Abstract
Purpose: To assess the long-term outcome of 516 consecutive patients treated with multiple-electrode switching system (MESS) radiofrequency ablation (RFA) for hepatocellular carcinoma (HCC) that met the Milan criteria.
Materials and methods: We performed 522 MESS RFAs on 516 patients from December 2006 to June 2011. A total of 956 tumours that met the Milan criteria with an average diameter of 2.64 cm (range, 0.9–4.6 cm) were treated with MESS RFA. Ultrasonic contrast and serum α-fetoprotein (AFP) were measured every 2 months during the first postoperative year and every 4 months thereafter. Enhanced computed tomography was performed every 6 months. Survival was estimated using the Kaplan–Meier method. Follow-up was censored at 60 months. Multivariate analysis was performed using the Cox proportional hazards model.
Results: For the 956 HCC tumours, the complete ablation rate with MESS was 98.83% (510/516). During a median of 34 months (IQR, 23–52 months) of follow-up, 171 patients died and 4 were lost to follow-up (15, 30, 38 and 42 months). The cumulative incidence of local tumour progression at 1, 3 and 5 years was 0.39%, 4.96% and 6.66%, respectively, and the 1-, 3- and 5-year overall survival was 99.42%, 83.97% and 68.42%, respectively. Tumour size >30 mm was the only parameter that was predictive of local tumour progression (p < .0001). Risk factors associated with overall survival included prothrombin time >14 s, serum AFP levels >200 ng/mL and tumour abutting vessel diameter <5 mm. The complication rate was 1.74%.
Conclusion: MESS RFA is a safe and effective method for HCC treatment. This approach results in a high local progression-free survival for HCC tumours that meet the Milan criteria.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common causes of cancer-related mortality worldwide [Citation1]. Currently, the management of early HCC includes liver resection, transplantation and radiofrequency ablation (RFA) [Citation2]. Among relatively recent therapeutic approaches, RFA exhibits relatively high effectiveness [Citation3]. This approach is associated with low complication rates and short hospital stays compared to surgery [Citation4]. The efficacy of RFA has been demonstrated for early HCC [Citation5], but until now, RFA has been limited for local tumour control of tumours >3 cm due to the difficulty in creating a sufficiently large and homogeneous ablation volume including the target tumour and a 5–10-mm safety margin [Citation6]. In addition, the local tumour progression rate is the main limitation of monopolar RFA [Citation7]. In this context, with the advance of single-site RFA technology, multiple-electrode switching system (MESS) RFA using a switching radiofrequency system has emerged as one of the most promising techniques. MESS RFA advanced the clinical application of techniques in the field of HCC treatment [Citation8]. Nevertheless, before MESS RFA can be considered as a first-line treatment for HCC meeting the Milan criteria (up to three lesions <3 cm, <5 cm for any single lesion, no extrahepatic manifestations, no vascular invasion), the effect of MESS RFA on these tumours must be clarified.
Materials and methods
Ethics statement
This study was performed in accordance with the Declaration of Helsinki and was reviewed and approved by the Southwest Hospital of Third Military Medical University Institutional Review Board (approval number 2105042). Written consent was provided by the patients for their information to be stored in the hospital database and used for research.
Patients
A retrospective analysis of the clinical data of 516 patients who met Milan criteria [Citation9] underwent MESS RFA between December 2006 and June 2011 was performed. All patients were newly diagnosed and did not undergo any prior treatment for HCC. A total of 516 patients included 438 (85%) males and 78 (15%) females, with an average age of 55.0 (range, 26–82) years. In total, 522 procedures of MESS RFA were performed. All patients were diagnosed with liver cirrhosis [Citation10,Citation11] (Child-Pugh class A in 199 patients and Child-Pugh class B in 317 patients) that was mostly related to infection with hepatitis virus (hepatitis B virus in 480 patients, and hepatitis C virus in 26 patients; all were treated with nucleotide analogues). Among the 956 HCC tumours in these 516 patients, the average tumour size was 2.64 (range, 0.9–4.6) cm. The diagnosis of HCC was made on the basis of needle biopsy for 128 patients and on the basis of non-invasive criteria for the remaining 388 patients. Non-invasive diagnosis and the initial staging of the tumours relied on at least standard triphasic cross-sectional imaging examinations with either computed tomography (CT) or magnetic resonance imaging (MRI). Tumour status was assessed by ultrasonic contrast-enhanced or gadoxetate disodium-enhanced MRI. summarises the characteristics of the patients and tumours at baseline.
