Abstract
Aim: To compare the effects of the liquid-isolating maneuver and the lever-elevating maneuver in protecting cervical structures during microwave ablation for treating high-risk benign thyroid nodules.
Methods: This prospectively study was approved by the Medical Ethics Committee of Panzhihua Central Hospital. A total of 174 patients were enrolled and randomly assigned to a liquid-isolating maneuver group (LIM, n = 87) or a lever-elevating maneuver group (LEM, n = 87). Operation time, postoperative voice change, time to recovery of baseline voice, peri-thyroid hematoma, neck tension, and intraoperative vasovagal reaction were assessed.
Results: Operation time was greater in the LIM group than in the LEM group (44.75 ± 13.14 vs. 32.87 ± 10.84 min; p = .017).Voice changes were observed in 6 patients in the LIM group and 2 in the LEM group (6.9% vs. 2.3%, p = .278). The time to recovery of baseline voice was significantly greater in the LIM group compared with the LEM group (36.15 ± 10.24 vs. 24.48 ± 11.53 days, p = .014). The incidences of peri-thyroid hematoma and neck tension were higher in the LIM than in the LEM group (11.5% vs. 3.4%, 10.3% vs. 2.3%, p = .044 and p = .029). One patient (1.1%) in the LEM group and none of the patients in the LIM group experienced a vasovagal response (p = 1.000).
Conclusion: The lever-elevating method is feasible and effective for the microwave ablation of benign thyroid nodules, with better protection of neck structures than observed with the liquid-isolating method.
Introduction
With the increased use of imaging technology, thyroid nodules are commonly detected [Citation1,Citation2]. Most nodules are benign and asymptomatic. Serial observation is usually recommended. Some benign nodules present with compressive symptoms and cosmetic concerns and require treatment [Citation1–5]. Thyroidectomy has been the main treatment for these nodules [Citation5–8]. In recent years, a number of minimally invasive non-surgical treatments have been widely used to treat thyroid nodules, including chemical ablation methods (e.g. alcohol injection) and thermal ablation methods (e.g. radiofrequency, microwave, laser, HIFU). These methods have been used to treat thyroid benign nodules with or without function, local recurrences of thyroid cancer, and cervical lymph node metastatic cancer [Citation2–5,Citation7,Citation9–11].
Thermal ablation helps in the treatment of benign thyroid nodules by reducing nodule volume,alleviating symptoms related to neck compression,mitigating the effects of trauma,improving patient appearance,and decreasing risk of complications. The incidence of total complications with use of thermal ablation ranges from 0.2% to 3.9%, which is lower than that of thyroidectomy (3–10%) [Citation4,Citation5,Citation10–14]. In particular, the incidence of injury to the recurrent laryngeal nerve during thermal ablation ranges from 0.5% to 1.2%,which was significantly lower than that of thyroidectomy (2.5–8.2%) [Citation10–12,Citation15–19]. In order to further decrease the risk of complications, additional research will be necessary to develop techniques to protect critical cervical structures such as the recurrent laryngeal nerve, trachea, esophagus, and cervical sympathetic trunk, et al. [Citation5,Citation12, Citation15,Citation20,Citation21].
Liquid-isolating technique, also known as hydrodissection, is widely used to protect vital tissue from thermal energy during image-guided ablation of thyroid nodules [Citation22]. The main idea of liquid isolation is to inject 0.9% saline into the spaces between the thyroid capsule and the anterior cervical muscles, blood vessels, trachea, and esophagus, thereby creating a liquid barrier that protects sensitive tissue from excessive heat.
The lever-elevating method, also named as the leverage pry-off method, is another technique used during the image-guided-ablation of thyroid nodules [Citation23]. This modality uses the electrode as leverage to increase the distance between vital tissues and nodules in order to protect them from excessive thermal energy [Citation24].
However, no study published to date has compared the lever-elevating method and the liquid-isolating method in terms of efficacy of protecting the vital tissues during the treatment of thyroid nodules.
Image-guided microwave ablation (MWA) is a safe and effective technique that has been widely used to treat benign thyroid nodules [Citation25,Citation26]. In this study, we prospectively compared the lever-elevating and liquid-isolating techniques for the MWA of thyroid nodules in terms of the risk of complications and clinical characteristics.
