ABSTRACT
Background
Satisfaction with the birth experience has been established to be critical for the wellbeing of the mother. The Birth Satisfaction Scale-Revised (BSS-R) is a brief and psychometrically robust multi-dimensional self-report tool designed to assess birth experience. The current investigation sought to translate and validate a Czech Republic version of the BSS-R (CZ-BSS-R).
Methods
Following translation psychometric assessment of the CZ-BSS-R was undertaken using a cross-sectional design. A between-subjects design was incorporated in order to evaluate known-groups validity evaluation of the translated measure. Four hundred and sixty-five Czech-speaking women within the Czech Republic took part in the study. Confirmatory factor analysis was undertaken and divergent and convergent validity and internal consistency characteristics also evaluated.
Results
The CZ-BSS-R was observed to have excellent psychometric properties and conceptually and measurement faithful to the original English-language measure. Consistent with previous investigations using the BSS-R significant differences were found in scores as a function of delivery type.
Conclusions
The CZ-BSS-R is a valid, robust and reliable measure of birth experience and suitable for use with Czech-speaking women in the Czech Republic. The study highlighted that instrument and emergency Caesarean section were associated with a lower level of birth satisfaction compared to vaginal delivery.
Introduction
Childbirth is one of the fundamental milestones in a woman’s life. When assessing the quality of perinatal care provision, the expert community has generally been more concerned with the physical health and safety of mother and child. However, over the last two decades, increasing attention has focused on childbearing women’s mental health, emotional security, and subjective delivery experience (Chabbert, Panagiotou, & Wendland, Citation2021; Chabbert, Rozenberg, & Wendland, Citation2021).
Larkin et al. (Citation2009) define the experience of labour and birth as an individual life event, which is influenced by social, environmental, organisational and political events, along with women’s individual life experience. Thus, the experience of childbirth is a complex construct, which is effected by a number of pre-delivery and intrapartum factors (Baguiya et al., Citation2021; Heuckendorff et al., Citation2021; Swain et al., Citation2021). Experiences of childbirth are connected with the quality of care and support provided by maternity care staff and the care provider interaction they provide, and each woman’s involvement in decision-making (Hodnett et al., Citation2002; Hollins Martin & Martin, Citation2014). The environment where the delivery takes place and support provided by the woman’s partner also impacts upon experiences of childbirth (Breman et al., Citation2019; Christiaens & Bracke, Citation2009; Mollard & Kupzyk, Citation2022; Yang et al., Citation2020). Individual influencers from the woman’ perspective, emphasis the importance and relevance of birth satisfaction (Christiaens & Bracke, Citation2007; Christiaens et al., Citation2007). Delivery satisfaction is comprised of both the woman’s emotional responses to the experience of labour and birth, and her cognitive evaluation of events. As such, birth satisfaction can be defined as a retrospective maternal evaluation of the woman’s own labour and birth events (Hollins Martin et al., Citation2012), which is influenced by many situational, cognitive and emotional factors (Preis et al., Citation2019). Levels of birth satisfaction will vary according to individual circumstances, with the woman content with some aspects of her experience and discontented with others (Lemmens et al., Citation2021).
Delivery experience and its evaluation can have long-term impact upon mother and infant well-being (Goodman et al., Citation2004; Nilver et al., Citation2017; Preis et al., Citation2019), with a positive experience associated with positive personal growth and self-respect (Goodman et al., Citation2004; Lundgren, Citation2005; Nilver et al., Citation2017). In contrast, a negative birth experience increases risk of developing post-natal depression (PND; Bell & Andersson, Citation2016), post-traumatic stress disorder (PTSD; Garthus-Niegel et al., Citation2013; Harrison et al., Citation2021), fear of future childbirth, and request for subsequent elective caesarean section (Goncu Serhatlioglu et al., Citation2018; Hildingsson et al., Citation2011; Jomeen et al., Citation2021; Nilsson et al., Citation2017).
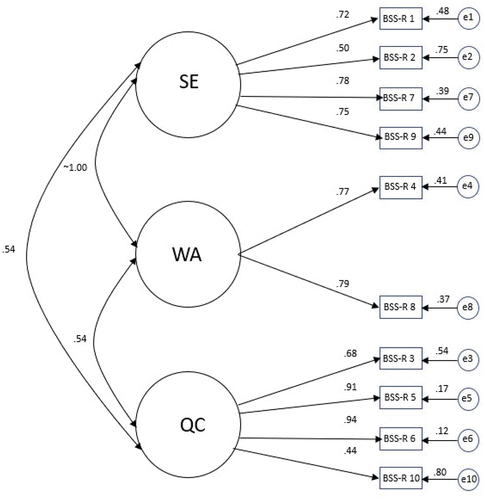
The 10-item Birth Satisfaction Scale-Revised (BSS-R) is a multi-dimensional psychometrically robust tool developed in the UK to measure women’s experiences of childbirth (Hollins Martin & Martin, Citation2014). Since its adoption by the International Consortium for Health Outcome Measurement (ICHOM) into the standard set for pregnancy and childbirth in 2016 (The International Consortium for Health Outcome Measurement, Citation2016), the BSS-R has been recommended as the key clinical measure of birth experience globally (Nijagal et al., Citation2018). The BSS-R (Hollins Martin & Martin, Citation2014) is comprised of three sub-scales, which measure distinct domains of: (1) quality of care provision (4-items), (2) women’s personal attributes (2-items), and (3) stress experienced during labour (4-items) (see, Hollins Martin & Martin, Citation2014), with each item scored on a 0–4 scale underpinned by statements that the participant circles (strongly agree, agree, neither agree or disagree, disagree, strongly disagree) and a total scale score ranging from 0–40 . Higher BSS-R scores represent greater birth satisfaction. Since development of the original UK-BSS-R (Hollins Martin & Martin, Citation2014), the scale has been validated in several country-specific translated versions (Hollins Martin & Martin, Citation2022). Validation studies (Hollins Martin & Martin, Citation2022) of the BSS-R have generally found the tool to have good-exemplary psychometric properties, which are faithful to the conceptual model of birth satisfaction outlined in the original UK study (Hollins Martin & Martin, Citation2014). This underlying measurement model of the BSS-R established and confirmed by factor analysis comprises three correlated factors related to the aforementioned sub-scales of Stress Experienced during labour (SE sub-scale), Women’s personal Attributes (WA sub-scale) and Quality of Care (QC sub-scale; Hollins Martin & Martin, Citation2014). Many previous studies examining the factor structure of the BSS-R have found a good fit to data of the BSS-R three-dimensional measurement model, for example, Barbosa-Leiker et al. (Citation2015), Nasiri et al. (Citation2020), Romero-Gonzalez et al. (Citation2019), and Skodova et al. (Citation2019). Previous investigations have also found good fit to a bifactor model, indicating the utility of the measure both in the context of a multidimensional sub-scaled index of birth experience and as a summary single total score of birth experience Emmens et al. (Citation2021), Martin et al. (Citation2018), and Nakić Radoš et al. (Citation2022).