Table 1. Characteristics of 516 patients with 956 HCCs treated with MESS RFA.
Definitions
During follow-up, all patients underwent enhanced CT imaging and blood tests [including α-fetoprotein (AFP), complete blood count and liver function tests]. Local tumour progression was defined as solid tissue with arterial enhancement around the necrotic treated nodule and in continuity with its border. Otherwise, new tumours were classified as intrahepatic remote recurrence and extrahepatic metastasis. If any of these occurred, further treatment was determined after discussion between the patient and the clinician, considering the patient’s condition [Citation12]. Liver cirrhosis was diagnosed according to imaging, laboratory tests and/or biopsy [Citation10,Citation11].
MESS RFA
All MESS RFA procedures were performed percutaneously by three hepatobiliary surgeons with 15 years of experience in RFA treatment of HCC. Consent to surgery was obtained from all patients preoperatively. All operations were performed under monitored anaesthesia. Fentanyl citrate injection (0.1–0.2 mg, Humanwell Pharmaceutical Co., Ltd., Yichang, China) was administered for analgesia. Dexmedetomidine hydrochloride injection (50–100 mg, Hengrui Medicine Co., Ltd., Jiangsu, China) was administered for sedation. Lidocaine hydrochloride injection (Zhaohui Pharmaceutical Co., Ltd., Shanghai, China) was used for topical anaesthesia. All ablations were performed using a MESS (Cool-tip™ RF Ablation System and Switching Controller; Valley Lab, Boulder, CO). The RF electrode (Covidien LLC, Mansfield, MA) was placed under ultrasound guidance at the site of the tumour. Preoperative imaging was performed to assess tumour size, location, number, edge and blood supply. In general, in order to obtain sufficient ablative volume to fully cover the entire tumour, at an ablative margin of ≥0.5 cm beyond the index tumour was required. One RFA electrode was suitable for tumours size of ≤3 cm. For tumours >3 cm, two or more RFA electrodes were needed. Two or three RFA electrodes were placed at a spacing of 1–2 cm and connected to the power supply [Citation13]. The electrodes were placed within the tumour. The switching machine was set to the automatic mode, and all electrodes worked alternately and switched off automatically after any impendence surge. When the impedance was more than the original 10, the radiofrequency current was reduced to 0.1 A, maintained for a few seconds, and then increased again to repeat the cycle. Treatment time was set to 12 min for each site until adequate hyperechoic change of the ablated area was achieved [Citation13]. Before withdrawal of the needle, the system was set to manual mode at 35 W for ablation of the needle tract [Citation14].
Postoperative evaluation
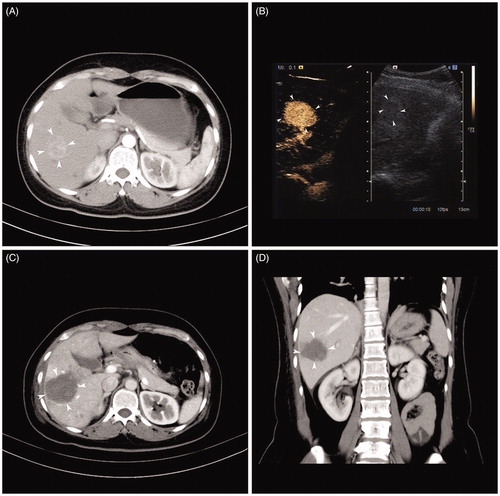
Ultrasound contrast and contrast-enhanced CT of the liver was performed 48 h after RFA to assess effect and complications. If ultrasound contrast and/or contrast-enhanced CT did not indicate enhanced areas in the tumour ablation zone, the case was considered effective and defined as complete ablation. If there was sustained enhancement, which was determined to be residual tumour by the attending radiologist, the case was defined as incomplete ablation, and another RFA procedure was performed ().