Materials and methods
Patients
This was a prospective, single-center, case-control study. The protocol for the study was approved by the Medical Ethics Committee of Panzhihua Central Hospital (No. S2016013). During the period from February 2016 to November 2018, a total of 174 patients with high-risk benign thyroid nodules were enrolled in the study and scheduled to undergo ultrasound-guided percutaneous MWA. Each patient provided his or her signed informed consent.
The subjects were enrolled according to the following inclusion and exclusion criteria. The inclusion criteria were: (1) pathological biopsy evidence that the patient’s thyroid nodule was benign; (2) distance from the edge of the thyroid nodule to the recurrent laryngeal nerve ≤ 0.2 cm. In addition to meeting both of these criteria for inclusion, each patient was required to meet one of the following conditions: (1) related symptoms such as pain, pressure, and/or foreign body sensation; (2) cosmetic effects of the thyroid nodule; (3) refusal to undergo surgery.
The exclusion criteria were: (1) evidence, obtained during follow-up, that the thyroid nodule was malignant; (2) distance from the edge of the thyroid nodule to the recurrent laryngeal nerve > 0.2 cm; (3) coagulopathy.
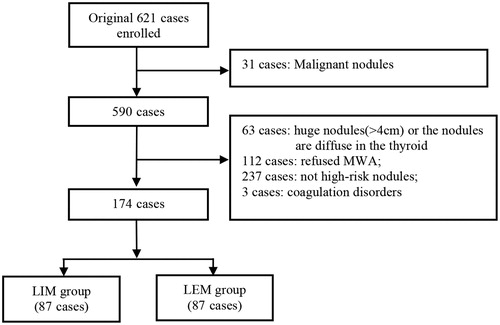
All patients underwent fine needle aspiration cytology prior to undergoing MWA. All operations were performed by a trained radiologist who had successfully performed thyroid MWA at least 30 times. The flow-chart for the study is shown in .
High-risk thyroid nodules
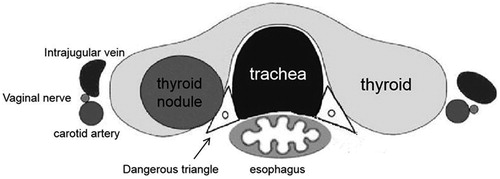
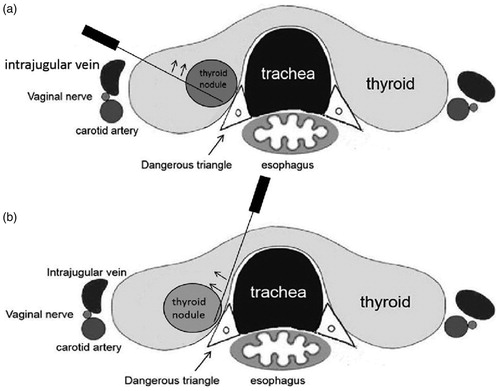
High-risk thyroid nodules are defined as nodules for which the distance between the thyroid nodule margin and the recurrent laryngeal nerve is ≤ 0.2 cm [Citation27]. Because ultrasonographic technology cannot distinguish the recurrent laryngeal nerve, we chose to use the shortest distance from the edge of the thyroid nodule to the edge of the “area of danger” triangle as an index for the distance to the recurrent laryngeal nerve. The triangular area of the thyroid risk triangle is bounded by the posterior medial edge of the thyroid capsule, the anterior lateral edge of the esophageal wall, and the outer edge of the tracheal wall ().
Microwave ablation procedure
The GE LOGIQ-E9 ultrasound system (General Electric≥ Healthcare, Wauwatosa, WI, USA) was used to determine the shape, size and location of the thyroid nodule and to guide MWA. MWA was performed with an ECO-100 microwave applicator (YI GAO Microwave System Engineering Co. Ltd, Nanjing, China) with a disposable microwave antenna (16 G, length 10 cm, active component 3 mm). The microwave antenna was internally cooled with normal saline. In the current study, the applied power setting was 35 W at a frequency of 2,450 MHz.
The procedure was performed with the patient in a supine position, under aseptic conditions, with local anesthesia (2% lidocaine). There are types of sites for insertion of the microwave antenna. With one approach, the antenna is inserted in a lateral region of the neck; with the second approach, the antenna is inserted along the neck midline (). In this study, the site to be used was determined by the position of the nodule. The microwave antenna is positioned in the deepest portion of the thyroid nodule under ultrasound guidance. A transient hyperechoic zone surrounding the microwave antenna is observed 3 ∼ 5 s after the MWA applicator is activated. The moving-shot technique [Citation28] was performed to ensure that the transient hyperechoic zone encompassed the entire tumor. For the nodules (≥2 cm), multi-slice and mobile ablation methods were used to cover the tumor entirely with the transient high-echo zone. Ultrasound was used to evaluate the progression of thyroid nodule ablation in real time. The thyroid nodule was examined using contrast-enhanced ultrasound immediately after ablation to determine whether ablation had been successfully completed (Supplementary Figure S1).
