Abstract
Objective: This study evaluated the effect of oxytocin administration prior to microwave ablation (MWA) of hypervascular uterine fibroids.
Methods: Thirty-two patients with 38 hypervascular uterine fibroids (Adler blood flow grade 3) were equally apportioned to receive intravenous oxytocin infusion (0.32 U/min) 20 min before ultrasound-guided percutaneous MWA, or no oxytocin (control). Changes in Adler blood supply grade and myoma volume were observed via color Doppler ultrasonography (CDU). All patients underwent quantitative ablation with single or double needle and microwave power 50 W (180 s). Treatment continued for those who did not reach the therapeutic goal. The myoma necrotic volume was evaluated by contrast-enhanced ultrasound. Ablation rate was the percent of MRI nonenhanced myoma volume after treatment, relative to myoma volume before treatment, 2 days after surgery.
Results: Twenty minutes after oxytocin administration, CDU showed significant decrease of blood vessels in myomas, and Adler blood supply decreased from grade 3 to grade 1 or grade 0 in 10 and 9 myomas, respectively. Myoma volumes were reduced by 2.12 ± 0.24%. Necrotic volumes in the oxytocin (control) groups were 36.96 ± 2.78 cm3 (22.68 ± 3.38 cm3) and ablation rates were 95.4 ± 2.7% (85.7 ± 3.3%; t = 12.68, 8.866, p = 0.001, both). No serious complication was noted.
Conclusion: Intravenous oxytocin administered before percutaneous MWA of hypervascular uterine fibroids can effectively block the blood supply vessels of the myoma, reduce the heat sink effect, and thereby increase the ablation volume and improve the local therapeutic effect.
Introduction
Uterine fibroids are the most common benign lesion in the female reproductive system. The rate of incidence n women of childbearing age is 20–25%. They are the main cause of abnormal menstrual flow, anemia, chronic pelvic pain, infertility and frequent urination [Citation1]. With general improvements in people’s quality of life and health awareness, patients have come to expect effective and minimally invasive treatment of uterine fibroids, with uterine preservation.
Treatment options for uterine fibroids may be medical, surgical or nonsurgical. Medical methods can be hormonal or nonhormonal; surgeries include myomectomy and hysterectomy. The available non-surgical treatments are uterine artery embolization (UAE), and image-guided local thermal ablation. In the former, patients are exposed to X-ray radiation. Common complications include postoperative pain, postembolization syndrome and infection, while premature ovarian failure and endometrial atrophy are rarer [Citation2].
Image-guided local thermal ablation includes high-intensity focused ultrasound (HIFU), microwave ablation (MWA) and radiofrequency ablation (RFA). HIFU is noninvasive and local [Citation3], but may be less effective for treating large uterine fibroids [Citation4].
Medical imaging-guided MWA and RFA are minimally invasive thermal techniques that are feasible and safe, with fewer complications, strong reproducibility and definite curative effect. They have been widely used in the treatment of liver, kidney, thyroid and lung tumors [Citation5–8]. A previous study reported that the indications and clinical efficacy of MWA and RFA were comparable for hepatocellular carcinoma [Citation9].
Ultrasound-guided percutaneous MWA is an easy and fast procedure [Citation10] that in recent years has been used to treat uterine fibroids and adenomyosis. Reports are that, for uterine fibroids, the percent volume of the non-enhanced field in the lesion after ablation relative to the volume before ablation (i.e., the ablation rate) ranges from 64.9 to 100% [Citation11,Citation12]. However, all these investigations focused on the changes in the fibroid volume, whereas the ablation effect on blood supply of the fibroid was not addressed.
A heat sink effect in thermal ablation occurs when the blood supply around or inside the tumor is abundant, and the blood flow carries away the local heat generated by the MWA or RFA. This can mean that the tissue around the blood vessel is not sufficiently heated, the temperature rises slowly, and ultimately the tissue is not completely ablated [Citation13]. Therefore, the question remains whether using a chemical blockade before treatment to reduce the blood supply of tumors will improve the ablation effect. Previous studies found that the blood perfusion of uterine fibroids could be significantly reduced by administration of oxytocin [Citation14]. This could significantly decrease the energy required for ablating the uterine fibroids, shorten treatment time and improve treatment efficiency [Citation15].
