ABSTRACT
Background
Increasing evidence has linked repetitive negative thinking (RNT) to postnatal depression and anxiety, yet the factors moderating this relationship have been minimally investigated. During the COVID-19 pandemic of 2020, social restrictions imposed to reduce viral transmission limited access to social support, which is critical to postnatal psychological wellbeing – potentially intensifying RNT.
Objective
We examined whether perceived social support (from friends, family, and a significant other) played a moderating role in the relationship between RNT and maternal postnatal anxiety and depressive symptoms.
Methods
A sample of women (N = 251) who had given birth in the preceding 12 months completed an online battery of standardised measures during the COVID-19 ‘lockdown’ of May 2020.
Results
As predicted, social support moderated the relationship between RNT and depression such that the association between RNT and depression was stronger for women who reported lower levels of social support. Interestingly, this finding emerged for social support from friends only; for support from family and significant other, social support did not play a moderating role. Further, and unexpectedly, overall social support did not moderate the relationship between RNT and postnatal anxiety, however, social support from friends was a significant moderator.
Conclusions
High levels of perceived social support from friends (but not family or significant others) buffered the effects of RNT on depression and anxiety during the postpartum period. Strategies to bolster peer social support may be a valuable inclusion in interventions to prevent and treat postnatal depression and anxiety.
Introduction
The perinatal period is a time of significant change and uncertainty which often brings with it mental health issues such as depression and anxiety (Fawcett et al., Citation2019; Howard et al., Citation2018). This is problematic, as poor postnatal mental health is associated with negative mother–child interactions (Lefkovics et al., Citation2018; Matthies et al., Citation2017; Seymour et al., Citation2014), infant feeding behaviours (Fallon et al., Citation2018), and adverse outcomes for the child (Bauer et al., Citation2016; Glasheen et al., Citation2010; Netsi et al., Citation2018; Rees et al., Citation2019). In addition to the challenges of the postnatal period (e.g. caring for a newborn, feeding, sleep deprivation), the COVID-19 pandemic of 2020 imposed further stressors on new mothers (e.g. social isolation, fear of contracting the virus), which in turn served as additional risk factors for poor mental health (Holmes et al., Citation2020; Van Bavel et al., Citation2020). Indeed, there is accruing evidence of increased rates of perinatal depression and anxiety during the pandemic (Davenport et al., Citation2020; Lebel et al., Citation2020; Moyer et al., Citation2020; Wu et al., Citation2020).
Repetitive negative thinking (RNT) refers to perseverative, abstract thought in various forms; for example, rumination about the past (e.g. why did that happen?) and worry about the future (e.g. what if something goes wrong?) (Samtani & Moulds, Citation2017). Rumination has been most studied in the context of depression, guided by Response Styles Theory which proposes that the tendency to respond to sad mood by dwelling on its causes and consequences heightens vulnerability to developing depression (Nolen-Hoeksema, Citation1991). Worry has primarily been conceptualised and investigated in the context of anxiety (Borkovec, Ray, Stober et al., Citation1998). However, more recent theoretical acknowledgement of the overlapping and shared features of rumination and worry have prompted the consideration of both under the broad umbrella of RNT (McEvoy et al., Citation2010: Watkins, Citation2008).
RNT is an established transdiagnostic process, evident across psychological disorders including depression and anxiety. This relationship has been replicated in the perinatal context, such that there is evidence that RNT is associated with levels of both depression (DeJong et al., Citation2016) and anxiety (Moulds et al., Citation2018) symptoms in perinatal samples. In addition, there is evidence that RNT plays a predictive role. RNT levels in the first trimester predict depression later in pregnancy (Schmidt et al., Citation2016), and RNT in the third trimester predicts changes in depression symptoms from later pregnancy to 8 weeks post-birth – an association that was not moderated by antenatal depressive symptoms (Barnum et al., Citation2013). There are many ways in which the pandemic potentially fuelled RNT, for example, significant behavioural changes (e.g. reduced socialising) were required to slow transmission of the virus, and women faced disruptions in postnatal care. Moreover, many new mothers experienced anxiety about the possibility of both themselves and their babies contracting the virus, and (ongoing) uncertainty about the potential consequences (Caparros-Gonzalez & Alderdice, 2020).
In the broader literature, RNT (in the form of rumination) has been linked to reduced social support in both adults (Nolen-Hoeksema et al., Citation2008) and children (Abela et al., Citation2004). Extending this to a perinatal population, O’Mahen et al. (Citation2010) found that in pregnant women at high risk of developing depression, rumination predicted increases in depression symptoms 3 months later for those with low levels of social functioning. For women with high levels of social functioning, rumination and increases in depression symptoms were unrelated, suggesting that social functioning buffered the impact of rumination on depression (O’Mahen et al., Citation2010).