The aim of the current investigation was to develop and validate a Czech-BSS-R for the purpose of measuring women’s experiences of childbirth in the Czech Republic. Our aim was to validate the Czech Republic-BSS-R (CZ-BSS-R) through delivering the following objectives:
Evaluate the established three-dimensional measurement model of the BSS-R in the context of the Czech Republic version.
Determine the internal consistency of CZ-BSS-R Quality of Care (QC), Women’s Attributes (WA), and Stress Experienced during Childbearing (SE) sub-scales and the total CZ-BSS-R scale.
Evaluate the known-groups discriminant validity of the CZ-BSS-R.
Determine the convergent validity of the CZ-BSS-R.
Determine the divergent validity of the CZ-BSS-R.
Evaluate differences between CZ-BSS-R scores in relation to gestational category (pre-term <37 weeks, term 37–42 weeks, post-term >42 weeks).
It is predicted that (i) the BSS-R three-dimensional measurement model will offer a good fit to data, (ii) a bifactor model of the BSS-R will offer a good fit to the data, (iii) the CZ-BSS-R scales and sub-scales will demonstrate acceptable internal consistency (iv), the CZ-BSS-R will demonstrate good known-groups discriminant validity based on groups differentiated on the basis of delivery type (v), good convergent validity with a self-perceived birth management measure (a statistically significant (p < 0.05) and negative correlation) and finally (vi), the CZ-BSS-R will demonstrate acceptable divergent validity with non-significant correlation (p > 0.05) with participant age.
Method
A retrospective cross-sectional study design was used to address the study objectives. Inclusion criteria included speaking Czech, age >18 years, having given birth within the past 12 months.
Ethical approval
Ethical approval was gained from the Ethical committee of the University of West Bohemia in Pilsen.
Translation processes of the measuring instrument
To create a Czech Republic BSS-R (CZ-BSS-R), the original UK version of the BSS-R (Hollins Martin & Martin, Citation2014) was translated into Czech language using a forward and back translation method (Brislin, Citation1970; Tyupa, Citation2011). The aim of the translation process was to create a tool that precisely expresses meaning of each English item in Czech language. First, a professional translator performed forward translation from English into Czech, with a second translator back translating items from Czech into English. Post back translation, discrepancies were discussed using an analysis of word meaning conducted within a focus group. Expert members of the focus group were bilingual and had knowledge of both English and midwifery. Within the group, the final Czech-BSS-R was compared with the Slovak-BSS-R (Skodova et al., Citation2019), because of similarity in language. In terms of translating the scale, the neutral middle point was changed from ‘neither agree nor disagree’ to ‘I do not know’, which is more matched in meaning within Czech language and a better fit with custom and culture. The comprehensibility of the CZ-BSS-R was then verified in a pilot study conducted with (n = 10) postnatal women. During this process, items were established to be unambiguously comprehensible, with no doubt concerning meaning recorded.
Data collection
The participants were recruited by means of an online survey using convenience sampling. Informed consent for study participation was embedded in the survey. The call for participation and the online questionnaire was published in four different forums for women on maternity leave in October 2021. A total number of 539 responses were recorded with 465 (86%) fully completed questionnaires included in the initial data screen and analysis.
Participants
Four-hundred and sixty-five women consented to take part in the study, and completed full questionnaire data. Mahalanobis distances were calculated to identify multivariate outliers (n = 4), and following removal, the dataset for psychometric evaluation was comprised of N = 461 participants mean age 29.81 (SD 4.82). The majority of women (n = 392; 85%) delivered at term, whereas 33 women delivered pre-term (7%). The majority of participants were married (n = 242; 52%), n = 202 (44%) were single, and a small minority divorced (n = 17; 4%). Three-hundred and twenty-seven (71%) women had a vaginal delivery and n = 134 (29%) had an intervention delivery. Ninety-nine women had a Caesarean section of which n = 33 (33%) women had an elective Caesarean section and n = 66 (67%) had an emergency Caesarean section. Three-hundred and sixteen (69%) women were nulliparous and n = 145 (31%) multiparous.
