Abstract
Introduction: Minimally invasive nonsurgical techniques are gaining ground as alternatives to surgery for the treatment of benign thyroid nodules. Here, we aimed at comparing patient satisfaction after radiofrequency ablation (RFA) to that after surgery.
Methods: In this cross-sectional study, we recruited 126 patients treated with RFA and 84 treated with surgery for a single benign thyroid nodule. All patients were contacted by phone call and were asked the following questions: Are you satisfied with the symptom resolution?; Are you satisfied with the cosmetic results?; Are you satisfied overall with the procedure?; Are you taking any medication for your thyroid? Patients’ general characteristics were collected from our database.
Results: In the surgery group, there was a higher percentage of patients fully satisfied with the resolution of nodule-related symptoms (p = .02). In the RFA group, there was a higher percentage of patients fully satisfied with the cosmetic results (p = .001). In terms of overall satisfaction, there were no differences between the groups (p = .26). Nevertheless, RFA led to differing results based on thyroid nodule function. In patients with nonfunctioning thyroid nodules, RFA was as effective as surgery in terms of satisfaction with symptom resolution, while it was not in patients with autonomously functioning thyroid nodules (AFTN).
Conclusion: Our data on postoperative patient satisfaction support the notion that both RFA and surgery are valid therapeutic options for nonfunctioning thyroid nodules, while surgery should be still preferred for AFTN.
Introduction
Minimally invasive nonsurgical techniques are gaining ground as an alternative to surgery for the treatment of benign thyroid nodules [Citation1,Citation2]. These techniques include percutaneous sclerotherapy, which is usually performed with ethanol, as well as thermal ablation techniques. Percutaneous sclerotherapy with ethanol injection has been the first ultrasound (US)-guided nonsurgical technique to be used for the treatment of thyroid nodules, and it is now indicated only for symptomatic thyroid cysts [Citation3,Citation4]. On the other hand, thermal ablation procedures, which make the target nodule shrink via heat generation [Citation5], have been mostly used to treat solid thyroid nodules. These techniques include laser, radiofrequency and microwave ablation, as well as high-intensity focused ultrasound [Citation3,Citation6].
Thus far, the thermal ablation techniques that have been most widely used are laser and radiofrequency ablation (LA and RFA, respectively). It is still a matter of debate whether one is superior to the other [Citation7]. Regarding their efficacy, LA can reduce nodule volume by 40%–80% [Citation2], while RFA can reduce it by 50%–80% [Citation2,Citation8]. Although it may be perceived that RFA is somehow superior to LA in reducing thyroid nodule volume [Citation9], Mauri et al. have demonstrated that RFA and LA are similarly feasible, safe and effective in treating benign thyroid nodules when performed by the same team [Citation10]. In other words, the operators’ experience seems to be a more important indicator of treatment outcome than the ablation technique in US-guided thermal ablations [Citation11].
Recently, both LA and RFA have been included in the American Association of Clinical Endocrinologists’ guidelines as therapeutic options for symptomatic benign thyroid nodules [Citation12]. Nevertheless, for other authoritative medical societies [Citation13], surgery remains the only therapy for symptomatic benign thyroid nodules [Citation13]. To date, only a few studies have compared thermal ablations to surgery in patients with benign thyroid nodules [Citation14–16], highlighting several potential advantages of RFA over surgery. While these studies have compared the efficacy, tolerability, cost and health-related quality of life of RFA to surgery [Citation14–16], postoperative patient satisfaction has been overlooked. The current study aimed to compare RFA to surgery in terms of patient satisfaction after 12 months from the procedure.