Social support is critical to perinatal psychological wellbeing (e.g. Bayrampour et al., 2016; Dennis et al., Citation2017; Harrison et al., Citation2020; Hetherington et al., Citation2018; Hughes et al., Citation2020; Milgrom et al., Citation2019). Low levels of social support during pregnancy have been associated with an increased risk of anxiety and depression postnatally, and similarly, low levels of social support at four-months postpartum have been related to an increased risk of anxiety at one-year postpartum (Hetherington et al., Citation2018). Although social support may come from a range of sources, not all forms of support are equally beneficial to postnatal wellbeing. Qualitative research has consistently highlighted the unique value of peer support (Coates et al., Citation2014; Harrison et al., Citation2020), whilst support from friends but not family is associated with decreasing levels of self-reported anxious-depressive symptoms across the transition to motherhood (pregnancy to 24 months postpartum) (Hughes et al., Citation2020). Social contact with other mothers, both one-to-one and in organised postnatal groups, has been found to help women normalise experiences, providing benefits over and above support from partners who may struggle to fully understand maternal experiences (Coates et al., Citation2014; Harrison et al., Citation2020). Given that lockdown restrictions during the pandemic (imposed to reduce the spread of the virus) reduced access to social support (Holmes et al., Citation2020; O’Connor et al., Citation2020), these measures may have had a particularly negative impact on postnatal women. It is possible that the absence of social support may have given rise to persistent RNT, which may (at least in part) have led to the increases in postnatal anxiety and depression documented during the pandemic (e.g. Wu et al., Citation2020).
We thus sought to investigate whether social support plays a role in postnatal mental health in the context of the COVID-19 pandemic; and in particular, whether it moderates the association between RNT and depression. Consistent with studies of RNT in the perinatal context to date, we measured self-reported symptoms of depression and anxiety, rather than establishing formal clinical diagnoses. Perception of social support is a highly subjective phenomenon, defined in this paper as the perceived adequacy of the assistance one receives from others (in line with Dambi et al, Citation2018). In keeping with previous research, this may take the form of emotional, informational, interactional or instrumental support (e.g. Brown, Citation1986; Hetherington et al., Citation2018). We were particularly interested in whether a differential moderating role of social support would emerge dependent upon the source of support (e.g. friends, family, significant other). To our knowledge, this possibility has not been explored in a perinatal sample. Further, given the link between RNT and antenatal anxiety (Harrison et al., Citation2021), we also examined whether perceived social support moderated this relationship in a sample of women who had had a baby in the previous 12 months.
As described above, previous research has found that RNT plays a predictive role in perinatal wellbeing (Barnum et al., Citation2013; Schmidt et al., Citation2016), and those with lower levels of social support may be more likely to engage in ruminative thoughts (Puterman et al., Citation2010) and experience anxiety and depression (Hetherington et al., Citation2018). Thus, we hypothesised that social support would moderate the relationship between RNT and depression; that is, that RNT and depression symptoms would be more strongly correlated in women with low levels of perceived social support than in those with high levels of social support. We predicted the same pattern of findings for RNT and anxiety symptoms. In the absence of previous research examining whether the moderating role varied as a function of the source of social support, we did not have any predictions about differences between sources of perceived social support in moderating the relationships between RNT and either depression or anxiety symptoms.
A secondary aim was to investigate how women sought support to mitigate the effects of isolation during the pandemic. As online technologies provide a means by which new mothers can gather parenting and wellbeing information, and engage with other expectant/new mothers online (Gleeson et al., Citation2019; Pedersen & Lupton, Citation2018), the use of technology in this period may protect against the effects of social isolation. We therefore examined participants’ use of technology to facilitate social contact and support, as well as explore its relationship with perceived social support and psychological wellbeing.
Materials and methods
Participants and procedure
A convenience sample of 251 postnatal women (who had given birth in the preceding 12 months) were recruited by advertising through mum-focused social media, forums and companies (n = 197), and via the participant recruitment service Prolific (n = 54). Inclusion criteria specified women were: (1) within 12 months postpartumFootnote1; (2) aged 18 and over; (3) living in the UK; and (4) fluent in English. All participants who completed the questionnaire were entered into a prize draw for one of three £20 Amazon vouchers.
Participants anonymously completed our online questionnaire between 1st May and 1 June 2020. Their demographic information is included in .
Table 1. Demographic information.
Measures
Edinburgh postnatal depression scale (EPDS)
10-item measure of perinatal depressive symptoms (Cox et al., Citation1987). Respondents rate the extent to which each item applied to them over the past week using a 4-point Likert scale. Higher scores indicate more symptoms; scores ≥13 indicate probable perinatal depression. Cronbach’s α = 0.87 (Cox et al., Citation1987).
Perinatal anxiety screening scale (PASS)
31-item measure of perinatal anxiety symptoms (Somerville et al., Citation2014). Scores range from 0 to 93 (≥26 indicating probable perinatal anxiety); scores between 21 and 41 suggest mild-moderate anxiety, and scores between 42 and 93 imply severe symptoms (Somerville et al., Citation2015). Cronbach’s α = 0.96 (Somerville et al., Citation2014).
Repetitive negative thinking questionnaire (RTQ-10; McEvoy et al., Citation2010, Citation2014)
10-item transdiagnostic measure of RNT. Items index the extent to which the respondent engages in RNT following a distressing event; higher scores indicate more RNT. Cronbach’s α = .89 (McEvoy et al., Citation2010).
Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al., Citation1988)
12-item measure of the respondent’s perception of support from friends, family and a significant other rated along a seven-point Likert scale from 1 (very strongly disagree) to 7 (very strongly agree). Cronbach’s α = 0.92 in perinatal cohorts (Zimet et al., Citation1990).
We initially included a measure of loneliness, but the Cronbach’s α was so low (<.5), we deemed it unreliable. Participants also provided demographic information, including details about how COVID-19 affected access to social support, the use of technology to access support during lockdown, and opinions/worries about COVID-19.