The present preliminary prospective study investigated whether the use of oxytocin prior to MWA of uterine fibroids with abundant blood supply could improve the efficacy of MWA.
Methods
Research subjects
The research treatment protocol was approved by the ethics committee of the hospital. All patients provided informed signed consent prior to surgery.
Patients between May 2016 and May 2018 who met the International Federation of Gynecology and Obstetrics (FIGO) classification for uterine fibroids grades 1–6 were selected. All received diagnoses, in our hospital or by our collaborator. The patients conformed to the following criteria: excessive menstruation, abdominal pain, low back pain, anemia or oppression of adjacent organs; Adler blood supply grade 3 [Citation16]; and fibroid diameter and volume 4.5–7.5 cm and 47.6–220.8 cm3, respectively. In addition, none of the patients sought to maintain fertility, and all refused surgical excision or other treatment methods.
Patients with any of the following were excluded from this study: severe acute or chronic heart, brain or lung disease; suspicious malignant tumors such as uterine sarcoma, endometrial cancer or other malignant tumors; previously received local thermal ablation or interventional therapy; or uterine fibroids category 0 or 7 under FIGO classification.
The qualified patients were equally apportioned to receive oxytocin (oxytocin group) or not (control group) by random allocation. The patient groups were matched with regard to volume and number of fibroids.
Study characteristics
Thirty-nine patients met the inclusion criteria, but seven were excluded according to the exclusion criteria. Thus, 32 patients (38 myomas) were included in this study. Paired design grouping based on the principle of equal size and number of myomas led to two groups of 16 patients each (each group with 19 fibroids, of which 13 were single myoma and 3 were double myoma). The mean ages of patients in the oxytocin and control groups were 38.3 ± 4.3 and 39.2 ± 4.1 years, respectively. The mean diameters of the myomas were 5.6 ± 0.82 and 5.6 ± 0.81 cm, and mean volumes were 89.6 ± 36.7 and 89.9 ± 37.3 cm3. Of the 19 myomas in the oxytocin and control groups, 14 were intramural (FIGO grades 2–5), 2 were subserosal (FIGO grade 6) and 3 were submucosal (FIGO grade 1). The study characteristics of both groups were comparable at baseline. Baseline was defined as the demographic and clinical data collected for each participant at the beginning of study before intervention. There were no significant differences between the groups (p > 0.05; ).
Table 1. Characteristics of patients in both treatment groups.
Preoperative preparation
For all patients who underwent preoperative pelvic magnetic resonance imaging (MRI), the size, shape, location and surrounding tissues and organs of the fibroids were observed. The diameter of the fibroids was calculated as (length + width + height)/3. The volume of the fibroids was defined as 4/3πr3, where r = mean radius of the myoma.
Uterine fibroids were observed using color Doppler ultrasound (CDU). Blood flow signals were adjudged according to Adler blood supply grade [Citation16], as follows: 0, no blood flow signal; I, stellate blood flow signals (diameter <1 mm); II, short strip blood flow signals (number of blood vessels ≤3); III, >4 blood vessels or vessels were interwoven into a network in the myoma. Routine blood and biochemical examination, serum lactate dehydrogenase examination, and routine ultrasound-guided 18 G cutting needle biopsy (HS Hospital Service S.P.A., Roma, Italy) were performed. The biopsy success rate was 100%. Patients were fasted 12 h before surgery. Skin preparation at the pubic symphysis was performed and urinary catheter was indwelled 1 h before surgery.
Application of oxytocin
For the oxytocin group, oxytocin 80 U (Hepatunn, Chengdu, P. R. China) was added into 500 ml physiological saline solution, and administered by intravenous drip at a rate of 2 ml/min (0.32 U/min) 20 min before MWA. The control group was administered with 500 ml physiological saline.
Equipment
For MWA, a MWA therapeutic instrument was used (KY 2000, Nanjing Yigao Microwave System Engineering, Nanjing, P. R. China) with the following features: frequency 2450 MHz; low-temperature water circulation cooling system 14 G electrode needle; and front-end microwave radiator, 1.0 cm. The puncture guidance device was a CDU diagnostic instrument (GE LOGIQ-E9, GE Healthcare, Chicago, IL), probe model L2-5 MHz. Sulfur hexafluoride microbubbles (Bracco Imaging SpA, Milan, Italy) were used as an ultrasound contrast agent. The contrast agent was dissolved in 5.0 ml of sodium chloride solution (0.9%) w/v and after mixing, 2.4 ml of intravenous injection was used each time. The MRI equipment was from Centauri (1.5 T, Altech Medical Systems, Chengdu, P. R. China). The contrast agent gadodiamide (GE Healthcare, Chicago, IL), 0.3 mmol/kg at 2.0 ml/s, was used for enhanced MRI.