Materials and methods
Population
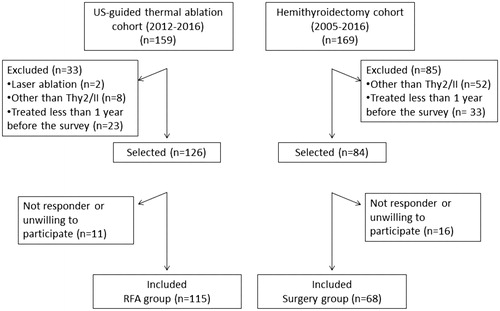
This is a cross-sectional pilot study involving patients treated with thyroid RFA (between March 2012 and March 2016) or hemithyroidectomy (hEMItx; between March 2005 and March 2016). The inclusion criteria were the following: being treated 1.) due to a solitary benign thyroid nodule (Bethesda II/Thy2/Tir2), 2.) at least one year before the survey and 3.) by the same operator (radiologist or surgeon, respectively). The benign nature of the nodules was assessed by fine needle aspiration cytology [Citation17]. Based on these criteria, we selected 126 patients previously treated with RFA (out of 159 RFA procedures) and 84 patients who had undergone hemithyroidectomy (out of 169 hemithyroidectomies). When contacted by phone, 115 patients out of 126, in the RFA group, and 68 out of 84, in the surgery group, completed the survey (). The RFA group was composed of 83 patients with nonfunctioning thyroid nodules and 32 patients with autonomously functioning thyroid nodules (AFTN). The surgery group contained 44 patients with nonfunctioning thyroid nodules and 24 patients with AFTN. The response rate to our survey was 91.3% for patients treated with RFA and 81% for patients treated with surgery (p = .04 vs RFA). The missing rate, which was lower than 20%, was acceptable in both groups [Citation18,Citation19]. For all patients that completed the survey, the following characteristics were collected from our database: baseline age, sex, thyroid nodule features, thyroid function, calcitonin, autoimmunity, and post-procedure thyroid nodule features and overall complications. It must be noted that in the RFA group, complications were classified according to the criteria defined by the Society of Interventional Radiology [Citation20], where major complications are events that lead to substantial morbidity and disability that increase the level of care and all other complications are considered minor. Given that surgical complications are not usually classified like those that follow RFA [Citation21,Citation22], we compared the rate of overall complications between the groups. The protocol of this study was approved by the Institutional Review Board of the Azienda Ospedaliera – Ospedali Riuniti di Trieste [Citation14], and all patients had given written informed consent prior to the procedures.
Thyroid nodule features
The thyroid nodule features that we took into account were nodule maximum diameter (mm), nodule volume (mL), type of nodule and vascularity. As previously reported [Citation23], the formula that we used for calculating nodule volume was πabc/6 (where ‘a’ is the maximum diameter of the nodule, and ‘b’ and ‘c’ are the other two perpendicular diameters). Volume (V) reduction was calculated as follows: (initial–finalV/initialV)*100. As for the type of the nodules, they were defined as solid when the solid component was greater than 70%, mixed when the solid component was lesser than 70% and greater than 30%, and cystic when the solid component was less than 30%. Vascularity was evaluated according to a five-point scale, where 0 is defined as no visible flow, 1 as peripheral flow only, 2 as peripheral flow with a small amount of central flow, 3 as peripheral flow plus extensive intranodular flow and 4 as central flow only. Therapeutic success was defined as a volume reduction greater than 50%.
RFA and surgical techniques
RFA. All RFA procedures were performed by the same radiologist in an outpatient regimen. After local anesthesia at the puncture site (2% lidocaine hydrochloride), the electrode was inserted under US-guidance into the thyroid nodule with a transisthmic approach (whenever possible). For the procedures, we used a radiofrequency generator (AMICA RF generator) and 18-gauge internally cooled electrodes with a 0.7–1.0–1.5 cm active-tip (Amica probes, HS AMICA). All RFA were performed with the moving-shot technique [Citation24]. Ablation was begun with 30 W of radiofrequency power, starting from the deepest areas of the nodule. If a hyperechoic zone had not formed at the electrode tip within 5–10 s, radiofrequency power was progressively increased in 10 W steps up to 60 W. Ablation was terminated when transient hyperechoic zones could be identified around the whole nodule.
Surgery. All operations were carried out by the same team, which included two surgeons (lead and assistant surgeon). These operations were carried out in an inpatient regimen. Hemithyroidectomy was performed by a single access of 2–5 cm in the middle area of the neck, approximately 2 cm above the sternal notch. Patients, under general anesthesia, were placed in the supine position with the neck extended. Minimal subplatysmal flaps were created. The midline was incised and the strap muscles were retracted laterally. The vessels of the upper thyroid peduncle were selectively ligated or closed by conventional vascular clips or other devices. Special care was taken to preserve the parathyroid glands and the inferior laryngeal nerve. Once the thyroid lobe and isthmus had been removed, the area was examined for bleeding. If there was no bleeding, the incision was closed with sutures. In some cases, a surgical drain was placed to remove fluids from the area in the following days. Finally, anesthesia was discontinued and medication was given to wake the patient.