Results
The data were analysed using a positivist approach, within a conceptual framework that characterises depression and anxiety as biopsychosocial constructs which result from (and are maintained by) an interaction between biological, social/environmental and psychobehavioural/cognitive factors. The current study focused specifically on two important social (perceived social support) and cognitive (RNT) factors, and how they may interact to predict depression and anxiety.
Depression and anxiety were analysed as separate outcome variables. Data were screened using SPSS v26. Assumptions of normality and linearity were met, and Cook’s Distance values were all <1. Using the above-described cut-offs for the PASS (≥26) and EPDS (≥13), 49% of participants scored above the cut-off for probable anxiety, and 49% reported probable depression.
Bivariate analyses
There were significant correlations among all variables (see ). Both depression and anxiety were negatively related to perceived social support, and positively related to RTQ-10. Variables in were examined as potential covariates using one-way ANOVAs and correlations as appropriate. Months since childbirth was significantly related to EPDS (rs = −.14, p< .05), while age was correlated with PASS (rs = −.13, p< .05).
Table 2. Intercorrelations between the four variables of interest.
Moderation analyses
Depression
Moderation analysis was carried out using the SPSS PROCESS macro model 1 (Hayes, Citation2018). Variables were centred within the macro to avoid potentially problematic high multicollinearity with the interaction term. summarises the moderating effect of perceived social support when confounding variables were controlled. A significant association was found between RNT and depression (b= .221, p < .001) and social support and depression (b= −.058, p = .002). Importantly, perceived social support appeared to moderate this relationship, as there was a significant interaction effect of RNT and perceived social support on depression (b= −.004, p < .05). The total model accounted for 32.8% of the variance in the data, and including the interaction term significantly improved the model (F(1,246) = 4.64, p< .05).
Table 3. Moderating effect of MSPSS (and its subscales) on the association between RNT and postnatal depression.
Individual moderation analyses were then carried out with the three subscales of the MSPSS as moderators: i.e. family support, friends support, significant other support, respectively. While social support from each of these sources was associated with depression (significant other: b = −.137, p < .01; family: b = −.119, p = .01; friends: b = −.120, p < .05), only the moderating effect of friends’ support was statistically significant (b = −.009, p < .05).
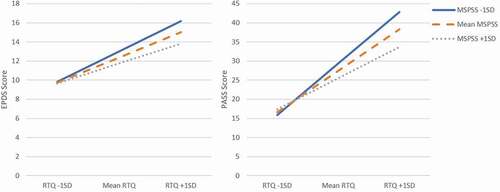
To illustrate the RNT × social support interaction for support from friends, we plotted the regression of depression on RNT at high (mean score + 1SD), medium (mean score) and low (mean score −1 SD) levels of support (see ). The relationship between RNT and depression grew stronger as perceived support weakened, such that at lower levels of RNT, the amount of support participants perceived having from friends made little difference to EPDS scores; in contrast, when participants experienced high levels of RNT, those with higher levels of support experienced lower EPDS scores than those with lower levels of support.
Anxiety
A similar moderation model was investigated with anxiety as the outcome, and age as a covariate. Findings are summarised in .
Table 4. Moderating effect of MSPSS (and its subscales) on the association between RNT and postnatal anxiety.
A significant association was found between RNT and anxiety (b = .916, p < .001). However, perceived social support did not demonstrate a moderating effect as there was no significant association between MPSS and anxiety (b = −.096, p > .05), and no interaction effect of RNT and perceived social support (b = −.008, p > .05).
Individual moderation analyses with the three subscales of the MSPSS found that neither family support nor support from significant others were associated with anxiety, nor moderated the relationship with RNT. However, as with depression, support from friends was related to anxiety (b= −.336, p = .014) and functioned as a significant moderator (b = −.041, p = .002). The RNT × social support interaction for support from friends is illustrated in . Again, participants with high levels of RNT had lower PASS scores the higher their perceived level of support, while support made little difference to PASS scores at low levels of RNT.
COVID-19 and perceived social support
Participants indicated how important different sources of support were to them during the pandemic on a scale from 1 to 5. Partners were rated as most important (mean = 4.74, SD = .60), followed by family (mean = 4.40, SD = .85), parent friends (mean = 3.98, SD = .98) and non-parent friends (mean = 3.57, SD = 1.05). Paired t-tests with Bonferroni corrections showed that all groups significantly differed from one another (all ps<.001). In these questions, the ‘friends’ category was broken down into those who were parents, and those who were not. The MSPSS does not make this distinction, yet previous research has suggested it is support from peers who also have children that is more critical to wellbeing in the perinatal period (e.g. Harrison et al., Citation2020).
Use of technology
Participants indicated the different ways in which they used technology during lockdown on a scale of 1 to 5, where high scores indicate more frequent technology usage. Correlations between the frequency of these activities, perceived social support, RNT, depression and anxiety are shown in . In order of strength, perceived support was significantly positively related to making/receiving video calls (r = .345, p < .001), traditional voice calls (r = −.337, p < .001), sending/receiving texts (r = .321, p < .001) and using technology to access parenting-related information (r = .146, p < .05). Increases in texting and video calls were also negatively associated with anxious and depressive symptoms. Additionally, increased forum use was associated with increased anxiety, depression and repetitive negative thinking, and using technology to access wellbeing information was associated with increased anxiety. In contrast, general frequency of technology use, social media use, using technology to support wellbeing, and forum use were not related to perceived support.