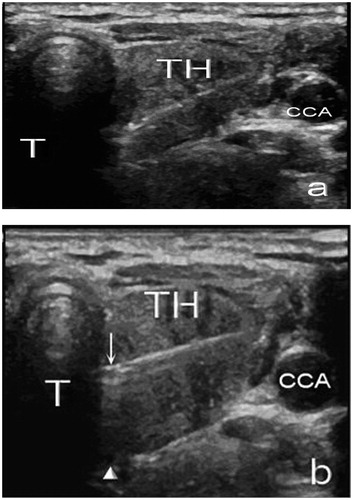
Figure 3. Two types of lever-elevating maneuvers were performed, as determined by the site to be used for insertion of the microwave needle. With one approach, the needle was inserted into a lateral region of the neck (a). With the trans-isthmic approach, the needle is inserted along the neck midline (b).
Lever-elevating and liquid-isolating technique
Liquid-isolating maneuver
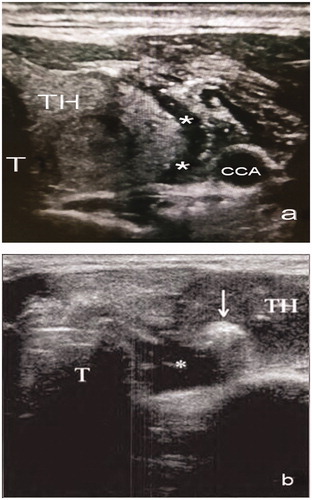
Before ablation, ultrasound guidance was used to inject a volume of 0.9% saline sufficient to fill the space between the anterior thyroid capsule and the anterior cervical muscle, between the thyroid lateral capsule and the carotid artery, between the posterior thyroid and the recurrent laryngeal nerve, and between the esophagus and the parathyroid gland. A liquid barrier (3–5 mm in width) was thus created to separate the thyroid gland from the tissues in order to protect the anterior cervical muscles, the carotid artery, the recurrent laryngeal nerve, the parathyroid gland, and the esophagus ().
Lever-elevating maneuver
Major benign thyroid nodule tissue is soft, without a tough wrap. If a lever-elevating maneuver is performed immediately, the microwave antenna cannot effectively lift the nodule because of the soft tissue. We therefore activated the microwave applicator when the microwave antenna reached the edge of the thyroid nodule, prior to preforming the lever-elevating maneuver. The tissue around the antenna subsequently became dehydrated and solidified. After a hyperechoic zone of sufficient size appears around the microwave antenna, the microwave antenna is lifted 0.2–0.3 cm (with the trachea or finger as the fulcrum) to increase the distance between the thyroid and surrounding structures, and ablation was performed. The moving-shot technique [Citation28] was performed to ensure that the transient hyperechoic zone encompassed the entire tumor.
There are two types of lever-elevating maneuvers, based on the site to be used for insertion of the microwave antenna (). depicts insertion of the antenna in a lateral region of the neck.
Variables
Information pertaining to operation time, postoperative voice changes, time to recovery of baseline voice, appearance of a hematoma, neck tension, and intraoperative vasovagal reaction were recorded and analyzed. Voice changes were assessed using voice handicap index-10/VHI-10 [Citation29]. A score > 4 points above baseline was defined as an anomaly, and a laryngeal examination was performed to assess vocal cord condition. Patients found to have vocal cord paralysis conducted a weekly self-assessment until the score had returned within four points of baseline. The laryngeal examination was performed again to determine the condition of the vocal cords 3 mo after ablation. Identification of a neck hematoma during or after surgery was taken as the discovery of a new heterogeneous mass in or adjacent to the thyroid gland or under the envelope. Neck tension was scored with the visual analog scale (VAS). Presence of a vasovagal reaction was recorded when a patient had dizziness, cold sweat, pale skin, decreased heart rate, and decreased blood pressure during the operation, but then quickly recovered.
Follow-up examination
Patients were followed up by the clinical technician on day 1, day 3, month 1, month 3, and month 6 after the procedure. Any complications that arose were documented.
