Abstract
Objective: The aim of this study was to compare the treatment outcomes of ultrasound-guided high-intensity focused ultrasound (USgHIFU) for uterine fibroids in patients with an anteverted uterus versus a retroverted uterus.
Materials and methods: Based on the principles of statistics we enrolled 221patients with an anteverted uterus and 221 with a retroverted uterus. All patients had a solitary uterine fibroid and every fibroid was identified as hypointense on the T2 weighted images (T2WI) on magnetic resonance. The baseline characteristics of the patients, treatment results and adverse events were compared between the two groups.
Results: There were no significant differences in baseline characteristics between the two groups. The average non-perfused volume ratio of fibroids was 85.2 ± 18.7% in the group of patients with a retroverted uterus, while it was 87.7 ± 11.8% in patients with an anteverted uterus (P < 0.05). The fibroids in patients with a retroverted uterus were treated using lower sonication power and longer sonication time. During the procedure patients with a retroverted uterus had a higher incidence of sciatic/buttock pain and groin pain, while patients with an anteverted uterus complained of lower abdominal pain or a burning sensation on the skin. Immediately after USgHIFU, the rates of sciatic/buttock pain and skin burn were significantly higher in patients with a retroverted uterus.
Conclusion: The results of this study indicated that uterine fibroids with hypointensity on T2WI in a retroverted uterus can be safely and effectively treated with USgHIFU. However, the fibroids in an anteverted uterus are easier to treat with USgHIFU.
Introduction
Uterine fibroids or leiomyomas are the most common benign tumours of the female genital tract found in gynaecological practice. These benign tumours are diagnosed in 20–25% of women of reproductive age and 30–40% of women greater than 40 years of age [Citation1,Citation2]. Fibroid-related symptoms were observed in almost half of these patients [Citation3].
Currently, the mainstream treatment of uterine fibroids is surgery. However, surgical treatment has a relatively high impact on patient lifestyle. In an effort to reduce this impact and decrease other effects (such as the cost of surgical procedures), several less invasive treatment modalities including uterine artery embolisation (UAE), radiofrequency ablation (RFA), and high intensity focused ultrasound (HIFU) ablation have been used in the management of uterine fibroids [Citation4–6]. In particular, over the last 10 years, many studies have confirmed that HIFU can be used safely and effectively to treat patients with uterine fibroids; it also has long-term sustained symptom relief, which is associated with the non-perfused volume (NPV) ratio of the fibroids [Citation7,Citation8]. Several studies have demonstrated that ultrasound-guided HIFU (USgHIFU) can safely achieve a large NPV ratio [Citation9–11]. In many gynaecological centres in China this non-invasive treatment has become a routine option for patients with uterine fibroids.
In earlier studies with magnetic resonance imaging guided focused ultrasound surgery (MRgFUS) for the treatment of uterine fibroids, patients with bowel lying anterior to the uterus were excluded because a clear acoustic pathway is required during HIFU treatment [Citation12,Citation13]. Later, Zhang et al. [Citation14] successfully treated these patients with MRgHIFU using a degassed water balloon placed on the anterior abdominal wall to compress or push away the bowel lying anterior to the uterus. In clinical practice we find many patients with uterine fibroids had a retroverted uterus and the bowel lies anterior to the uterus. To the best of our knowledge, no study has compared HIFU treatment results between patients with an anteverted uterus and patients with a retroverted uterus. The purpose of this study was to investigate whether large NPV ratios of fibroids could be safely achieved in patients with a retroverted uterus and to compare these results to those of patients with an anteverted uterus.
Materials and methods
The ethics committee at Suining Central Hospital approved this retrospective study and every patient signed an informed consent form before the USgHIFU procedure.