Telephone survey
Telephone surveys are used widely in public health research internationally [Citation25]; given this vast use, we have herein employed such a method to investigate patient satisfaction after undergoing thyroid nodule treatment. Between April and August 2017, all the patients selected were contacted by phone call by the same interviewer, who was an undergraduate medical student. Based on a script, patients were informed about the nature of the survey and the organization carrying it out, and they were asked the same four questions. These were (1) Are you satisfied with the resolution of nodule-related symptoms?; (2) Are you satisfied with the cosmetic results?; (3) Are you satisfied overall with the procedure?; and (4) Are you taking any medication for your thyroid? After each of the first three questions, patients were given three options as possible answers: yes, partially and no. When interviewed about the resolution of nodule-related symptoms, they could also answer that they had never had symptoms. As for thyroid medications, they were asked an open question and their answers were coded as levothyroxine, antithyroid drugs or no medication. The script of this questionnaire has been developed taking into account that: 1) telephone survey must be concise, otherwise answers might be affected by consumer fatigue [Citation25]; and 2) questions had to fit patients who had been treated with two vastly different approaches.
Statistical analysis
Quantitative (continuous) variables are reported as mean ± SD. Qualitative (categorical) variables are reported as absolute frequencies and/or percentages. Continuous variables were compared by student's t test or by Mann–Whitney test, depending on data distribution (parametric or non-parametric, respectively). In order to control potential confounding effects and selection bias and to assure that groups were comparable, we performed a sensitivity analysis using propensity score matching with the R package ‘MatchIt’ (method nearest neighbor) [Citation26]. The patients were matched 1:1 by age and type of nodule. The details of this analysis are reported in the Supplementary material. Variations over time of nodules’ volume were evaluated with linear mixed-effects models (LME) for repeated measures and multiple comparisons of nodules’ volume respect to different follow-up periods (baseline vs 1, 12 and 24 months) were performed with Tukey’s post-hoc test. Categorical variables were compared by Chi-square test or Fischer’s exact test whenever appropriate. All statistical analyses were carried out in R system for statistical computing (Ver. 3.3.2; R Development Core Team, 2016). Statistical significance was set at p < .05.
Results
Patient characteristics
Patients did not differ in terms of sex, nodule volume and vascularity, thyroid function, autoimmunity and calcitonin (). On the other hand, patients treated with RFA were older, which is consistent with the fact that RFA was initially used to treat patients with contraindications to surgery [Citation27,Citation28], those of whom are generally older. In addition, in the RFA group, there was a lower percentage of cystic nodules (). This is consistent with the fact that when patients with cystic nodules preferred a non-surgical treatment, they were initially treated with percutaneous ethanol injection, which should be the first-line treatment in this case [Citation3,Citation4]. Only if clinical problems were incompletely resolved after ethanol ablation were patients then treated with RFA [Citation29,Citation30]. Having said that, age and type of nodule did not affect our results, as shown with a propensity score-matching (Supplementary material) [Citation26].
Table 1. Patients’ characteristics at baseline.
Thyroid nodule features after RFA
In this study, the patients who underwent RFA had been followed for 33.7 ± 14.6 months. Follow-up revealed that RFA significantly reduced thyroid nodule volume, as shown in . In particular, the nodules’ volume decreased linearly with time (p < .001 Linear Mixed-Effects model for repeated measures) being 18.0 ± 16.1 ml at baseline, 9.4 ml ±10.1 ml after 1 month from the procedure, 5.1 ± 6.7 ml after 12 months and 4.7 ± 8.4 ml after 24 months. In other words, the volume decreased by 46%, 74% and 76% at 1, 12 and 24 months after RFA, respectively. Therapeutic success was achieved with a single session in 111 out of 115 patients, while 4 patients required two sessions (average number of sessions per patient was 1.03 ± 0.17).
Table 2. Nodule volume reduction after RFA.
When looking at the subgroups of patients with nonfunctioning thyroid nodules (83 patients) and AFTN (32 patients) who were treated with RFA, nodular volume decreased linearly with time in both cohorts (p < .001, Linear Mixed-Effects model for repeated measures), as shown in . In the subgroup of patients with nonfunctioning thyroid nodules, 3 patients underwent 2 sessions of RFA and the average number of sessions per patient was 1.04 ± 0.19. In the subgroup of patients with AFTN, 1 patient underwent 2 sessions of RFA and the average number of sessions per patient was 1.03 ± 0.18.