Anesthesia and assisting techniques
Anesthesia was applied using local 1.0% lidocaine (Shandong Hualu Pharmaceutical, Shandong, P. R. China) combined with intraoperative intravenous sufentanil (Yichang Humanwell Pharmaceutical, Hubei, P. R. China; 0.2–0.3 µg/kg, starting dose at 0.2 µg/kg, intravenous slow injection). Artificial ascites was produced to assist ablation of the myoma adjacent to the intestine or bladder, and 500–800 ml of physiological saline was injected into the pelvic cavity before treatment to isolate the intestine and bladder. A central venous catheter was introduced via ultrasound guidance pelvic puncture, and 0.9% sodium chloride solution was injected into the catheter under real-time ultrasound monitoring. The injection was stopped when the ultrasound showed that the uterus was separated from the surrounding intestinal tract. Before treating the submucosal fibroids, an 8.0 Fr catheter was inserted into the uterine cavity and 5.0 ml of physiological saline was injected to protect the endometrium. There were 14 patients (7 in each group) in whom artificial ascites had to be induced. Overall, the success rate at the first attempt was 100%.
Microwave therapy
According to the lesion site, the nearest location of myoma to the abdominal wall was chosen as the puncture point. The operative area was routinely disinfected and covered with a clean towel. The probe was covered with a sterile protective sheath. The microwave electrode was inserted into the myoma under ultrasound guidance and the electrode needle was inserted along the central axis of the lesion. After needle placement, the water-cooled catheter and microwave cable were connected, the power was set at 50 W, and time was set to 180 s for quantitative ablation. After stopping ablation for 5 min, contrast-enhanced ultrasonography (CEUS) was performed and the range of non-perfusion area was measured.
After CEUS was complete, treatment was continued for patients in both groups who did not achieve the treatment goal after quantitative ablation. Quantitative ablation was defined as quantitative assessment of MWA fibroid coverage by 50 W × 180 s. The mean diameter of myoma in both groups was 4.5–7.5 cm, the mean volume was 47.6–220.8 cm3. Thus the minimum volume of myoma was larger than the volume of quantitative ablation, and the ablation time of both groups was longer than the initial (quantitative ablation) time. The primary therapeutic goal of the ablation was based on the echogenic changes covering the fibroid area. The end indication was changes of the myoma from hypoechoic before treatment to diffuse hyperechoic. The main indicator of the end of ablation in both groups was uniform hyperechogenicity of the myoma.
Ultrasound was used to monitor the myoma changes. The microwave radiation was stopped when the hyperechoic area reached the edge of the myoma. Myomas with a mean diameter ≤5.0 cm were treated by single needle therapy. Otherwise, myomas were treated with double needle therapy, with the distance between two needles ranging from 1.0 to 1.5 cm. In both the oxytocin group and control group, 6 fibroids were treated with single needle, and 13 fibroids were treated with double needle. Respiration, blood pressure, electrocardiogram and oxygen saturation were monitored during the procedure. Pelvic contrast-enhanced MRI was performed 2 days afterward.
Observation indicators
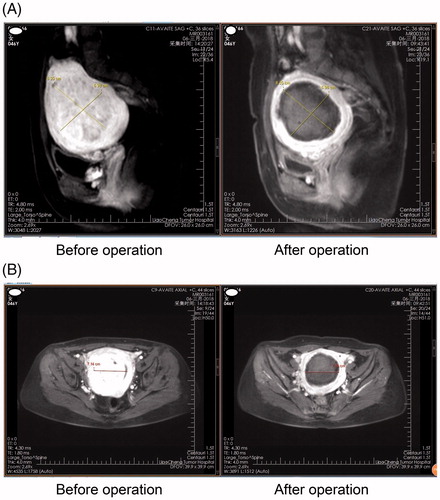
CDU was used to observe changes in intrauterine vessels and myoma volume before and after oxytocin infusion in the oxytocin group. The rate of reduction of myoma was calculated as [(myoma volume before treatment—myoma volume after treatment)/myoma volume before treatment] × 100%. CEUS was used to assess the necrotic volume of myomas in both groups after quantitative ablation. Contrast-enhanced MRI was used to evaluate the ablation rate of myoma in the two groups before and after surgery (). The ablation rate of myoma was calculated as: (MRI non-enhanced myoma volume after treatment/myoma volume before treatment) × 100%. Adverse reactions during and after surgery were observed.