Table 5. Relationship between technology use, and key variables of interest (Spearman’s r reported, *p < .05, **p < .01).
Discussion
We investigated whether perceived social support played a moderating role in the relationship between RNT and postnatal wellbeing during the COVID-19 pandemic. In line with previous research (e.g. Dennis et al., Citation2017; Hetherington et al., Citation2018; Hughes et al., Citation2020; Milgrom et al., Citation2019), poor levels of perceived social support were significantly related to elevated postnatal depression and anxiety symptoms. Perceived social support was also negatively correlated with RNT, indicating that postpartum women with lower levels of support engaged in more RNT. Additionally, RNT was significantly positively related to depression and anxiety symptoms.
Moderation analyses indicated that overall perceived social support moderated the relationship between RNT and depression, in accord with O’Mahen et al. (Citation2010) who found a buffering effect of social functioning on the impact of rumination on depression in a perinatal cohort. Together, these findings highlight the importance of social relationships during this time. Interestingly, all three sources of social support (friends, family, significant other) were significantly associated with depression within the models, supporting previous work that has highlighted social support as a protective factor against depression in the postpartum period (Hetherington et al., Citation2018; Milgrom et al., Citation2019). However, only support from friends drove the moderation effect. The pattern differed for anxiety. Specifically, only support from friends was significantly related to anxiety within the models, and also acted as a moderator. Overall, these findings are in line with evidence suggesting that poor social support may negatively impact wellbeing due to an increased likelihood of rumination (Puterman et al., Citation2010). Furthermore, the present findings fit with previous evidence of perceived social support from friends, but not family, being associated with decreasing rates of anxious-depressive symptoms in the postnatal period (Hughes et al., Citation2020).
The findings are consistent with the theory that stronger social support may enhance wellbeing through a reduction in rumination (Trapnell & Campbell, Citation1999). One possible explanation is that social support acts as a buffer against the effects of RNT on wellbeing, as it may enable individuals to externalise their issues by talking them through with others, resulting in a range of potential benefits (e.g. active problem-solving, gaining an alternative perspective) which could disrupt the cycle of perseverative thinking. In contrast, in the absence of such support individuals may become ‘stuck’ in their unhelpful thoughts, potentially driving further RNT and increasing symptoms of anxiety and depression (e.g. Nolen-Hoeksema & Davis, Citation1999; Rimé, Citation1995).
Why only support from friends acted as a moderator in the relationship between RNT and psychological outcomes is unclear, especially given that women in this study reported support from partners as being most important, in general terms. Although previous research has suggested that some women find even very supportive partners sometimes struggle to understand maternal experiences (Coates et al., 2015), and women often cite support from their peers as being more fundamental to their wellbeing in the perinatal period (Harrison et al., Citation2020). For example, women often hold unrealistic expectations about motherhood, and report significant psychological distress when they are unable to live up to the fallacious notion of the ‘perfect mum’ so often portrayed by social (and mainstream) media (Coates et al., Citation2014; Djafarova & Trofimenko, Citation2017; Harrison et al., Citation2020; Law et al., Citation2018; Wardrop & Popadiuk, Citation2013). However, mothers experience significant relief when they can exchange motherhood stories with their peers, as this allows them to break down unrealistic ideals, and can explicitly lead to the realisation that they are not abnormal, inadequate or alone in their experience (Harrison et al., Citation2020). This also maps on to our finding that women rated friends who were parents as a more important source of support than friends who were not. Therefore, peer interactions (and particularly those with fellow parents) during the perinatal period may be more therapeutically powerful than social support from partners and family. This idea that women’s anxiety and distress can be ameliorated by normalising their own experiences through conversations and interactions with their peers may, therefore, be at the heart of our moderation finding. Furthermore, this finding is consistent with research that has emphasised the role of shared human experience in reducing postnatal distress (Coates et al., Citation2014; Wardrop & Popadiuk, Citation2013), and evidence linking holding unattainable high standards to postnatal anxiety and distress (Macedo et al., Citation2009; Oddo-Sommerfeld et al., Citation2016).
Sharing experiences with peers may have been particularly therapeutic during the pandemic, as rumination often occurs when there is a discrepancy between an idealised or desired state and one’s actual experience (Martin & Tesser, Citation1996). Given the significant disruption caused by COVID-19, it is likely that the discrepancies between notions of motherhood and reality were more pronounced during this time. To illustrate, our recent qualitative work (Jones et al., in Citationprep) has found that postnatal women report struggling with the ‘loss’ of their maternity leave plans owing to COVID-19 restrictions. For example, not being able to engage in mother/baby groups, attend baby-related activities, or spend time with family and friends. In a similar vein, in addition to the daily responsibilities of caring for a newborn, during the pandemic many women experienced additional stressors such as home-schooling, and the loss of childcare and domestic support. The compounding effect of these stressors – e.g. on mothers’ time and mental health – may have undermined their capacity to meet their own expectations of the ‘perfect mum’, resulting in increasing rumination and negatively impacting their wellbeing.