Patients
In total 442 patients with hypointense T2 weighted MR image solitary uterine fibroids were enrolled. The determination of whether each patient had an anteverted or a retroverted uterus was first made by a screening MR and a simulation on a HIFU table before HIFU treatment, then it was reassessed on treatment day. On treatment day 16 patients were reclassified from retroverted to anteverted, while 11 were re-classified from anteverted to retroverted. Among them, 221 patients had an anteverted uterus and 221 patients had a retroverted uterus. The USgHIFU was performed between November 2011 and December 2015 in the HIFU unit of Suining Central Hospital.
The diagnosis of uterine fibroids was made through clinical examination, ultrasound (US) and magnetic resonance imaging (MRI).
The inclusion criteria were as follows: 1) patients were premenopausal and at least 18 years of age, 2) patients agreed to have MRI examinations before and after USgHIFU treatment, 3) patients had solitary uterine fibroids and the fibroids presented with hypointensity on T2 weighted imaging (T2WI) of an MRI.
Exclusion criteria included 1) patients with uterine fibroids presenting as isointensity or hyperintensity on T2WI, 2) patients with multiple fibroids, 3) patients with suspected or confirmed malignant diseases.
Pre-treatment preparation
To avoid the unique adverse effects and complications of HIFU, patients were instructed on the strict preparations required before USgHIFU treatment.
Preparation of the bowel was performed as follows: the patient had to follow a bland diet on day 1, a semi-liquid diet on day 2 and liquid diet (without milk) on day 3. In addition, the patient had to fast 12 h pretreatment and have an enema on the morning of the treatment. Skin preparation included shaving hair from the umbilicus to the upper margin of the pubic symphysis, degreasing with 75% ethanol and degassing with degassed water.
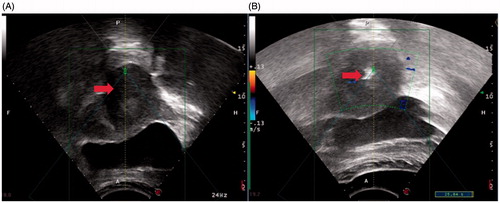
The therapeutic acoustic window was improved by adjusting the volume of fluid in the bladder. This was achieved by inserting a urinary catheter. The bladder could thus be filled with normal saline, or urine could be released. In general, 350–500 mL of normal saline was used to fill the bladder of the patients with a retroverted uterus (), while 150–250 mL of normal saline was sufficient to fill the bladder of patients with an anteverted uterus (). Degassed water balloons of various sizes and tensions were applied to every patient to compress or push away the bowel from the acoustic pathway.
Figure 1. Monitoring ultrasound images obtained from a 42-year-old patient with an anteverted uterus. The bladder was filled with 150 mL of normal saline. (A) Pre-HIFU ultrasound image showed a 4.3 × 4.0 × 3.8 cm uterine fibroid located at the anterior wall of the uterus (arrow). (B) Intra-HIFU ultrasound image showed a significant greyscale change area in the fibroids (arrow).
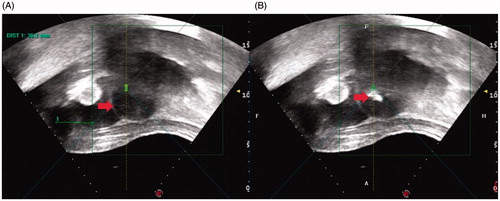
Figure 2. Monitoring ultrasound images obtained from a 39-year-old patient with a retroverted uterus. The bladder was filled with 300 mL of normal saline and lay between the uterus and abdominal wall. (A) Pre-HIFU ultrasound image showed a 4.1 × 3.9 × 3.8 cm of uterine fibroid located at the posterior wall of the uterus (arrow). (B) Intra-HIFU ultrasound image showed a significant greyscale change area in the fibroids (arrow).
