Abstract
Objective: We evaluated long-term follow-up results of radiofrequency ablation of benign thyroid nodules to analyse the role of marginal vital tissue on nodule regrowth.
Materials and methods: We reviewed the medical records of 54 patients who underwent radiofrequency ablation between June 2008 and November 2013 with pressure symptoms, and/or cosmetic problems. All patients were followed up at least 12 months on three occasions. To evaluate an early sign of regrowth, three types of nodule volumes (total volume, ablated volume and vital volume) were measured and calculated using ultrasonography. Regrowth was defined as a more than a 50% increase in the total volume and vital volume increase was defined as a more than 50% increase compared to the previously reported smallest volume on ultrasonography.
Results: The mean follow-up period was 39.4 ± 21.7 (range, 13–87) months. Vital volume increases occurred in 31 nodules (57.4%) and there was regrowth in 13 nodules (24.1%). The mean timing of the vital volume increase was 27.5 ± 18.5 months, and for regrowth it was 39.9 ± 17.5 months. Vital volume increase tended to precede regrowth.
Conclusion: Vital volume increase tended to occur earlier than regrowth and might be an early sign of regrowth in following-up after the radiofrequency ablation of benign thyroid nodules.
Introduction
Thermal ablations for benign thyroid nodules have been reported to be an effective and safe treatment [Citation1–4]. Particularly for radiofrequency ablation (RFA), the recommendations of the Korean Society of Thyroid Radiology suggested a trans-isthmic approach and a moving-shot technique [Citation5]. These techniques have been reported to have a high efficacy with a low complication rate [Citation1,Citation6]. Recently, thermal ablation for recurrent thyroid cancers and primary thyroid cancers has been reported [Citation4,Citation7–12].
Regarding the efficacy of thyroid RFA, short-term results have reported a 50–80% volume reduction at 6 months [Citation1,Citation13], 79–90% volume reduction at 2 years [Citation14,Citation15], and 93% volume reduction at 4 years [Citation14]. Although thyroid RFA can achieves excellent volume reduction and may improve symptoms and/or cosmetic problems, several studies have reported recurrence after RFA. Recurrence rates of 5.6% and 9% have been reported after RFA [Citation14] and laser ablation [Citation16], respectively. All recurrent cases showed regrowth of the incompletely treated nodule margin. Baek et al. [Citation17] also proposed marginal regrowth as an important cause of recurrence after RFA of autonomously functional nodules.
Because of recurrence induced by marginal regrowth [Citation17,Citation18], it is important to completely treat the nodule margin. In cases of incompletely treated nodule margins, repeat treatment is necessary to prevent recurrence. Although there was no widely-accepted consensus on the optimal timing of additional ablation we usually did it when symptom resolution was not achieved, regrowth of the residual vital tissue was evident or growing vascularity was observed. However, there has been no research to determine the proper timing of additional treatment for the remaining undertreated nodule margin. We therefore evaluated long-term follow-up results of RFA of benign thyroid nodules to analyse the role of marginal vital tissue on nodule regrowth.
Materials and methods
Patients
The national public IRB designated by the Korean Ministry of Health and Welfare approved this retrospective study (P01–201606-21–002) and it waived the requirement for written informed consent for use of these data. However, all patients provided written informed consent for RFA.
From June 2008 to November 2013, among the patients who were treated by ultrasonography (US)-guided RFA in Withsim clinic for symptomatic benign thyroid nodules, 52 patients (54 nodules) were included in this study. Eligibility criteria for inclusion in the study were patients with nodules and cosmetic or symptomatic problems [Citation5], a follow-up period of at least 12 months and at least three follow-ups. The demographic characteristics of patients and thyroid nodules are summarised in . All the nodules treated were cold nodules. The mean follow-up period was 39.4 ± 21.7 (range, 13–87) months.
Table 1. Patients’ demographic data and information of nodules.
