Abstract
Purpose: Our study aims to compare ultrasound (US)-guided percutaneous microwave ablation (PMWA) and conventional thyroidectomy in benign thyroid nodules (BTN) treatment.
Materials and methods: From December 2015 to December 2017, a total of 280 patients with at least one benign thyroid nodule were studied retrospectively, including 156 patients treated with US-guided PMWA and 124 patients treated with conventional thyroidectomy. Propensity score matching was performed to decrease the confounding bias due to retrospective assignment and to balance the pre-operation data of the two groups. A total of 106 pairs (1:1) was created. The operation time, intraoperative blood loss, postoperative hospitalization time, serum levels of interleukin (IL-6), C-reactive protein (CRP), tumor necrosis factor-α (TNF-α) 12 h after operation and postoperative complications incidence rate were compared between the two groups. The volume reduction ratio was calculated in the US-guided PMWA group at 1, 3, 6 and 12 months after treatment. Registration number: ChiCTR1800015531.
Results: Significant differences were found between the two groups in levels of CRP, IL-6, and TNF-α after the operation; there were significant differences between the two groups in intraoperative blood loss, operation time, postoperative hospitalization time and postoperative complications rate. The volume reduction ratio at 1, 3, 6 and 12 months after treatment was 15.2%, 47.6%, 67.2% and 79.6%, respectively.
Conclusions: Our study demonstrated that US-guided PMWA is characterized by a definite therapeutic success rate, good cosmetic effect, slight injury and rapid recovery. US-guided PMWA is an effective technique for benign thyroid nodules treatment.
Introduction
One study has shown that about 10–70% of adults worldwide can be found to have thyroid nodules under US examination and iodine deficiency is a risk factor [Citation1]. Most thyroid nodules are benign according to current research [Citation2]. Large thyroid nodules can compress the trachea and esophagus, leading to a series of symptoms around the neck, such as cosmetic issues, pain, difficulty swallowing [Citation3] and serious respiratory problems which can even threaten the life of patients [Citation4]. For thyroid goiter treatment, conventional thyroidectomy will leave a permanent scar on the neck, and certain complications may set in, such as injury of recurrent laryngeal, parathyroid gland damage and secondary hemorrhage [Citation4]. Some patients who received conventional bilateral thyroidectomy need to take levothyroxine after the operation for the rest of their lives to prevent hypothyroidism. In some rare cases, long-term and large-dose levothyroxine may lead to an adverse effect such as reduction of bone density [Citation5].
The invention of thermal ablation largely solves surgery complications. The method is proved to be effective by researchers from all over the world through different kinds of research [Citation6]. US-guided PMWA was proved to be efficient in thyroid nodules treatment in 2012 for the first time by Feng et al. [Citation3]. Compared to other ablation therapies, the advantage of US-guided PMWA is an exactly defined area of ablation. Since then, many studies have been done to prove the effectiveness and practicability of US-guided PMWA. However, there was no related research comparing US-guided PMWA and conventional thyroidectomy by the propensity score matching method.
Our study is the first propensity score matching study between US-guided PMWA and conventional thyroidectomy for BTN. We aimed to compare the safety, therapeutic success rate, cosmetic score, intraoperation blood loss, postoperative hospitalization and operation-related complications of US-guided PMWA and conventional thyroidectomy.
Materials and methods
Our study was approved by [Institutional Review Boards of Affiliated Zhuhai Hospital of Jinan University] and registered at Chinese Clinical Trial Registry as required by legislation (Registration number: ChiCTR1800015531). We conducted this study as a retrospective analysis. We obtained written informed consent from each subject before the operation, and for each subject, the follow-up period was one year.
Patients
All patients were selected according to the following criteria: (a) the thyroid nodule was over 2 mm apart from the thyroid capsule; (b) the maximum diameter of the TN ≥2 cm; (c) existence of cosmetic problems or compressive symptoms; (d) cytological conformation of the benign nature of the nodule through US-guided fine needle aspiration cytology (FNAC); and (e) serum levels of thyrotropine and thyroid hormone within normal levels. Patients who fully complied with all of the inclusion criteria (a)– (e) were studied. The exclusion criteria were as follows: (a) whole or a large part of the TN is located behind the sternum; (b) function of the vocal cords on the opposite side of the TN is abnormal; (c) patients with serious coagulation disorders; (d) patients with serious cardiopulmonary diseases; and (e) patients with a history of chemotherapy or radiotherapy. Patients who were in accordance with any one of the exclusion criteria (a)–(e) were excluded.