Instruments
The Birth Satisfaction Scale-Revised (BSS-R)
The BSS-R is a 10-item self-report measure of birth experience comprising three sub-scales of Stress Experienced during labour (SE sub-scale, 4-items), Women’s personal Attributes (WA sub-scale, 2-items) and Quality of Care (QC sub-scale, 4-items; Hollins Martin & Martin, Citation2014). Consistent with contemporary practice of robust self-report measures, a number of items of the BSS-R are reverse scored and greater sub-scale and total scale scores equate to greater satisfaction with the birth experience. The BSS-R can be used as a sub-scaled instrument, as a total score instrument or both depending on specific purpose of use.
Self-Perceived Birth Management (SPBM) measure
The SPBM is a single-item measure of self-perceived birth management incorporated specifically for the study as an idiom to elicit a response in everyday language. The prime was I think I managed my birth to which the responses were ‘great’, ‘well’, ‘not well’ and ‘not well at all’. Since these were scored positive to negative but with ‘great’ scored at ‘1’ and ‘not well at all’ scored at ‘4’, a higher score indicates comparatively poorer self-perceived birth management.
In addition to the BSS-R and SPBM, a questionnaire developed by researchers in accordance with the literature was used in this study. It included demographic questions and 15 semi-closed questions related to the circumstances of the birth (e.g. questions about the place of birth, the condition of the child, pain management at birth, the presence of a close person at birth).
Data analysis
Confirmatory Factor Analysis (CFA) was used to evaluate the established three-dimensional measurement model of the BSS-R. The underlying parametric assumptions of CFA require data to be distributionally normal (Brown, Citation2015). An initial screen of the dataset is thus undertaken to evaluate item skew and kurtosis, and identify and remove multivariate outliers (P. Kline, Citation2000). The underlying measurement model of the BSS-R is comprised of three correlated factors and associated sub-scales of Stress Experienced during labour (SE sub-scale), Women’s personal Attributes (WA sub-scale) and Quality of Care (QC sub-scale; Hollins Martin & Martin, Citation2014). Consistent with previous investigations of a single-factor model was also evaluated. Adopting the approach of previous studies, model estimation was by the maximum-likelihood method (R. B. Kline, Citation2011; Brown, Citation2015) and model fit determined by using the comparative fit index (CFI; Bentler, Citation1990), the root mean squared error of approximation (RMSEA; Steiger & Lind, Citation1980), and the square root mean residual (SRMR; Hu & Bentler, Citation1999). Threshold values of >0.90 (CFI), <0.08 (RMSEA) and <0.06 (SRMR) were set to determine model fit adequacy.
Internal consistency
Adopting accepted practice and threshold values (P. Kline, Citation2000), internal consistency of the CZ-BSS-R sub-scales SE and QC and total score was determined using Cronbach’s Alpha (Cronbach, Citation1951), with values of 0.70 or greater indicating acceptable internal consistency. Further, and again adopting convention and the approach of previous BSS-R validation studies, for example, Emmens et al. (Citation2021) the two-item WA sub-scale was evaluated using inter-item correlation (Pearson’s r) and adopting an acceptable threshold range of 0.15–0.50 (Clark & Watson, Citation1995). We also calculated the total scale internal consistency of the CZ-BSS-R using McDonalds Omega (ω), Omega hierarchical (ωh) and Omega total (ωt) since ω has been suggested as a better indicator of total scale internal consistency (Hayes & Coutts, Citation2020) and it has also been suggested that ωh and ωt should be reported when reporting total-scale Cronbach’s alpha (Revelle & Condon, Citation2019). Comparisons to the original Hollins Martin and Martin (Citation2014) study were made using the method of Diedenhofen and Musch (Citation2016) which is based on the Cronbach alpha sampling error theory of Feldt et al. (Citation1987) which details how Cronbach alpha estimations may be compared and statistically evaluated for statistically significant differences by reference to the chi-square distribution. Given similarity of Czech language to Slovak, a comparison was also made with the internal consistency findings of Skodova et al. (Citation2019).
Known-groups discriminant validity
Numerous validation studies, for example, Zafar et al. (Citation2021) have evaluated known-groups discriminant validity of the BSS-R, by comparing BSS-R sub-scale scores with total score, as a function of delivery type. Recent studies have investigated BSS-R score differences on the basis of CS type (elective vs. emergency) with equivocal findings (Emmens et al., Citation2021; Nakić Radoš et al., Citation2022). Type of delivery was therefore categorised into vaginal delivery, instrumental (vaginal)/vacuum delivery, elective Caesarean Section (CS) and emergency CS. One-way analysis of variance (ANOVA) was used to compared differences between these groups on CS-BSS-R sub-scale and total scores and in the event that a statistically significant main effect was observed, post-hoc testing is undertaken using the Bonferroni correction to control for Type 1 error.
One-way ANOVA was used to determine any differences in CZ-BSS-R sub-scale and total scores, as a function of gestation categorised into (pre-term, term, and post-term). Post-hoc testing is undertaken using the Bonferroni correction to control for Type 1 error. Error in the event of a statistically significant main effect being observed.
Convergent validity
Divergent validity was evaluated using correlations that compared Spearman’s rho CZ-BSS-R sub-scale and total scores, with the SPBM measure of how women believed they managed their birth.
Divergent validity
Correlation coefficients (Pearson’s r) were calculated between CZ-BSS-R total and sub-scale scores, and participant age to determine divergent validity.
Results
The descriptive and distributional characteristics of CZ-BSS-R items and scale scores are summarised in . No evidence of excessive skew or kurtosis was observed.
Table 1. Descriptive and distributional characteristics of the CZ-BSS-R.