Figure 1. Representative case showing the usefulness of the MESS RFA in ablating a large volume at one time. (A) Image before MESS-RFA showing a 3.5-cm nodule with enhancement in the arterial phase. (B) Intra-procedural contrast enhanced ultrasound guiding tumour (arrowheads) targeting and monitoring. (C) Axial CT image immediately after MESS-RFA showing that the ablation zone (arrowheads) covers the index tumour (5.5 cm in size). (D) Coronal CT image reconstructed from the immediate post-procedural CT scan shows that the ablation zone (arrowheads) measures 5.4 cm in its coronal long axis.
Patient follow-up
AFP assays and contrast-enhanced ultrasound were performed every 2 months in the first postoperative year and every 4 months thereafter. Postoperative enhanced CT was performed every 6 months. The follow-up was terminated after 60 months if there was no recurrence.
Statistical analysis
Each ablation zone was measured independently by a physician from the Department of Ultrasound Intervention and another from the Department of Radiology. Quantitative data were presented as the mean ± standard deviation or median [interquartile range (IQR)], as appropriate. Qualitative data are provided as the number of cases and frequencies. Survival was estimated using the Kaplan–Meier method. A multivariate analysis was performed using the Cox proportional hazards model (stepwise, p < .10 for entry, p < .05 for statistical significance). For 15 patients underwent transplantation or resection, survival was censored on the date of accepted transplantation or resection. All statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NY). p < 0.05 was considered as statistically significant.
Results
Over the entire study period, 522 RFA procedures were performed on 956 tumours from 516 patients (). A total of 1096 RFA electrodes were used, with a mean of 2.12 RFA electrodes per procedure (). The mean tumour size was 2.64 (range, 0.9–4.6) cm. Among the 516 patients, complete ablation was achieved after a single procedure for 510 patients (98.8%). The technical success rate was 100%. No postoperative mortality occurred.
Figure 2. Flowchart showing the outcome of the 516 patients who underwent. MESS RFA as a first-line treatment for HCC meeting the Milan criteria.
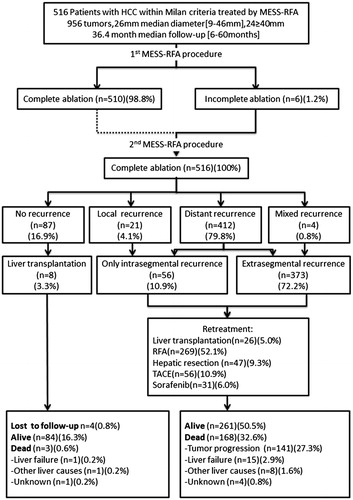
Table 2. Technical data of 522 MESS RFA procedures for the treatment of 956 HCCs in 516 patients.
Local tumour progression-free survival
Patients were followed up of a median of 34 months (IQR, 23–52 months). Twenty-one (2.20%) of the 956 tumours showed local tumour progression (). The cumulative incidence of local tumour progression at 1, 3 and 5 years was 0.39%, 4.96% and 6.66%, respectively (). Tumour size >30 mm was predictive of local tumour progression (p < .0001) (). Among 15 patients who subsequently underwent transplantation and resection, histopathological analysis of the liver tumours revealed complete necrosis of the 10 tumours originally treated with MESS RFA. In the surrounding liver parenchyma, viable microsatellite tumours were present in only one patient. For these 15 patients, survival was censored on the date of confirmed tumour progression.
Figure 3. Local tumour progression-free survival. Probability of developing local tumour progression in 516 patients with 956 HCCs [median tumour size, 26 mm (range, 9–46 mm)] treated with MESS RFA after a median follow-up of 36.4-month.
![Figure 3. Local tumour progression-free survival. Probability of developing local tumour progression in 516 patients with 956 HCCs [median tumour size, 26 mm (range, 9–46 mm)] treated with MESS RFA after a median follow-up of 36.4-month.](/cms/asset/f8367811-3593-44a8-a52b-9d0e39c980cb/ihyt_a_1330495_f0003_b.jpg)
Table 3. Risk factors in the univariate and multivariate analysis for local tumour progression in 516 patients treated with MESS RFA.