Pre-ablation assessment
One radiologist (J.S.S.) with 13 years of experience with thyroid imaging and US-guided procedures performed careful US examinations [Citation19,Citation20] and US-guided cytology/biopsy [Citation21,Citation22]. RFA was performed using high-frequency linear probes on real-time US machines (Accuvix XG or Accuvix V10, Samsung Medison, Seoul, Korea). Three orthogonal diameters were measured between the outer margins of the nodule [Citation1]. The width and height of the nodule were measured on an axial image. The length was measured on a sagittal image [Citation23]. The volume of each nodule was calculated using the following equation: V = πabc/6 (V: volume, a: the largest diameter, b and c: the other two perpendicular diameters) [Citation24–26]. All nodules were confirmed to be benign by at least two instances of fine needle aspiration cytology and/or core needle biopsy [Citation5,Citation27]. Serum levels of calcitonin were checked to rule out the possibility of medullary carcinoma, and these proved to be within normal limits in all patients [Citation5].
Procedure
The same operator (J.S.S.) performed RFA using RF generators (RF150 and RF 300, Apro-Korea, Gyeonggi, Korea) and straight-type modified internally cooled electrodes with active tip lengths of 5, 7, 10 and 15 mm (Well-Point RF Electrode, STARmed, Gyeonggi, Korea; CoATherm electrode, Apro-Korea, Gyeonggi, Korea). We used the following basic techniques suggested by the Korean Society of Thyroid Radiology [Citation5]. Patients were in a supine position with their necks fully extended. Under local anaesthesia with 2% lidocaine, we used a trans-isthmic approach and a moving-shot technique. If the nodule had cystic portion, we aspirated the fluid first as much as possible, and then RFA was done for the remaining solid portion [Citation28]. Complications during and immediately after the procedure were checked for proper management [Citation6]. After RFA, the patients were observed for 4–6 hours in the hospital [Citation1].
Follow-up
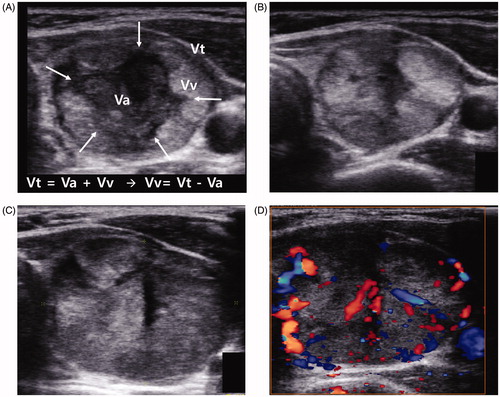
The same operator (J.S.S.) assessed volume changes at 1, 3 or 6, and 12 months and additionally at 1-year intervals. Three types of nodule volumes (total volume [Vt], ablated volume [Va] and vital volume [Vv]) were defined, measured and calculated using US images (. Vt was defined as the total nodule volume, Va was defined as an ablated nodule volume that presents as a hypoechoic area without vascularity on US. Vv was defined as an incompletely treated vital nodule volume, which was calculated by the following equation, Vv = Vt - Va. When a Vt increased by more than 50% compared to the previously reported smallest volume, we defined it as regrowth [Citation14]. When Vv increased by more than 50% compared to the previously reported smallest volume, we defined it as a Vv increase [Citation29].
Figure 1. (A) Transverse image from a 29-year-old woman who received RFA for a benign thyroid nodule 4 months previously. The index nodule volume was 21.1 mL. At the centre of the nodule, the ablated area was seen as a hypoechoic area (Va, arrows). At the margin of the nodule, the incompletely treated viable portion showed an isoechoic area (Vv). The volumes at 4 months were Vt = 7.4 mL, Va = 2.1 mL and Vv = 5.3 mL. (B) Transverse image at the 7-month follow-up. The Vt decreased to 5.3 mL whereas the Vv increased to 5.2 mL. (C) Transverse image at the 21-month follow-up. The Va decreased and nearly disappeared. The Vt increased to 12.4 mL through an increase in the Vv (12.3 mL). (D) Colour Doppler US image showing increased vascularity in the viable area of the nodule.
Additional treatment was recommended when patient’s symptom or cosmetic problem had not been resolved or recurred. When regrowth was observed without symptom recurrence, we considered additional treatment and decision was made after share discussion with patients. When Vv increase was observed but regrowth was not observed, we considered additional treatment and decision was made after share discussion with patients. When colour Doppler signal was observed to be more abundant than previous ultrasonogram, we also considered additional treatment and decision was made after share discussion with patients. Additional RFA was done seldom by the patient’s need only, such as anxiety. Data collection was done until the retreatment.