Confirmatory factor analysis
Model 1. (unidimensional) offered a poor-fit to data (). The three-factor measurement model () offered a generally excellent fit to data across most indices, with RMSEA offering an acceptable fit (model 2). The bifactor model (model 3) revealed an excellent fit to data across all model fit indices. In terms of CFI and SRMR indices, RMSEA was found to be borderline acceptable. A strong general factor of combined SE and WA items was observed, and in addition, a separate QC factor.
Table 2. Confirmatory factor analysis and model fit of the CZ-BSS-R.
CZ-BSS-R sub-scale and total score correlations
Correlation combinations () were all observed to be statistically significant (p < 0.01). Comparison with the original UK study, using the method of Diedenhofen et al. (Citation2015), revealed a greater degree of correlation in the current study across all combinations (p < 0.05).
Table 3. Correlations of Czech bss-r sub-scales and total score and comparison with original UK BSS-R validation study.
Internal consistency
Cronbach’s alpha of CZ-BSS-R total scale and all sub-scales were acceptable (>0.70). Cronbach’s alpha of WA and QC sub-scales, and the BSS-R total scale, were significantly higher than the original UK study (). Total scale McDonalds Omega (ω), Omega hierarchical (ωh) and Omega total (ωt) were all acceptable based on threshold values detailed in the Monte Carlo simulation study of Nájera Catalán (Citation2019) at 0.88, 0.77 and 0.91, respectively. Comparison with the Slovakian study (Skodova et al., Citation2019) also revealed significantly higher WA sub-scale and total scale internal consistency estimations. Inter-item correlation of the CZ-BSS-R sub-scale WA items was r = 0.61, p < 0.001, (95% CI 0.55–0.66).
Table 4. Cronbach’s alpha of Czech BSS-R sub-scales and total score.
Known-groups discriminant validity
Highly statistically significant main effects were observed for delivery-type category across all CZ-BSS-R sub-scales and the total score (p < 0.001). Post-hoc testing revealed those having an emergency CS to have significantly lower SE, WA, QC sub-scale and total scale scores compared to elective CS and vaginal delivery groups. Women having an instrumental (vaginal)/vacuum delivery had significantly lower SE and WA sub-scale and total scale scores compared to vaginal delivery. The instrumental (vaginal)/vacuum delivery group had significantly lower SE sub-scale scores than those having an emergency CS. Effect sizes were large for the WA sub-scale and the CZ-BSS-R total score, medium for the SE sub-scale, and small for the QC sub-scale ().
Table 5. Comparison of Czech BSS-R total and sub-scale scores differentiated by delivery type.
The elective CS group was observed to have significantly higher CZ-BSS-R sub-scale and total scale scores, compared to the emergency CS group. Effect sizes were medium for all CZ-BSS-R sub-scales, and large for the total scale score.
One-way ANOVA based on gestational-term categorisation revealed significant main effect across all scales, with the exception of the QC sub-scale (). Post-hoc testing revealed signficantly higher scores in the term group compared to the post-term group on the SE sub-scale and the total score. Post-hoc differences between groups were not signficant on the WA sub-scale when the Bonferroni correction was applied to comparisons. No statisticially signficant differences were observed between pre-term and term and pre-term and post-term on any post-hoc comparisons.
Table 6. Comparison of Czech BSS-R total and sub-scale scores differentiated by term status.
Convergent validity
CZ-BSS-R total and sub-sale scores were observed to be significantly (p < 0.001) and negatively correlated, with SPBM (SE rs = −0.55, WA rs = −0.54, QC rs = −0.31, CZ-BSS-R total rs = −0.55).
Divergent validity
No significant correlations were observed between SE, WA, and QC sub-scales, and the CZ-BSS-R total score and participant age (SE r = 0.07, p = 0.12, WA r = 0.06, p = 0.19, QC r = 0.07, p = 0.11, and total scale, r = 0.08, p = 0.07).
Discussion
Our findings indicate that the CZ-BSS-R is a psychometrically robust measure and faithful to the measurement model of the original UK-BSS-R (Hollins Martin & Martin, Citation2014). The three-factor measurement model of the BSS-R offered an excellent fit to data across all fit indices confirming the transferability of the three-dimensional structure to Czech Republic language and context. The bifactor model was found to offer an excellent fit to data, again supporting the suggestion of Martin et al. (Citation2018) regarding the utility of the measure in terms of total scale or sub-scale scoring. We are reminded to reflect that although the bifactor model revealed a better fit to data than the three-dimensional model of the BSS-R, bifactor models are known to exhibit statistical bias (Burke & Johnston, Citation2020; Greene et al., Citation2019; Murray & Johnson, Citation2013) compared to other model types in terms of model fit indices, and therefore conclusions regarding bifactor model fit superiority cannot be made with confidence.
The CZ-BSS-R was observed to have good internal consistency for all sub-scales and the total scale score, thus confirming this domain of reliability and confidence in use of the measure. Correlations between BSS-R sub-scales and total scores were significantly higher than those observed in the original UK BSS-R development study (Hollins Martin & Martin, Citation2014). It may be that within the context of the social, cultural and service delivery factors that uniquely define the Czech birthing experience, there may be the potential to influence a more powerful and statistically stronger relationship between QC delivery, SE by birthing woman, and their innate attributes.