Methods
Pre-ablation assessments
US examination was conducted before the operation to verify the volume, shape, location and number of TN to make sure the vessels, lymph nodes, trachea and other vital structures were adjacent to the TN. FNAC was carried out to confirm the benign nature of the TN. Serum concentrations of thyrotropine, triiodothyronine, free thyroxine, thyroglobulin, complete blood count, activated partial thromboplastin time, prothrombin time, IL-6, TNF-α and CRP were verified by laboratory examinations. The largest diameter and two other perpendicular diameters of TNs were measured. TN volume and volume reduction rate (VRR) (%) were calculated according to the following formulas: TN volume = π*a*b*c/6 (where a is the largest diameter, b and c are the other two perpendicular diameters) and VRR(%) = [(baseline volume − final volume)*100]/baseline volume.
Before ablation, the cosmetic grade score was recorded according to the following standard: score 1, no palpable mass; score 2, no cosmetic problem and a palpable mass; score 3, cosmetic problem on swallowing only; and score 4, a readily observable cosmetic problem. On the other hand, we asked the patients to rate their symptoms on a 10 cm visual analog scale [Citation7].
Ablation procedures
Ablation was conducted by experienced surgeons in our hospital who have been trained in US-guided PMWA. Patients were placed in a supine position with their necks fully exposed. Patients’ respiratory rate, pulse, blood pressure, blood oxygen saturation and other vital signs were monitored during the operation with vein access opened simultaneously. Local anesthesia with a mixture of 2 ml 2% lidocaine and 2 ml saline was performed along the puncture pathway from skin to thyroid capsule under US (). The ‘hydrodissection technique’ proposed by Yue et al. [Citation6] was adapted in puncture conduction. A small incision about 2 mm in length was made in the puncture site. A mixture of 2% lidocaine and 0.9% normal saline was infused into the surrounding thyroid capsule to protect the vital structures adjacent to the TNs. After that, manipulators inserted an MWA antenna into the TN at the designated place (). The largest TN was subject to our study for patients with two or more TNs.
Figure 1. US scans in a 57-year-old woman: (a) US scans showed that the largest diameter was 3.67 cm; (b) US scans showed that the two other perpendicular diameters were 2.46 cm and 2.28 cm, respectively. (c) Contrast-enhanced ultrasonography (CEUS) showed a cyst-solid mixed TN. The TN’s volume was 10.8 ml, of which the solid portion was 95.1%; the arrow highlights the central region of the TN.
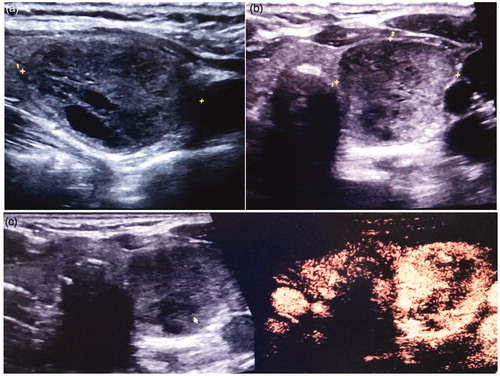
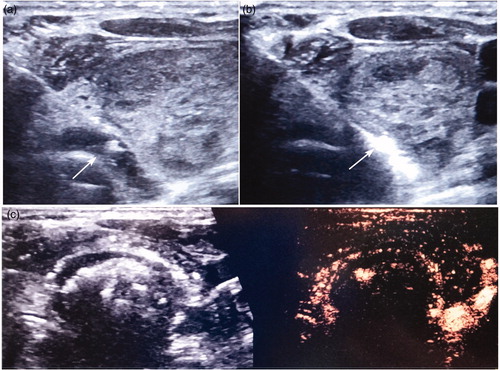
Figure 2. The same patient as in Figure 1. (a) In the MWA procedure, the ‘hydrodissection technique’ was applied. The isolation zone is marked with an arrow in the figure. (b) MWA antenna could be visualized as a hyperechoic line in the MWA process under US. The area that surrounds the antenna also shows the hyperechoic region. (c) CEUS showed that approximately 99% of the TN had been ablated.