USgHIFU ablation
USgHIFU ablation was performed using an ultrasound-compatible HIFU tumour therapeutic system (JC200, Haifu® Technology, Chongqing, China). This system is equipped with a therapeutic focused ultrasound transducer of 20 cm diameter and a focal length of 15 cm. A B-mode ultrasound diagnostic probe sits at the centre of the therapeutic transducer and is used to monitor the ablation process. The patients were carefully placed in a prone position on the HIFU table with the anterior abdominal wall immersed in degassed water. HIFU treatment was performed using intravenous conscious sedation. Patients received 50–400 μg of fentanyl and 1–4 mg of midazolam hydrochloride to minimise discomfort and to prevent unnecessary body movement.
Sagittal ultrasound scanning mode was used for observing the positional relationship between the uterine lesion and the bladder. The applied ultrasound had a frequency of 1.0 MHz, an oval focal point with width 3 mm and length 8 mm, a pulse with a sonication time of 1–2 s, and an interval time of 3–6 s. An acoustic power of 350–400 W was used. When a significant greyscale change was observed or sufficient thermal dosage was reached the focal point was moved to the next location. This procedure was used to achieve complete ablation of the planned treatment volume (). There was 5 mm distance between the spots, lines and layers. All HIFU treatments were administered with a margin of 5 mm from the fibroid surface in order to prevent thermal damage to the adjacent endometrium or myometrium.
During treatment the respiration, heart rate, blood pressure and oxygen saturation levels were monitored using an ambulatory electrocardiogram monitor. Contrast-enhanced ultrasound (CEU) was performed before, during and immediately after the procedure of USgHIFU to assess the therapeutic results. The contrast agent used was SonoVue (25 mg, Bracco, Milan, Italy) which was reconstituted using 5 mL of normal saline; 2 mL of SonoVue (10 mg) was injected intravenously each time. Two experienced radiologists analysed the results of CEU independently.
Pre- and post-USgHIFU MR imaging
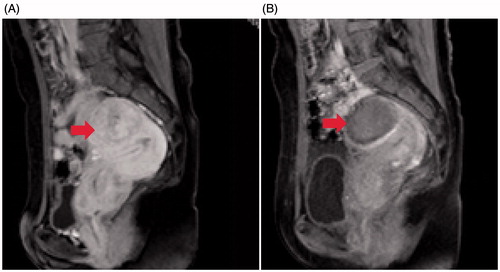
All patients were examined using contrast-enhanced MRI (Siemens Healthcare, Erlangen, Germany) before USgHIFU treatment to confirm the diagnosis, determine the intensity of fibroids on T2WI, the location of the fibroids, and the location of the uterus. NPV of the fibroid (defined as the volume that was not enhanced in the contrast-enhanced MRI) was measured post-HIFU treatment ( and ). Two senior radiologists evaluated all MR images independently.
Figure 3. Contrast-enhanced MR images obtained from a patient with an anteverted uterus. (A) A pre-procedure contrast-enhanced MR image showed a 8.0 × 6.8 × 6.7 cm fibroid located at the anterior wall of the uterus (arrow). (B) Contrast-enhanced MRI obtained 1 day after HIFU showed the non-perfused volume ratio was 91% (arrow).
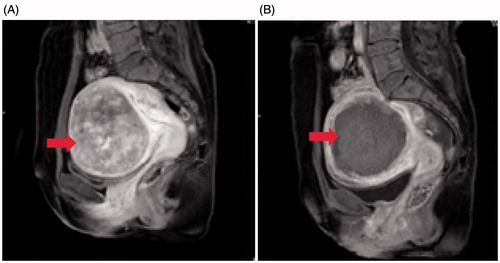
Figure 4. Contrast-enhanced MR images obtained from a patient with a retroverted uterus. (A) A pre-procedure contrast-enhanced MR image showed a 4.1 × 3.8 × 3.7 cm fibroid located at the anterior wall of the uterus (arrow). (B) Contrast-enhanced MRI obtained 1 day after HIFU showed the non-perfused volume ratio was 100% (arrow).
Safety assessments
HIFU-related adverse events, including any skin discomfort, lower abdominal pain, leg pain, sciatic or buttock pain, and vaginal discharge or bleeding were recorded.