Overall survival
Four patients were lost to follow-up after 15, 30, 38 and 42 months, and 171 died. The causes of deaths were: liver failure (n = 15, 8.8%), HCC progression (n = 141, 82.5%), non-liver-related causes (n = 8, 4.7%) and unknown causes (n = 4, 2.3%). Among the 345 patients who were still alive at the end of follow-up, 84 had no detectable tumour progression (). The estimated overall 1-, 3- and 5-year survival was 99.42%, 83.97% and 68.42%, respectively (). Risk factors associated with overall survival included prothrombin time >14 s, serum AFP levels >200 ng/mL and tumour abutting vessel diameter <5 mm ().
Figure 4. Overall survival. The probability of survival in 516 patients with 956 HCCs [median diameter, 26 mm (range, 9–46 mm)] treated with MESS RFA after a median follow-up of 51.8-month.
![Figure 4. Overall survival. The probability of survival in 516 patients with 956 HCCs [median diameter, 26 mm (range, 9–46 mm)] treated with MESS RFA after a median follow-up of 51.8-month.](/cms/asset/7c0ead85-b806-4458-a051-dd15582c8522/ihyt_a_1330495_f0004_b.jpg)
Table 4. Risk factors in the univariate and multivariate analysis for overall survival in 516 patients treated with MESS RFA.
Complications
All ablation-related complications and side effects were defined as described by Ahmed et al. [Citation12]. Over the entire study period, nine major complications were observed, resulting in a complication rate of 1.74%. The complications consisted of hemothorax (n = 1), jejunal perforation (n = 1), liver failure (n = 3) and minor bleeding at the liver puncture site (n = 4). The hemothorax was treated with thoracoscopic surgery. The jejunal perforation was treated with an intestinal repair surgery. The jejunal perforation occurred in one patient with recurrent liver cancer after open hepatectomy. In this case, the jejunum was adhering to the surface of the liver, and heat conduction through the RFA electrodes led to perforation of the jejunal wall. The symptoms appeared 6 h after RFA. After clinical diagnosis, surgery was performed, and the condition was cured. The other patients received symptomatic and supportive treatment for 3–4 days without further complications. No factor could be associated with the incidence of adverse events (data not shown).
Discussion
Because the effectiveness of monopolar RFA decreases dramatically for tumours >3 cm, several strategies have been suggested to overcome this limitation. In single overlapping RFA, an increase in the number of sequential overlapping ablations usually results in an irregular coagulation shape. Incomplete ablation may occur with irregular ablated zones and it is a common reason for treatment failure [Citation15,Citation16]. According to a mathematical estimation, a single-electrode RFA needs 4–6 placements for sequential overlapping to treat tumours of 3.0–5.0 cm [Citation17]. Microwave ablation (MWA) induces higher and quicker temperature increases than RFA, has aroused great interest, especially regarding the fact that the technique could be less sensitive to the cooling effect of tissue perfusion [Citation18,Citation19]. In addition, MWA leads in favourable outcomes in large tumours [Citation20,Citation21]. Recent studies showed that no-touch multibipolar RFA could achieve high rates of local tumour progression-free survival [Citation7,Citation22]. Multipolar RFA has also been shown to achieve better tumour control than unipolar RFA [Citation23]. Nevertheless, studies directly comparing these modalities are required to determine the best one.
The reason why the treatment of large tumour leads to a high rate of complete remission is the application of trying to increase the volume of coagulation. MESS RFA and single over-lapping RFA both have the ability to increase the ablation area [Citation24]. MESS RFA can create a larger and approximately spherical converging ablation zone compared to single overlapping RFA, thus achieving a better curative effect on large tumour in less time because there are no successive overlapping ablations [Citation15,Citation16]. This system involves simultaneous placement of up to three RFA electrodes into a tumour and the alternate activation of the electrodes by the RF generator, and the synergistic effect of thermal energy (1 + 1 > 2) can further expand the ablation volume [Citation25]. Several preclinical in vivo experiments have demonstrated that switching to monopolar RFA can create a larger ablation volume than consecutive overlapping RFA [Citation26,Citation27].
In the present study, no technical failures were recorded. The first-time complete ablation rate was 98.8%. These numbers are higher than those in reports about monopolar RFA systems (91.1–96.8%) [Citation28,Citation29]. The estimated 1-, 3- and 5-year local recurrence-free survival was 99.61%, 95.04% and 93.34%, respectively. Local tumour progression was identified in 21 of 516 patients (4.1%). This rate is lower than that seen in other studies, which has been reported to be about 10% 3 years after RFA [Citation30,Citation31], suggesting a high rate of treatment effectiveness with MESS RFA.