Known-groups discriminant validity analysis revealed further insights into the impact of delivery type beyond previous investigations that have shown that intervention delivery is associated with comparatively lower BSS-R scores compared to vaginal delivery (Jefford et al., Citation2018; Nespoli et al., Citation2021; Romero-Gonzalez et al., Citation2019; Skvirsky et al., Citation2020). Additionally, our findings expand on the observations of Emmens et al. (Citation2021) and Nakić Radoš et al. (Citation2022) regarding differences in BSS-R scores with respect to elective CS compared to emergency CS. No significant differences were observed between CZ-BSS-R sub-scale and total scores between women who birthed vaginally and those who had an elective CS. This highlights that even though the proportion of women having an elective CS was comparatively small in the study population, their appraisal of their birth experience was similar to those having a vaginal delivery and thus suggesting that clinical support and preparative activity for an elective CS promotes equity in terms of perceived birth experience. Women may thus suffer from psychological trauma post-emergency CS (Tomsis et al., Citation2021), which is not the case when they have had time to prepare for CS that is planned and managed (Fenwick et al., Citation2003). The Fenwick et al. (Citation2003) study also supports the importance of providing choice and control to childbearing women, which is a key premise of the concept of birth satisfaction. Also, when a woman wishes to have a Caesarean section, support and information is provided, which due to time constraints would not happen in an emergency situation (Kenyon et al., Citation2016). Clearly, an emergency CS is an unanticipated event and it can be no surprise that this has a deleterious impact on the birth experience, incorporating as it does, all aspects of subjective experience which precipitate the emergency CS.
Instrumental (vacuum)/vacuum delivery was associated with significantly lower CZ-BSS-R SE and WA sub-scale scores and the total scale score, again these findings resonate with key evidence that instrumental (vaginal) deliveries are associated with increased perceived trauma, even greater than CS (Muraca et al., Citation2017) thus a relatively impoverished birth experience may be anticipated. A vaginal delivery compared to an operative procedure such as a CS remains arguably the optimal birthing type for the mothers’ birth experience where this is possible (Guittier et al., Citation2014) and desirable by the woman herself. Our findings also support the health agenda of reducing the level of CS’s undertaken where possible (Negrini et al., Citation2021) and consistent with the woman’s choice but also extends this tenet to the reduction of instrumental (vaginal) delivery where possible.
Good convergent validity was observed with the anticipated significant and negative correlation observed between self-perceived birth management and sub-scales and the total CZ-BSS-R score. The significant correlation between the SPBM score and the QC sub-scale was the lowest observed, which corroborates the notion that the perception of ‘quality of care’ represents the woman’s insight into actual care delivered (essentially, external to the woman herself). Whereas and in contrast, the SE and WA sub-scales, may relate more to characteristics of the individual and their interaction with the environment. Good divergent validity was also found, with no statistically significant relationships observed between participants age and any of the CZ-BSS-R sub-scale or total scale scores.
It was observed that those who delivered post-term had significantly lower SE sub-scale and total CZ-BSS-R scores, compared with women who birthed at term. There is comparatively little research on post-term birth experience, compared with pre-term. Nonetheless, some explanatory accounts for these observations are now considered. For example, it may be that women in the post-term group experience increasing discomfort, which impacts upon their experience of stress. An alternative and perhaps conflating explanation might be that the woman’s expectations about birth are simply not being met. As such, this gives rise to uncertainty and stress that reduced women’s levels of birth satisfaction, specifically within the SE domain. This may be a fruitful area for further research, both to gather evidence regarding women’s perception of post-term delivery, and also to proactively consider potential interventions that reduce stress and enhance birth satisfaction. A limitation of the study is that though we noted the marital status of participants, we did not collect specific data on the partnership status of the large minority of women who were single. This omission we plan to address in future research with the CZ-BSS-R since there may well be differences in scores between single women with and those without, a partner.
Conclusion
The CZ-BSS-R was found to have excellent psychometric properties and measurement properties in terms of factor structure, consistent with the original UK version (Hollins Martin & Martin, Citation2014). Our study also corroborates observations of others, that emergency CS and instrumental (vaginal) delivery is associated with a comparatively impoverished birth experience, compared with vaginal delivery. Elective CS was found to be broadly comparable with vaginal delivery.
Availability of the BSS-R
The BSS-R is free to use for clinical and research purposes, but requires permission. Please contact Professor Caroline J Hollins Martin at [email protected] for permission to use. Also, for more information about the BSS-R, see the dedicated BSS-R website at: www.bss-r.co.uk
Acknowledgments
We would like to express our deepest gratitude to all participants who helped us conduct this study. We are also grateful for the advice, encouragement and insights of two anonymous reviewers for their excellent comments and suggestions on an earlier version of this manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Baguiya, A., Bonet, M., Cecatti, J. G., Brizuela, V., Curteanu, A., Minkauskiene, M., … group, G. R. (2021). Perinatal outcomes among births to women with infection during pregnancy. Archives of Disease in Childhood, 106(10), 946–953. https://doi.org/10.1136/archdischild-2021-321865
- Barbosa-Leiker, C., Fleming, S., Hollins Martin, C. J., & Martin, C. R. (2015). Psychometric properties of the Birth Satisfaction Scale-Revised (BSS-R) for US mothers. Journal of Reproductive and Infant Psychology, 33(5), 504–511. https://doi.org/10.1080/02646838.2015.1024211
- Bell, A. F., & Andersson, E. (2016). The birth experience and women’s postnatal depression: A systematic review. Midwifery, 39(August), 112–123. https://doi.org/10.1016/j.midw.2016.04.014
- Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. http://www.ncbi.nlm.nih.gov/pubmed/2320703.
- Breman, R. B., Storr, C. L., Paul, J., LeClair, M., & Johantgen, M. (2019). Women’s Prenatal and Labor Experiences in a Hospital With an Early-Labor Lounge. Nursing for Women’s Health, 23(4), 299–308. https://doi.org/10.1016/j.nwh.2019.05.005
- Brislin, R. W. (1970). Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology, 1(3), 185–216. https://doi.org/10.1177/135910457000100301
- Brown, T. (2015). Confirmatory factor analysis for applied research (2nd ed.). Guilford Press.
