Abstract
Objective: Cervical pregnancy (CP) is a rare type of ectopic pregnancy and is considered to be a life-threatening condition due to the risk of severe hemorrhage. Unfortunately, no consensus on standard conservative treatment for CP has been established. The study objective was to evaluate the efficacy and safety of high-intensity focused ultrasound (HIFU) followed by suction curettage for cervical pregnancy.
Method: Three patients with cervical pregnancy undergoing high-intensity focused ultrasound followed by suction curettage were analyzed. Patient age, gestational age, endocervical mass, serum human chorionic gonadotrophin (HCG) level, blood loss, and time for normal menstruation recovery were recorded.
Results: Three patients with cervical pregnancy were successfully treated with HIFU followed by suction curettage. After HIFU treatment, the fetal cardiac activity disappeared or the blood flow in the pregnancy tissue significantly decreased. The termination of the cervical pregnancy of all three patients was performed successfully without heavy bleeding. The estimated blood loss was 10–20 ml. The time for menstruation recovery was 30–45 days. No obvious complications of HIFU were observed in these cases.
Conclusion: High-intensity focused ultrasound followed by suction curettage seems to be considered as conservative management for patients who desire to preserve their uterus.
Introduction
Cervical pregnancy (CP) is the implantation of a developing conceptus in the cervical glands and the fibrous cervical wall. The incidence of CP was 1:16,000–1:18,000 in all pregnancies and 1:1000 in all ectopic pregnancies [Citation1]. It is a rare type of ectopic pregnancy and considered to be a life-threatening condition due to the risk of severe bleeding. Previously, treatment of CP often required a hysterectomy to save the patient’s life. In recent decades, it is diagnosed early by transvaginal ultrasound in patients in their first trimester of pregnancy and could be conservatively treated to preserve the uterus. The general principles in the management of cervical pregnancy are as follows: (1) minimize the risk of hemorrhage; (2) eliminate the gestational cervical product; (3) spare fertility [Citation2]. Various conservative methods for cervical pregnancy termination have been suggested in an attempt to preserve the uterus and the patient’s future fertility and to avoid hemorrhage [Citation1,Citation3,Citation4]. Unfortunately, no consensus on standard conservative treatment for CP has been established [Citation5]. Since cervical pregnancy is even more unusual than before, case reports concerned with the conservative management of cervical pregnancy are increasingly important. Below, we report three cases of CP in which high-intensity focused ultrasound (HIFU) was performed as a prophylactic procedure before suction curettage.
Materials and methods
Patients
This work was approved by the Institutional Review Board of our institution and was performed in the Department of Obstetrics and Gynecology, Third Xiangya Hospital of Central South University, Changsha, China between March 2015 and March 2017. The diagnosis of CP was based on the medical history of the patients, clinical examination, serum human chorionic gonadotrophin (HCG), and ultrasonographic findings. The main ultrasound criteria of CP in this study are as follows: enlargement of the endocervical canal, the presence of an entire gestational sac inside the endocervical canal, closure of the internal cervical os, and an empty uterine cavity [Citation6]. Data on age, gravidity and parity, gestational age, clinical manifestations, physical examination findings, serum HCG, ultrasonographic findings, estimated intra-operational blood loss, blood transfusion, hospitalization stay, time of resumption of menstruation were collected from electronic medical records and telephone interviews.
High-intensity focused ultrasound ablation
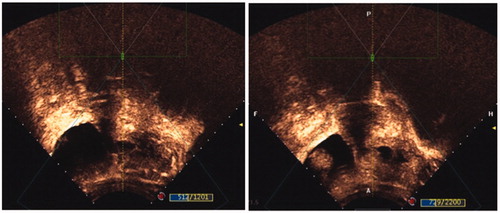
The procedure of HIFU was similar to the procedure we used to treat Cesarean scar pregnancy as described in our previous publication [Citation7]. In brief, after conscious sedation with fentanyl and midazolam via the peripheral vein, the patient was positioned prone on the HIFU system (JC-200 focused ultrasound tumor therapeutic system, Chongqing Haifu Medical Technology Co., Ltd., Chongqing, China). We used real-time ultrasonography to confirm the location of the gestational sac and to monitor the response to HIFU. The ultrasound waves produced by the HIFU treatment system penetrated the abdominal wall and focused at the gestational tissue. Coagulative necrosis of the targeted tissue occurred when the temperature increased. When the gray-scale change at the target tissue appeared or when the signal of the blood flow of the gestational sac disappeared, the treatment was considered complete (). The energy used was 400 W.
Suction curettage under hysteroscopic guidance
Suction curettage under hysteroscopic guidance was performed by experienced gynecologists. After general anesthesia, the location of the pregnancy tissue and the uterine cavity were visualized using a diagnostic hysteroscopy. Next, suction curettage was performed to detach the pregnancy tissues from the cervical canal. The hysteroscope was used again to detect any retained pregnancy tissues. If necessary, it was used to remove the retained pregnancy tissues and stop bleeding from the wound surface by electrocoagulation. The specimens were sent for pathological examination.
