Abstract
Objective
This study was aimed at investigating the clinical efficacy and studying the possible mechanism of FUS applications to treat cervical intraepithelial neoplasia 1 (CIN1).
Methods
This was a prospective clinical study, in which 30 patients with CIN1 (28/30 of the patients were HPV positive) were enrolled and treated with FUS therapy by gynecologist. All patients were followed up for 3 months after FUS therapy. Telephone interviews, PAP smear, colposcopic examinations, cervical biopsies and HPVDNA tests were performed to assess the safety and effectiveness of FUS therapy for HPV-positive CIN1. The expression of p16, Ki-67 and Fas in the cervical tissues were examined in order to account for the possible mechanism of FUS therapy for CIN1 with HPV infection.
Results
FUS therapy was tolerated well, and no severe complications were observed in any patient. After FUS treatment, twenty-five patients were cured completely, and two cases were improved with the cervical smear results reversed to normal, and three cases remained the same status as before treatment. The total effectiveness rate was 90.00% (27/30). The expression of P16 and Ki-67 in the treated cervical tissues was significantly lower than that before treatment, and the expression of Fas was found up-regulated (all p < .05).
Conclusion
FUS therapy appears to be a feasible and effective treatment for patients with HPV positive CIN1. FUS therapy may help to reduce the expression of p16 and Ki-67 and enhance the expression of Fas in the treated cervical tissues to regulate cell proliferation and increase apoptosis, and thus prevent the disease from evolving into high grade lesions.
As the National Comprehensive Cancer Network (NCCN) reported in 2016 [Citation1], the incidence of cervical cancer in developing counties accounts for 85% of the cases in the world, and it was also one of the major causes of death. Cervical intraepithelial neoplasia (CIN) is cervical precancerous lesions closely related to invasive cervical cancer, and it typically takes about 10–20 years to develop into cervical cancer. However, the incidence of CIN is on the rise in recent years, and the age of patients is becoming younger and younger [Citation2], threatening the physical and mental health of women [Citation3]. Patients with these reports may experience significant psychological distress, while clinicians are required to repeat tests, which involve high healthcare costs. CIN1 is a disease that in most cases progresses to cervical cancer, so it is important to actively treat and control CIN1.
Persistent HPV infection denotes the presence of the same type-specific HPV DNA on repeated sampling after 6–12 months [Citation4]. Only one-tenth of all infections become persistent, and these women could develop cervical precancerous lesions. A prospective study of Hu [Citation5] showed that HR-HPV infection was closely related to the progression of CIN1, and that the cases with positive HR-HPV infection have a higher risk of progressing into the high grade lesion than the cases with negative HR-HPV infection. The risk of progression was highest for the HR-HPV infection in follow-ups, and with long follow-up the progression risk increases gradually.
In recent years [Citation6,Citation7], more and more research studies have been focused on the cellular level of cervical lesion. p16 encoded by the CDKN2A gene is a protein acting as tumor suppressor which is directly involved in the regulation of cell cycle and the proliferation and division of cells [Citation8]. Ki-67, as well as of cell proliferation control, such as p16, may be a potential tool for identifying women at the risk of developing high-grade precursors and cervical cancer [Citation3]. It is also worth noticing that women with persistent simultaneous expression of p16 and Ki-67 in any of their cervical cells during follow-up had a 23% risk of developing high-grade lesions. Therefore, p16/Ki-67 dual staining should be used for screening CIN1 with HPV infection.