Statistical analysis
All data were analyzed with SPSS 19.0 statistical software (SPSS, Chicago, IL). The results were presented as mean ± standard deviation. Comparisons between groups were determined with the paired t-test, while categorical data were compared with chi-squared test. p < 0.05 was considered statistically significant.
Results
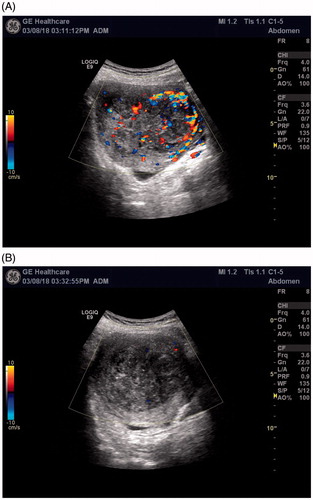
Changes in CDU after oxytocin infusion in the oxytocin group
After 20 min of intravenous oxytocin infusion, the mean volume of the uterine fibroids decreased slightly from 89.6 ± 36.7 cm3 before infusion to 86.6 ± 33.7 cm3, with a mean reduction of 2.12 ± 0.24%. CDU showed that the Adler blood supply grading of the 19 hypervascular fibroids decreased from grades 3 to 1 in 10 myomas, and to grades 0 in 9 myomas ().
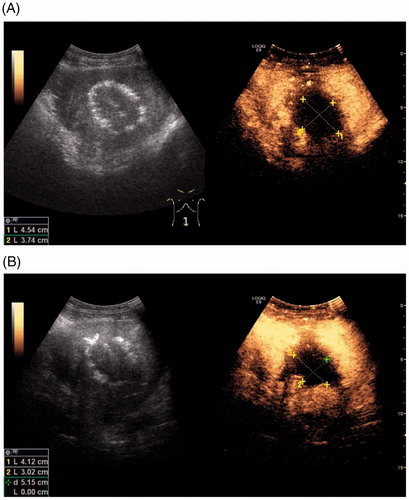
Quantitative MWA
The technical success rate of ultrasound-guided myoma puncture in both groups was 100%. After quantitative ablation, CEUS showed different degrees of filling and missing areas, which indicated coagulative necrosis of the myoma (). The volume of coagulative necrosis in the oxytocin group was significantly larger than that of the control group ().
Table 2. Results of quantitative ablation (50 W × 180 s) of myoma in both groups.
The final therapeutic effect of both groups
In both groups, treatment was continued for patients who did not reach the therapeutic goal after quantitative ablation. By the end of treatment, the ablation time of the control group (485 ± 79 s) was significantly longer than that of the oxytocin group (362 ± 55 s; t = 15.2669, p = 0.000). On the second postoperative day, contrast-enhanced MRI showed that the ablation rate of myoma in the oxytocin group (95.4 ± 2.7%) was significantly higher than that of the control group (85.7 ± 3.3%; t = 8.866, p = 0.001).
Adverse reactions
In the oxytocin group, four drug-related adverse reactions occurred, including one case of prickling precordial pain, and three cases of facial flushing, increased heart rate and dizziness that were alleviated after slowing the oxytocin drip rate. There were six cases of adverse reactions related to microwave therapy during the procedure, all of which involved lower abdominal distension and pain, and which disappeared after treatment. In the control group, there were five cases of lower abdominal distension and pain, and no adverse drug reactions occurred. All cases of abdominal pain in both groups were treated with sufentanil 0.1 µg/kg by the anesthesiologist via slow intravenous injection, and the pain was significantly relieved. Vaginal secretions (fluid discharge from the vagina) occurred in both groups after ablation, including eight and six cases in the oxytocin and control groups, respectively. All vaginal secretions consisted of a small amount of light yellow or bloody fluid. Patients were advised to clean the perineum and take prophylactic anti-inflammatory drugs orally for 5 days, and all vaginal secretions resolved after 6–21 days.