Implications
In line with previous research, RNT significantly predicted postnatal depression and anxiety. This finding has implications for psychological assessment and treatment in the postnatal period – suggesting the value of screening levels of RNT in new mothers, and further, that reducing RNT should be an important goal for intervention programmes designed to support postnatal wellbeing. One possibility is that recently developed brief interventions for RNT (e.g. Hirsch et al., Citation2018) could be adapted for delivery in the perinatal period, with the goal of both preventing and treating depression and anxiety. In addition, as social support from friends moderated the relationship between RNT and depression/anxiety, interventions (including preventive programmes) should emphasise the importance of maintaining social contact during the postnatal period. During lockdown, this can be done via online/digital means; for example, by encouraging regular engagement with friends through digital technologies (such as WhatsApp, FaceTime or Zoom).
Our findings suggest that some technology usage behaviours may be more effective in terms of protecting against depression and anxiety whilst in social isolation. Specifically, using technology to communicate with loved ones (via text or video calls) may be particularly helpful, while social media or internet use may not be. Furthermore, forum usage (e.g. Mumsnet) and wellbeing technology use was associated with increased anxiety and depression. While the direction of this relationship is unclear, we note that while some evidence suggests forum usage may be detrimental to perinatal mental health (Harrison et al., Citation2020), other work suggests it may be helpful (Moore et al., Citation2016). For example, a recent review of women’s use of social networking and forums in the perinatal period suggests that online social environments can provide a valuable opportunity for social interaction, promoting virtual peer bonding, and providing both emotional and instrumental aspects of support (Gleeson et al., Citation2019). Furthermore, a need to both express how they are feeling, and hear about peers’ opinions and experiences, have been highlighted as key motivators for forum engagement by perinatal women (Ellis & Roberts, Citation2020). Thus, it seems likely that anxiety and depression symptoms were driving these behaviours, and that encouraging contact with other mothers in online forums and chat rooms may increase perceived social support and promote positive maternal mental health.
Limitations
We note some limitations. First, the context (a pandemic) may limit generalisability of the results. We found elevated levels of perinatal mental health symptoms – in line with other studies during this period (Davenport et al., Citation2020; Wu et al., Citation2020) – and high levels of RNT. Further research is needed to explore whether the findings replicate post-COVID-19, and to consider their application in other situations in which postpartum women are socially isolated (e.g. during recovery from a caesarean birth). Secondly, we used self-report scales, which are subject to bias, and did not ask participants whether they had ever been diagnosed with depression or anxiety. Future work could include more objective measures (e.g. structured clinical interviews), and request information about participants’ psychological history to explore differences between persistent, recurring and incident anxiety. Finally, the self-selected sample consisted of women who were predominantly white, educated, over 25 years old and in relationships. We do not know whether the findings extend beyond this population.
Conclusions and future directions
The findings have important implications for the prevention and treatment of postnatal depression and anxiety. Given that RNT is a modifiable risk factor (Hirsch et al., Citation2018), the findings highlight the value of helping women to identify potential triggers for their RNT (e.g. mood states, contexts, challenging situations/relationships) and incorporating specific strategies to reduce RNT in existing prevention and treatment programs. Indeed, the similar pattern of findings for depression and anxiety (and significant comorbidity between these symptoms; Falah-Hassani et al., Citation2017) suggest a transdiagnotic approach may have potential clinical value – that is, using similar supportive strateiges whether clients are at risk of or are experiencing depression or anxiety, or both. In addition, our findings suggest the value of educating women about the importance of social support postpartum, and encouraging behaviours to initiate and maintain supportive links.
Consent to participate
Written consent was obtained from all participants for participation in this study.
Consent to publication
Participants all consented to their data being published in an aggregated, anonymised format.
Disclosure of interest
The authors report no conflict of interest
Ethic approval
The study received ethical approval from the Open University’s Human Research Ethics Committee.
Additional information
Funding
Notes
1. We also simultaneously recruited pregnant women as part of a second antenatal study. For the purpose of brevity and clarity, we present findings for the post-natal study only in this paper. Findings for the prenatal study are reported elsewhere.