Statistical analysis
All data was analysed using SPSS 17.0 (SPSS, IBM, Armonk, NY, USA). Data was recorded as means ± standard deviations (SD). The Wilcoxon test and chi-square test were applied for the analysis of the quantitative and enumerated data. ANOVA analysis was also applied when comparing variables between the two groups. A P value of less than 0.05 was considered to indicate a significant difference.
Results
Baseline characteristics of patients with uterine fibroids
shows that the average age was 41.5 ± 6.1 years in the group of anteverted uterus patients with uterine fibroids and 41.8 ± 5.8 years in the group with a retroverted uterus. Based on MR images, the average diameter and volume of fibroids were 3.8 ± 1.4 cm (range 2.0–8.0 cm) and 33.7 ± 40.0 cm3 respectively in the anteverted uterus group, while they were 3.7 ± 1.3 cm (range 2.0–7.9 cm) and 31.6 ± 35.2 cm3 in the retroverted uterus group. No significant differences in baseline characteristics between the two groups were observed (P > 0.05).
Table 1. Baseline characteristics of 442 patients with a solitary uterine fibroid in either an anteverted uterus or a retroverted uterus. Data are numbers or mean value ± SD. No significant difference was observed between the two groups (P > 0.05).
Evaluation of USgHIFU ablation
showed that the sonication power used to treat uterine fibroids in a retroverted uterus was significantly lower than that used in an anteverted uterus (P < 0.05). When using similar sonication time, sonication time/h, and room time, the total energy used to treat the fibroids in a retroverted uterus was significantly less than that of fibroids in an anteverted uterus (P < 0.05). Although the NPV ratio of uterine fibroids in the retroverted uterus group was significantly lower than that of the anteverted uterus group (87.7 ± 11.8% versus 85.2 ± 18.7%, P < 0.05), 85.2 ± 18.7% for the NPV ratio of fibroids obtained in the retroverted uterus group was still high.
Table 2. Treatment results of HIFU for patients with fibroids in an anteverted uterus or a retroverted uterus.
Safety evaluation
Since USgHIFU ablation was performed under conscious sedation, the patients could communicate with a nurse or physician during the procedure. shows the common adverse events during HIFU ablation included transient leg pain, sciatic or buttock pain, lower abnormal pain, a burning skin sensation, and groin pain. The sciatic or buttock pain and groin pain were seen more frequently in the group of patients with a retroverted uterus; while lower abdominal pain and the burning skin sensation were more often encountered in the group of patients with an anteverted uterus (P < 0.05).
Table 3. Incidence rates of adverse effects during the HIFU procedure. No significant difference was observed between the two groups (P > 0.05).
Immediately after USgHIFU treatment, most of the pain that patients experienced during the procedure subsided. shows the common post-treatment adverse effects included lower abdominal pain, sciatic/buttock pain, and vaginal discharge. No significant difference was observed between the two groups regarding lower abdominal pain and vaginal discharge. The rate of lower abdominal pain was 17.2% in the anteverted uterus group of patients, and it was 19.5% in the retroverted uterus group of patients. The rate of vaginal discharge was 5.0% for the anteverted uterus patients, and it was 7.2% in the retroverted uterus patients. Significant differences were observed between the two groups in the occurrence of sciatic/buttock pain, leg pain, and skin burn. The rate of sciatic/buttock pain was significantly higher in the patients with a retroverted uterus than that of patients with an anteverted uterus (14.0% versus 4.5%, P < 0.05). In this study no skin burn occurred in the patients with an anteverted uterus, but five, patients (2.3%) in the group with a retroverted uterus had skin burns (P < 0.05). One patient in the retroverted uterus group complained of leg pain; no patients complained of leg pain in the anteverted uterus group. No patients reported fever, bladder injury or urinary retention in either group.