Follow-up
Potential complications included lower abdominal pain, fever, skin burn, and radiating pain in the lower limbs during or after the procedure were recorded. The patients were advised to check serum HCG once a week after surgery until HCG normalization. The time of the patients’ resumption of menstruation and the subsequent pregnancy outcome in patients desiring pregnancy was followed up with telephone interviews.
Results
Case 1
A 29-year-old pregnant woman (gravida 3, para 2) with ultrasonographic diagnosis of cervical pregnancy was seen at our hospital. According to her last menstrual period, the gestational age was six weeks. Transvaginal ultrasound scan revealed a 19 × 13 × 8 mm sized gestational sac in the cervix with active cardiac motion and no evidence of intrauterine pregnancy. The serum β-human chorionic gonadotropin (β-hCG) was 32506 mUI/mL. The cervix was inspected with a bivalve speculum during gynecologic examination and findings were unremarkable. She was treated with HIFU. Ultrasound showed that the fetal cardiac activity disappeared after HIFU. One day after the HIFU, suction curettage under hysteroscopic guidance was then performed. Hysteroscopic examination revealed the gestational sac was located in the posterior wall of the cervical canal. The estimated blood loss was 20 ml. One day after the surgery, the serum β-hCG was significantly declined to a value of 8758 mUI/mL. Thirty-two days after the treatment, the woman resumed her regular menstrual cycles. No obvious complications of HIFU were observed in this case. This patient did not attempt to conceive after the treatment.
Case 2
A 27-year-old woman (gravida 3, para 1) at 6 weeks + 2 days of gestation was referred to our department for vaginal bleeding. A transvaginal ultrasound scan demonstrated a gestational sac (21 × 18 mm) with a positive fetal heartbeat located in the endocervical canal. The serum β-hCG was 24789 mUI/mL and the hemoglobin was 12.2 g/dL. After written informed consent was obtained, the patient underwent HIFU. Ultrasound showed that the fetal cardiac activity disappeared after HIFU. One day after this procedure, hysteroscopic examination revealed the gestational sac was located in the posterior wall of the cervical canal. Suction curettage under hysteroscopic guidance was successfully performed with an estimated blood loss of 10 ml. Within 48 h, the serum β-hCG decreased to 6896 mUI/mL. The patient resumed a normal menstruation cycle 30 days later. No complications associated with HIFU (such as fever, skin burn, and radiating pain in the lower limbs) were observed during the follow-up period. This patient did not attempt to conceive after the treatment.
Case 3
In Case 3 (gestational age 8 weeks + two days according to last menstrual period) the patient was 43 years old and hospitalized after ultrasound detection of a CP. Transvaginal ultrasound scan revealed a 9 × 8 mm sized gestational sac in the cervix without active cardiac motion. The serum β-hCG was 9752 mUI/mL. After HIFU, the blood flow in the pregnancy tissue significantly decreased. The serum β-hCG declined to a value of 7872 mUI/mL one day after HIFU. Suction curettage under hysteroscopic guidance was performed on the third day after HIFU. No obvious vaginal bleeding or discharge was encountered during the surgery. The estimated blood loss was 10 ml. One day after the surgery, the serum β-hCG was significantly declined to a value of 3713 mUI/mL and the patient was discharged from the hospital. Forty-five days after the procedure, the patient resumed regular menstrual cycles. This patient did not attempt to conceive during the follow-up period.
Discussion
High-intensity focused ultrasound as a non-invasive treatment has been used in the treatment of Cesarean scar pregnancy with many advantages [Citation8]. However, to the best of our knowledge, no study has been performed to research the efficacy and safety of HIFU in the management of cervical pregnancy. In this report, we present three cases of cervical pregnancy in which high-intensity focused ultrasound was performed as a prophylactic procedure before suction curettage. Considering our previous experience of using HIFU in cesarean scar pregnancy with positive results, we hypothesized that HIFU has its advantages in treating cervical pregnancy. Through HIFU procedure, the ultrasound waves produced by the HIFU treatment system penetrated the abdominal wall and focused at the gestational tissue. The waves were converted to thermal energy. Coagulative necrosis of the targeted tissue occurred when the temperature increased to over 65 °C. HIFU can also destroy small vessels with a diameter <2 mm. Therefore, HIFU could be used to kill gestational tissues and destroy small blood vessels around the gestational tissues. Consequently, HIFU may help reduce the risk of hemorrhage during the procedure of suction curettage. Our results showed that the estimated blood loss during the procedure was 10 ∼ 20 ml. These case reports show that cervical pregnancy can be successfully treated with HIFU combined with suction curettage under hysteroscopic guidance with minimal risk of hemorrhage. Followup with the patients indicated that the menstruation recommenced after about 30–45 days and the serum hCG level returned to normal within about two to three weeks after suction curettage, which suggests that the uterine function was preserved.