Data analysis
The endpoint of this study was to find early sign of regrowth by evaluating the total volume, ablated volume and vital volume of treated nodules. During the follow-up periods, we compared the frequency and timing of Vv increase and regrowth of treated nodules.
Results
A total of 54 nodules met the eligibility criteria. The mean volume reduction ratio (VRR) after the first RFA was 77.0%. Central well-ablated areas showed hypoechogenicity, and incompletely ablated nodule margins showed isoechogenicity (). During the follow-up period (), central well-ablated areas gradually decreased and nearly disappeared; however, marginal vital areas showed continuous regrowth with increased vascularity.
and shows the changes in Vt, Va and Vv during the follow-up period. Vt and Va showed a declining curve. compares the amount of Vv increase and regrowth. Vv increase occurred in 31 nodules (57.4%) and there was regrowth in 13 nodules (24.1%). The mean timing of Vv increase was 27.5 ± 18.5 months after RFA and that of regrowth was 39.9 ± 17.5 months. As shown in , Vv increase occurred about 1 year prior to the regrowth.
Figure 2. Changes in the Vt, Va and Vv. The Vt and Va showed a declining slope during follow-up, whilst the Vv showed relatively still.
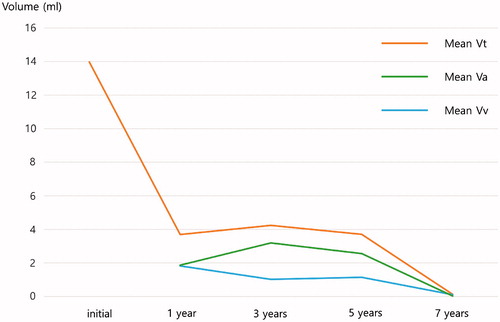
Figure 3. Comparison of the amount of Vv increase and Vt increase. The peak timing of Vv increase was 1 year after RFA. Regrowth started to occur after 1 year and occurred most frequently at 2–4 years after RFA. The mean timing of regrowth was 39.9 ± 17.5 months after RFA.
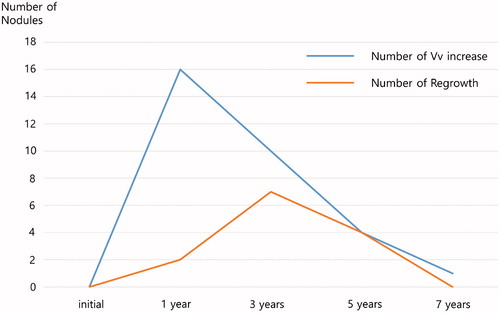
Table 2. Nodule volume changes according to the follow-up period.
The overall complication rate was 3.6% (2/56), with one major and one minor complication. One patient complained of a change in voice during the procedure but had completely recovered at 3-month follow-up. The side-effect rate was 3.6% (2/56). There were no life-threatening complications and all patients with complications recovered without sequelae ().
Table 3. Complications and side effects.
Discussion
Our current study has demonstrated that Vv increase preceded regrowth. Therefore, monitoring Vv increase is important to predict regrowth and symptom recurrence. To the best of our knowledge, there has been no previous investigation of, and there is no consensus on, the proper timing of additional treatment. We found that changes in Vt consist of two parts, namely, a Va decrease and a Vv increase. When the Va decrease is greater than the Vv increase, Vt becomes smaller. This kind of change in volume usually occurs in the earlier period after RFA. When the Vv increase exceeds the Va decrease, Vt becomes larger, which means regrowth. This kind of change in volume usually occurs late. If we trace only Vt, the Vv increase can be masked by the Va decrease. Therefore, we suggest that tracing Vv can indicate regrowth earlier than tracing Vt. If a Vv increase is detected, we should be ready to do additional sessions of ablation. In this aspect, tracing Vv rather than Vt may provide earlier signs of regrowth.