Table 4. Incidence rates of adverse effects and complications immediately after HIFU treatment. Skin burn was observed in five (2.3%) patients with a retroverted uterus; Resection was performed in two of them. One patient with a retroverted uterus reported leg pain.
Discussion
Uterine fibroids or leiomyomas consist mainly of smooth muscle cells and different amounts of fibrous tissue [Citation1,Citation15]. Based on their varying histological features, they are classified as typical fibroids/leiomyomas, cellular fibroids/leiomyomas, bizarre fibroids/leiomyomas and lipoleiomyomas. On T2 weighted MR images these fibroids presented as hypointense, isointense, or hyperintense signals, respectively [Citation16]. Earlier studies have shown that fibroids with hypointensity or isointensity are easier to treat with HIFU than those with hyperintensity [Citation9,Citation17]. In order to compare the therapeutic results of patients with an anteverted uterus to patients with a retroverted uterus we enrolled patients with similar baseline characteristics. Although Zhao et al. [Citation9] have demonstrated that fibroids with hyperintensity can also be effectively treated with USgHIFU, we only enrolled patients with hypointense fibroids in this study. The results of this study showed that a NPV ratio of 85.2 ± 18.7% was achieved in patients with a retroverted uterus and 87.7 ± 11.8% in anteverted uterus patients. Previous studies have shown that achieving large NPV ratios could provide long-term symptom relief and decrease the rate of re-intervention [Citation7,Citation8]. Although the NPV ratio of fibroids in the patients with a retroverted uterus was significantly lower than that of patients with an anteverted uterus, it was still higher than that in previous publications [Citation9–11]. Thus our results indicated that USgHIFU treatment is effective in treating uterine fibroids in patients with a retroverted uterus.
Treatment time and sonication time are practical concerns. In this study, the average treatment time (defined as the duration from the first sonication to the last sonication) was 1 h and the average sonication time was around 520 s. No significant differences were observed between the groups (P > 0.05). In patients with a retroverted uterus the bowel was located anterior to the uterus. To create a better acoustic window the bladder was filled with 350–500 mL of normal saline and a degassed water balloon was placed on the abdominal wall to compress or move the bowel out of the way; the uterus is thus pushed closer to the sacrum and during treatment these patients frequently reported sciatic or buttock pain. To decrease the pain the sonication power used was significantly lower in patients with a retroverted uterus than that used for patients with an anteverted uterus. Although all patients received similar sonication time, the average energy delivered to the fibroids in the retroverted uterus group was significantly less than that for the anteverted uterus group. In clinical practice it was found that many factors influenced the NPV ratio of the fibroids. Peng et al. [Citation18] demonstrated that the distance from the ventral surface of the fibroid to the skin, enhancement type on T1WI, size of uterine fibroid, and signal intensity on T2WI are key factors and can be used as dosimetric predictors of HIFU treatment for uterine fibroids. However, in this study the smaller NPV ratio was more likely caused by less acoustic energy being delivered. Using lower power with longer sonication time, a larger NPV ratio could be achieved.