At present, the treatment modalities for CIN include expectant management and surgical treatment [Citation9]. It is expected that the expectant management is suitable for the patients with CIN1 [Citation10]. From the view of a colposcopy clinic, women transferred because of borderline or LSIL cytology should undergo colposcopic assessment with biopsies. Both RCTs support the broad consensus that, in women with biopsy-proven CIN1 and satisfactory colposcopy, invasive treatment is not indicated. These women should be followed with intensified screening. However, in women referred to colposcopy because of HSIL cytology, who receive a histologic diagnosis of CIN1 in corresponding targeted biopsies, most guidelines recommend a diagnostic excision of the transformation zone because the risk of underlying high-grade disease is high. When should cervical intraepithelial neoplasia 1 be treated? How long it will take before CIN1 can undergo invasive treatment? Of course, a few of progressing lesions require intervention treatment and a large number of lesions will regress spontaneously, but what should be done with persistent CIN1? Is it cost-efficient to follow these women with intensified screening for many years? What subgroups can benefit from invasive treatment and can we apply destructive methods in these women to avoid unnecessary morbidity? These hot topics in this field need further research.
FUS is a new and noninvasive tool for the treatment of vulvar diseases and multiple solid tumors and etc [Citation11–13]. FUS generates heat effects, mechanical effects and cavitation effects that denature the diseased tissues, facilitate necrosis and allow them to be replaced by surrounding normal healthy tissues. In 2009 [Citation14], we have reported for the first time that focused ultrasound therapy could be safe, effective and feasible in the treatment of patients with HPV-infected cervicitis [Citation15]. Lin indicated that FUS for the treatment of CIN1 was effective, and the duration of postoperative vaginal discharge and cervical wound healing was shorter compared with other treatments. In this study, we hypothesized that focused ultrasound therapy could treat CIN1 with HPV infection that was uncontrollable by conventional therapy. Thus, the goal of this study was to investigate the safety, effectiveness and feasibility of focused ultrasound therapy as a noninvasive tool for the management of CIN1 with HPV infection, and the changes of the expressions of p16 and Ki-67 in the cervical tissues after FUS as a possible mechanism of focused ultrasound treatment for CIN1.
Materials and methods
General information
The study was approved by the Ethics Committee of Chongqing Medical University. Written informed consent was obtained from all patients.
From December 2013 to December 2014, 30 women with abnormal thin-layer fluid-based cytological findings subsequently undergoing colposcopy examination and cervical biopsy with a result of confirmed CIN1 in this study were diagnosed and treated at Chongqing Haifu Hospital, Chongqing People’s Hospital of Jiangbei District and Chongqing Health Center for Women and Children of Yubei District. The medium age of these patients was 38 ± 9.9 years old, ranging from 21 to 58. Among these patients, 5 cases were primiparous, 10 cases had children and still had fertility desire, and 15 cases had children and did not have fertility desire in the future. In this study conventional antibiotic therapy had failed before to control the symptoms related with CIN1 with HPV infection, such as abundant leukorrhea, pelvic pain and postcoital bleeding. Twenty eight out of the thirty patients had positive HPV results, among which 19 cases were high-risk HPV infection, 5 cases were low-risk HPV infection, and 4 cases were mixed HPV infection. There was no statistically significant difference in age, fertility, fertility desire and the age of first sexual intercourse. The characteristics of enrolled patients are shown in .
Table 1. Characteristics of the enrolled patients with CIN.
Methods
The focused ultrasound equipment (Model-CZF Focused Ultrasound Therapeutic Device for Gynecology) used for treatment was manufactured by Chongqing Haifu Medical Technology Co, Ltd (Chongqing, China), with therapeutic power of 3.5–4.5 W, working frequency of 10.0 MHz and impulse of 1000 Hz. The equipment was operated by doctors who were trained and granted with the qualification certificate for performing the procedure. Patients undergoing treatment were positioned in a lithotomy position, with their cervix disinfected and exposed by a speculum. The surface of cervix was coated with ultrasound coupling gel prior to treatment. The treatment probe was placed in close contact with the cervix over the transition zone (TZ) and CIN lesion and moved continuously against the skin over the diseased area with 2 mm more of healthy tissue around at a speed of 5–10 mm/sec. The treatment lasted until the treatment area turned white and the lesion presented a depressed area. The treatment time was 120–180 s.