Patient satisfaction
Resolution of nodule-related symptoms. From the first set of pie charts (), it can be seen that the majority of the patients in both the RFA and surgery group answered that they were fully satisfied with the symptom resolution. The percentage of patients who were asymptomatic prior to the procedure did not differ between the groups (p = .56), being 19% in the RFA and 23.5% in the surgery group. If we excluded the patients that were asymptomatic, the percentage of patients fully satisfied in the surgery group (96%) became significantly higher as compared to RFA (81%; p = .02). Conversely, the percentage of patients only partly satisfied was significantly higher in the RFA group (18%) than in the surgery group (4%; p = .03), as shown in .
Figure 2. Survey outcome in all patients. Patients included 115 subjects treated with RFA and 68 subjects treated with surgery. (A) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied with the resolution of nodule-related symptoms?’. Upper panel: pie charts that include asymptomatic patients; lower panel: pie charts that exclude asymptomatic patients. (B) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied with the cosmetic results?’. (C) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied overall with the procedure?’.
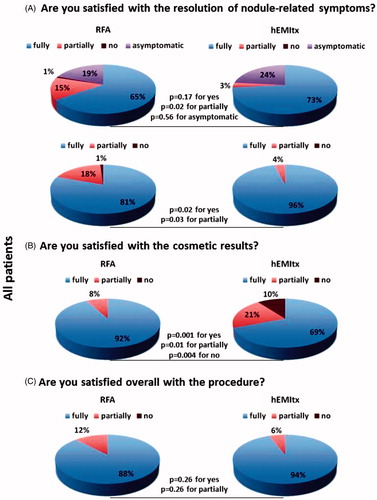
Cosmetic results. In the RFA group, there was a significantly higher percentage of patients fully satisfied with the cosmetic results (92%) as compared to the surgery group (69%; p = .001), as shown in . Conversely, in the surgery group, there was a higher percentage of patients who were only partially satisfied (p = .01) or not satisfied with the cosmetic results (p = .004), as shown in .
Overall satisfaction. There were no differences in terms of overall satisfaction between the groups. Surgery was associated with a tendency towards a greater percentage of patients fully satisfied, which, however, was not statistically significant (p = .26), as shown in .
Subgroup analysis
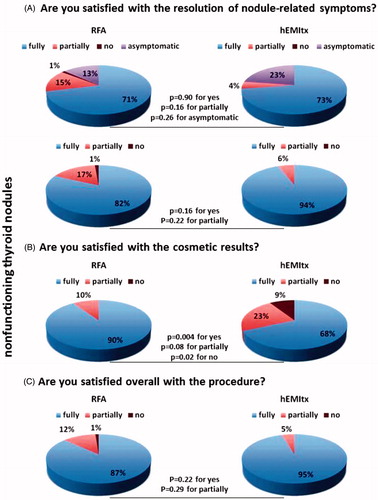
Nonfunctioning thyroid nodules. It has been argued that the best candidate for thyroid RFA is a single, cold, benign, symptomatic thyroid nodule [Citation5] and that RFA might be not as effective in AFTN [Citation2,Citation17]. Based on these premises, we carried out a subgroup analysis and looked at patient satisfaction in the subgroup of subjects with nonfunctioning thyroid nodules and in that of subjects with AFTN. In the subgroup of patients with nonfunctioning thyroid nodules, the majority answered that they were fully satisfied with the symptom resolution after both procedures (). The percentage of patients who were asymptomatic prior to the procedure did not differ between the groups (p = .26), being 13.3% in the RFA and 22.7% in the surgery group. If we excluded the patients that were asymptomatic, the percentage of patients fully satisfied in the surgery group (94.1%) did not significantly differ from the RFA group (81.9%; p = .16). Regarding the cosmetic results (), there was a significantly higher percentage of patients in the RFA group that were fully satisfied with the cosmetic results (90%) as compared to the surgery group (68%; p = .004). Conversely, there was a higher percentage of patients in the surgery group who were not satisfied with the cosmetic results (p = .02 vs RFA), as shown in . There were no differences in terms of overall satisfaction between the two groups .