References
- Abela, J. R. Z., Vanderbilt, E., & Rochon, A. (2004). A test of the integration of the response styles and social support theories of depression in third and seventh grade children. Journal of Social and Clinical Psychology, 23(5), 653–674. https://doi.org/10.1521/jscp.23.5.653.50752
- Barnum, S. E., Woody, M. L., & Gibb, B. E. (2013). Predicting changes in depressive symptoms from pregnancy to postpartum: The role of brooding rumination and negative inferential styles. Cognitive Therapy and Research, 37(1), 71–77. https://doi.org/10.1007/s10608-012-9456-5
- Bauer, A., Knapp, M., & Parsonage, M. (2016). Lifetime costs of perinatal anxiety and depression. Journal of Affective Disorders, 192(January), 83–90. https://doi.org/10.1016/j.jad.2015.12.005
- Biaggi, A., Conroy, S., Pawlby, S., & Pariante, C. M. (2016). Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of Affective Disorders, 191, 62–77. https://doi.org/10.1016/j.jad.2015.11.014
- Borkovec, T. D., Ray, W., & Stober, J. (1998). Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognitive Therapy and Research, 22(6), 561–576. https://doi.org/10.1023/A:1018790003416
- Brown, G. W., Andrews, B., Harris, T., Adler, Z., & Bridge, L. (1986). Social support, self-esteem and depression. Psychological medicine, 16(4), 813–831. https://doi.org/10.1017/s0033291700011831
- Coates, R., Ayers, S., & de Visser, R. (2014). Women’s experiences of postnatal distress: A qualitative study. BMC Pregnancy and Childbirth, 14(1), 359. https://doi.org/10.1186/1471-2393-14-359
- Cox, J., Holden, J., & Sagovsky, R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh postnatal depression scale. British Journal of Psychiatry, 150(6), 1–2. https://doi.org/10.1192/bjp.150.6.782
- Dambi, J.M., Corten, L., Chiwaridzo, M. et al. (2018). A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS). Health Qual Life Outcomes, 16, 80. https://doi.org/10.1186/s12955-018-0912–0
- Davenport, M. H., Meyer, S., Meah, V. L., Strynadka, M. C., & Khurana, R. (2020). Moms are not OK: COVID-19 and maternal mental health. Frontiers in Global Women’s Health, 1, 1. https://doi.org/10.3389/fgwh.2020.00001
- DeJong, H., Fox, E., & Stein, A. (2016). Rumination and postnatal depression: A systematic review and a cognitive model. Behaviour Research and Therapy, 82, 38–49. https://doi.org/10.1016/j.brat.2016.05.003
- Dennis, C.-L., Falah-Hassani, K., & Shiri, R. (2017). Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. British Journal of Psychiatry, 210(5), 315–323. https://doi.org/10.1192/bjp.bp.116.187179
- Djafarova, E., & Trofimenko, O. (2017). Exploring the relationships between self-presentation and self-esteem of mothers in social media in Russia. Computers in Human Behavior, 73, 20–27. https://doi.org/10.1016/j.chb.2017.03.021
- Ellis, L., & Roberts, L. (2020). Exploring the use and quality of Internet discussion forums in pregnancy: A qualitative analysis. Birth, 47(1), 153–161. https://doi.org/10.1111/birt.12459
- Emmanuel, E., St John, W., & Sun, J. (2012). Relationship between social support and quality of life in childbearing women during the perinatal period prevention and treatment of obessive-compulsive disorder using cognitive behaviour therapy approach view project. Journal of Obstetric Gynecologic & Neonatal Nursing, 41(6), e62. https://doi.org/10.1111/j.1552-6909.2012.01400.x
- Falah-Hassani, K., Shiri, R., & Dennis, C. L. (2017, September 1). The prevalence of antenatal and postnatal co-morbid anxiety and depression: A meta-analysis. Psychological Medicine, 47(12), 2041–2053. Cambridge University Press. https://doi.org/10.1017/S0033291717000617
- Fallon, V., Halford, J. C. G., Bennett, K. M., & Harrold, J. A. (2018). Postpartum-specific anxiety as a predictor of infant-feeding outcomes and perceptions of infant-feeding behaviours: New evidence for childbearing specific measures of mood. Archives of Women’s Mental Health, 21(2), 181–191. https://doi.org/10.1007/s00737-017-0775-0
- Fawcett, E. J., Fairbrother, N., Cox, M. L., White, I. R., & Fawcett, J. M. (2019). The prevalence of anxiety disorders during pregnancy and the postpartum period: A multivariate Bayesian meta-analysis. Journal of Clinical Psychiatry, 80, 4. https://doi.org/10.4088/JCP.18r12527
- Glasheen, C., Richardson, G. A., & Fabio, A. (2010). A systematic review of the effects of postnatal maternal anxiety on children. Archives of Women’s Mental Health, 13(1), 61–74. https://doi.org/10.1007/s00737-009-0109-y
- Gleeson, D. M., Craswell, A., & Jones, C. M. (2019, August 1). Women’s use of social networking sites related to childbearing: An integrative review. Women and Birth, 32(4), 294–302. Elsevier B.V. https://doi.org/10.1016/j.wombi.2018.10.010
- Harrison, V., Moore, D., & Lazard, L. (2020). Supporting perinatal anxiety in the digital age; A qualitative exploration of stressors and support strategies. BMC Pregnancy and Childbirth, 20(1), 1. https://doi.org/10.1186/s12884-020-02990-0
- Harrison, V., Moulds, M., & Jones, K. (2021). Perceived social support and prenatal wellbeing; the mediating effects of loneliness and repetitive negative thinking on anxiety and depression during the COVID-19 pandemic. Women and Birth: Journal of the Australian College of Midwives, S1871-5192(20)30404-2. Advance online publication. https://doi.org/10.1016/j.wombi.2020.12.014
- Hayes, A. F. (2018). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. 1. public/process2012.pdf
- Hetherington, E., McDonald, S., Williamson, T., Patten, S. B., & Tough, S. C. (2018). Social support and maternal mental health at 4 months and 1 year postpartum: Analysis from the all our families cohort. Journal of Epidemiology and Community Health, 72(10), 933–939. http://dx.doi.org/10.1136/jech-2017-210274
- Hirsch, C. R., Krahé, C., Whyte, J., Loizou, S., Bridge, L. S., Norton & Mathews, A., & Mathews, A. (2018). Interpretation training to target repetitive negative thinking in generalized anxiety disorder and depression. Journal of Consulting and Clinical Psychology, 86(12), 1017–1030. https://doi.org/10.1037/ccp0000310
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Cohen Silver, R., Everall, I., Ford, T., John, A., Kabir, T., King, K., Madan, I., Michie, S., Przybylski, A. K., Shafran, R., Sweeney, A., Yardley, L., … Bullmore, E. (2020, June 1). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. Elsevier Ltd. https://doi.org/10.1016/S2215-0366(20)30168-1
- Howard, L. M., Ryan, E. G., Trevillion, K., Anderson, F., Bick, D., Bye, A., Byford, S., O’Connor, S., Sands, P., Demilew, J., Milgrom, J., & Pickles, A. (2018). Accuracy of the Whooley questions and the Edinburgh Postnatal Depression Scale in identifying depression and other mental disorders in early pregnancy. British Journal of Psychiatry, 212(1), 50–56. https://doi.org/10.1192/bjp.2017.9
- Hughes, C., Devine, R. T., Foley, S., Ribner, A. D., Mesman, J., & Blair, C. (2020). Couples becoming parents: Trajectories for psychological distress and buffering effects of social support. Journal of Affective Disorders, 265, 372–380. https://doi.org/10.1016/j.jad.2020.01.133
- Jones, K., Harrison, V., & Moulds, M. (in prep). A qualitative analysis of feelings and experiences associated with perinatal distress during the COVID-19 pandemic.
