Abstract
Objective
To compare the safety and efficacy of ultrasound-guided thermal ablation and conventional thyroidectomy for benign thyroid nodules (TNs) by performing a systematic review and meta-analysis.
Methods
We searched PubMed, Embase, Web of Science and Cochrane Library databases for clinical trials from the date of their inception to 1 April 2019. Two investigators independently examined the trials to select qualified studies, extracted relevant information and assessed the risk of bias according to the Cochrane Collaboration checklist (Oxford, UK). The primary study outcomes were safety (hoarseness, hypothyroidism and postoperative pain) and efficacy (symptom improvement, postoperative cosmetic effects and hospitalization time). This study is registered with PROSPERO (CRD42019125643).
Results
Seven studies involving 1289 patients were included. The results demonstrated that the incidences of hoarseness [odds ratio (OR) 0.33, 95% confidence interval (95% CI) (0.14, 0.79)], hypothyroidism [risk difference (RD) −0.31, 95% CI (−0.34, −0.28)] and postoperative pain [OR 0.35, 95% CI (0.25, 0.49)] were lower, and the hospitalization time was shorter [standard mean difference (SMD) −4.01, 95% CI (−4.22, −3.81)], in the thermal ablation group than in the conventional thyroidectomy group, and postoperative cosmetic effects were better [relative risk (RR) ratio 1.12, 95% CI (1.01, 1.24)] (p < 0.05). For symptom improvement, the difference was not statistically significant.
Conclusions
This study shows that for benign TNs, ultrasound-guided thermal ablation may have potential advantages in terms of safety, cosmetic effects and shorter hospitalization time compared with conventional thyroidectomy, while symptom improvement is the same.
Introduction
Thyroid nodules (TNs) are commonly detected, with a prevalence of up to 76% in the general population [Citation1]. According to current research, most TNs are benign [Citation2]. In most cases, TNs are completely asymptomatic and do not need treatment; they are occasionally found by ultrasound during a health check. For benign TNs that become symptomatic, conventional thyroidectomy is the standard therapy [Citation3], but it may lead to complications, such as damage to the recurrent laryngeal nerve and parathyroid gland, or cosmetic concerns, such as permanent scar formation. Some patients who undergo total thyroidectomy may develop hypothyroidism and require lifelong levothyroxine treatment, which can cause economic losses and can potentially lead to adverse effects [Citation4,Citation5]. In addition, thyroidectomy may not be an option for patients with high surgical risks. Levothyroxine and radioiodine have been used as alternative noninvasive treatments for older and high surgical risk patients; however, these treatments cannot avoid iatrogenic hypothyroidism or hyperthyroidism [Citation6,Citation7].
Ultrasound-guided thermal ablation (laser, radiofrequency, microwave and high-intensity focused ultrasound ablation) is an excellent alternative treatment for benign TNs [Citation8–11]. Previous systematic reviews and meta-analyses of thermal ablation have proven its role in improving the outcomes and prognosis of patients with benign TNs [Citation12,Citation13]. However, whether thermal ablation can be equivalent or even superior to conventional thyroidectomy for benign TNs is still unknown. This is a very important issue for patients with benign TNs as it may determine whether a more suitable treatment method is available.
The purpose of this study was to perform a systematic review and meta-analysis to compare the safety and efficacy of ultrasound-guided thermal ablation and conventional thyroidectomy for benign TNs.
Methods
Search strategy
We searched the PubMed, Embase, Web of Science and Cochrane Library databases for clinical trials from the date of their inception to 1 April 2019. We used the search terms ‘benign’ AND ‘thyroid nodules’ OR ‘thyroid neoplasm’ OR ‘thyroid tumor’ AND ‘surgery’ OR ‘operation’ OR ‘surgical’ OR ‘resection’ OR ‘thyroidectomy’ AND ‘ablation’ OR ‘ablative’. This study is registered with PROSPERO (CRD42019125643).