Safety is always a major concern in the management of uterine fibroids. USgHIFU is a non-invasive treatment modality and the procedure is performed under conscious sedation so patients could report any pain or discomfort including leg, sciatic/buttock or lower abdominal pain, deep abdominal pain at the treated region, and burning skin sensation during the procedure. The HIFU-related adverse effects are often mild and transient. In this study we found more patients with a retroverted uterus complained of sciatic pain/buttock pain and/or groin pain (). This phenomenon could potentially be explained by the location of the uterus adjacent to the sacrum. Lower abdominal pain and burning skin sensation were more often observed in patients with an anteverted uterus (). These adverse effects were also related to the location of the uterus. Immediately after HIFU treatment, patients often reported lower abdominal pain, sciatic/buttock pain, vaginal discharge or bleeding. However, the other adverse effects or complications including leg pain or numbness, and skin burns were rare (). No other adverse effects or complications such as fever, bowel injury, bladder injury or urinary retention occurred in any of these patients. We further compared the adverse effects and complications between the two groups of patients in this study and found that patients with a retroverted uterus had higher incidence rates of adverse effects than those of patients with an anteverted uterus (). Following the Society of Intenventional Radiology (SIR) classification system for complications by outcome [Citation19], these adverse effects were classified as grade A except for two patients who had a second-degree burn of skin and leg pain/numbness, respectively. No severe adverse effects were reported by anteverted uterus patients, nor did they report leg pain or skin burns. One patient with a retroverted uterus reported leg pain after USgHIFU treatment because of a temporary sacral nerve irritation. The pain lasted for 1 month and medication for pain control was suggested and thus this was classified as a major complication. Of the five patients who experienced skin burns, three had redness or blisters and two patients with surgical scars developed second-degree burns. The blisters subsided within 1 week without any specific treatment and thus this was classified as grade B. Two patients who had second-degree burns were classified as major complications because the burnt area was resected. Skin burns were only observed in patients with a retroverted uterus and could be explained by prolonged compression of the skin without lowering the transducer and the degassed water balloon to allow the skin to cool down. Poor skin preparation, scar tissue (which is avascular and has sensory loss) may have also played a role in the burns. With increased experience and frequent skin checks, the rate of skin burn in patients with a retroverted uterus can be further reduced. Although retroverted uterus patients had higher rates of adverse effects than anteverted uterus patients, the adverse effect incidence rate of USgHIFU was lower and major adverse effects more rare when compared with other treatment techniques for uterine fibroids [Citation20,Citation21]. Therefore, USgHIFU is considered a safe treatment modality in the management of uterine fibroids in patients with anteverted or retroverted uteri.
This study is limited because the non-randomisation of patients into the anteverted and retroverted groups in this retrospective study may cause bias. The study included a large number of subjects, but patients enrolled were limited by fibroid size. In addition, we did not enrol patients with fibroids that presented isointensity or hyperintensity signals on T2 weighted MR images; thus we cannot conclude whether this treatment is suitable for isointensive or hyperintensive fibroids in patients with a retroverted uterus. Further studies with a large number of subjects and longer follow-up time are required. This will allow for a prospective comparison between the two groups and establish the long-term recurrence rate and the re-intervention rate.
Conclusion
In summary, the present study indicated that USgHIFU can safely be used in the management of hypointensive fibroids in patients with anteverted and retroverted uteri. Although the rates of adverse effects were higher in patients with a retroverted uterus than those patients with an anteverted uterus, these effects were mild and transient. The NPV ratio of the fibroids in the group of patients with a retroverted uterus was significantly lower than that of patients with an anteverted uterus, but large average NPV ratio of 85.2 ± 18.7% was still achieved. Therefore, USgHIFU is also effective in treating fibroids with hypointensity signals on T2 weighted MR images in patients with a retroverted uterus. However, the fibroids in an anteverted uterus are easier to treat with USgHIFU. Future prospective studies with larger sample sizes and longer follow-up times are needed to investigate the long-term results, including long-term symptom relief, the recurrence rate, as well as the re-intervention rate.
Disclosure statement
The authors have no conflicts of interest to declare. The authors alone are responsible for the content and writing of the paper.
References
- Okolo S. Incidence, aetiology and epidemiology of uterine fibroids. Best Pract Res Clin Obstet Gynaecol 2008;22(4):571–88.
- Duhan N. Current and emerging treatments of uterine myoma-an update. Int J Womens Health 2011;3:231–41.
- Vollenhoven BJ, Lawrence AS, Healy DL. Uterine fibroids: a clinical review. BJOG 1990;97:285–98.
- Spies JB. Current role of uterine artery embolization in the management of uterine fibroids. Clin Obstet Gynecol 2016;59:93–102.
- Jones S, O’Donovan P, Toub D. Radiofrequency ablation for treatment of symptomatic uterine fibroids. Obstet Gynecol Int 2012;2012:194839.