- Law, K. H., Jackson, B., Guelfi, K., Nguyen, T., & Dimmock, J. A. (2018). Understanding and alleviating maternal postpartum distress: Perspectives from first-time mothers in Australia. Social Science & Medicine, 204, 59–66. https://doi.org/10.1016/j.socscimed.2018.03.022
- Lebel, C., MacKinnon, A., Bagshawe, M., Tomfohr-Madsen, L., & Giesbrecht, G. (2020). Elevated depression and anxiety among pregnant individuals during the COVID-19 pandemic. PsyArXiv. https://doi.org/10.31234/OSF.IO
- Lefkovics, E., Rigó, J., Kovács, I., Talabér, J., Szita, B., Kecskeméti, A., Szabó, L., Somogyvári, Z., & Baji, I. (2018). Effect of maternal depression and anxiety on mother’s perception of child and the protective role of social support. Journal of Reproductive and Infant Psychology, 36(4), 434–448. https://doi.org/10.1080/02646838.2018.1475726
- Macedo, A., Bos, S. C., Marques, M., Maia, B., Soares, M. J., Pereira, T., Gomes, A. A., Valente, J., & Azevedo, M. H. (2009). Perfectionism dimensions in pregnancy—a study in Portuguese women. Archives of Women’s Mental Health, 12(1), 43–52. https://doi.org/10.1007/s00737-008-0042-5
- Martin, L. L., & Tesser, A. (1996). Some ruminative thoughts. In R. S. Wyer (Ed.), Ruminative thoughts. Advances in social cognition (pp. 1–47). Lawrence Erlbaum Associates.
- Matthies, L. M., Wallwiener, S., Müller, M., Doster, A., Plewniok, K., Feller, S., Sohn, C., Wallwiener, M., & Reck, C. (2017). Maternal self-confidence during the first four months postpartum and its association with anxiety and early infant regulatory problems. Infant Behavior & Development, 49, 228–237. https://doi.org/10.1016/j.infbeh.2017.09.011
- McEvoy, P. M., Mahoney, A. E. J., & Moulds, M. L. (2010). Are worry, rumination, and post-event processing one and the same? Development of the repetitive thinking questionnaire. Journal of Anxiety Disorders, 24(5), 509–519. https://doi.org/10.1016/j.janxdis.2010.03.008
- McEvoy, P. M., Thibodeau, M. A., & Asmundson, G. J. G. (2014). Trait repetitive negative thinking: A brief transdiagnostic assessment. Journal of Experimental Psychopathology, 5(3), 1–17. https://doi.org/10.5127/jep.037813
- Milgrom, J., Hirshler, Y., Reece, J., Holt, C., & Gemmill, A. W. (2019). Social support—a protective factor for depressed perinatal women? International Journal of Environmental Research and Public Health, 16(8), 1426. https://doi.org/10.3390/ijerph16081426
- Moore, D., Ayers, S., & Drey, N. (2016). A thematic analysis of stigma and disclosure for perinatal depression on an online forum. JMIR Mental Health, 3(2), e18. https://doi.org/10.2196/mental.5611
- Moulds, M. L., Black, M. J., Newby, J. M., & Hirsch, C. R. (2018). Repetitive negative thinking and its role in perinatal mental health. Psychopathology, 51(3), 161–166. https://doi.org/10.1159/000488114
- Moyer, C. A., Kaselitz, E., & Muzik, M. (2020). Pregnancy-related anxiety during COVID-19: A nationwide survey of 2,740 pregnant women. https://doi.org/10.21203/rs.3.rs-37887/v1
- Netsi, E., Pearson, R. M., Murray, L., Cooper, P., Craske, M. G., & Stein, A. (2018). Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry, 75(3), 247–253. https://doi.org/10.1001/jamapsychiatry.2017.4363
- Nolen-Hoeksema, S. (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100(4), 569–582. https://doi.org/10.1037/0021-843X.100.4.569
- Nolen-Hoeksema, S., & Davis, C. G. (1999). “Thanks for sharing that”: Ruminators and their social support networks. Journal of Personality and Social Psychology, 77(4), 801–814. https://doi.org/10.1037/0022-3514.77.4.801
- Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x
- O’Connor, D. B., Aggleton, J. P., Chakrabarti, B., Cooper, C. L., Creswell, C., Dunsmuir, S., Fiske, S. T., Gathercole, S., Gough, B., Ireland, J. L., Jones, M. V., Jowett, A., Kagan, C., Karanika‐Murray, M., Kaye, L. K., Kumari, V., Lewandowsky, S., Lightman, S., Malpass, D., Morgan, B. P., … Armitage, C. J. (2020). Research priorities for the COVID‐19 pandemic and beyond: A call to action for psychological science. British Journal of Psychology, 111(4), 603–629. https://doi.org/10.1111/bjop.12468
- O’Mahen, H. A., Flynn, H. A., & Nolen-Hoeksema, S. (2010). Rumination and interpersonal functioning in perinatal depression. Journal of Social and Clinical Psychology, 29(6), 646–667. https://doi.org/10.1521/jscp.2010.29.6.646