Figure 3. Survey outcome in the subgroup of patients with nonfunctioning thyroid nodules. Patients included 83 subjects treated with RFA and 44 subjects treated with surgery. (A) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied with the resolution of nodule-related symptoms?’. Upper panel: pie charts that include asymptomatic patients; lower panel: pie charts that exclude asymptomatic patients. (B) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied with the cosmetic results?’. (C) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied overall with the procedure?’.
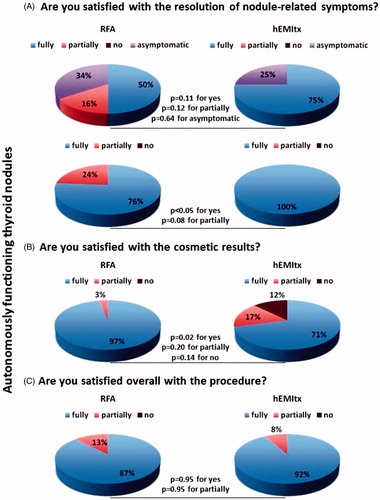
Autonomously functioning thyroid nodules. It is in patients with AFTN that RFA was not as fully satisfactory as surgery with respect to the resolution of nodule-related symptoms (). If we excluded the patients that were asymptomatic, the percentage of patients fully satisfied with RFA was 76% as compared to the surgery group where the rate was 100% (p < .05). The percentage of patients partially satisfied did not differ between the groups. Regarding the cosmetic results, in the RFA group, there was a significantly higher percentage of patients fully satisfied with the cosmetic results (97%), as compared to the surgery group (71%; p = .02), as shown in . There were no differences in terms of overall satisfaction between the two groups, as shown in .
Figure 4. Survey outcome in the subgroup of patients with autonomously functioning thyroid nodules. Patients included 32 subjects treated with RFA and 24 subjects treated with surgery. (A) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied with the resolution of nodule-related symptoms?’. Upper panel: pie charts that include asymptomatic patients; lower panel: pie charts that exclude asymptomatic patients. (B) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied with the cosmetic results?’. (C) Pie charts representing the distribution of the answers ‘yes’, ‘partially’ and ‘no’ to the question: ‘Are you satisfied overall with the procedure?’.
Complications
Consistent with the literature [Citation31], in the RFA group, two patients had a major complication (1.7%). These were one case of voice change that lasted more than 1 month and one case of third-degree skin burn. Moreover, three patients had a minor complication (2.6%). These were two cases of voice change that lasted less than 1 month and one case of late-onset thyroiditis with thyrotoxicosis. Thus, in the RFA group, the rate of overall complications was 4.3% (5 patients out of 115). In the hEMItx group, the rate of overall complications was 10.3% (7 patients out of 68). The majority of them had a voice change due to a transient unilateral vocal cord palsy (5 out of 7), while the remaining patients had a transient hypocalcemia (1 out of 7) and a wound complication (1 out of 7). The groups did not significantly differ in terms of complication rate (p = .13). Nevertheless, in the surgery group, 28 patients out of 68 (41.1%) became hypothyroid and started taking levothyroxine after the procedure. If we included the prevalence of postoperative hypothyroidism, which is an occurrence that increases the level of care and requires medication, there was a significant difference in the complication rate following RFA vs surgery, as the surgery group became significantly higher in complications (p = .001).
Thyroid function and medication in patients with AFTN
The percentage of patients with AFTN was the same in both groups, being 28% in the RFA group and 35% in the hEMItx group (p = .29). Among these patients, surgery was more effective than RFA in terms of resolution of a hyperthyroid state without the need of antithyroid drugs (p = .002 vs RFA). After surgery, almost all patients (95.8%) withdrew from antithyroid drugs except for one (4.2%), who continued taking methimazole afterwards. On the other hand, RFA was effective in 18 patients out of 34 (52.9%), and the remaining 16 patients (47.1%) had to continue with methimazole. Nevertheless, RFA did not cause hypothyroidism, while 37.5% of surgery patients (9 patients out of 24) started taking levothyroxine after surgery. Overall, there were no differences between the two groups in terms of patients who kept taking medication after each procedure (p = .55), being 47.1% in the RFA group and 41.7% in the surgery group.