Several studies have suggested marginal recurrence of ablated thyroid nodules. Baek et al. [Citation17] first described the clinical significance of marginal recurrence after treating autonomously functioning thyroid nodules by RFA. Deandrea et al. [Citation13] also reported an improvement in thyroid function after RFA of autonomous nodules, but a complete normalisation was obtained in only a few patients (approximately 24%). Although their case number was too small to draw a conclusion and the meaning of the terminologies of recurrence and regrowth might be different, we could agree to their concept of marginal recurrence. These authors explained that it was difficult to ablate the entire nodule to minimise complications. There are several critical structures in the perithyroidal area, such as the trachea, oesophagus, recurrent laryngeal nerve [Citation30], vagus nerve [Citation31], sympathetic ganglion [Citation32] and blood vessels [Citation19]. Previous studies have suggested that the primary purpose of RFA for benign thyroid nodules is to perform debulking to reduce symptoms of pressure rather than obtaining complete ablation [Citation13]. However, we previously experienced a regrowth of the incompletely treated nodule margin [Citation33]. In a laser ablation study, Dossing et al. [Citation34] also reported that thyroid-stimulating hormone in serum was normalised in only 50% of patients. Therefore, the margin of the thyroid nodule should be completely treated to minimise marginal recurrence.
Several factors were described to influence the nodule regrowth. Several investigators described that initial solidity and initial nodule volume was the factors affecting treatment response. Larger nodules were known to require more treatment session, because complete ablation of all the periphery of the nodule could not be achieved by single session of treatment [Citation1,Citation14,Citation35]. Post-procedural marginal vascularity was another influencing factor [Citation36]. Moreover, possible other influencing factors of the regrowth are nature of thyroid nodule, the maximum temperature reached during treatment, treatment modalities and the type of energy source. In the future, validation of these factors is necessary.
Regarding minimising marginal recurrence, Ha et al. [Citation37] suggested that a moving-shot technique using a straight-type, internally cooled electrode could minimise marginal recurrence. The small active tip of the electrode could minimise thermal damage to the surrounding critical structures [Citation7]. A hydrodissection technique has also been suggested to minimise thermal damage [Citation38]. Knowledge of critical structures in the perithyroidal area has been suggested [Citation19]. Huh et al. [Citation18] suggested that single-session ablation is effective in most thyroid nodules; however, for nodules larger than 20 mL, additional ablation may be required to achieve sufficient volume reduction.
Our current study has demonstrated that RFA is effective for the volume reduction of a benign thyroid nodule for up to 7-year follow-up. We also found a low complication rate without sequelae or procedure-related deaths during this follow-up period. In the earlier period of follow-up, about 1 year, our data indicated a VRR of 73.6%, which is comparable to previous investigations [Citation1, Citation14] and recently published RFA and LTA comparing study [Citation39,Citation40]. Our data indicated mean VRR of 77.0%, which is comparable to previous studies, namely, 93% at a 4-year follow-up [Citation14] and 79% at a 2-year follow-up [Citation15]. Our results showed a lower VRR than previous report by Lim et al. [Citation14], especially in larger tumour group. These results may be due to marginal regrowth in our study series. Therefore, additional ablation sessions are necessary to prevent recurrence [Citation18].
Single-session laser-ablation studies have also shown a gradual volume reduction up to 2 years but also reported recurrence after 3–5 years of follow-up [Citation15,Citation16,Citation41]. We found a similar pattern in our current analyses. Regrowth began at 12 months and tended to be prominent at 2–4 years of follow-up. A secondary peak of regrowth appeared later than 5 years. This delayed regrowth suggests that long-term stabilised nodules can show regrowth in a slowly growing, marginal, incompletely treated area; therefore, additional ablation is necessary to prevent long-term regrowth. Lim et al. [Citation14] used multiple treatment sessions (2.2 ± 1.4 sessions) to achieve continuous volume reduction and to prevent marginal recurrence. Their final mean VRR was 93.5% at 4-year follow-up, and the recurrence rate was 5.6%. Single-session laser ablation effectively decreased nodule volume and relieved nodule-related symptoms until 2 years; however, nodule volume increase was detected after 3 years, probably due to marginal regrowth [Citation16,Citation41,Citation42]. In a 3-year follow-up laser ablation study, the final VRR was 58% [Citation42].
Conclusions
In conclusion, Vv increase occurred about 1 year earlier than regrowth. Thus, tracing Vv can indicate regrowth of marginal vital tissue earlier than tracing Vt after RFA of benign symptomatic thyroid nodules.