We used the microwave system (MTI-5DT, Changcheng Medical Instruments Cooperation, Nanjing, China, YZB National 7534-2013) which contains a microwave generator and a water circulating cooled ablation antenna for US-guided MWA. The MWA antenna (Z16.100) is 10 cm in total length and has an active tip 3 mm in length.
In the ablation procedures, the operator divided the TN into several units, and moved the antenna from the bottom of the TN in a unit by unit way. This method was called ‘moving shot technique’ method, which was proposed by Jeong et al. [Citation8] for the first time in 2008. To prevent the antenna from being hindered by the gas produced during the ablation procedures, the tip of the antenna was initially positioned at the bottom of the TN. The gas caused by the ablation would produce a hyperechoic cloud. The ablation process was done when the hyperechoic cloud covered all of the areas of the TN.
For conventional thyroidectomy, patients received general anesthesia with endotracheal intubation. After that they were placed in a supine position with their necks slightly extended. A 4–6 cm incision was made on the superior border of the sternum. Platysma myoides were abstracted to expose the TN. From the sternal notch to the level of the thyroid cartilage, subplatysmal flap dissection was conducted. The linea alba cervicalis was vertically divided from the strap muscles to expose the thyroid gland. The thyroid goiter was dissected with an ultrasound knife (Johnson&Johnson Inc., New Brunswick, NJ, USA). In the process of the operation, recurrent laryngeal nerves, superior thyroid arteries, inferior thyroid arteries, superior thyroid veins, inferior thyroid veins and middle thyroid veins should be carefully identified or transected. According to the TN’s location, volume and adjacent structures, the TN was cut off solely or accompanied with the other part of the thyroid gland lobes. Parathyroid glands were identified and the blood supply to parathyroid glands was protected carefully during the operation. The surgical field was douched with 100 ml sterile distilled water (37 °C). The surgical wound was sutured with a traumatic needle and 5–0 absorbable sutures.
Post-procedural follow-up
Double-blinded method was applied in this study. After the operation, all patients got the same type of wound dressing. The operation time, intraoperative blood loss, postoperative hospitalization and postoperative complication rates were recorded respectively and compared between the two groups. Weighing method was applied to calculate the intraoperative blood loss. Intraoperative blood loss = (postoperative weight of gauze − preoperative weight of gauze)/blood density. Blood density in this study was regarded as 1.05. For each subject, the operation complications include paralysis of vocal cords, skin burn, vomit, fever and hypothyroidism. Postoperative laryngoscopy and radionuclide scan of the thyroid were conducted on each subject to verify the function of the vocal cords and residual thyroid. Serum concentrations of thyrotropine, triiodothyronine, free thyroxine, thyroglobulin, IL-6, TNF-α and CRP were detected at 12 h after the operation. US assessments were performed at 1, 3, 6 and 12 months after treatment. For patients in the conventional thyroidectomy group, pathological examination was conducted to verify that the nodules were benign.
Statistical analysis
Multiple logistic-regression models were used to estimate the propensity scores for each subject. The covariates contained the following baseline characteristics: gender, age, three diameters of TN, volume, symptoms and cosmetic score. Qualitative variables were analyzed by the χ2 test. One-way analysis of variance was used to compare the normal distribution quantitatively. Mann–Whitney U-test was used to analyze the skewed distribution data. Bivariate correlation test was used to evaluate the relationship between baseline volume and VRR. To estimate whether or not the resultant sample size had sufficient magnitude comparing US-guided PMWA to traditional thyroidectomy, a power analysis with a one-sided α level set as 8% for the VRR was applied. SPSS software (version 22.0; SPSS, Chicago, IL, USA) was used to conduct the statistical analyses. We defined the significance level as p values of less than .05.