Statistical analysis
SPSS software, version 17.0, was used for all statistical analyses. Continuous parameters are expressed as median and range, and categorical variables are expressed as number and percentage. The independent t test was used to compare continuous variables. Fisher’s exact test or Chi-square test was used to analyze categorical variables. The threshold for statistical significance was set at p < .05.
Results
Patient characteristics
This study enrolled a total of 174 eligible cases (). These 174 patients were randomly assigned to the liquid-isolating method group (LIM group) or the lever-elevating method group (LEM group). The LIM group included 87 patients (35 males and 52 females, aged 22–63 years; mean age, 44.5 ± 10.8 years). The mean number of thyroid nodules was 3.4 ± 0.8. Mean thyroid nodule diameter was 2.52 ± 1.38 cm. The LIM group included 83 cases of nodular goiter and 4 cases of thyroid adenoma. The LEM group included 87 patients (39 males and 48 females, aged 20–65 years; mean age, 42.3 ± 11.6 years). The mean number of thyroid nodules was 3.2 ± 0.5. Mean thyroid nodule diameter was 2.46 ± 1.07 cm. The LEM group included 85 cases of nodular goiter and 2 cases of thyroid adenoma. There was no significant difference in clinical data between groups (all p > .05), as shown in .
Table 1. Patient characteristics.
Treatment outcomes
Mean operation time was longer in the LIM group, compared with the LEM group (44.75 ± 13.14 min vs. 32.87 ± 10.84 min; p = .017). After establishing the liquid isolation zone in the LIM group, liquid retention time ranged from 5 to 14 min, with an average of 5.83 ± 1.74 min.
Six patients (6.9%) of the 87 cases in the LIM group had voice changes, while 2 (2.3%) in the LEM group had voice changes (p = .278). One out of two individuals in the LEM group was recurrence of the thyroid nodule after thyroidectomy. Vocal cord paralysis was confirmed by fiberoptic laryngoscopy. The difference between groups was not significant (p = .278). Patients with voice changes were treated with oral corticosteroids for 3–10 days. The time to recovery of baseline voice characteristics was 9–87 days after the procedure. No patient reported permanent hoarseness. The time to recovery of baseline voice in the LIM group was 36.15 ± 10.24 days, which was significantly longer than the time to recovery of baseline voice in the LEM group 24.48 ± 11.53 days (p = .014). Fiberoptic laryngoscopy was performed 3 mo postoperatively to determine whether vocal cord function had recovered. Patient outcomes are shown in .
Table 2. Operative time and complications in both study groups.
The neck hematoma was absorbed 3–7 days after surgery. Peri-thyroid hematoma was observed in 10 cases (11.5%) in the LIM group and 3 cases (3.4%) in the LEM group. The difference between groups was statistically significant (p = .044). Nine patients (10.3%) in the LIM group and 2 patients (2.3%) in the LEM group had postoperative neck tension. The difference between groups was statistically significant (p = .029).
During the MWA procedure, one patient in the LEM group (1.1%) exhibited a vasovagal response; no patient in the LIM group exhibited a vasovagal response. For the case that involved a vasovagal response, ablation was discontinued. After inhaling oxygen for 6 min, the patient recovered. There was no significant difference between groups in risk for a vasovagal response (p = 1.000).
Discussion
Image-guided ablation techniques (percutaneous ethanol ablation, radiofrequency, laser, microwave ablation, and high-intensity focused ultrasound) have been proposed for the treatment of clinically relevant benign thyroid nodules. These techniques may shrink thyroid nodules and alleviate local symptoms [Citation5,Citation17]. Due to a higher benefit-risk ratio, they are even proposed as first-choice options for patients with symptomatic benign thyroid nodules [Citation4,Citation5]. Although image-guided ablation techniques have many advantages, their performance still entails risks. Comprehension of the reasons for complications and efforts to further lower the rate of complications are extremely important.
Among the complications, recurrent laryngeal nerve injury is the most common [Citation15,Citation16,Citation30]. Xin et al. [Citation25] reported that the incidence of hoarseness after LEM or LIM MWA for thyroid nodules was 1 out of 28 (3.6%). However, the study did not distinguish the usage of LEM or LIM. Our data indicated that the incidence of recurrent laryngeal nerve injury in LIM was higher than that in LEM, but this trend was not significant (6.9% vs. 2.3%, p > .05). Time to recovery of baseline voice was longer in the LIM group than in the LEM group (p < .05), indicating that the extent of recurrent laryngeal nerve injury was greater for the LIM approach, compared with the LEM approach.