Follow up
Patients were advised to avoid sexual intercourse, bath and swimming for 2 months after treatment, and they were followed up every week for 1 month to observe any heavy bleeding or abnormal vaginal discharge. Three months after treatment, patients underwent cytological test, colposcopy and cervical biopsy for pathological examination, immunohistochemical staining, and HPV testing.
Immunohistochemical tests
The biopsy specimens were fixed with 4% paraformaldehyde. After dehydration, clearing, wax impregnation and embedding treatment, the paraffin-embedded tissue blocks were sectioned, and Streptavidin-Peroxidase (SP) method was used for immunohistochemical test. p16 antibody (rabbit-anti-human, number: bs-0740R), Ki-67 antibody (rabbit-anti-human, number: bs-2130R) and Fas polyclonal antibody (rabbit-anti-human, number: bs-6477R) were used. SP kits were purchased from Beijing Boosen Biological Co, Ltd. The steps of immunohistochemical staining followed strictly the operation instructions of the SP kit and the antigen staining instructions.
Determination of results
The positive expressions of p16, Ki-67 and Fas were represented by the percentage of positively stained cells. Immuno-positive cells of p16 were characterized by brownish-yellow granules in cell nuclei and/or cytoplasm, immuno-positive cells of Ki-67 were characterized by brownish-yellow granules in cell nuclei, and the positive expression of Fas was characterized by the staining in cytoplasm and/or cell membrane. In 5 high power microscopic fields, the number of immunohistochemically positive-stained cells was randomly chosen from the positive or negative. The average number of cells per high-power field (HPF) represented the positive expression of p16, Ki-67 and Fas. And then the percentage of positive cells in the tissue of 5 HPF was counted.
Statistical analysis
SPSS 21.0 statistical analysis software was used for descriptive analysis. Normally distributed data were depicted as mean ± standard deviation. The Chi-Square (χ2) test was used for statistical comparisons of the expression of p16, Ki-67 and Fas. A p values below .05 was considered to indicate a significant difference.
Results
FUS therapy was tolerated well, and no severe complications were observed in any patient. Two weeks after FUS treatment, patients experienced moderate vaginal discharge and some spotting until next menstruation. The cervical wound appeared dry upon examination at 4 weeks after treatment. The surface of cervical wound recovered to normal without scar at 3 months after treatment (). After FUS treatment, 25 patients were cured with biopsies indicating that the CIN lesions had disappeared. The cure rate was 83.33% (25/30). 2 cases were improved with the cervical smear results reversed to normal, and the other 3 cases remained the same status as before. The total effectiveness rate was 90.00% (27/30). Post-operative HPV testing revealed that 85.71% (24/28) of patients presented negative HPV infection after treatment. Among the 28 patients with positive HPV results, 24 had conversion to negative after treatment, 1 had a change of virus type, and 3 showed persistently positive HPV smear results. And cytological test and biopsies of the 3 patients revealed that the CIN lesions had remained the same status as before ().
Figure 1. (a) The cervical appearance of a patient under colposcopy before focused ultrasound treatment. Acetic acid staining showed white plaque on the outside of the cervix (CIN1 for cervical biopsy. (b) The cervical appearance of the same patient under colposcopy at 3 months after treatment. The cervix is completely back to normal. (c) the expressions of P16 in cervical tissue were strongly positive and darkly staining (immunostaining, 400 × magnification) before treatment; 1d. 3 months after treatment, the expressions of P16 were weakly positive with light staining, and the number of cells of positive expressions had reduced; 1e. the expressions of Ki-67 in cervical tissue were strongly positive and darkly staining (immunostaining, 400x magnification) before treatment; 1f. 3 months after treatment, the expressions of Ki-67 were weakly positive with light staining, and the number of cells of positive expressions had reduced; 1g. the expressions of Fas at lower 1/3 of the cervical epithelium were weakly positive with light staining, and the number of cells of positive expressions was less (immunostaining, 400x magnification) before treatment; 1h. 3 months after treatment, the expressions of Fas were strongly positive and with darker staining, and the number of cells with positive expression had increased compared to before treatment.
