et al., Citation2005). The spastic type is the most common subtype (80%) and is itself subdivided into unilateral spastic CP (USCP), with one side of the body involved, and bilateral spastic CP (BSCP), with both sides involved (Himmelmann & Uvebrant, Citation2018; Prevalence & characteristics of children with cerebral palsy in Europe, 2002; Sellier et al., Citation2016). Motor impairment in CP is multifactorial and may include spasticity, dystonia, muscle contractures, bony deformities, incoordination, and muscle weakness (Arner et al., Citation2008; Christine et al., Citation2007; Gormley, Citation2001; Park et al., Citation2011). Additional challenges include impaired sensitivity and cognition as well as visual impairment and epilepsy.
Human regulation of arm and hand function is complex and involves several systems – visual, tactile sense, coordination, perception, neuromotor control, and muscle strength. All of those systems may be affected by a lesion in the central nervous system such as CP (Arnould et al., Citation2014). Most children with BSCP have a limited ability to use their hands during bimanual activities and find it difficult to handle objects in everyday life (Arner et al., Citation2008; Klevberg et al., Citation2017), but it is not yet fully established to what extent muscle weakness affects motor function in the upper extremities in children with BSCP. Muscle weakness in the legs in children with BSCP, and its effect on gross motor abilities such as walking, has been described by several authors (Desloovere et al., Citation2006; Ross & Engsberg, Citation2007). Motor function in the upper limbs has been described in terms of grip force, which is linked to the ability to reach and grasp (Eliasson et al., Citation2006), but there are few studies focusing on muscle strength in other muscle groups in the arms (Braendvik & Roeleveld, Citation2012). Furthermore, most upper-extremity research has been conducted in children with USCP, whereas reports on children with BSCP are scarce (Arner et al., Citation2008; Klevberg et al., Citation2017; Plasschaert et al., Citation2019). In children with USCP, muscle weakness alone or in combination with spasticity has been found to correlate with the ability to perform daily activities (Braendvik et al., Citation2013; Braendvik & Roeleveld, Citation2012; Klingels et al., Citation2012).
Normative values for typically developing children have been published for grip strength (Hager-Ross & Rosblad, Citation2002) and for four muscle groups in the upper extremity (Eek et al., Citation2006). However, to our knowledge, there are no reference values for these muscle groups in children with BSCP. The aim of this study was to assess arm-muscle strength relative to motor-function classification in children with BSCP, 5–15 years old.
Methods
Participants
Children were recruited for the study from a regional rehabilitation center in Sweden. The primary purpose was to measure muscle strength in the legs; related findings have been presented in a previous study (Eek & Beckung, Citation2008). Inclusion criteria were (i) a diagnosis of BSCP classified at level I, II, or III according to the Gross Motor Function Classification System (GMFCS) (Palisano et al., Citation1997), i.e. able to walk with or without assistive devices, and (ii) age 5 to 15 years. Measurements of arm-muscle strength were made at the same time as those of leg-muscle strength. The children were classified according to the Manual Ability Classification System (MACS) (Eliasson et al., Citation2006) and their hand dominance was noted based on the hand preferred for writing or drawing. Exclusion criteria were (i) dyskinetic CP, (ii) hand surgery in the past 12 months, and (iii) botulinum neurotoxin A injections in the past six months.
The study was approved by the Board of Ethics at Sahlgrenska University Hospital, case No. Ö 478-01, January 17, 2002. Written informed consent was obtained from the parents for all participants.
Measures
Muscle strength was measured for four muscle groups in the arms (shoulder abductors, elbow extensors and flexors, and wrist extensors) using a handheld myometer (adapted Chatillon dynamometer; Axel Ericson Medical AB, Gothenburg, Sweden).