- Burke, J. D., & Johnston, O. G. (2020). The Bifactor S-1 model: A psychometrically sounder alternative to test the structure of ADHD and ODD? Journal of Abnormal Child Psychology, 48(7), 911–915. https://doi.org/10.1007/s10802-020-00645-4
- Chabbert, M., Panagiotou, D., & Wendland, J. (2021). Predictive factors of women’s subjective perception of childbirth experience: A systematic review of the literature. Journal of Reproductive and Infant Psychology, 39, 43-66. https://doi.org/10.1080/02646838.2020.1748582
- Chabbert, M., Rozenberg, P., & Wendland, J. (2021). Predictors of negative childbirth experiences among French women. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 50(4), 450–463. https://doi.org/10.1016/j.jogn.2021.02.004
- Christiaens, W., & Bracke, P. (2007). Assessment of social psychological determinants of satisfaction with childbirth in a cross-national perspective. BMC Pregnancy and Childbirth, 7(1), 26. https://doi.org/10.1186/1471-2393-7-26
- Christiaens, W., & Bracke, P. (2009). Place of birth and satisfaction with childbirth in Belgium and the Netherlands. Midwifery, 25(2), e11–19. https://doi.org/10.1016/j.midw.2007.02.001
- Christiaens, W., Gouwy, A., & Bracke, P. (2007). Does a referral from home to hospital affect satisfaction with childbirth? A cross-national comparison. BMC Health Services Research, 7(1), 109. https://doi.org/10.1186/1472-6963-7-109
- Clark, L. A., & Watson, D. (1995). Constructing validity: Basic issues in objective scale development. Psychological Assessment, 7(3), 309–319. https://doi.org/10.1037/1040-3590.7.3.309
- Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–334. https://doi.org/10.1007/BF02310555
- Diedenhofen, B., Musch, J., & . (2015). cocor: A comprehensive solution for the statistical comparison of correlations. PloS One, 10(4), e0121945. https://doi.org/10.1371/journal.pone.0121945
- Diedenhofen, B., & Musch, J. (2016). cocron: A web interface and R package for the statistical comparison of Cronbach’s alpha coefficients. International Journal of Internet Science, 11(1), 51–60.
- Emmens, B., Hollins Martin, C. J., & Martin, C. R. (2021). Translation and validation of the Dutch version of the Birth Satisfaction Scale-Revised (BSS-R). Journal of Reproductive and Infant Psychology, 1–15. https://doi.org/10.1080/02646838.2021.1979200
- Feldt, L. S., Woodruff, D. J., & Salih, F. A. (1987). Statistical Inference for Coefficient Alpha. Applied Psychological Measurement, 11(1), 93–103. https://doi.org/10.1177/014662168701100107
- Fenwick, J., Gamble, J., & Mawson, J. (2003). Women’s experiences of Caesarean section and vaginal birth after Caesarian: A Birthrites initiative. International Journal of Nursing Practice, 9(1), 10–17. https://www.ncbi.nlm.nih.gov/pubmed/12588615.
- Garthus-Niegel, S., von Soest, T., Vollrath, M. E., & Eberhard-Gran, M. (2013). The impact of subjective birth experiences on post-traumatic stress symptoms: A longitudinal study. Archives of Women’s Mental Health, 16(1), 1–10. https://doi.org/10.1007/s00737-012-0301-3
- Goncu Serhatlioglu, S., Karahan, N., Hollins Martin, C. J., & Martin, C. R. (2018). Construct and content validity of the Turkish Birth Satisfaction Scale - Revised (T-BSS-R). Journal of Reproductive and Infant Psychology, 36(3), 235–245. https://doi.org/10.1080/02646838.2018.1443322
- Goodman, P., Mackey, M. C., & Tavakoli, A. S. (2004). Factors related to childbirth satisfaction. Journal of Advanced Nursing, 46(2), 212–219. https://doi.org/10.1111/j.1365-2648.2003.02981.x
- Greene, A. L., Eaton, N. R., Li, K., Forbes, M. K., Krueger, R. F., Markon, K. E., Waldman, I. D., Cicero, D. C., Conway, C. C., Docherty, A. R., Fried, E. I., Ivanova, M. Y., Jonas, K. G., Latzman, R. D., Patrick, C. J., Reininghaus, U., Tackett, J. L., Wright, A. G. C., & Kotov, R. (2019). Are fit indices used to test psychopathology structure biased? A simulation study. Journal of Abnormal Psychology, 128(7), 740–764. https://doi.org/10.1037/abn0000434
- Guittier, M. J., Cedraschi, C., Jamei, N., Boulvain, M., & Guillemin, F. (2014). Impact of mode of delivery on the birth experience in first-time mothers: A qualitative study. BMC Pregnancy and Childbirth, 14(1), 254. https://doi.org/10.1186/1471-2393-14-254
- Harrison, S. E., Ayers, S., Quigley, M. A., Stein, A., & Alderdice, F. (2021). Prevalence and factors associated with postpartum posttraumatic stress in a population-based maternity survey in England. Journal of Affective Disorders, 279, 749–756. https://doi.org/10.1016/j.jad.2020.11.102
- Hayes, A. F., & Coutts, J. J. (2020). Use omega rather than cronbach’s alpha for estimating reliability. But. Communication Methods and Measures, 14(1), 1–24. https://doi.org/10.1080/19312458.2020.1718629