Discussion
Effect of oxytocin on uterine fibroids
Oxytocin is a nonpeptide hormone secreted by the hypothalamus, which has been widely used worldwide to induce labor. Intravenous oxytocin infusion during myomectomy can significantly reduce intraoperative blood loss [Citation17,Citation18], indicating that it has a contractile effect on the non-pregnant uterus. Uterine fibroids are estrogen-dependent tumors, and the estrogen level is often higher in patients with uterine fibroids [Citation19]. High estrogen levels increase the sensitivity of oxytocin binding to its receptor [Citation20], resulting in contraction of uterine smooth muscle via an increase of intracellular Ca2+ concentration in the myometrium [Citation21].
In this study, the uterine volume was reduced upon administration of intravenous oxytocin, and the Adler blood supply grade of the hypervascular fibroids decreased. This further confirmed that oxytocin affects uterine smooth muscle contraction, and promotes the contraction and reduction of blood vessels in fibroids.
Dose of oxytocin
Oxytocin is a commonly used drug in obstetrics for prevention and treatment of postpartum hemorrhage. However, due to its receptor saturation effect and large individual differences, large doses do not achieve better results, but can cause adverse reactions that affect hemodynamic stability [Citation22]. The effective dose of intravenous oxytocin infusion in HIFU treatment of adenomyosis was previously reported as 0.32 U/min [Citation23]. Thus, a similar dosage was used in this study, and the adverse drug reactions were consistent with those already reported, which is, increased heart rate and hypotension. There were no serious adverse reactions. This further showed that application of oxytocin in MWA of uterine fibroids is safe and reliable.
Heat sink effect on the ablation rate of tumors
Goldberg et al. [Citation24] first confirmed the heat sink effect in RFA, in which the local heat generated by radio frequency is dissipated by the blood flow in the tumor. The intended thermal field is thus altered, and the temperature adjacent to the blood vessels of the tumor is insufficient for tissue coagulation and necrosis. The actual ablation range becomes smaller than expected, leading to incomplete ablation of the lesion and in situ recurrence [Citation25].
It is particularly important to study the temperature dynamics of the heat sink effect and explore ways to improve the one-time ablation rate of tumors. At present, there are physical and chemical methods for blocking the nourishing vessels of tumors. Intravascular interventional embolization is the commonly used physical method for treatment of malignant liver tumors [Citation26]. Intravenous infusion of vasoconstrictor drugs is used as a chemical method, and the commonly used drugs are pituitary vasopressin, adrenaline and oxytocin [Citation24].
A previous study [Citation27] reported that oxytocin administration in HIFU treatment of uterine fibroids can increase the fibroid necrosis rate and reduce operative time. In this study, the reduction in tumoral volume after quantitative ablation of the oxytocin group was significantly greater than that of the control group, and the operative time was significantly shorter and ablation rate significantly higher. Oxytocin was associated with reduced ablation time and improved ablation rate of myoma, and an apparent effective reduction in the heat sink effect during MWA.
Potential advantages of MWA
UAE has been demonstrated effective to treat hypervascular fibroids [Citation28], but fibroid recurrence is possible, with approximately 20% of patients subsequently requiring hysterectomy [Citation29]. HIFU is the only completely noninvasive ablation technique available to date. However, it can be time consuming, especially for large and hypervascular nodules [Citation4,Citation10,Citation30–32]. RFA often require the aid of laparoscopy, which is invasive [Citation33,Citation34]. Previous studies showed that RFA is only effective for fibroids with volume ≤75 cm3; there was no significant improvement in symptoms for fibroids with larger volume, but a high rate of reoperation [Citation33,Citation35]. The potential advantages of MWA include consistently higher intratumoral temperatures, larger tumor ablation volumes, faster ablation times, use of multiple applicators, and less procedural pain [Citation10]. Percutaneous puncture under ultrasound guidance makes the puncture easier and more accurate.