The isometric “make” technique was used where the child gradually builds up force against the myometer for about 5 seconds. Three attempts were made for each muscle group and the highest recorded force value was used for data analysis. The test began with different sides of the body for different individuals. The lever arm was measured using a tape measure and the torque (Nm) was calculated by multiplying the force with the length of each lever arm. All values were then normalized to Nm/kg through division with each subject’s body weight. The procedure is described in greater detail in a normative study of children 5–15 years of age (Eek et al., Citation2006). For a description of measurement details, see . The normative material includes equations that yield predicted muscle-strength values for each muscle group, based on age, body weight, and sex. Calculating percentages of the predicted values for each patient and muscle group enables comparison of muscle strength across muscle groups as well as group-level comparison of children at different ages.
Table 1. Description of measurements with the myometer. Position and stabilization of the subject, placement of the myometer’s resistance to the body movement and point for measurement of lever arm.
For a subgroup of participants, a recording was also made of maximal grip strength (in Newton), measured using the Grippit® dynamometer. Their values were compared with reference values for the respective age groups, presented along with SDs (Hager-Ross & Rosblad, Citation2002). A handle adapted to the child’s hand size (depth and width 27 mm, circumference 5 mm) was used.
Data Analysis
The data were tested for normality using the Shapiro–Wilk test and were found to be normally distributed. Comparison between dominant and non-dominant side was made using the paired-samples t-test, and comparison between MACS levels was made using the independent-samples t-test. Correlations between muscle-strength values and age, weight, height, and MACS level were calculated using the Pearson product-moment coefficient. Correlations were graded as follows: 0–0.25 = little; 0.26–0.49 = low; 0.50–0.69 = moderate; 0.70–0.89 = high; and 0.90–1 = very high (Domholdt, Citation2000). The significance level was set to <0.05.
The Statview (SAS Institute Inc., 100 SAS Campus Dr. Cary, NC 27513) and SPSS version 25 (SPSS Inc., 233 S Wacker Dr., 11th Fl., Chicago, IL 60606) software packages were used for the statistical analysis.
Results
A total of 42 children were tested. However, since the few children at MACS levels III (two) and IV (one) were excluded from the statistical analysis, only 39 children at MACS levels I–II were included in the study. There were 12 girls and 27 boys with a mean age of 11.3 (see ); 38 of them were tested for muscle strength in the arms and 15 were tested for grip strength.
Table 2. Description of participants, mean (SD).
The children at MACS levels I and II did not differ as a group in terms of age, weight, or height. Twenty-six children had right-hand dominance and ten had left-hand dominance. For three children, dominance was not known or no clear hand dominance could be determined; those three were excluded from the analysis of differences between sides.
Muscle Strength
Muscle strength in the arms, calculated as a percentage of normal predicted values, is presented in and . The values varied, but most were within the normal prediction interval. The shoulder abductors were the weakest, with a mean of 80% of the predicted value in children at MACS level I and 66% in those at MACS level II. Variation was greatest for the wrist extensors. Comparison of children at MACS levels I and II showed lower values for children at MACS level II, with significant differences for shoulder abductors and wrist extensors.
Figure 1. Box plot for four muscle groups in the arms, divided by MACS level. Data in % of predicted value, boxes indicating median and 25–75 percentile, and circles show observations outside 10 or 90 percentile. Dashed line indicating predicted normal.
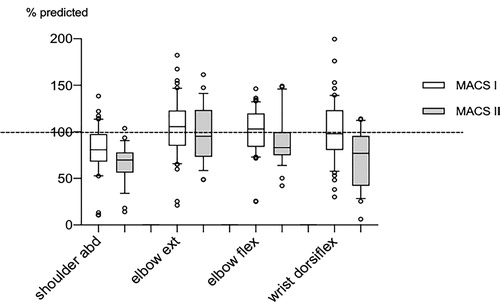
Table 3. Mean muscle strength in four muscle groups in the arms and grip strength. Data divided by MACS level and split by hand dominance. Values presented as % of predicted normal, mean (SD), and grip strength in Newton. Difference between non-dominant and dominant side calculated as a ratio.