Disclosure statement
Grant: none.
Jung Hwan Baek. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: patent holder of the unidirectional ablation electrode. Other relationships: none to disclose.
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Jeong WK, Baek JH, Rhim H, et al. (2008). Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol 18:1244–50.
- Negro R, Salem TM, Greco G. (2016). Laser ablation is more effective for spongiform than solid thyroid nodules. A 4-year retrospective follow-up study. Int J Hyperthermia 32:822–8.
- Pacella CM, Mauri G, Achille G, et al. (2015). Outcomes and risk factors for complications of laser ablation for thyroid nodules: a multicenter study on 1531 patients. J Clin Endocrinol Metab 100:3903–10.
- Mauri G, Cova L, Tondolo T, et al. (2013). Percutaneous laser ablation of metastatic lymph nodes in the neck from papillary thyroid carcinoma: preliminary results. J Clin Endocrinol Metab 98:E1203–7.
- Na DG, Lee JH, Jung SL, et al. (2012). Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol 13:117–25.
- Baek JH, Lee JH, Sung JY, et al. (2012). Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology 262:335–42.
- Lim HK, Baek JH, Lee JH, et al. (2015). Efficacy and safety of radiofrequency ablation for treating locoregional recurrence from papillary thyroid cancer. Eur Radiol 25:163–70.
- Kim JH, Baek JH, Sung JY, et al. (2016). Radiofrequency ablation of low-risk small papillary thyroid carcinoma: preliminary results for patients ineligible for surgery. Int J Hyperthermia 20:1–11.
- Sun J, Liu X, Zhang Q, et al. (2016). Papillary thyroid carcinoma treated with radiofrequency ablation in a patient with hypertrophic cardiomyopathy: a case report. Korean J Radiol 17:558–61.
- Suh CH, Baek JH, Choi YJ, et al. (2016). Efficacy and safety of radiofrequency and ethanol ablation for treating locally recurrent thyroid cancer: a systematic review and meta-analysis. Thyroid 26:420–8.
- Zhang M, Luo Y, Zhang Y, et al. (2016). Efficacy and safety of ultrasound-guided radiofrequency ablation for treating low-risk papillary thyroid microcarcinoma: a prospective study. Thyroid 26:1581–7.
- Mauri G, Cova L, Ierace T, et al. (2016). Treatment of metastatic lymph nodes in the neck from papillary thyroid carcinoma with percutaneous laser ablation. J Vasc Interv Radiol 39:1023–30.
- Deandrea M, Limone P, Basso E, et al. (2008). US-guided percutaneous radiofrequency thermal ablation for the treatment of solid benign hyperfunctioning or compressive thyroid nodules. Ultrasound Med Biol 34:784–91.
- Lim HK, Lee JH, Ha EJ, et al. (2013). Radiofrequency ablation of benign non-functioning thyroid nodules: 4-year follow-up results for 111 patients. Eur Radiol 23:1044–9.
- Spiezia S, Garberoglio R, Milone F, et al. (2009). Thyroid nodules and related symptoms are stably controlled two years after radiofrequency thermal ablation. Thyroid 19:219–25.
- Valcavi R, Riganti F, Bertani A, et al. (2010). Percutaneous laser ablation of cold benign thyroid nodules: a 3-year follow-up study in 122 patients. Thyroid 20:1253–61.
- Baek JH, Moon WJ, Kim YS, et al. (2009). Radiofrequency ablation for the treatment of autonomously functioning thyroid nodules. World J Surg 33:1971–7.
- Huh JY, Baek JH, Choi H, et al. (2012). Symptomatic benign thyroid nodules: efficacy of additional radiofrequency ablation treatment session-prospective randomized study. Radiology 263:909–16.
- Ha EJ, Baek JH, Lee JH. (2015). Ultrasonography-based thyroidal and perithyroidal anatomy and its clinical significance. Korean J Radiol 16:749–66.
- Russ G. (2015). Risk stratification of thyroid nodules on ultrasonography with the French TI-RADS: description and reflections. Ultrasonography 35:25–38.