Selection criteria
Inclusion criteria: (1) retrospective or prospective studies on both ultrasound-guided thermal ablation and conventional thyroidectomy for benign TNs; (2) sample size ≥30 patients who had thermal ablation or conventional thyroidectomy for compressive symptoms or cosmetic problems or anxiety about a malignancy; (3) results that included preestablished outcome indicators; and (4) diagnosis of benign TNs confirmed by surgical pathology or cytopathology.
Exclusion criteria: (1) repeated studies; (2) insufficient sample size; (3) research indicators inconsistent with the preestablished indicators; (4) case reports, meeting summaries, comments, letters or reviews.
Study selection
Two investigators independently examined titles and abstracts to select qualified studies. They focused on potentially relevant studies and read the full texts to determine which ones met the inclusion criteria.
Data extraction and data quality assessment
Two investigators independently extracted relevant information from the included trials, including the author, nation, study type, publication year, patient characteristics and observed indices, including safety and efficacy. Safety was assessed in terms of hoarseness, hypothyroidism and postoperative pain, and efficacy was assessed in terms of symptom improvement, postoperative cosmetic effects and hospitalization time.
To assess hoarseness, patients with voice changes identified by multidimensional voice program (MDVP) testing underwent laryngoscopy to verify vocal cord palsy. Postoperative pain was estimated according to the visual analog scale (VAS), and an increased postoperative score indicated that the pain was positive. For symptom improvement, patients were asked to score the improvement in nodule-related symptoms after treatment (0 = same; 1 = slight improvement; 2 = moderate improvement; 3 = significant improvement), and a score greater than 0 represented a positive result. Postoperative cosmetic effects were graded as poor, acceptable, good and excellent. When the results were excellent, the patient considered that the cosmetic effects of the treatment outweighed the presence of scars.
Two investigators independently assessed the quality of the randomized controlled trials (RCTs) according to the Cochrane Collaboration checklist (Oxford, UK) [Citation14] and assessed the quality of the nonrandomized studies using the Newcastle Ottawa scale (NOS). The results were discussed with a third investigator, and any discrepancies were resolved by consensus.
Statistical analysis
We used Review Manager Version 5.3 software (Cochrane Collaboration) to analyze the data. To account for the differences between thermal ablation and conventional thyroidectomy, odds ratios (ORs) with 95% confidence intervals (95% CIs) were used to analyze hoarseness and postoperative pain; risk differences (RDs) with 95% CIs were used to analyze hypothyroidism; standard mean differences (SMDs) with 95% CIs were used to analyze hospitalization time; and relative risk (RR) ratios with 95% CIs were used to analyze symptom improvement and postoperative cosmetic effects. For all analyses, p < 0.05 was considered statistically significant.
Heterogeneity was assessed using the chi-square test and I2 statistic. For the chi-square test, p > 0.1 indicates no heterogeneity. When p ≤ 0.1, the I2 statistic was performed for further evaluation of heterogeneity (I2 ≥ 25%, low heterogeneity; I2 ≥ 50%, moderate heterogeneity; I2 ≥ 75%, significant heterogeneity). A fixed-effects model was suitable for data with no or low heterogeneity; otherwise, a random-effects model was used [Citation15,Citation16]. When heterogeneity was significant, we performed subgroup and sensitivity analyses to estimate heterogeneity and explore the source of the heterogeneity.
Funnel plots were used to assess publication bias. When a funnel plot is symmetrical, no publication bias exists. Otherwise, publication bias should be considered [Citation17].