Results
Baseline characteristics
From December 2015 to December 2017, 280 patients with BTNs were selected as our subjects, which were classified into the US-guided PMWA group (n = 156) and conventional thyroidectomy group (n = 124), and the baseline clinical and demographic parameters are shown in . Patients in the US-guided PMWA group possessed a higher prevalence of lower age, longer tumor diameter and higher cosmetic scores compared to patients in the conventional thyroidectomy group. Then, 106 pairs were matched after propensity score matching was performed (). For patients in the US-guided MWA group, the propensity score was 0.521 before matching. For patients in the conventional thyroidectomy group, the propensity score was 0.623. The standardized difference was 10.8% (p < .001). We matched 106 pairs in the two groups. After matching, the mean propensity score in the US-guided PMWA group (n = 106) was 0.521. In the conventional thyroidectomy group (n = 106), the propensity score was 0.583. The standardized difference was 5.2% (p = .101). Before and after matching, we used a standardized difference to estimate the balance of all of the baseline covariates between the US-guided PMWA group and the conventional thyroidectomy group. We effectively discriminated and calibrated our propensity score model between the subjects of the two groups. The conventional thyroidectomy group was composed of 78 women and 28 men. The US-guided MWA group was composed of 75 women and 31 men. Other characteristics did not reveal a significant difference between the propensities of the matched groups.
Table 1. Baseline characteristics of patients with TNs treated by US-guided PMWA and conventional thyroidectomy before and after matching.
Treatment outcomes
The follow-up period for each subject was 12.8 months in the US-guided PMWA group and 12.6 months in the conventional thyroidectomy group. shows a better cosmetic effect in the US-guided PMWA group compared to the conventional thyroidectomy group. Each characteristic of the treatment results is summarized in . In the US-guided PMWA group, the operation time, intraoperative blood loss, postoperative hospitalization and postoperational complication rates were respectively 28.6 ± 5.2 min, 6.5 ± 2.0 ml, 1.6 ± 0.5 day and 1.0 ± 0.5%. In the conventional thyroidectomy group, the characteristics were respectively 80.2 ± 15.6 min, 30.6 ± 4.3 ml, 4.3 ± 0.5 day and 12.0 ± 2.3% (p < .005). Paralysis of vocal cords appeared in one patient (0.94%) and skin burn appeared in one patient (0.94%) in the US-guided PMWA group and both patients recovered within three months after ablation. In the conventional thyroidectomy group, paralysis of vocal cords appeared in seven patients (6.60%). All of the patients also recovered within three months after the operation (). Radionuclide scan of the thyroid showed that the residual thyroid function of all of the subjects in this study was normal. The pathological examination showed that all of the nodules in the conventional thyroidectomy group were benign.
Figure 3. (a) A 61-year-old woman in the thyroidectomy group; the picture shows her early postoperative wound within a highly visible area; (b) The same patient as in Figures 1 and 2, the picture shows her cosmetic results of US-guided PMWA, where there is no obvious cervical scar in her neck.

Table 2. Operation results in the MWA and conventional thyroidectomy groups in a propensity-matched population of patients with TNs.
Table 3. Serum Concentrations of CRP in the MWA and conventional thyroidectomy groups in a propensity-matched population of patients with TNs (mg/L).
Table 4. Serum Concentrations of IL-6 in the MWA and conventional thyroidectomy groups in a propensity-matched population of patients with TNs (ng/L).
Table 5. Serum Concentrations of TNF-α in the MWA and conventional thyroidectomy groups in a propensity-matched population of patients with TNs (mg/L).
Table 6. Treatment results in the MWA group in a propensity-matched population of patients with TNs.