Matters requiring attention
Ultrasound-guided percutaneous MWA of uterine fibroids has a real-time display, allows dynamic observation, and the operation is relatively simple. However, the following points should be noted: After application of oxytocin, the uterus contracts and the texture become stiff. When puncturing the uterus or myoma, the uterus may retract and slip. Thus, puncturing the uterus or myoma with the ablation needle should be rapid and forceful.
This is a prospective preliminary study. The myoma regression rate after MWA has not been reported, and further follow-up reports will be forthcoming. A large sample study and long-term follow-up is warranted to evaluate the long-term efficacy and treatment effect on fertility with this method.
Conclusion
Percutaneous MWA combined with intravenous oxytocin application in the treatment of hypervascular uterine fibroids can effectively reduce or block the blood supplying vessels of the myoma, reduce the heat sink effect during the ablation process, and thereby increase the ablation rate of myoma and reduce ablation time.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The datasets generated and analyzed during the present study are available from the corresponding author on reasonable request.
References
- Coyne KS, Soliman AM, Margolis MK, et al. Validation of the 4 week recall version of the uterine fibroid symptom and health-related quality of life (UFS-QOL) questionnaire. Curr Med Res Opin. 2017;33:193–200.
- Chittawar PB, Kamath MS. Review of nonsurgical/minimally invasive treatments and open myomectomy for uterine fibroids. Curr Opin Obstet Gynecol. 2015;27:391–397.
- Lee JS, Hong GY, Park BJ, et al. Ultrasound-guided high-intensity focused ultrasound treatment for uterine fibroid & adenomyosis: a single center experience from the Republic of Korea. Ultrason Sonochem. 2015;27:682–687.
- Ren XL, Zhou XD, Zhang J, et al. Extracorporeal ablation of uterine fibroids with high-intensity focused ultrasound: imaging and histopathologic evaluation. J Ultrasound Med. 2007;26:201–212.
- Liu SR, Liang P, Yu XL, et al. Percutaneous microwave ablation for liver tumours adjacent to the marginal angle. Int J Hyperthermia. 2014;30:306–311.
- Zhou W, Arellano RS. Thermal ablation of T1c renal cell carcinoma: a comparative assessment of technical performance, procedural outcome, and safety of microwave ablation, radiofrequency ablation, and cryoablation. J Vasc Interv Radiol. 2018;29:943–951.
- Shen Y, Liu M, He J, et al. Differences in treatment outcomes between ultrasound-guided percutaneous microwave ablation and endoscopic thyroidectomy for patients with papillary thyroid microcarcinoma: protocol for a systematic review and meta-analysis. Medicine (Baltimore). 2019;98:e13953.
- Yang X, Ye X, Zhang L, et al. Microwave ablation for lung cancer patients with a single lung: clinical evaluation of 11 cases. Thorac Cancer. 2018;9:548–554.
- Vietti Violi N, Duran R, Guiu B, et al. Efficacy of microwave ablation versus radiofrequency ablation for the treatment of hepatocellular carcinoma in patients with chronic liver disease: a randomised controlled phase 2 trial. Lancet Gastroenterol Hepatol. 2018;3:317–325.
- Zhang J, Feng L, Zhang B, et al. Ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroid treatment—a clinical study. Int J Hyperthermia. 2011;27:510–516.
- Liu H, Zhang J, Han ZY, et al. Effectiveness of ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroids: a multicentre study in China. Int J Hyperthermia. 2016;32:876–880.
- Turtulici G, Orlandi D, Dedone G, et al. Ultrasound-guided transvaginal radiofrequency ablation of uterine fibroids assisted by virtual needle tracking system: a preliminary study. Int J Hyperthermia. 2018;35:97–104.
- Ringe KI, Lutat C, Rieder C, et al. Experimental evaluation of the heat sink effect in hepatic microwave ablation. PLoS One. 2015;10:e0134301.
- Wang Y, Ren D, Wang W. The influence of oxytocin on the blood perfusion of uterine fibroids: contrast-enhanced ultrasonography evaluation. J Med Ultrasound. 2016;24:13–17.
- Huang X, He M, Liu YJ, et al. Effect of oxytocin on uterine fibroids treated by ultrasound ablation. Zhonghua Fu Chan Ke Za Zhi. 2011;46:412–415.
- Adler DD, Carson PL, Rubin JM, et al. Doppler ultrasound color flow imaging in the study of breast cancer: preliminary findings. Ultrasound Med Biol. 1990;16:553–559.