The mean values were slightly higher on the dominant side, but the differences were small and the non-dominant arm was actually stronger in almost half of the cases (46%) in children at MACS level I. Greater differences between the sides were found for children at MACS level II, with a statistically significant difference for wrist extensors (p = 0.024). To determine the magnitude of the differences, a ratio was calculated between strength values for the non-dominant and dominant arms. Differences were found to be greatest for wrist extensors both at MACS level I and at MACS level II.
As mentioned above, the study only included two children at MACS level III. They both exhibited muscle weakness, with values below 60% of the predicted value for the non-dominant side in all muscle groups and for the dominant side in their wrist extensors. Further, there was a single child at MACS level IV, aged 5.9 years. That child was able to activate the elbow extensors and flexors but had difficulties in selective voluntary activation of shoulder abductors and wrist extensors.
Grip Strength
Grip strength was measured in twelve children at MACS level I and three at MACS level II (). Their mean age was 12.1 years (SD 2.0) for MACS level I and 12.1 years (SD 2.6) for MACS level II. Nine of the fifteen children had a grip strength within 1 SD of the normal range for their age. Of the others, one was above the 2 SD band, four were below 1 SD, and one was below 2 SD. The mean values were slightly higher for the dominant hand, but there was no significant difference between hands (p = 0.094).
Since grip strength was measured for only three children at MACS level II, no statistical analysis was made of differences between MACS levels. However, it is noticeable that the children at MACS level II had higher mean values. Those three children all used a walker, while the children at MACS level I could all walk without aids.
Correlation with Age, Weight, and Height
There were low to moderate correlations between the strength of the shoulder, elbow, and wrist muscles, on the one hand, and age, body weight, and height, on the other, with a single exception: for elbow flexors, there was only a correlation with height; see . Muscle strength showed a slight increase with age for shoulder abductors and elbow extensors, and a decrease for wrist extensors, compared with typical development. For grip strength, there was a high correlation with age and height for both the dominant hand and the non-dominant one, and a moderate correlation with weight for the non-dominant hand.
Table 4. Correlations between muscle strength and age, weight and height.
Discussion
This study presents data on upper-limb muscle strength in children with BSCP. We found that muscle strength was mostly within the normative predicted values for the elbow extensors and flexors. The wrist extensors and the shoulder abductors were the muscle groups most affected by weakness, with a significant difference between children at MACS levels I and II, respectively, for these muscle groups. For the wrist extensors, a difference was also found between the dominant and non-dominant sides for children at MACS level II. Grip strength in children at MACS level I was in most cases within the normal range (within 2 SDs), with no difference between the dominant and non-dominant side. In relative terms, muscle strength in the arms was closer to the predicted values than muscle strength in the legs as previously reported (Eek & Beckung, Citation2008). This was to be expected, as it is consistent with definitions of children with BSCP where it is stated that the involvement is greater in the legs (Surveillance of cerebral palsy in Europe: A collaboration of cerebral palsy surveys & registers. Surveillance of Cerebral Palsy in Europe (SCPE), 2000).
Muscle strength has previously been studied in children with USCP. Findings include that distal muscles are generally more affected than proximal muscles (Klingels et al., Citation2012; van Meeteren et al., Citation2007). This is in line with the present findings to the extent that distal-muscle weakness was found in the wrist extensors, but it is contradicted by our finding of muscle weakness in the shoulder abductors. This may be explained by a difference in measuring instruments. The study by Klingels et al. used a manual muscle test while a hand-held myometer was used in the present study. A portable hand-held dynamometer has been shown to be a reliable method for measuring muscle strength in children with CP (Taylor et al., Citation2004), and it is more sensitive than a manual muscle test, especially in grades 4 and 5 (moderate or maximal resistance to movement) (Schwartz et al., Citation1992). Another explanation could be that there is in fact a difference in shoulder-muscle strength between BSCP and USCP.