In the US-guided PMWA group, serum concentrations of CRP increased slightly from 0.6 ± 0.2 mg/L to 0.7 ± 0.1 mg/L at 12 h after ablation (p > .1); and in the conventional thyroidectomy group, CRP levels increased significantly from 0.6 ± 0.18 mg/L to 12.0 ± 1.9 mg/L at 12 h after the operation (p < .01) (). In the US-guided PMWA group, serum concentrations of IL-6 increased slightly from 3.5 ± 1.3 mg/L to 3.6 ± 1.2 mg/L at 12 h after ablation (p > .05); in the conventional thyroidectomy group, serum levels of IL-6 increased from 3.5 ± 1.2 mg/L to 14.2 ± 4.5 mg/L at 12 h after the operation (p < .001) (). In the US-guided PMWA group, serum concentrations of TNF-α increased from 35.6 ± 5.2 mg/L to 42.2 ± 5.9 mg/L at 12 h after ablation (p < .001); in the conventional thyroidectomy group, serum levels of TNF-α increased from 37.2 ± 2.1 mg/L to 50.1 ± 2.8 mg/L at 12 h after the operation (p < .001) (); There were no significant between-group differences in serum concentrations of CRP, IL-6 and TNF-α before the operation.
Factors related to the treatment outcome
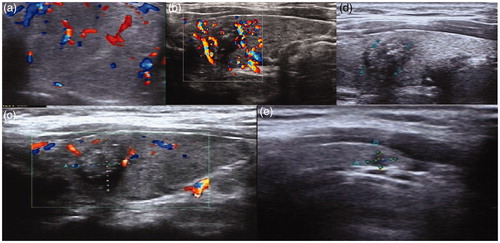
For the US-guided PMWA group, VRRs at 1, 3, 6, and 12 months after ablation were 15.2 ± 2.3%, 47.6 ± 3.6%, 67.2 ± 6.8% and 79.6 ± 10.2%, respectively. shows the volume reduction of the thyroid nodule after US-guided PMWA treatment. We conducted bivariate correlation analyses between six months VRR and baseline volume in the US-guided PMWA group. The results showed that the correlation coefficient was 0.067 (p = .486). Thus, VRR was not associated with the baseline volume.
Figure 4. US scans in a 30-year-old woman: (a) US reveals a cyst-solid mixed TN. The TN’s volume was 4.1 ml, of which the solid portion was 83.6%. (b) One month after the ablation, the volume of the TN decreased to 2.5 ml with a VRR of about 39.6%. (c) Three months after US-guided PMWA, the volume was 1.2 ml, with a VRR of about 73.8%. (d) Twelve months after US-guided PMWA, the volume was 0.03 ml with a VRR of about 97.6%.
Discussion
Conventional thyroidectomy will leave a scar on patients within a highly visible area, and PMWA can avoid this problem. Most patients who chose PMWA therapy method were most concerned with cosmetic outcome. PMWA eliminates goiters mainly by its thermal effect. In the process of ablation, the temperature can rise over 60 °C. This heat can cause protein denaturation and necrosis. Goiters can be ablated in this way. The present study showed that in patients with BTN, PMWA does not affect the function of the thyroid. This is mainly because only the nodules are affected and normal thyroid tissue can be minimized through the PMWA technique. In the study of Korkusuz et al. [Citation9], 99mTc-pertechtenate uptake declined only in the ablation area and was completely normal in the surrounding tissue, indicating that the function of the surrounding tissue was not affected.
The moving shot technique applied in this study could reduce the heat deposition and in this way, the critical structures adjacent to the TN were protected from damage. This technique is more controllable and safer than the traditional multiple fixed shot technique [Citation10]. The entire goiter can be treated by moving the antenna tip unit by unit. This method can ensure that a significant nodule volume reduction can be achieved safely.
Thermal injury of the recurrent laryngeal nerve is the most serious complication after PMWA. The morbidity of dysphonia after PMWA is 0–9.1% [Citation3,Citation6,Citation11]. The operator in our study was experienced in US-guided PMWA. In our study, only one patient in the PMWA group experienced hoarseness, and the patient recovered in three months without any treatment. The morbidity of hoarseness in the PMWA group was higher than that of conventional thyroidectomy. There was no one in the PMWA group who experienced dysdipsia, while the morbidity of dysdipsia in the conventional thyroidectomy group was 2.83%. In the present research, VRRs at 1, 3, 6, and 12 months after ablation were 15.2 ± 2.3%, 47.6 ± 3.6%, 67.2 ± 6.8% and 79.6 ± 10.2%, respectively. Almost all of the nodules got a volume reduction of nearly 80% after 12 months, which revealed an effective therapy effect of PMWA. Significant differences were found between the two groups in levels of CRP, IL-6, and TNF-α after the operation. Since serum levels of CRP, IL-6, and TNF-α are a good representation of trauma [Citation12], these results indicate minimal invasion of PMWA compared to conventional thyroidectomy. There were also significant differences between the two groups in blood loss, operation time, postoperative hospitalization time and postoperative complication rate. These results all reflected the obvious advantages of US-guided PMWA in BTN treatment.