The incidences of peri-thyroid hematoma and postoperative neck tension were significantly greater in the LIM group, compared with the LEM group. Operation time was also greater in the LIM group than in the LEM group (p < .05). Notably, the risk for bleeding and neck tension and the operation time may have increased because of the multiple saline injections.
There was no vasovagal reaction in the LIM group. One patient in the LEM group with a target thyroid nodule (diameter 3.2 cm) on the lateral part of the thyroid lobe sustained a vasovagal response. The vasovagal reaction may have been triggered because the thyroid nodule was located adjacent to the common carotid artery and the internal jugular vein [Citation15].
Numerous authors have recommended use of the LIM for thyroid MWA or RFA [Citation26,Citation31,Citation32], but our data suggest that LIM has limited effectiveness in protecting structures adjacent to the thyroid gland. The tissues between various neck structures are relatively loose, so injected saline is easily absorbed and diffused. Compression of the thyroid gland during the puncture and ablation also accelerate this process. Thus the liquid zone could retain only for a short time. In the study, liquid retention time after establishment of the liquid isolation zone was only 5–14 min (average, 5.83 ± 1.74 min). Once the liquid separation zone disappears, the associated protective effect is eliminated. The administration of multiple injections of saline may increase the rate of injury of small vessel and cause bleeding, resulting in neck hematoma,also contribute to neck tension, resulting in discomfort after the procedure. As stated above, multiple injections of saline also prolongs the operation time.
In 2008, Park et al. [Citation24] moved the kidney away from the surrounding structure by a similar leverage technique, using a radiofrequency needle, in order to protect the nerves, intestines, and inferior vena cava from damage caused by excessive thermal energy. Unlike kidney tumors, benign thyroid nodules are soft, without tough capsules. So lift the nodules immediately with the microwave needle is difficult. In our study, we activated the microwave device prior to preforming the Lever-elevating maneuver for dehydrating and solidifying the adjacent tissue, so the microwave antenna can lift the nodule more easily. In the LEM group, 2 patients had voice changes, one of which involved recurrence of a thyroid nodule after thyroidectomy. The results showed that LEM had a limited effect in cases with history of neck surgery due to the adhesion.
In summary, the LEM is superior to the LIM in protecting vital cervical tissues during thyroid MWA. It could be considered as a technique that may decrease the risk of complications for the ablation treatment of benign thyroid nodules.
Supplemental Material
Download TIFF Image (695.2 KB)Disclosure statement
The authors declare that they have no conflict of interest.
Data availability statement
The datasets generated and analyzed during the present study are available from the corresponding author on reasonable request.
References
- Durante C, Costante G, Lucisano G, et al. The natural history of benign thyroid nodules. Jama. 2015;313(9):926–935.
- Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical guidelines for clinical practice for the diagnosis and management of thyroid nodules–2016 update. Endocr Pract. 2016;22(Supplement 1):1–39.
- Papini E, Gugliemi R, Pacella CM. Laser, radiofrequency, and ethanol ablation for the management of thyroid nodules. Curr Opin Endocrinol Diabetes Obes. 2016;23(5):400–406.
- Papini E, Pacella CM, Solbiati LA, et al. Minimally-invasive treatments for benign thyroid nodules: a Delphi-based consensus statement from the Italian minimally-invasive treatments of the thyroid (MITT) group. Int J Hyperthermia. 2019;36(1):376–382.
- Mainini AP, Monaco C, Pescatori LC, et al. Image-guided thermal ablation of benign thyroid nodules. J Ultrasound. 2017;20(1):11–22.
- Boutzios G, Tsourouflis G, Garoufalia Z, et al. Long-term sequelae of the less than total thyroidectomy procedures for benign thyroid nodular disease. Endocrine. 2019;63(2):247–251.
- Nicosia L, Ferrari F, Mauri G, et al. Image guided ablations for thyroid tumours. JTC. 2019;1(2):16–20.
- Cervelli R, Mazzeo S, De Napoli L, et al. Radiofrequency ablation in the treatment of benign thyroid nodules: an efficient and safe alternative to surgery. J Vasc Interv Radiol. 2017;28(10):1400–1408.
- Deandrea M, Trimboli P, Garino F, et al. Long term efficacy of a single session RFA of benign thyroid nodules: a longitudinal 5-Year observational study. J Clin Endocrinol Metab. 2019;104(9):3751–3756.