There are several other treatments for CP [Citation2,Citation3,Citation9–13]. MTX has been systemically administrated for the treatment of CP [Citation14]. However, a high level of HCG (>5000 mIU/ml) and/or the presence of a gestational sac with fetal cardiac activity are contraindications to the systemic use of MTX for CP management. Yamaguchi et al. reported 15 CP patients treated with local MTX injection under transvaginal ultrasonography [Citation4]. Three patients required an additional local MTX injection and one patient required UAE to control persistent vaginal bleeding. Fylstra et al. have shown that 13 consecutive first-trimester cervical pregnancies were successfully treated with suction curettage using a cervical canal balloon [Citation15]. Uterine artery embolization (UAE) is another option for patients with CP, but severe side effects such as infertility, infection, and ovarian dysfunction may occur after UAE. Our study suggests that HIFU as a non-invasive treatment may have some advantages.
Even though HIFU is known to have some adverse effects, including lower abdominal pain, low-grade fever, skin burn, and radiating pain in the lower limbs, the incidence of severe adverse effects is very low [Citation16]. In these three cases, no obvious complications were observed with this procedure. Furthermore, for these cases, no additional chemotherapy was needed and no uterine bleeding occurred after the suction curettage.
The limitations of our study included a small number of patients and the lack of a control group. In addition, the patients in this study did not attempt to conceive after the treatment, it was not yet known about the effect of this treatment on fertility.
Conclusion
HIFU, combined with suction curettage under hysteroscopic guidance, seems to be effective for patients with cervical pregnancy during the first trimester, who requests to preserve their uterus. This procedure has the potential to minimize the risk of hemorrhage. Further experiences are needed to validate this new combined conservative approach in the treatment of cervical pregnancy.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Hosni MM, Herath RP, Mumtaz R. Diagnostic and therapeutic dilemmas of cervical ectopic pregnancy. Obstet Gynecol Surv. 2014;69:261–276.
- Bianchi P, Salvatori MM, Torcia F, et al. Cervical pregnancy. Fertil Steril. 2011;95:2123.e3–2124.
- Timor-Tritsch IE, Monteagudo A, Bennett TA, et al. A new minimally invasive treatment for cesarean scar pregnancy and cervical pregnancy. Am J Obstet Gynecol. 2016;215:351.e1–358.
- Yamaguchi M, Honda R, Erdenebaatar C, et al. The treatment of cervical pregnancy with ultrasound-guided local methotrexate injection. Ultrasound Obstet Gynecol. 2017;50:781–787
- Atallah A, Lacalm A, Massoud M, et al. Prenatal diagnosis of pericallosal curvilinear lipoma: specific imaging pattern and diagnostic pitfalls. Ultrasound Obstet Gynecol. 2018;51:269–273
- Hu J, Tao X, Yin L, et al. Successful conservative treatment of cervical pregnancy with uterine artery embolization followed by curettage: a report of 19 cases.Int J Obstet Gynecol. 2016;123:97–102.
- Zhu X, Deng X, Wan Y, et al. High-intensity focused ultrasound combined with suction curettage for the treatment of cesarean scar pregnancy. Medicine. 2015;94:e854.
- Huang L, Du Y, Zhao C. High-intensity focused ultrasound combined with dilatation and curettage for Cesarean scar pregnancy. Ultrasound Obstet Gynecol. 2014;43:98–101.
- Junior JE, Musiello RB, Araujo JE, et al. Conservative management of cervical pregnancy with embryonic heart activity by ultrasound-guided local injection: an eight case series. J Matern Fetal Neonatal Med. 2014;27:1378–1381.
- Matteo M, Nappi L, Rosenberg P, et al. Combined medical-hysteroscopic conservative treatment of a viable cervical pregnancy: a case report. J Minim Invasive Gynecol. 2006;13:345–347.
- De La Vega GA, Avery C, Nemiroff R, et al. Treatment of early cervical pregnancy with cerclage, carboprost, curettage, and balloon tamponade. Obstet Gynecol. 2007;109:505–507.
- Kofinas JD, Purisch SE, Brandt JS, et al. Hysteroscopic removal of cervical ectopic pregnancy following failed intramuscular/intra-sac methotrexate: a case report. J Gynecol Surg. 2012;28:369–371.
- Stefanovic M, Vukomanovic P, Kutlesic R, et al. Intra-amnial methotrexate in cervical pregnancy treatment. Clin Exp Obstet Gynecol. 2016;43:125–127.
- Masuda H, Endo T, Yoshimasa Y, et al. A case of hysteroscopic resection of cervical pregnancy after successful treatment with systematic methotrexate. J Obstet Gynaecol. 2016;18:1–2.
- Fylstra DL. Cervical pregnancy: 13 cases treated with suction curettage and balloon tamponade. Am J Obstet Gynecol. 2014;210:581.e1–585.
- Chen J, Chen W, Zhang L, et al. Safety of ultrasound-guided ultrasound ablation for uterine fibroids and adenomyosis: a review of 9988 cases. Ultrason Sonochem. 2015;27:671–676.