Conventional thyroidectomy will dislodge a large part of the thyroid, and inevitably cause hypothyroidism after surgery. US-guided PMWA, as a minimally invasive procedure, does not damage normal thyroid tissues, and will not cause postoperative hypothyroidism.
Our study also contained some shortcomings. It mainly contained the following limitations: (1) we will increase the number of patients and TNs in our work for the forthcoming period. (2) The follow-up time is relatively short for a complete research cycle. In the next stage, we will extend our follow-up time and verify the long-term results.
Although our research has its limitations, it still provided an encouraging conclusion verifying that US-guided PMWA has many advantages over conventional thyroidectomy. US-guided PMWA may become a promising and attractive option for BTN patients.
Conclusions
Our study revealed that US-guided PMWA has advantages over conventional thyroidectomy with regards to operation injury, postoperative complications and cosmetic effects, providing an attractive option in benign thyroid nodules treatment.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review boards of the Affiliated Zhuhai Hospital of Jinan University (Zhuhai, China) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgements
We are deeply grateful to all of the scientists who have supported and encouraged this work.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Papini E, Pacella CM, Misischi I, et al. The advent of ultrasound-guided ablation techniques in nodular thyroid disease:towards a patient-tailored approach. Best Pract Res Clin Endocrinol Metab. 2014;28:601–618.
- Che Y, Jin S, Shi C, et al. Treatment of benign thyroid nodules: comparison of surgery with radiofrequency ablation. AJNR Am J Neuroradiol. 2015;36:1321–1325.
- Feng B, Liang P, Cheng Z, et al. Ultrasound-guided percutaneous microwave ablation of benign thyroid nodules: experimental and clinical studies. Eur J Endocrinol. 2012;166:1031–1037.
- Happel C, Korkusuz H, Koch DA, et al. Combination of ultrasound guided percutaneous microwave ablation and radioiodine therapy in benign thyroid diseases. Nuklearmedizin. 2015;53:118–124.
- Schneider R, Schneider M, Reiners C, et al. Effects of levothyroxine on bone mineral density, muscle force, and bone turnover markers: a cohort study. J Clin Endocrinol Metab. 2012;97:3926–3934.
- Yue W, Wang S, Wang B, et al. Ultrasound guided percutaneous microwave ablation of benign thyroid nodules: safety and imaging follow-up in 222 patients. Eur J Radiol. 2013;82:e11–e16.
- Sung JY, Baek JH, Kim KS, et al. Single-session treatment of benign cystic thyroid nodules with ethanol versus radiofrequency ablation: a prospective randomized study. Radiology. 2013;269:293–300.
- Jeong WK, Baek JH, Rhim H, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008;18:1244–1250.
- Korkusuz H, Happel C, Heck K, et al. Percutaneous thermal microwave ablation of thyroid nodules. Preparation, feasibility, efficiency. Nuklearmedizin. 2014;53:123–130.
- Yue W, Wang S, Yu S, et al. Ultrasound-guided percutaneous microwave ablation of solitary T1N0M0 papillary thyroid microcarcinoma: initial experience. Int J Hyperthermia. 2014; 30:150–157.
- Heck K, Happel C, Grünwald F, et al. Percutaneous microwave ablation of thyroid nodules: effects on thyroid function and antibodies. Int J Hyperthermia. 2015;31:560–567.
- Aomatsu M, Kato T, Kasahara E, et al. Gender difference in tumor necrosis factor-α production in human neutrophils stimulated by lipopolysaccharide and interferon γ.Biochem Biophys Res Commun. 2013;441:220–222.