- Kim JH, Baek JH, Lim HK, et al. 2017 Thyroid radiofrequency ablation guideline: Korean society of thyroid radiology. Korean J Radiol. 2018;19(4):632–655.
- Dietrich CF, Muller T, Bojunga J, et al. Statement and recommendations on interventional ultrasound as a thyroid diagnostic and treatment procedure. Ultrasound Med Biol. 2018;44(1):14–36.
- Pacella CM, Mauri G, Achille G, et al. Outcomes and risk factors for complications of laser ablation for thyroid nodules: a multicenter study on 1531 patients. J Clin Endocrinol Metab. 2015;100(10):3903–3910.
- Durante C, Grani G, Lamartina L, et al. The diagnosis and management of thyroid nodules: a review. Jama. 2018;319(9):914–924.
- Nicholson KJ, Teng CY, McCoy KL, et al. Completion thyroidectomy: a risky undertaking? Am J Surg. 2019;218(4):695–699.
- Baek JH, Lee JH, Sung JY, et al. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012;262(1):335–342.
- Dobnig H, Amrein K. Monopolar radiofrequency ablation of thyroid nodules: a prospective Austrian Single-Center study. Thyroid. 2018;28(4):472–480.
- Cesareo R, Palermo A, Pasqualini V, et al. Radiofrequency ablation for the management of thyroid nodules: a critical appraisal of the literature. Clin Endocrinol. 2017;87(6):639–648.
- Randolph GW, Shin JJ, Grillo HC, et al. The surgical management of goiter: part ii. surgical treatment and results. Laryngoscope. 2011;121(1):68–76.
- Chahardahmasumi E, Salehidoost R, Amini M, et al. Assessment of the early and late complication after thyroidectomy. Adv Biomed Res. 2019;8:14.
- Kohlhase KD, Korkusuz Y, Groner D, et al. Bipolar radiofrequency ablation of benign thyroid nodules using a multiple overlapping shot technique in a 3-month follow-up. Int J Hyperthermia. 2016;32(5):511–516.
- Wang JF, Wu T, Hu KP, et al. Complications following radiofrequency ablation of benign thyroid nodules: a systematic review. Chin Med J (Engl). 2017;130(11):1361–1370.
- Xiaoyin T, Ping L, Dan C, et al. Risk assessment and hydrodissection technique for radiofrequency ablation of thyroid benign nodules. J Cancer. 2018;9(17):3058–3066.
- Liu YJ, Qian LX, Liu D, et al. Ultrasound-guided microwave ablation in the treatment of benign thyroid nodules in 435 patients. Exp Biol Med (Maywood). 2017;242(15):1515–1523.
- Park BK, Kim CK. Using an electrode as a lever to increase the distance between renal cell carcinoma and bowel during CT-guided radiofrequency ablation. Eur Radiol. 2008;18(4):743–746.
- Zhi X, Zhao N, Liu Y, et al. Microwave ablation compared to thyroidectomy to treat benign thyroid nodules. Int J Hyperthermia. 2018;34(5):644–652.
- Korkusuz Y, Mader OM, Kromen W, et al. Cooled microwave ablation of thyroid nodules: Initial experience. Eur J Radiol. 2016;85(11):2127–2132.
- Ha EJ, Baek JH, Lee JH, et al. Clinical significance of vagus nerve variation in radiofrequency ablation of thyroid nodules. Eur Radiol. 2011;21(10):2151–2157.
- Jung SL, Baek JH, Lee JH, et al. Efficacy and safety of radiofrequency ablation for benign thyroid nodules: a prospective multicenter study. Korean J Radiol. 2018;19(1):167–174.
- Rosen CA, Lee AS, Osborne J, et al. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114(9):1549–1556.
- Wang LF, Lee KW, Kuo WR, et al. The efficacy of intraoperative corticosteroids in recurrent laryngeal nerve palsy after thyroid surgery. World J Surg. 2006;30(3):299–303.
- Guang Y, He W, Luo Y, et al. Patient satisfaction of radiofrequency ablation for symptomatic benign solid thyroid nodules: our experience for 2-year follow up. BMC Cancer. 2019;19(1):147.
- Deandrea M, Sung JY, Limone P, et al. Efficacy and safety of radiofrequency ablation versus observation for nonfunctioning benign thyroid nodules: a randomized controlled international collaborative trial. Thyroid. 2015;25(8):890–896.