In the present study, we observed a tendency for the difference between the dominant and non-dominant sides to be greater in children at MACS level II, although this was statistically significant only for the wrist extensors. In children with BSCP, functional impairment can be either symmetrical or predominant on one side. The existence of the latter possibility may explain the differences found between sides in the present study (Klevberg et al., Citation2018). This hypothesis is corroborated by the even greater differences found between sides in the two children at MACS level III. The child at level IV had problems activating shoulder abductors and wrist extensors selectively. Such difficulties in activating some muscle groups can be seen to reflect findings from the study of muscle strength in the legs, where children at GMFCS level IV could not selectively activate several muscle groups in the legs (Eek & Beckung, Citation2008).
With regard to grip strength, the children at MACS level I obtained values similar to the reference material. Our results differ somewhat from those of a previous study where grip strength was reported to be significantly lower in nine children with CP than in typically developing children (von Walden et al., Citation2017). However, that study included mixed subgroups as well as a large proportion of children at MACS levels II and III, making comparison with our study difficult.
Findings from the present study and from previous ones indicate that distal-muscle weakness and a difference between sides are aspects of importance for bimanual performance, as described by MACS, in children with BSCP (Eliasson et al., Citation2006). In everyday activities both hands are used, but most often for different purposes: one hand performs the manipulative task while the other stabilizes the object being used. In theory, the latter task requires more muscle strength than the former (Eliasson, Citation2005). However, the role of muscle strength for hand function and the performance of everyday activities is not clear in children with BSCP. In fact, other aspects may be equally or more important, including selective motor control, different aspects of sensation, spasticity, co-contraction, and range of motion (Eliasson et al., Citation2006; Klingels et al., Citation2012). Further, the importance and impact of muscle weakness on performance may also vary between different activities. The combination of weak arms and hands, contractures, and increased muscle tone in the legs entails that various daily activities become difficult for children with BSCP, including walking and transfers. Finally, for children using walking aids, arm strength can be vital. Increased muscle strength because of frequent hand use is a likely explanation for the higher grip-strength values obtained in the present study by the children who used walkers.
There are several possible interventions targeting the upper limbs in CP: bimanual training, botulinum neurotoxin A injection, hand splints, and hand surgery – separately or in combined interventions (Novak & Honan, Citation2019; Ponten et al., Citation2011). All of these may theoretically affect muscle strength, both in order to increase but in some cases by decreasing it. Hence knowledge of the presence of muscle weakness is important when planning interventions.
There was a strong correlation between grip strength, on the one hand, and increasing age and weight, on the other. By contrast, correlations with age, height, and body weight were only low to moderate for the other muscle groups. An increase with age in (relative) grip strength has also been reported for children with USCP (Klingels et al., Citation2018). This difference in the development of muscle strength is difficult to explain and would require further investigation. However, it might be noted that the reference values for grip strength are based on age only, while weight is also considered for the other muscle groups. This might potentially cause the change to be of a different magnitude. Further, the values for wrist extensors manifested a slight decrease as compared with normal development. This negative trend may add to problems over time. A study of children at 14–76 months of age found decreased improvement over time in bimanual performance, with less development in children with BSCP than in those with USCP (Klevberg et al., Citation2018).
The pattern of correlation between hand-muscle strength and age differs from that found for leg-muscle strength, where there was a high correlation with weight but no correlation with age. Further, leg-muscle strength also showed a strong correlation with GMFCS level, suggesting that it is vital for walking capacity (Eek & Beckung, Citation2008). By contrast, motor performance in the upper limbs is dependent on several systems and muscle weakness is only one of the factors that may be relevant. Knowledge about the various components of the hand function is important for an increased understanding of how they affect performance and hence everyday-life activities. The present findings may contribute to the existing body of knowledge and lead to improved interventions for children with BSCP in the future.