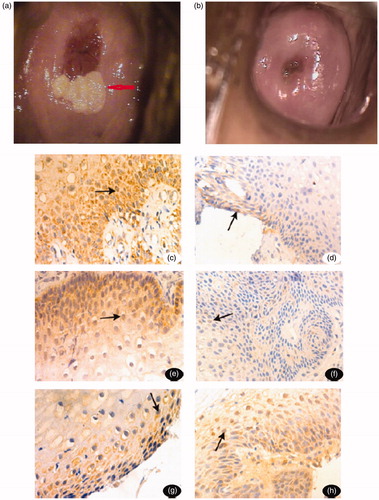
Table 2. Changes in symptoms, cytology and biopsy before and after FUS therapy.
Before FUS treatment, 24 cases showed moderate to strong positive expressions of p16, and 10 cases showed moderate to strong positive expression of Ki-67. Three months after FUS treatment, 26 and 30 cases become weakly positive and negative of p16 and Ki-67 respectively (). Before treatment, 20 cases showed weakly positive expression of Fas; however, three months after treatment, 10 cases showed moderate to strong positive expression (). These were statistically significant differences in the expressions of p16, Ki-67 and Fas before and after focused ultrasound treatment [(p16:80.00%(24/30), 13.33%, χ2 = 31.543. p < .001; Ki-67:33.33%(10/30), 0, χ2 = 22.051. p < .001; Fas:0, 33.33%(10/30), χ2 = 20.000, p < .001)] ().
Table 3. The expression of P16, Ki-67 and Fas before and after treatment (n = 30).
Discussion
Management approaches for clinically relevant HPV infection of the cervix include local therapies targeting the HPV lesions and systemic therapies such as immunotherapy and antiviral treatment for HPV infection. Surgical removal and minimally invasive ablative techniques, such as laser, cryoablation and electrocautery are the standard therapeutic strategies that are focused on the management of the symptoms related with cervical infection and CIN1. They are performed individually in clinical practice based on the extent of disease and the needs of the patient. FUS is a novel noninvasive therapy for targeted tissues, and our preliminary results showed that it was safe and effective in the treatment of patients with HPV-infected cervicitis [Citation14]. Compared with laser ablation, FUS therapy had the equivalent therapeutic efficacy in patients with symptomatic cervicitis, but post-operative bleeding and reactive discharge were much less in the patients who underwent focused ultrasound therapy [Citation16]. Due to its noninvasiveness, without loss of normal tissue during the therapeutic procedure, the diseased cervix is anatomically well-preserved with normal elasticity and the physiological function of the cervix not compromised after ultrasound therapy. However, as the diseased tissues are completely destroyed by ultrasound energy, it is very important to screen the patients thoroughly through colposcopy, PAP smear and biopsy before ultrasound therapy in order to make sure that the cervical lesion to be treated is low-grade squamous intraepithelial lesion (LSIL) or CIN1 with HPV infection. In this study conventional antibiotic therapy had failed before to control the symptoms related with CIN1 with HPV infection, such as abundant leukorrhea, pelvic pain and postcoital bleeding. It was found that after FUS therapy the symptoms were relieved significantly. Colposcopic examination showed no evidence of CIN in (27/30) patients, postoperative cytological tests and biopsies during follow-up showed that the CIN lesions had disappeared in 83.33% (25/30) of patients after FUS therapy, and that the CIN lesion of 3 cases remained the same status as before. The total effectiveness rate was 90.00% (27/30). The significant improvement of symptoms after treatment in this study indicates that FUS therapy cures the HPV-infected cervical lesions. However, for the sake of safety, only patients with low-grade squamous intraepithelial lesion (LSIL) or CIN1 with HPV infection were enrolled in this study. Our further research is aimed at investigating the FUS therapy for cervical high-grade squamous intraepithelial lesion (HSIL) which prevails in the cases of HPV infection.