Discussion
While we are entering the era of interventional thyroidology [Citation5,Citation12,Citation27], surgery remains the first-line therapy for most patients with symptomatic benign thyroid nodules [Citation13]. In this study, we compared RFA to surgery in terms of patient satisfaction. Overall, the vast majority of our patients who underwent surgery were fully satisfied with the outcome (94%). This is in line with the observation that thyroid surgery profoundly improves patient overall quality of life [Citation32]. Thyroid surgery has clear advantages over any other technique. It represents a definitive solution to a symptomatic thyroid nodule. Moreover, it does not only relieve from local symptoms and/or remove an AFTN, but it can exclude malignancy. In this study, it is likely that the vast majority of our patients were fully satisfied after being operated on (94%) because surgery relieved them fully from nodule-related local symptoms (96%), and/or hyperthyroidism (95.8%). On the other hand, however, the price that is paid for such a treatment includes postoperative hypothyroidism, a neck scar, and a rate, albeit low, of other complications, such as laryngeal nerve injury, hypoparathyroidism, postoperative bleeding and wound infection [Citation33].
Minimally invasive techniques, and among them thyroid RFA, represent a promising therapeutic alternative to surgery that allow to avoid its drawbacks [Citation34]. The efficacy and safety of thyroid RFA have been demonstrated in several studies [Citation17]. In particular, in a recent randomized controlled trial where RFA was compared to observation, RFA significantly reduced the volume of benign thyroid nodules, such that cosmetic and compressive symptoms significantly improved after the procedure, without relevant side effects [Citation35]. To our knowledge, only three studies have compared surgery to RFA [Citation14–16], suggesting that RFA was not inferior to surgery in nonfunctioning benign thyroid nodules [Citation14], and that it was even superior in terms of complications [Citation15] and post-procedure health-related quality of life (HRQoL) [Citation16]. In particular, the group of Yue, who assessed HRQoL, showed that it significantly improved after 6 months from both surgery and RFA, but that patients who had been treated with RFA had better HRQoL as compared to those surgically treated. Nevertheless, the same authors argued that these differences could have disappeared over time, as HRQoL of patients that are operated on take some time to convalesce after surgery [Citation36].
At a first glance, our data seemed to challenge the concept that RFA and surgery are equal in terms of clinically efficacy. When comparing all the patients, surgery was found more effective than RFA in terms of satisfaction with the resolution of nodule-related symptoms, as well as with the cure of hyperthyroidism. This is consistent with the ATA recommendation [Citation13] to choose surgery as the preferred therapeutic option for a patient with a symptomatic benign thyroid nodule, and the concept that RFA should be taken into account in case of refusal or contraindications to it [Citation28]. Nevertheless, when we looked at the rate of satisfaction with the resolution of nodule-related symptoms in the subgroups of patients with nonfunctioning thyroid nodules and with AFTN, we found that RFA led to different results based on thyroid nodule function. In patients with nonfunctioning thyroid nodules, RFA was actually as effective as surgery in terms of satisfaction with the resolution of nodule-related symptoms, while it was not in patients with AFTN. This is in line with our previous work, in which we analyzed the outcomes of patients treated by RFA to those who underwent hemithyroidectomy and found that both techniques were equally effective for treating nodule-related clinical problems, with the exception being patients with an initial nodular volume greater than 35 ml and AFTN [Citation14], where surgery should be still preferred. This is also in line with the literature suggesting that the best results from RFA appear to be limited to small and, partially, medium nonfunctioning thyroid nodules [Citation5,Citation8].
Interestingly, in this study, both RFA and surgery had a similar overall satisfaction score. One reason accounting for the high percentage of patients who were overall fully satisfied after RFA – also in the AFTN subgroup – is that patient satisfaction is multidimensional. It includes more aspects than local symptom relief or hyperthyroidism control. It has recently been argued that modern medicine should aim not only to treat the relevant disease, but also to take care of the patient as a whole [Citation34]. For example, although RFA does not completely remove the nodule, it has the advantage of not leaving any scar. Consistent with this outcome, patient satisfaction with the cosmetic results was greater in the RFA than the surgery group. Second, RFA does not cause hypothyroidism, has a low rate of complications [Citation37], and post-procedural pain is rare [Citation37]. In this study, the rate of complications after RFA was lower than after surgery, and 41.1% of the patients surgically treated had to take levothyroxine. Finally, RFA is an outpatient procedure, which does not require general anesthesia and hospitalization days. We speculate that it must have been for these reasons that, in the subgroup of patients with AFTN, the rate of patients overall fully satisfied with RFA was similar to surgery.