Limitations
There are a few of limitations that affect the generalizability of the present findings.
First, the sample size was small, particularly when broken down by MACS level. Further, because of the small numbers of participants for grip strength and at MACS levels III and IV, no proper statistical analysis of the relevant subgroups could be performed.
Second, the children were recruited based on their GMFCS level. Since children with BSCP often have better function in the arms, this may have influenced the results (Carnahan et al., Citation2007).
Third, the proportions of girls and boys were not representative of the CP population – boys were overrepresented. However, the normative material relating to muscle strength did not show any differences between boys and girls until the age of 13 (Eek et al., Citation2006).
Conclusions
Muscle weakness was found in wrist extensors and shoulder abductors in children with BSCP at MACS level II. There were more differences between the dominant and non-dominant side in those with more difficulties in manual ability. For the wrist extensors, the children with CP did not keep pace with normal development.
Acknowledgements
We would like to express our sincere gratitude to all the children and adolescents as well as their parents who took the time to participate in and contribute to this study.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
Notes on contributors
Meta N. Eek
Meta N. Eek is an Associate Professor of physiotherapy at the Institute of Neuroscience and Physiology at the Sahlgrenska Academy, University of Gothenburg, Sweden.
Git Lidman
Git Lidman is a PhD and a registered Occupational Therapist, specialist in Habilitation and Disability Care at the Regional Rehabilitation Centre, Queen Silvia's Children's Hospital, Sahlgrenska University Hospital, Gothenburg, Sweden and a lecturer at the Institute of Neuroscience and Physiology at the Sahlgrenska Academy, University of Gothenburg, Sweden.
References
- Arner, M., Eliasson, A. C., Nicklasson, S., Sommerstein, K., & Hagglund, G. (2008). Hand function in cerebral palsy. Report of 367 children in a population-based longitudinal health care program. The Journal of Hand Surgery, 33(8), 1337–1347. https://doi.org/10.1016/j.jhsa.2008.02.032
- Arnould, C., Bleyenheuft, Y., & Thonnard, J. L. (2014). Hand functioning in children with cerebral palsy. Frontiers in Neurology, 5, 48phttps://doi.org/10.3389/fneur.2014.00048
- Braendvik, S. M., Elvrum, A.-K G., Vereijken, B., & Roeleveld, K. (2013). Involuntary and voluntary muscle activation in children with unilateral cerebral palsy-relationship to upper limb activity. European Journal of Paediatric Neurology: EJPN: Official Journal of the European Paediatric Neurology Society, 17(3), 274–279. https://doi.org/10.1016/j.ejpn.2012.11.002
- Braendvik, S. M., & Roeleveld, K. (2012). The role of co-activation in strength and force modulation in the elbow of children with unilateral cerebral palsy. Journal of Electromyography and Kinesiology: Official Journal of the International Society of Electrophysiological Kinesiology, 22(1), 137–144. https://doi.org/10.1016/j.jelekin.2011.10.002
- Carnahan, K. D., Arner, M., & Hägglund, G. (2007). Association between gross motor function (GMFCS) and manual ability (MACS) in children with cerebral palsy. A population-based study of 359 children. BMC Musculoskeletal Disorders, 8(1), 50. 2007/06/23. https://doi.org/10.1186/1471-2474-8-50
- Christine, C., Dolk, H., Platt, M. J., Colver, A., Prasauskiene, A., & Krageloh-Mann, I. (2007). Recommendations from the SCPE collaborative group for defining and classifying cerebral palsy. Developmental Medicine and Child Neurology. Supplement, 109, 35–38. https://doi.org/10.1111/j.1469-8749.2007.tb12626.x
- Desloovere, K., Molenaers, G., Feys, H., Huenaerts, C., Callewaert, B., & Van de Walle, P. (2006). Do dynamic and static clinical measurements correlate with gait analysis parameters in children with cerebral palsy? Gait & Posture, 24(3), 302–313. https://doi.org/10.1016/j.gaitpost.2005.10.008
- Domholdt, E. (2000). Statistical analysis of relationships: The basics. In Physical therapy research, principles and applications, 2nd ed. (pp. 354). Saunders.