It was also found that cervical HPV infection reversed to negative in 3 months after FUS therapy in 85.71% (24/28) of patients who had HPV-positive CIN1 previously. This result suggests that FUS therapy could locally clear HPV infection by removing all HPV-infected cervical cells. However, the infection persisted in the remaining 14.28% (4/28) of patients among whom 1 patient experienced transformation of virus type, and 3 patients with persistently positive HPV smear results had CIN lesion remained as before treatment according to their postoperative cytological test and biopsy results. This may have been due to multifocal infection and HR-HPV infection. The follow-up lasted only for 3 months, relatively short for patients with HPV-infected CIN1.
FUS therapy, as a new promising therapeutic technology, offers patients and doctors more options. It is shown that FUS can reduce the expression p16 and Ki-67 in the diseased cervical tissues, regulate cell proliferation and up-regulate the expression of Fas for controlling cell apoptosis, and thus keep the balance of cell proliferation and apoptosis and facilitate the recovery of patients. This could be one of the therapeutic mechanisms of FUS therapy for the conversion of CIN1 and HPV.
As Cao reported [Citation17], 2%–21% of CIN1 could develop into CIN3 or invasive cervical cancer without any treatment of HPV infection, especially the high-risk HPV (HR-HPV) infection [Citation18]. It is because HPV was found to be the causative agent for cervical cancer and cervical precancerous lesions. Many papers [Citation19–21] proved that cervical cancers with positive HPV result showed over-expression of p16 protein. In our study, 28 patients with positive HPV result were treated with FUS therapy, among whom 24 cases reversed to negative results with a cure rate of 85.71% (24/28). Therefore, FUS therapy is an effective cure for HPV infection of cervix. The decrease in p16 expression after FUS treatment indicates that the normal regulation mechanism of p16 was not destroyed with the elimination of HPV, which could ensure the normal proliferation cycle of cells.
Ki-67, also known as a cell proliferation index, is a nuclear antigen expressed in proliferating cells. It is synthesized in the G1, S, G2 and M phases of cell proliferation cycle. It was not expressed in G0 phase and its half-life is short, which could accurately reflect the activity of cell proliferation. Bean confirmed [Citation22] that the positive rate of Ki-67 expression increased gradually in cervical inflammatory disease, CIN and cervical cancer; therefore, it could be used as a potential biomarker for cervical biopsy to identify the precancerous epithelial lesions. Researchers reported [Citation23–25] that there was a positive correlation and high consistency between the expression of p16 and Ki-67 in cervical tissues. Their expressions are similar in benign cervical lesions, CIN, cancer and glandular epithelial lesions; however, the expressions of p16 and Ki-67 are significantly enhanced with the increase of the grade of CIN. By combined testing, the sensitivity and specificity of the diagnosis of CIN lesions are both improved. The results of our study showed the expression of p16 and Ki-67 both decreased in cervical tissues of LSIL patients in 3 months after focused ultrasound treatment, which is consistent with the results of previous reported studies [Citation23,Citation24].
Fas is a type I transmembrane glycoprotein encoded by Fas gene. Fas and Fas Ligand (FasL) are members of the tumor necrosis factor (TNF)-receptor and TNF family, respectively. Fas is cell-surface protein receptor, widely expressed in a variety of cells. There is higher expression of Fas on the activation of T lymphocytes [Citation25]. The interaction of Fas and FasL contributes to the induction of cell apoptosis. Fas binding to FasL sends apoptotic signals and induces apoptosis of target cells. Therefore, Fas expression signifies a dynamic balance of cell proliferation and apoptosis. Normal apoptosis is important for the stability of cells and organs as well as the internal environment of the body. This study showed low Fas expression in cervical lesion with CIN1 before treatment. However, after FUS therapy, the expression of Fas increased. This implies that FUS therapy can enhance the expression of Fas to prevent further progression of cells into HSIL or even to cervical cancer.