It is noteworthy that in the present study, tumour size was the only risk factor for local tumour progression-free survival, which corroborates a report by Kim et al. [Citation32]. We found that the rate of LTP was high for tumours >4 cm (53.57%). Hocquelet et al. [Citation33] and Seror et al. [Citation22] studies of NoTouch Multibipolar RFA showed a LTP rate of <15% for tumours of 4–5 cm, which seems better than MESS results, but they used 4–6 electrodes to treat HCC. On the basis of experimental and clinical observations of standard intratumour techniques like monopolar RFA, it can be assumed that the insertion of the applicator and even more high-power centrifugal energy deposition inside the tumour might increase intratumoural pressure and therefore promote metastatic spread due to tumour cells being released in the liver microcirculation [Citation34,Citation35]. The greater the tumour diameter and the longer ablation time, the higher the likelihood of local recurrence due to the metastatic spread.
Although MESS-RFA is an intratumour ablation method, the energy is superimposed from the surrounding of the tumour to the tumour centre, thus ensuring that the maximum energy deposition is within the target surrounded by the safety border. In addition, MESS RFA can also block the blood flow in the ablation zone. This accelerates the formation of local vascular thrombosis and reduces heat loss, thereby increasing the ablation efficiency and reducing postoperative overall tumour progression [Citation16,Citation36].
In the present study, the estimated overall 1-, 3- and 5-year overall survival after RFA was 99.22%, 82.71% and 66.68%, respectively. These results agree with previous studies about RFA of early liver cancer [Citation32,Citation37]. In addition, the 5-year survival rate was similar to that of previous surgical studies in which the reported 5-year survival was 34.4–70.0% [Citation38,Citation39]. Interestingly, we found that despite tumour size being a predictor of local recurrence, it did not impact overall survival. The main explanations of these apparently paradoxical results could be, first, that MESS RFA can result in a lower local recurrence rate and, second, that the majority of these local recurrences were sufficiently limited to be completely ablated by iterative RFA.
There may also be theoretical concerns over the safety of switching RFAs using multiple electrodes. These concerns include unexpected thermal damage to vital structures and an increased risk of bleeding due to the placement of multiple electrodes. However, our complication rate was similar to those of previous reports regarding complications using the conventional RF system with a single electrode [Citation40,Citation41]. We believe that the increased risk related to the use of multiple electrodes may not be substantial. Indeed, all patients with major complications recovered fully. Multiple needle RFA, as a regional intervention, has become a significant technological breakthrough in the management of HCC. Real-time virtual ultrasound and multiple electrode overlapping increased the indications for RFA. Therefore, we suggest that it is possible and feasible of using RFA for patients with liver cancer meeting The Milan criteria.
Our study has some limitations. First, this was retrospective study without a control group. In addition, most patients had HBV, which is different from that observed in western populations. Furthermore, we had no details about the antiviral therapy of the patients. Randomized multicentre trials of MESS RFA are needed to confirm these results.
Conclusions
MESS RFA could be a safe and effective first-line treatment for patients with HCC meeting the Milan criteria. An ongoing multicentre prospective study might help to clarify the role of this approach for the treatment of early HCC (ClinicalTrials.org ID: NCT02046356).
Acknowledgements
The authors thank Chen Shu and all the medical staff at the Clinical Research Center of Southwest Hospital, the Medical Record Library of Southwest Hospital, and the anonymous reviewers for their excellent advice. This study was supported by the Clinical innovation Fund of Southwest Hospital (projects # SWH2013LC15).
Disclosure statement
The authors report no declarations of interest.
Additional information
Funding
References
- Nishikawa H, Kimura T, Kita R, Osaki Y. (2013). Radiofrequency ablation for hepatocellular carcinoma. Int J Hyperthermia 29:558–68.
- Fitzmorris P, Shoreibah M, Anand BS, Singal AK. (2015). Management of hepatocellular carcinoma. J Cancer Res Clin Oncol 141:861–76.
- Kao WY, Chiou YY, Hung HH, et al. (2012). Younger hepatocellular carcinoma patients have better prognosis after percutaneous radiofrequency ablation therapy. J Clin Gastroenterol 46:62–70.