For this cross-sectional survey, patients were selected from our database. Although RFA and surgery had been carried out at different times before the survey, we made sure that all patients had been treated at least one year prior to it, as postsurgical complications might need one year to recover [Citation38]. Certainly, in some patients survey point was far from initial surgery, which should be taken into account when looking at our data. Having said that, the strengths of this study include the homogeneity of treatments (patients were treated by the same radiologist or surgeon) and of interviews, which were carried out by the same neutral person. Regarding telephone surveys, their strength is that they allow to collect data of a sensitive nature because respondents gain perceived anonymity [Citation25]. On the other hand, these kinds of surveys have some limitations. First, they must be concise, and therefore less detailed than other questionnaires. Second, a growing percentage of patients refuses to participate due to the recent phenomenon of consumer fatigue [Citation25]. These are the reasons underlying the choice of this questionnaire. Nevertheless, given that this survey had not been validated before it was used, further larger studies with validated surveys are needed to confirm our data and look into postoperative patient satisfaction.
In conclusion, our results on postoperative patient satisfaction show that RFA and surgery were both desirable for the patients and support the notion that both RFA and surgery are valid first-line therapeutic options in case of benign nonfunctioning thyroid nodules. On the other hand, given that the percentage of patients with AFTN that were fully satisfied over symptom resolution was lower after RFA than after surgery, this study suggests that surgery should be still the preferred first-line therapeutic option in this subgroup of patients.
Supplemental Material
Download MS Power Point (178.6 KB)Supplemental Material
Download PDF (94.1 KB)Supplemental File 1
Download PDF (99.8 KB)Acknowledgements
Thanks are due to Dr. Georgette Argiris for her precious help in editing the language of this paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Gharib H, Hegedus L, Pacella CM, et al. Clinical review: Nonsurgical, image-guided, minimally invasive therapy for thyroid nodules. J Clin Endocrinol Metab. 2013;98:3949–3957.
- Papini E, Pacella CM, Hegedus L. Diagnosis of endocrine disease: thyroid ultrasound (US) and US-assisted procedures: from the shadows into an array of applications. Eur J Endocrinol. 2014;170:R133–R146.
- Dietrich CF, Muller T, Bojunga J, et al. Statement and recommendations on interventional ultrasound as a thyroid diagnostic and treatment procedure. Ultrasound Med Biol. 2018;44:14–36.
- Sung JY, Kim YS, Choi H, et al. Optimum first-line treatment technique for benign cystic thyroid nodules: ethanol ablation or radiofrequency ablation?. AJR Am J Roentgenol. 2011;196:W210–W214.
- Lupo MA. Radiofrequency ablation for benign thyroid nodules – a look towards the future of interventional thyroidology. Endocr Pract. 2015;21:972–974.
- Mainini AP, Monaco C, Pescatori LC, et al. Image-guided thermal ablation of benign thyroid nodules. J Ultrasound. 2017;20:11–22.
- Ferrara V, Buonomenna C, Mauri G. Image-guided ablations in patients with thyroid tumors. J Cancer Res Clin Oncol. 2017;143:2637–2639.
- Cesareo R, Palermo A, Pasqualini V, et al. Radiofrequency ablation for the management of thyroid nodules: a critical appraisal of the literature. Clin Endocrinol (Oxf.). 2017;87(6):639–648.
- Ha EJ, Baek JH, Kim KW, et al. Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and bayesian network meta-analysis. J Clin Endocrinol Metab. 2015;100:1903–1911.
- Mauri G, Cova L, Monaco CG, et al. Benign thyroid nodules treatment using percutaneous laser ablation (PLA) and radiofrequency ablation (RFA). Int J Hyperthermia. 2017;33:953–954.
- Mauri G, Sconfienza LM. Is operators' experience more important than the ablation technique in image-guided thermal ablations? Int J Hyperthermia. 2017;33:955–956.
- Gharib H, Papini E, Garber JR, et al. AAATFoT: American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical Guidelines for clinical practice for the diagnosis and management of thyroid nodules – 2016 update. Endocr Pract. 2016;22(5):622–639.
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1–133.
- Bernardi S, Dobrinja C, Fabris B, et al. Radiofrequency ablation compared to surgery for the treatment of benign thyroid nodules. Int J Endocrinol. 2014;2014:934595.