- Shin JH, Baek JH, Chung J, et al. (2016). Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean society of thyroid radiology consensus statement and recommendations. Korean J Radiol 17:370–95.
- Lee YH, Baek JH, Jung SL, et al. (2015). Ultrasound-guided fine needle aspiration of thyroid nodules: a consensus statement by the Korean society of thyroid radiology. Korean J Radiol 16:391–401.
- Choi YJ, Baek JH, Hong MJ, et al. (2015). Inter-observer variation in ultrasound measurement of the volume and diameter of thyroid nodules. Korean J Radiol 16:560–5.
- Hong MJ, Baek JH, Choi YJ, et al. (2015). Radiofrequency ablation is a thyroid function-preserving treatment for patients with bilateral benign thyroid nodules. J Vasc Interv Radiol 26:55–61.
- Turtulici G, Orlandi D, Corazza A, et al. (2014). Percutaneous radiofrequency ablation of benign thyroid nodules assisted by a virtual needle tracking system. Ultrasound Med Biol 40:1447–52.
- Ugurlu MU, Uprak K, Akpinar IN, et al. (2015). Radiofrequency ablation of benign symptomatic thyroid nodules: prospective safety and efficacy study. World J Surg 39:961–8.
- Lee HY, Baek JH, Ha EJ, et al. (2016). Malignant-looking thyroid nodules with size reduction: core needle biopsy results. Ultrasonography 35:327–34.
- Baek JH, Ha EJ, Choi YJ, et al. (2015). Radiofrequency versus ethanol ablation for treating predominantly cystic thyroid nodules: a randomized clinical trial. Korean J Radiol 16:1332–40.
- Haugen BRM, Alexander EK, Bible KC, et al. (2016). 2015 American Thyroid Association Management Guidelines for Adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133.
- Shin JH, Baek JH, Ha EJ, et al. (2012). Radiofrequency ablation of thyroid nodules: basic principles and clinical application. Int J Endocrinol 2012:919650.
- Ha EJ, Baek JH, Lee JH, et al. (2011). Clinical significance of vagus nerve variation in radiofrequency ablation of thyroid nodules. Eur Radiol 21:2151–7.
- Shin JE, Baek JH, Ha EJ, et al. (2015). Ultrasound features of middle cervical sympathetic ganglion. Clin J Pain 31:909–13.
- Sung JY, Baek JH, Jung SL, et al. (2015). Radiofrequency ablation for autonomously functioning thyroid nodules: a multicenter study. Thyroid 25:112–7.
- Dossing H, Bennedbaek FN, Hegedus L. (2003). Ultrasound-guided interstitial laser photocoagulation of an autonomous thyroid nodule: the introduction of a novel alternative. Thyroid 13:885–8.
- Baek JH, Kim YS, Lee D, et al. (2010). Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol 194:1137–42.
- Ahn HS, Kim SJ, Park SH, et al. (2016). Radiofrequency ablation of benign thyroid nodules: evaluation of the treatment efficacy using ultrasonography. Ultrasonography 35:244–52.
- Ha EJ, Baek JH, Lee JH. (2014). Moving-shot versus fixed electrode techniques for radiofrequency ablation: comparison in an ex-vivo bovine liver tissue model. Korean J Radiol 15:836–43.
- Kim JH, Yoo WS, Park YJ, et al. (2015). Efficacy and safety of radiofrequency ablation for treatment of locally recurrent thyroid cancers smaller than 2 cm. Radiology 276:909–18.
- Ha EJ, Baek JH, Kim KW, et al. (2015). Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and Bayesian network meta-analysis. J Clin Endocrinol Metab 100:1903–11.
- Mauri G, Sconfienza LM. (2016). Image-guided thermal ablation might be a way to compensate for image deriving cancer overdiagnosis. Int J Hyperthermia 30:1–2.
- Døssing H, Bennedbæk FN, Hegedus L. (2011). Long-term outcome following interstitial laser photocoagulation of benign cold thyroid nodules. Eur J Endocrinol 165:123–8.
- Papini E, Rago T, Gambelunghe G, et al. (2014). Long-term efficacy of ultrasound-guided laser ablation for benign solid thyroid nodules. Results of a three-year multicenter prospective randomized trial. J Clin Endocrinol Metab 99:3653–9.