In recent years, FUS therapy becomes a new promising therapeutic technology widely applied in clinical treatment of HPV infection and some other gynecological diseases with good curative efficacy and minimal complications [Citation16,Citation26–28]. FUS therapy has unique advantages compared with other treatments. Firstly, it destroys the HPV lesions in the basal layers of cervical epithelium with the penetrating focused ultrasound energy. Secondly, all inflammatory cells and diseased tissues are sensitive to ultrasound energy, while the normal cervical tissues are free from the influence of FUS therapy. FUS therapy can preserve the integrity of cervical tissue structure, and there is no scab or necrosis after treatment. Furthermore, FUS therapy is simple to operate and can be repeated. And patients do not need to receive anesthesia. It is also an pollution-free operation without generating smell or smoke, burning of tissue, or radiation. The shortcomings of this study lie in the following. The follow-up period in this study is 3 months, which is relatively short for patient with HPV-infected CIN1 in view of the potential risk of local recurrence. We are recently undertaking a Phase III clinical trial in which the enrolled patients will be followed up for 2 years after FUS therapy to investigate the long-term effects of FUS therapy on HPV-infected CIN1 and the local recurrence of the HPV-infected lesions. Our next step is to perform multiple randomized clinical trials to compare FUS therapy with other local therapeutic approaches such as laser for the treatment of HR-HPV- positive CIN2–3 in terms of its long-term efficacy. The second shortcoming is the lack of numerical rating of the treatment responses. In this study, the treatment responses were assessed based on changes in patients’ symptoms and histological examination before and after FUS therapy. Quantitative assessment will be applied in our ongoing randomized clinical trial to evaluate the local responses after treatment.
In summary, FUS therapy appears to be safe, effective and feasible in the treatment of patients with HPV-infected CIN1. It can provide a noninvasive approach for treating CIN1 with HPV infection. FUS therapy may reduce the expression of p16 and Ki-67 and enhance the expression of Fas in the treated cervical tissues to regulate cell proliferation and increase apoptosis, and thus prevent it from progressing into high grade lesions.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: cervical cancer (V1. 2016) [EB/OL]. [cited 2015 Nov 25]. Available from: https://www.nccn.org/professionals/physician.gls/pdf/cervical.pdf.
- Henk HJ, In Sing a. R, Singhal PK, et al. Incidence and costs of cervical intraepithelial neoplasiain a US commercially insured Population. J Low Genit Tract Dis. 2010; 14(1):29–36.
- Velasco J, Álvarez-Ruiz E, González-Fernández L, et al. Expression of p16/Ki-67 in ASC-US/LSIL or Normal Cytology with Presence of Oncogenic HPV DNA. Anticancer Res . 2015;35:6291–6296.
- Neerja B, Daisuke A, Daya NS, et al. Cancer of the cervix uteri [J]. Int. J Gynecol Obstet. 2018;143(supp12):22–26.
- Hu SY, Zhao FH, Ma JF, etc. A prospective cohort study of prognosis of mild cervical intraepithelial neoplasia and its association with human papilloma virus. Chin J Prev Med. 2014;48(5):361–365.
- Gao BL, Qian P, Ma ZY, etc. Expression and significance of human papilloma virus L1 protein and p16. Ki 67 in Cervical Squamous Epithelial Lesions. Mat Child Health Care China. 2015;30(7):1109–1111.
- Sari Aslani F, Safaei A, Pourjabali M, et al. Evaluation of Ki – 67, p16 and CK17 markers in differentiating cervical intraepithelial neoplasia and benign lesions. Iran J Med Sci. 2013;38(1):15–21.
- Malinowski DP. Molecular diagnostic assays for cervical neoplasia: emerging markers for the detection of high-grade cervical disease. Biotechniques. 2005;38(4S):S17–S23.
- Wang RM, Peng JJ, You ZX. Interpretation of ASCCP 2012 guidelines for cervical cancer screening and management of precancerous lesions (two) [J]. Int J Obstet Gynecol. 2015;42(2):238–240.