- Heuckendorff, S., Christensen, L. F., Fonager, K., & Overgaard, C. (2021). Risk of adverse perinatal outcomes in infants born to mothers with mental health conditions. Acta Obstetricia et Gynecologica Scandinavica, 100(11), 2019–2028. https://doi.org/10.1111/aogs.14241
- Hildingsson, I., Nilsson, C., Karlstrom, A., & Lundgren, I. (2011). A longitudinal survey of childbirth-related fear and associated factors. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 40(5), 532–543. https://doi.org/10.1111/j.1552-6909.2011.01274.x
- Hodnett, E. D., Lowe, N. K., Hannah, M. E., Willan, A. R., Stevens, B., & Weston, J. A., & Nursing Supportive Care in Labor Trial, G. (2002). Effectiveness of nurses as providers of birth labor support in North American hospitals: A randomized controlled trial. JAMA, 288(11), 1373–1381. h ttps://d oi.org/1 0.1001/jama.288.11.1373
- Hollins Martin, C. J., & Martin, C. R. (2014). Development and psychometric properties of the Birth Satisfaction Scale-Revised (BSS-R). Midwifery, 30(6), 610–619. https://doi.org/10.1016/j.midw.2013.10.006
- Hollins Martin, C. J., & Martin, C. R. (2022). The Birth Satisfaction Scale-Revised (BSS-R). https://www.bss-r.co.uk/
- Hollins Martin, C. J., Snowden, A., & Martin, C. R. (2012). Concurrent analysis: Validation of the domains within the Birth Satisfaction Scale. Journal of Reproductive and Infant Psychology, 30(3), 247–260. https://doi.org/10.1080/02646838.2012.710833
- Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
- The International Consortium for Health Outcome Measurement. (2016). Pregnancy and childbirth standard set and reference guide. http://www.ichom.org/medical-conditions/pregnancy-and-childbirth/
- Jefford, E., Hollins Martin, C. J., & Martin, C. R. (2018). Development and validation of the Australian version of the Birth Satisfaction Scale-Revised (BSS-R). Journal of Reproductive and Infant Psychology, 36(1), 42–58. https://doi.org/10.1080/02646838.2017.1396302
- Jomeen, J., Martin, C. R., Jones, C., Marshall, C., Ayers, S., Burt, K., Frodsham, L., Horsch, A., Midwinter, D., O’Connell, M., Shakespeare, J., Sheen, K., & Thomson, G. (2021). Tokophobia and fear of birth: A workshop consensus statement on current issues and recommendations for future research. Journal of Reproductive and Infant Psychology, 39(1), 2–15. https://doi.org/10.1080/02646838.2020.1843908
- Kenyon, S. L., Johns, N., Duggal, S., Hewston, R., & Gale, N. (2016). Improving the care pathway for women who request Caesarean section: An experience-based co-design study. BMC Pregnancy and Childbirth, 16(1), 348. https://doi.org/10.1186/s12884-016-1134-2
- Kline, P. (2000). A Psychometrics Primer. Free Association Books.
- Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd ed.). Guilford Press.
- Larkin, P., Begley, C. M., & Devane, D. (2009). Women’s experiences of labour and birth: An evolutionary concept analysis. Midwifery, 25(2), e49–59. https://doi.org/10.1016/j.midw.2007.07.010
- Lemmens, S. M. P., van Montfort, P., Meertens, L. J. E., Spaanderman, M. E. A., Smits, L. J. M., de Vries, R. G., & Scheepers, H. C. J. (2021). Perinatal factors related to pregnancy and childbirth satisfaction: A prospective cohort study. Journal of Psychosomatic Obstetrics and Gynaecology, 42(3), 181–189. https://doi.org/10.1080/0167482X.2019.1708894
- Lundgren, I. (2005). Swedish women’s experience of childbirth 2 years after birth. Midwifery, 21(4), 346–354. https://doi.org/10.1016/j.midw.2005.01.001
- Martin, C. R., Hollins Martin, C. J., Burduli, E., Barbosa-Leiker, C., Donovan-Batson, C., & Fleming, S. E. (2018). The Birth Satisfaction Scale - Revised (BSS-R): Should the subscale scores or the total score be used? Journal of Reproductive and Infant Psychology, 36(5), 530–535. https://doi.org/10.1080/02646838.2018.1490498
- Mollard, E., & Kupzyk, K. (2022). Birth Satisfaction During the Early Months of the COVID-19 Pandemic in the United States. MCN: American Journal of Maternal Child Nursing, 47(1), 6–12. https://doi.org/10.1097/NMC.0000000000000777
- Muraca, G. M., Sabr, Y., Lisonkova, S., Skoll, A., Brant, R., Cundiff, G. W., & Joseph, K. S. (2017). Perinatal and maternal morbidity and mortality after attempted operative vaginal delivery at midpelvic station. CMAJ: Canadian Medical Association Journal, 189(22), E764–E772. https://doi.org/10.1503/cmaj.161156
- Murray, A. L., & Johnson, W. (2013). The limitations of model fit in comparing the bi-factor versus higher-order models of human cognitive ability structure. Intelligence, 41(5), 407–422. d oi:h ttps://doi.org/1 0.1016/j.intell.2013.06.004
- Nájera Catalán, H. E. (2019). Reliability, population classification and weighting in multidimensional poverty measurement: A monte carlo study. Social Indicators Research, 142(3), 887–910. https://doi.org/10.1007/s11205-018-1950-z