- Hocquelet A, Balageas P, Laurent C, et al. (2015). Radiofrequency ablation versus surgical resection for hepatocellular carcinoma within the Milan criteria: a study of 281 Western patients. Int J Hyperthermia 31:749–57.
- Shiina S, Tateishi R, Arano T, et al. (2012). Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol 107:569–77, quiz 78.
- Cucchetti A, Piscaglia F, Cescon M, et al. (2013). Cost-effectiveness of hepatic resection versus percutaneous radiofrequency ablation for early hepatocellular carcinoma. J Hepatol 59:300–7.
- Hocquelet A, Aube C, Rode A, et al. (2016). Comparison of no-touch multi-bipolar vs. monopolar radiofrequency ablation for small HCC. J Hepatol 66:67–74.
- Krokidis M, Ahmed I. (2013). Overview of thermal ablation devices: radiofrequency ablation. In: Clark T, Sabharwal T, Clark T, Sabharwal TS. Interventional radiology techniques in ablation. London: Springer-Verlag, 5–11.
- Mazzaferro V, Regalia E, Doci R, et al. (1996). Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334:693–9.
- National Guideline Centre (UK). (2016). Cirrhosis in over 16s: assessment and management. London: National Institute for Health and Care Excellence (UK), 66–7.
- Starr SP, Raines D. (2011). Cirrhosis: diagnosis, management, and prevention. Am Fam Physician 84:1353–9.
- Ahmed M, Solbiati L, Brace CL, et al. (2014). Image-guided tumor ablation: standardization of terminology and reporting criteria – a 10-year update. Radiology 273:241–60.
- Laeseke PF, Frey TM, Brace CL, et al. (2007). Multiple-electrode radiofrequency ablation of hepatic malignancies: initial clinical experience. AJR Am J Roentgenol 188:1485–94.
- Wang-Yuan Z, Jiang-Zheng Z, Lu YD, et al. (2016). Clinical efficacy of metronomic chemotherapy after cool-tip radiofrequency ablation in the treatment of hepatocellular carcinoma. Int J Hyperthermia 32:193–8.
- Lee JM, Han JK, Kim HC, et al. (2007). Multiple-electrode radiofrequency ablation of in vivo porcine liver: comparative studies of consecutive monopolar, switching monopolar versus multipolar modes. Invest Radiol 42:676–83.
- Brace CL, Sampson LA, Hinshaw JL, et al. (2009). Radiofrequency ablation: simultaneous application of multiple electrodes via switching creates larger, more confluent ablations than sequential application in a large animal model. J Vasc Interv Radiol 20:118–24.
- Chen MH, Yang W, Yan K, et al. (2004). Large liver tumors: protocol for radiofrequency ablation and its clinical application in 110 patients-mathematic model, overlapping mode, and electrode placement process. Radiology 232:260–71.
- Pillai K, Akhter J, Chua TC, et al. (2015). Heat sink effect on tumor ablation characteristics as observed in monopolar radiofrequency, bipolar radiofrequency, and microwave, using ex vivo calf liver model. Medicine (Baltimore) 94:e580.
- Dodd GD 3rd, Dodd NA, Lanctot AC, Glueck DA. (2013). Effect of variation of portal venous blood flow on radiofrequency and microwave ablations in a blood-perfused bovine liver model. Radiology 267:129–36.
- Potretzke TA, Ziemlewicz TJ, Hinshaw JL, et al. (2016). Microwave versus radiofrequency ablation treatment for hepatocellular carcinoma: a comparison of efficacy at a single center. J Vasc Interv Radiol 27:631–8.
- Thamtorawat S, Hicks RM, Yu J, et al. (2016). Preliminary outcome of microwave ablation of hepatocellular carcinoma: breaking the 3-cm barrier? J Vasc Interv Radiol 27:623–30.
- Seror O, N'Kontchou G, Nault JC, et al. (2016). Hepatocellular carcinoma within Milan Criteria: no-touch multibipolar radiofrequency ablation for treatment-long-term results. Radiology 280:981.
- Cartier V, Boursier J, Lebigot J, et al. (2016). Radiofrequency ablation of hepatocellular carcinoma: mono or multipolar? J Gastroenterol Hepatol 31:654–60.