- Che Y, Jin S, Shi C, et al. Treatment of benign thyroid nodules: comparison of surgery with radiofrequency ablation. AJNR Am J Neuroradiol. 2015;36:1321–1325.
- Yue WW, Li XL, Xu HX, et al. Quality of life and cost-effectiveness of radiofrequency ablation versus open surgery for benign thyroid nodules: a retrospective cohort study. Sci Rep. 2016;6:37838.
- Bernardi S, Stacul F, Zecchin M, et al. Radiofrequency ablation for benign thyroid nodules. J Endocrinol Investig. 2016;39:1003–1013.
- Dong Y, Peng CY. Principled missing data methods for researchers. Springerplus. 2013;2:222.
- Enders CK. Using the expectation maximization algorithm to estimate coefficient alpha for scales with item-level missing data. Psychol Methods. 2003;8:322–337.
- Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria – a 10-year update. Radiology. 2014;273:241–260.
- Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28:271–276.
- Rosato L, De Crea C, Bellantone R, et al. Diagnostic, therapeutic and health-care management protocol in thyroid surgery: a position statement of the Italian Association of Endocrine Surgery Units (U.E.C. CLUB). J Endocrinol Investig. 2016;39:939–953.
- Bernardi S, Stacul F, Michelli A, et al. 12-month efficacy of a single radiofrequency ablation on autonomously functioning thyroid nodules. Endocrine. 2017;57(3):402–408.
- Baek JH, Lee JH, Valcavi R, et al. Thermal ablation for benign thyroid nodules: radiofrequency and laser. Korean J Radiol. 2011;12:525–540.
- Boland M, Sweeney MR, Scallan E, et al. Emerging advantages and drawbacks of telephone surveying in public health research in Ireland and the U.K. BMC Public Health. 2006;6:208.
- Baek S, Park SH, Won E, et al. Propensity score matching: a conceptual review for radiology researchers. Korean J Radiol. 2015;16:286–296.
- Na DG, Lee JH, Jung SL, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012;13:117–125.
- Garberoglio R, Aliberti C, Appetecchia M, et al. Radiofrequency ablation for thyroid nodules: which indications? The first Italian opinion statement. J Ultrasound. 2015;18:423–430.
- Jang SW, Baek JH, Kim JK, et al. How to manage the patients with unsatisfactory results after ethanol ablation for thyroid nodules: role of radiofrequency ablation. Eur J Radiol. 2012;81:905–910.
- Sung JY, Baek JH, Kim KS, et al. Single-session treatment of benign cystic thyroid nodules with ethanol versus radiofrequency ablation: a prospective randomized study. Radiology. 2013;269:293–300.
- Chung SR, Suh CH, Baek JH, et al. Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J Hyperthermia. 2017;33:920–930.
- Sorensen JR, Watt T, Cramon P, et al. Quality of life after thyroidectomy in patients with nontoxic nodular goiter: a prospective cohort study. Head Neck. 2017;39:2232–2240.
- Verloop H, Louwerens M, Schoones JW, et al. Risk of hypothyroidism following hemithyroidectomy: systematic review and meta-analysis of prognostic studies. J Clin Endocrinol Metab. 2012;97:2243–2255.
- Mauri G, Sconfienza LM. Percutaneous ablation holds the potential to substitute for surgery as first choice treatment for symptomatic benign thyroid nodules. Int J Hyperthermia. 2017;33:301–302.
- Deandrea M, Sung JY, Limone P, et al. Efficacy and safety of radiofrequency ablation versus observation for nonfunctioning benign thyroid nodules: a randomized controlled international collaborative trial. Thyroid. 2015;25:890–896.
- Wickwar S, McBain H, Ezra DG, et al. The psychosocial and clinical outcomes of orbital decompression surgery for thyroid eye disease and predictors of change in quality of life. Ophthalmology. 2015;122:2568–2576. e2561.
- Kim C, Lee JH, Choi YJ, et al. Complications encountered in ultrasonography-guided radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers. Eur Radiol. 2017;27:3128–3137.
- Villarroya-Marquina I, Sancho J, Lorente-Poch L, et al. Time to parathyroid function recovery in patients with protracted hypoparathyroidism after total thyroidectomy. Eur J Endocrinol. 2018;178:105–113.