- Nakić Radoš, S., Matijaš, M., Brekalo, M., Hollins Martin, C. J., & Martin, C. R. (2022). Further validation of the birth satisfaction scale-revised: Factor structure, validity, and reliability. Current Psychology. https://doi.org/10.1007/s12144-021-02688-2
- Nasiri, S., Kariman, N., & Ozgoli, G. (2020). Psychometric properties of the Iranian version of Birth Satisfaction Scale-Revised. Journal of Research in Medical Sciences, 25(1), 90. https://doi.org/10.4103/jrms.JRMS_248_19
- Negrini, R., D’albuquerque, I., de Cassia Sanchez, E. O. R., Ferreira, R., De Stefani, L. F. B., & Podgaec, S. (2021). Strategies to reduce the caesarean section rate in a private hospital and their impact. BMJ Open Quality, 10(3), e001215. https://doi.org/10.1136/bmjoq-2020-001215
- Nespoli, A., Colciago, E., Fumagalli, S., Locatelli, A., Hollins Martin, C. J., & Martin, C. R. (2021). Validation and factor structure of the Italian version of the Birth Satisfaction Scale-Revised (BSS-R). Journal of Reproductive and Infant Psychology, 39(5), 516–531. https://doi.org/10.1080/02646838.2020.1836333
- Nijagal, M. A., Wissig, S., Stowell, C., Olson, E., Amer-Wahlin, I., Bonsel, G., Brooks, A., Coleman, M., Devi Karalasingam, S., Duffy, J. M. N., Flanagan, T., Gebhardt, S., Greene, M. E., Groenendaal, F., R Jeganathan, J. R., Kowaliw, T., Lamain-de-ruiter, M., Main, E., Owens, M., … Franx, A. (2018). Standardized outcome measures for pregnancy and childbirth, an ICHOM proposal. BMC Health Services Research, 18(1), 953. https://doi.org/10.1186/s12913-018-3732-3
- Nilsson, C., Lalor, J., Begley, C., Carroll, M., Gross, M. M., Grylka-Baeschlin, S., Lundgren, I., Matterne, A., Morano, S., Nicoletti, J., & Healy, P. (2017). Vaginal birth after caesarean: Views of women from countries with low VBAC rates. Women and Birth, 30(6), 481–490. https://doi.org/10.1016/j.wombi.2017.04.009
- Nilver, H., Begley, C., & Berg, M. (2017). Measuring women’s childbirth experiences: A systematic review for identification and analysis of validated instruments. BMC Pregnancy and Childbirth, 17(1), 203. https://doi.org/10.1186/s12884-017-1356-y
- Preis, H., Eisner, M., Chen, R., & Benyamini, Y. (2019). First-time mothers’ birth beliefs, preferences, and actual birth: A longitudinal observational study. Women and Birth, 32(1), e110–e117. https://doi.org/10.1016/j.wombi.2018.04.019
- Revelle, W., & Condon, D. M. (2019). Reliability from α to ω: A tutorial. Psychological Assessment, 31(12), 1395–1411. https://doi.org/10.1037/pas0000754
- Romero-Gonzalez, B., Peralta-Ramirez, M. I., Caparros-Gonzalez, R. A., Cambil-Ledesma, A., Hollins Martin, C. J., & Martin, C. R. (2019). Spanish validation and factor structure of the Birth Satisfaction Scale-Revised (BSS-R). Midwifery, 70, 31–37. https://doi.org/10.1016/j.midw.2018.12.009
- Skodova, Z., Nepelova, Z., Grendar, M., & Baskova, M. (2019). Psychometric properties of the Slovak version of the Birth Satisfaction Scale (BSS) and Birth Satisfaction Scale-Revised (BSS-R). Midwifery, 79(December), 102550. https://doi.org/10.1016/j.midw.2019.102550
- Skvirsky, V., Taubman-Ben-Ari, O., Hollins Martin, C. J., & Martin, C. R. (2020). Validation of the Hebrew Birth Satisfaction Scale - Revised (BSS-R) and its relationship to perceived traumatic labour. Journal of Reproductive and Infant Psychology, 38(2), 214–220. https://doi.org/10.1080/02646838.2019.1600666
- Steiger, J. H., & Lind, J. (1980). Statistically-based tests for the number of common factors. Paper presented at the Annual Spring Meeting of the Psychometric Society, Iowa City, USA.
- Swain, D., Begum, J., & Parida, S. P. (2021). Effect of preconception care intervention on maternal nutritional status and birth outcome in a low-resource setting: Proposal for a nonrandomized controlled trial. JMIR Research Protocols, 10(8), e28148. https://doi.org/10.2196/28148
- Tomsis, Y., Perez, E., Sharabi, L., Shaked, M., Haze, S., & Hadid, S. (2021). Postpartum post-traumatic stress symptoms following cesarean section-the mediating effect of sense of control. Psychiatric Quarterly, 92(4), 1839–1853. https://doi.org/10.1007/s11126-021-09949-0
- Tyupa, S. (2011). A theoretical framework for back-translation as a quality assessment tool. New Voices in Translation Studies, 7, 35–46.
- Yang, X., Ke, S., & Gao, L. L. (2020). Social support, parental role competence and satisfaction among Chinese mothers and fathers in the early postpartum period: A cross-sectional study. Women and Birth, 33(3), e280–e285. https://doi.org/10.1016/j.wombi.2019.06.009
- Zafar, S., Tayyab, F., Liaqat, A., Sikander, S., Hollins Martin, C. J., & Martin, C. R. (2021). Translation and validation of the Birth Satisfaction Scale-Revised in Urdu for use in Pakistan. International Journal of Childbirth, 11(2), 72–83. https://doi.org/10.1891/ijcbirth-d-21-00001