- Park MJ, Kim YS, Rhim H, et al. (2011). A comparison of US-guided percutaneous radiofrequency ablation of medium-sized hepatocellular carcinoma with a cluster electrode or a single electrode with a multiple overlapping ablation technique. J Vasc Interv Radiol 22:771–9.
- Lee JM, Han JK, Kim HC, et al. (2007). Switching monopolar radiofrequency ablation technique using multiple, internally cooled electrodes and a multichannel generator: ex vivo and in vivo pilot study. Invest Radiol 42:163–71.
- Laeseke PF, Sampson LA, Frey TM, et al. (2007). Multiple-electrode radiofrequency ablation: comparison with a conventional cluster electrode in an in vivo porcine kidney model. J Vasc Interv Radiol 18:1005–10.
- Laeseke PF, Sampson LA, Haemmerich D, et al. (2006). Multiple-electrode radiofrequency ablation creates confluent areas of necrosis: in vivo porcine liver results. Radiology 241:116–24.
- Lin SM, Lin CC, Chen WT, et al. (2007). Radiofrequency ablation for hepatocellular carcinoma: a prospective comparison of four radiofrequency devices. J Vasc Interv Radiol 18:1118–25.
- Solmi L, Nigro G, Roda E. (2006). Therapeutic effectiveness of echo-guided percutaneous radiofrequency ablation therapy with a LeVeen needle electrode in hepatocellular carcinoma. World J Gastroenterol 12:1098–104.
- Lencioni R, Cioni D, Crocetti L, et al. (2005). Early-stage hepatocellular carcinoma in patients with cirrhosis: long-term results of percutaneous image-guided radiofrequency ablation. Radiology 234:961–7.
- Choi D, Lim HK, Rhim H, et al. (2007). Percutaneous radiofrequency ablation for early-stage hepatocellular carcinoma as a first-line treatment: long-term results and prognostic factors in a large single-institution series. Eur Radiol 17:684–92.
- Kim YS, Lim HK, Rhim H, et al. (2013). Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol 58:89–97.
- Hocquelet A, Papadopoulos P, Trillaud H. (2016). No-touch multibipolar radiofrequency ablation: the new standard ablative technique for hepatocellular carcinoma 5 cm or smaller? Radiology 281:975.
- Kang TW, Lim HK, Lee MW, et al. (2015). Aggressive intrasegmental recurrence of hepatocellular carcinoma after radiofrequency ablation: risk factors and clinical significance. Radiology 276:274–85.
- Zavaglia C, Corso R, Rampoldi A, et al. (2008). Is percutaneous radiofrequency thermal ablation of hepatocellular carcinoma a safe procedure? Eur J Gastroenterol Hepatol 20:196–201.
- Woo S, Lee JM, Yoon JH, et al. (2013). Small- and medium-sized hepatocellular carcinomas: monopolar radiofrequency ablation with a multiple-electrode switching system-mid-term results. Radiology 268:589–600.
- Takahashi S, Kudo M, Chung H, et al. (2007). Outcomes of nontransplant potentially curative therapy for early-stage hepatocellular carcinoma in Child-Pugh stage A cirrhosis is comparable with liver transplantation. Dig Dis 25:303–9.
- Yamamoto J, Kosuge T, Saiura A, et al. (2007). Effectiveness of hepatic resection for early-stage hepatocellular carcinoma in cirrhotic patients: subgroup analysis according to Milan criteria. Jpn J Clin Oncol 37:287–95.
- Shimada K, Sano T, Sakamoto Y, Kosuge T. (2005). A long-term follow-up and management study of hepatocellular carcinoma patients surviving for 10 years or longer after curative hepatectomy. Cancer 104:1939–47.
- N'Kontchou G, Mahamoudi A, Aout M, et al. (2009). Radiofrequency ablation of hepatocellular carcinoma: long-term results and prognostic factors in 235 Western patients with cirrhosis. Hepatology 50:1475–83.
- Zhang F, Wu G, Sun H, et al. (2014). Radiofrequency ablation of hepatocellular carcinoma in elderly patients fitting the Milan criteria: a single centre with 13 years experience. Int J Hyperthermia 30:471–9.