- Eek, M. N., & Beckung, E. (2008). Walking ability is related to muscle strength in children with cerebral palsy. Gait & Posture, 28(3), 366–371. https://doi.org/10.1016/j.gaitpost.2008.05.004
- Eek, M. N., Kroksmark, A. K., & Beckung, E. (2006). Isometric muscle torque in children 5 to 15 years of age: normative data. Archives of Physical Medicine and Rehabilitation, 87(8), 1091–1099. https://doi.org/10.1016/j.apmr.2006.05.012
- Eliasson, A. C. (2005). Improving the use of hands in daily activities. Physical & Occupational Therapy in Pediatrics, 25(3), 37–60. https://doi.org/10.1080/J006v25n03_04
- Eliasson, A. C., Forssberg, H., Hung, Y. C., & Gordon, A. M. (2006). Development of hand function and precision grip control in individuals with cerebral palsy: a 13-year follow-up study. Pediatrics, 118(4), e1226–e1236. https://doi.org/10.1542/peds.2005-2768
- Gormley, M. E. Jr.(2001). Treatment of neuromuscular and musculoskeletal problems in cerebral palsy. Pediatric Rehabilitation, 4(1), 5–16. https://doi.org/10.1080/13638490151068393
- Hager-Ross, C., & Rosblad, B. (2002). Norms for grip strength in children aged 4-16 years. Acta Paediatr, 91(6), 617–625.
- Himmelmann, K., Hagberg, G., Beckung, E., Hagberg, B., & Uvebrant, P. (2005). The changing panorama of cerebral palsy in Sweden. IX. Prevalence and origin in the birth-year period 1995-1998. Acta paediatrica (Oslo, Norway : 1992), 94(3), 287–294. https://doi.org/10.1111/j.1651-2227.2005.tb03071.x
- Himmelmann, K., & Uvebrant, P. (2018). The panorama of cerebral palsy in Sweden part XII shows that patterns changed in the birth years 2007-2010. Acta Paediatrica, 107(3), 462–468. https://doi.org/10.1111/apa.14147
- Klevberg, G. L., Elvrum, A.-K G., Zucknick, M., Elkjaer, S., Østensjø, S., Krumlinde-Sundholm, L., Kjeken, I., & Jahnsen, R. (2018). Development of bimanual performance in young children with cerebral palsy. Developmental Medicine and Child Neurology, 60(5), 490–497. https://doi.org/10.1111/dmcn.13680
- Klevberg, G. L., Østensjø, S., Krumlinde-Sundholm, L., Elkjaer, S., & Jahnsen, R. B. (2017). Hand Function in a Population-Based Sample of Young Children with Unilateral or Bilateral Cerebral Palsy. Physical & Occupational Therapy in Pediatrics, 37(5), 528–540. https://doi.org/10.1080/01942638.2017.1280873
- Klingels, K., Demeyere, I., Jaspers, E., De Cock, P., Molenaers, G., Boyd, R., & Feys, H. (2012). Upper limb impairments and their impact on activity measures in children with unilateral cerebral palsy. European Journal of Paediatric Neurology: EJPN: Official Journal of the European Paediatric Neurology Society, 16(5), 475–484. https://doi.org/10.1016/j.ejpn.2011.12.008
- Klingels, K., Meyer, S., Mailleux, L., Simon-Martinez, C., Hoskens, J., Monbaliu, E., Verheyden, G., Verbeke, G., Molenaers, G., Ortibus, E., & Feys, H. (2018). Time course of upper limb function in children with unilateral cerebral palsy: A five-year follow-up study. Neural Plasticity. , 2018, 1–9. 2018/12/13. https://doi.org/10.1155/2018/2831342
- Novak, I., & Honan, I. (2019). Effectiveness of paediatric occupational therapy for children with disabilities: A systematic review. Australian Occupational Therapy Journal, 66(3), 258–273. https://doi.org/10.1111/1440-1630.12573