- Oddo-Sommerfeld, S., Hain, S., Louwen, F., & Schermelleh-Engel, K. (2016). Longitudinal effects of dysfunctional perfectionism and avoidant personality style on postpartum mental disorders: Pathways through antepartum depression and anxiety. Journal of Affective Disorders, 191, 280–288. https://doi.org/10.1016/j.jad.2015.11.040
- Pedersen, S., & Lupton, D. (2018). ‘What are you feeling right now?’ communities of maternal feeling on Mumsnet. Emotion, Space and Society, 26, 57–63. https://doi.org/10.1016/j.emospa.2016.05.001
- Puterman, E., Delongis, A., & Pomaki, G. (2010). Protecting us from ourselves: Social support as a buffer of trait and state rumination. Journal of Social and Clinical Psychology, 29(7), 797–820. https://doi.org/10.1521/jscp.2010.29.7.797
- Rees, S., Channon, S., & Waters, C. S. (2019). The impact of maternal prenatal and postnatal anxiety on children’s emotional problems: A systematic review. European Child & Adolescent Psychiatry, 28(2), 257–280. https://doi.org/10.1007/s00787-018-1173-5
- Rimé, B. (1995). Mental rumination, social sharing, and the recovery from emotional exposure. In J. W. Pennebaker (Ed.), Emotion, Disclosure, & Health. (p 271–291). American Psychological Association. https://doi.org/10.1037/10182-013
- Samtani, S., & Moulds, M. L. (2017). Assessing maladaptive repetitive thought in clinical disorders: A critical review of existing measures. Clinical Psychology Review, 53, 14–28. https://doi.org/10.1016/j.cpr.2017.01.007
- Schmidt, D., Seehagen, S., Vocks, S., Schneider, S., & Teismann, T. (2016). Predictive importance of antenatal depressive rumination and worrying for maternal–foetal attachment and maternal well-being. Cognitive Therapy and Research, 40(4), 565–576. https://doi.org/10.1007/s10608-016-9759-z
- Seymour, M., Giallo, R., Cooklin, A., & Dunning, M. (2014). Maternal anxiety, risk factors and parenting in the first post-natal year. Child: Care, Health and Development, 41(2), 314–323. https://doi.org/10.1111/cch.12178
- Somerville, S., Byrne, S. L., Dedman, K., Hagan, R., Coo, S., Oxnam, E., Doherty, D., Cunningham, N., & Page, A. C. (2015). Detecting the severity of perinatal anxiety with the perinatal anxiety screening scale (PASS). Journal of Affective Disorders, 186, 18–25. https://doi.org/10.1016/j.jad.2015.07.012
- Somerville, S., Dedman, K., Hagan, R., Oxnam, E., Wettinger, M., Byrne, S., Coo, S., Doherty, D., & Page, A. C. (2014). The perinatal anxiety screening scale: Development and preliminary validation. Archives of Women’s Mental Health, 17(5), 443–454. https://doi.org/10.1007/s00737-014-0425-8
- Trapnell, P. D., & Campbell, J. D. (1999). Private self-consciousness and the five-factor model of personality: Distinguishing rumination from reflection. Journal of Personality and Social Psychology, 76(2), 284–304. https://doi.org/10.1037/0022-3514.76.2.284
- Van Bavel, J. J., Baicker, K., Boggio, P. S., Capraro, V., Cichocka, A., Cikara, M., … Willer, R. (2020, May 1). Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. Nature Research. https://doi.org/10.1038/s41562-020-0884-z
- Wardrop, A. A., & Popadiuk, N. E. (2013). The qualitative report women’ s experiences with postpartum anxiety: Expectations, relationships, and sociocultural influences recommended APA citation. The Qualitative Report, 18(3), 1–21. https://nsuworks.nova.edu/tqr/vol18/iss3/2
- Watkins, E. (2008). Constructive and unconstructive repetitive thought. Psychological Bulletin, 134(2), 163–206. https://doi.org/10.1037/0033-2909.134.2.163
- Wu, Y., Zhang, C., Liu, H., Duan, C., Li, C., Fan, J., … Huang, H. (2020). Perinatal depressive and anxiety symptoms of pregnant women along with COVID-19 outbreak in China. American Journal of Obstetrics and Gynecology. https://doi.org/10.1016/j.ajog.2020.05.009
- Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. https://doi.org/10.1207/s15327752jpa5201_2
- Zimet, G. D., Powell, S. S., Farley, G. K., Werkman, S., & Berkoff, K. A. (1990). Psychometric characteristics of the multidimensional scale of perceived social support. Journal of Personality Assessment, 55(3–4), 610–617. https://doi.org/10.1080/00223891.1990.9674095