- Wang CJ, Lee CL, Yuen LT, et al. Oxytocin infusion in laparoscopic myomectomy may decrease operative blood loss. J Minim Invasive Gynecol. 2007;14:184–188.
- Zhang R, Shi H, Ren F, et al. Assessment of carboprost tromethamine for reducing hemorrhage in laparoscopic intramural myomectomy. Exp Ther Med. 2015;10:1171–1174.
- Sun X, Mittal K. MIB-1 (Ki-67), estrogen receptor, progesterone receptor, and p53 expression in atypical cells in uterine symplastic leiomyomas. Int J Gynecol Pathol. 2010;29:51–54.
- Ochedalski T, Subburaju S, Wynn PC, et al. Interaction between oestrogen and oxytocin on hypothalamic-pituitary-adrenal axis activity. J Neuroendocrinol. 2007;19:189–197.
- Simoes-Wust AP, Graos M, Duarte CB, et al. Juice of Bryophyllum pinnatum (Lam.) inhibits oxytocin-induced increase of the intracellular calcium concentration in human myometrial cells. Phytomedicine. 2010;17:980–986.
- Dupont C, Carayol M, Le Ray C, et al. Oxytocin administration during spontaneous labour: guidelines for clinical practice. Guidelines short text. Gynecol Obstet Fertil Senol. 2017;45:56–61.
- Zhang X, Zou M, Zhang C, et al. Effects of oxytocin on high intensity focused ultrasound (HIFU) ablation of adenomysis: a prospective study. Eur J Radiol. 2014;83:1607–1611.
- Goldberg SN, Hahn PF, Tanabe KK, et al. Percutaneous radiofrequency tissue ablation: does perfusion-mediated tissue cooling limit coagulation necrosis?. J Vasc Interv Radiol. 1998;9:101–111.
- Thanos L, Mylona S, Galani P, et al. Overcoming the heat-sink phenomenon: successful radiofrequency thermal ablation of liver tumors in contact with blood vessels. Diagn Interv Radiol. 2008;14:51–56.
- Hou YB, Chen MH, Yan K, et al. Adjuvant percutaneous radiofrequency ablation of feeding artery of hepatocellular carcinoma before treatment. World J Gastroenterol. 2009;15:2638–2643.
- Lozinski T, Filipowska J, Krol P, et al. Oxytocin administration in high-intensity focused ultrasound treatment of myomata. Biomed Res Int. 2018;2018:1.
- Sconfienza LM, Lacelli F, Gandolfo N, et al. Contrast-enhanced ultrasound (CEUS) assessment of superselective uterine fibroid embolization (SUFE): preliminary experience. J Ultrasound. 2008;11:158–161.
- Gabriel-Cox K, Jacobson GF, Armstrong MA, et al. Predictors of hysterectomy after uterine artery embolization for leiomyoma. Am J Obstet Gynecol. 2007;196:588.e1–e6.
- Mikami K, Murakami T, Okada A, et al. Magnetic resonance imaging-guided focused ultrasound ablation of uterine fibroids: early clinical experience. Radiat Med. 2008;26:198–205.
- Zhou XD, Ren XL, Zhang J, et al. Therapeutic response assessment of high intensity focused ultrasound therapy for uterine fibroid: utility of contrast-enhanced ultrasonography. Eur J Radiol. 2007;62:289–294.
- Ren XL, Zhou XD, Yan RL, et al. Sonographically guided extracorporeal ablation of uterine fibroids with high-intensity focused ultrasound: midterm results. J Ultrasound Med. 2009;28:100–103.
- Bergamini V, Ghezzi F, Cromi A, et al. Laparoscopic radiofrequency thermal ablation: a new approach to symptomatic uterine myomas. Am J Obstet Gynecol. 2005;192:768–773.
- Na BG, Kim JM, Oh DK, et al. Clinical outcomes of laparoscopic radiofrequency ablation of single primary or recurrent hepatocellular carcinoma (</=3 cm). Ann Surg Treat Res. 2017;92:355–360.
- Cho HH, Kim JH, Kim MR. Transvaginal radiofrequency thermal ablation: a day-care approach to symptomatic uterine myomas. Aust N Z J Obstet Gynaecol. 2008;48:296–301.