- Zhang L, Zhang W, Orsi F, Chen W, Wang Z. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: a review of safety and efficacy. Int J Hyperthermia 2015;31:280–4.
- Stewart EA, Rabinovici J, Tempany CM, Inbar Y, Regan L, Gostout B, et al. Clinical outcomes of focused ultrasound surgery for the treatment of uterine fibroids. Fertil Steril 2006;85:22–9.
- Quinn SD, Vedelago J, Gedroyc W, Regan L. Safety and five-year re-intervention following magnetic resonance-guided focused ultrasound (MRgFUS) for uterine fibroids. Eur J Obstet Gynecol Reprod Biol 2014;182:247–51.
- Zhao WP, Chen JY, Zhang L, Li Q, Qin J, Peng S, et al. Feasibility of ultrasound-guided high intensity focused ultrasound ablating uterine fibroids with hyperintense on T2-weighted MR imaging. Eur J Radiol 2013;82:e43–9.
- Xie B, Zhang C, Xiong C, He J, Huang G, Zhang L. High intensity focused ultrasound ablation for submucosal fibroids: a comparison between type I and type II. Int J Hyperthermia 2015;31:593–9.
- Peng S, Hu L, Chen W, Chen J, Yang C, Wang X, et al. Intraprocedure contrast enhanced ultrasound: the value in assessing the effect of ultrasound-guided high intensity focused ultrasound ablation for uterine fibroids. Ultrasonics 2015;58:123–8.
- Hindley J, Gedroyc WM, Regan L, Stewart E, Tempany C, Hynyen K, et al. MRI guidance of focused ultrasound therapy of uterine fibroids: early results. Am J Roentgenol 2004;183:1713–9.
- Stewart EA, Gedroyc WM, Tempany CM, Quade BJ, Inbar Y, Ehrenstein T, et al. Focused ultrasound treatment of uterine fibroid tumors: safety and feasibility of a noninvasive thermoablative technique. Am J Obstet Gynecol 2003;189:48–54.
- Zhang L, Chen WZ, Liu YJ, Hu X, Zhou K, Chen L, et al. Feasibility of magnetic resonance imaging-guided high intensity focused ultrasound therapy for ablating uterine fibroids in patients with bowel lies anterior to uterus. Eur J Radiol 2010;73:396–403.
- Vilos GA, Allaire C, Laberge PY, Leyland N, Vilos AG, Murji A, et al. The management of uterine leiomyomas. J Obstet Gynaecol Can 2015;37:157–81.
- Oguchi O, Mori A, Kobayashi Y, Horiuchi A, Nikaido T, Fujii S. Prediction of histopathologic features and proliferative activity of uterineleiomyoma by magnetic resonance imaging prior to GnRH analogue therapy: correlation between T2-weighted images and effect of GnRH analogue. J Obstet Gynaecol (Tokyo) 1995;21:107–17.
- Funaki K, Fukunishi H, Funaki T, Sawada K, Kaji Y, Maruo T. Magnetic resonance-guided focused ultrasound surgery for uterine fibroids: relationship between the therapeutic effects and signal intensity of preexisting T2-weighted magnetic resonance images. Am J Obstet Gynecol 2007;196:184.e1–6.
- Peng S, Zhang L, Hu L, Chen J, Ju J, Wang X, et al. Factors influencing the dosimetry for high-intensity focused ultrasound ablation of uterine fibroids: a retrospective study. Medicine (Baltimore) 2015;94:e650.
- Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol 2003;14:S199–S202.
- Hart R, Molnar BG, Magos A. Long term follow up of hysteroscopic myomectomy assessed by survival analysis. BJOG 1999;106:700–5.
- Moss JG, Cooper KG, Khaund A, Murray LS, Murray GD, Wu O, et al. Randomized comparison of uterine artery embolization (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG 2011;118:936–44.