- Palisano, R., Rosenbaum, P., Walter, S., Russell, D., Wood, E., & Galuppi, B. (1997). Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine and Child Neurology, 39(4), 214–223. https://doi.org/10.1111/j.1469-8749.1997.tb07414.x
- Park, E. S., Sim, E. G., & Rha, D. W. (2011). Effect of upper limb deformities on gross motor and upper limb functions in children with spastic cerebral palsy. Research in Developmental Disabilities, 32(6), 2389–2397. https://doi.org/10.1016/j.ridd.2011.07.021
- Plasschaert, V. F. P., Vriezekolk, J. E., Aarts, P. B. M., Geurts, A. C. H., & Van den Ende, C. H. M. (2019). Interventions to improve upper limb function for children with bilateral cerebral palsy: A systematic review. Developmental Medicine and Child Neurology, 61(8), 899–907. https://doi.org/10.1111/dmcn.14141
- Ponten, E., Ekholm, C. L., & Eliasson, A. C. (2011). Bimanuality is improved by hand surgery in children with brain lesions: preliminary results in 18 children. Journal of Pediatric Orthopaedics B, 20(6), 359–365. https://doi.org/10.1097/BPB.0b013e328348aa69
- Prevalence and characteristics of children with cerebral palsy in Europe. (2002). Developmental Medicine & Child Neurology 44(9), 633–640.
- Ross, S. A., & Engsberg, J. R. (2007). Relationships between spasticity, strength, gait, and the GMFM-66 in persons with spastic diplegia cerebral palsy. Archives of Physical Medicine and Rehabilitation, 88(9), 1114–1120. https://doi.org/10.1016/j.apmr.2007.06.011
- Schwartz, S., Cohen, M. E., Herbison, G. J., & Shah, A. (1992). Relationship between two measures of upper extremity strength: manual muscle test compared to hand-held myometry. Archives of Physical Medicine and Rehabilitation, 73(11), 1063–1068.
- Sellier, E., Platt, M. J., Andersen, G. L., Krageloh-Mann, I., De La Cruz, J., & Cans, C. (2016). Decreasing prevalence in cerebral palsy: a multi-site European population-based study, 1980 to 2003. Developmental Medicine & Child Neurology, 58(1), 85–92. https://doi.org/10.1111/dmcn.12865
- Surveillance of cerebral palsy in Europe: A collaboration of cerebral palsy surveys and registers. Surveillance of Cerebral Palsy in Europe (SCPE). (2000). Developmental Medicine & Child Neurology, 42(12), 816–824. https://doi.org/10.1017/s0012162200001511
- Taylor, N. F., Dodd, K. J., & Graham, H. K. (2004). Test-retest reliability of hand-held dynamometric strength testing in young people with cerebral palsy. Archives of Physical Medicine and Rehabilitation, 85(1), 77–80. pp https://doi.org/10.1016/S0003-9993(03)00379-4
- van Meeteren, J., van Rijn, R. M., Selles, R. W., Roebroeck, M. E., & Stam, H. J. (2007). Grip strength parameters and functional activities in young adults with unilateral cerebral palsy compared with healthy subjects. Journal of Rehabilitation Medicine, 39(8), 598–604. https://doi.org/10.2340/16501977-0095
- von Walden, F., Jalaleddini, K., Evertsson, B., Friberg, J., Valero-Cuevas, F. J., & Ponten, E. (2017). Forearm flexor muscles in children with cerebral palsy are weak, thin and stiff. Frontiers in Computational Neuroscience, 11, 30. p https://doi.org/10.3389/fncom.2017.00030