- Petry KU. Management options for cervical intraepithelial neoplasia.[J]. Best Pract Res Clin Obstet Gynaecol. 2011;25(5):641–651.
- Zhang L, Zhang W, Orsi F, et al. Ultrasound – guided high intensity focused Ultrasound for the treatment of gynecological diseases: a review of safety and efficacy[J]. Int J Hyperthermia. 2015;31(3):280–284.
- Poissonnier L, Chapelon JY, Rouviere O, et al. Control of prostate cancer by transrectal HIFU in 227 patients. Eur Urol. 2007;51(2):381–387.
- Ye M, Deng X, Mao S, et al. High intensity focused ultrasound treatment for non-neoplastic epithelial disorders of the vulva: factors affecting effectiveness and recurrence. Int J Hyperthermia. 2015;31(7):771–776.
- Li C-Z, Wang Z-B, Yang X, et al. Feasibility of focused ultrasound therapy for recurrent cervicitis with high-risk human papillomavirus infectionet. Ultrasound Obstet Gynecol. 2009;34(5):590–594.
- Lin C, Yang J, Li CZ, etc. Treatment of low grade cervical intraepithelial neoplasia with focused ultrasound. Chin Int Imag Thera. 2012;12(9):873–876.
- Chen J, Zhou D, Liu Y, et al. A comparison between ultrasound therapy and laser therapy for symptomatic cervical ectopy. Ultrasound Med Biol. 2008;34(11):1770–1774.
- Cao ZY. Obstetrics and Gynecology. Beijing: People’s Medical Publishing House; 2010. 567.
- Ren YF, Wu FY, Cai HF, etc. the comparison of curative effect for Focused ultrasound and laser power with electric coagulation for treating CIN I patients with high-risk human papilloma virus infection. J Third Military Med University. 2012;34(4):350–353.
- Lesnikova I, Lidang M, Hamilton-Dutoit S, et al. P16 as a diagnostic marker of cervical neoplasia: a tissue micmarray study of 796 archival specimens. Diagn Pathol. 2009;4(1):22.
- Cortecchia S, Galanti G, Sgadari C, et al. Follow -up study of patients with cervical intraepithelial neoplasia grade 1 overexpressing p16 Ink 4a. Int J Gynecol Cancer. 2013;23(9):1663–1669.
- Reuschenbach M, Seiz M, von Knebel Doeberitz C, et al. Evaluation of cervical cone biopsies for coexpression of p16 INK 4a and Ki – 67 in epithelial cells. Int J Cancer. 2012;130(2):388–394.
- Bean SM, Eltoum I, Horton DK, et al. Immunohistochemical expression of p16 and Ki – 67 Correlates with degree of anal intraepithelial neoplasia. Am J Aurg Pathol. 2007;31(4):555–561.
- Lu JY, Qin WP. The clinical significance of p16 and Ki – 67 in cervical lesions. Chin General Practitioner J. 2011;189(3):81–88.
- Calil LN, Edelweiss MI, Meurer L, et al. p16 INK 4a and Ki – 67 expression in normal dysplastic and neoplastic uterine cervical epithelium and human papilloma virus (HPV) infection. PatholRes Pract. 2014;210(8):482–487.
- Wu SF, Zhang JW, Qiu M, etc. Expression and relationship of survivin fas and fasl in cervical carcinoma. J Shanghai Jiao Tong University (Medical Edition). 2010;30(9):1138–1142.
- Li C, Xiong X, Li Y, et al. Therapeutic effects of focused ultrasound in 4014 patients with symptomatic cervical ectopy. Ultrasound Med Biol. 2013;39(4):604–610.
- Duan J, Li HY, Xiong J, et al. Comparative analysis of clinical efficacy of microwave and focused ultrasound in the treatment of CIN I. Public Health Prevent Med. 2010;21(6):124–125.
- Zhang B, Xu DM, Su XR. Efficacy of leep and focused Ultrasound in the treatment of CIN I with High risk HPV infection.China Med Eng. 2014;22(5):134–135.