Results
Literature retrieval
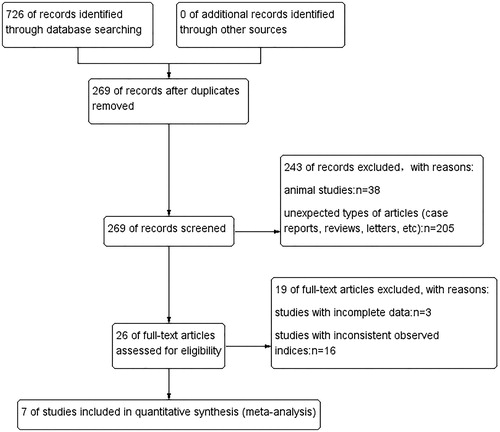
Initially, 726 records were identified in the target databases. After deleting duplicate records, we considered 269 articles for inclusion. We narrowed the scope to 26 articles by browsing the titles and abstracts of these articles. Thirty-eight animal studies and 205 unexpected types of articles (case reports, reviews, letters, etc.) were excluded. Then, we analyzed the full texts of the remaining 26 studies, removed studies with incomplete data or inconsistently observed indices, and finally obtained 7 studies (involving 1289 patients) ().
Data extraction and data quality assessment
The data extracted from the 7 included studies (1 RCT and 6 cohort studies) are shown in [Citation5,Citation18–23]. Propensity score matching was performed in the included studies to balance all baseline covariates between the thermal ablation group and the conventional thyroidectomy group. The patients’ baseline characteristics are reported in . We assessed the quality of the RCTs according to the risk of bias using the Cochrane Collaboration tool. For the cohort studies, we used the NOS, and the assessments are shown in and , respectively.
Table 1. Characteristics of the included studies.
Table 2. Patients’ characteristics at baseline.
Table 3. Risk of bias of randomized controlled trial.
Table 4. Quality assessment of cohort studies.
Safety
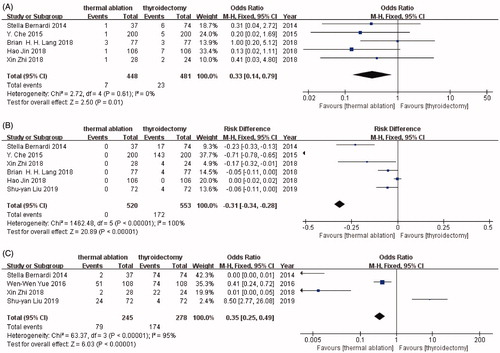
The meta-analysis results showed that the incidences of hoarseness [OR 0.33, 95% CI (0.14, 0.79)], hypothyroidism [RD −0.31, 95% CI (−0.34, −0.28)] and postoperative pain [OR 0.35, 95% CI (0.25, 0.49)] (p < 0.05) were significantly lower in the thermal ablation group than in the conventional thyroidectomy group. The incidence of hoarseness was 1.56% (7/448) in the thermal ablation group and 4.78% (23/481) in the conventional thyroidectomy group. The incidence of hypothyroidism was 0% (0/520) in the thermal ablation group and 31.10% (172/553) in the conventional thyroidectomy group. The incidence of postoperative pain was 32.24% (79/245) in the thermal ablation group and 62.59% (174/278) in the conventional thyroidectomy group. The chi-square test and I2 statistic indicated no heterogeneity in terms of hoarseness (I2 = 0%, p = 0.61), while significant heterogeneity was observed in terms of hypothyroidism (I2 = 100%, p < 0.00001) and postoperative pain (I2 = 95%, p < 0.00001). Therefore, we summarized the data for hoarseness with a fixed-effects model, while hypothyroidism and postoperative pain were summarized with a random-effects model (). Subgroup analyses and a sensitivity analysis for hypothyroidism and postoperative pain showed that the sources of heterogeneity were the study by CHE [Citation19] and the study by YUE [Citation18], respectively. Removing the studies had no effect on the results.
Figure 2. (A) Forest plot of hoarseness. Forest plot of hoarseness analyzed by odds ratio (OR) with 95% confidence intervals. The size of the data markers indicates the weight in the analysis. (B) Forest plot of hypothyroidism. Forest plot of hypothyroidism analyzed by risk difference (RD) with 95% confidence intervals. The size of the data markers indicates the weight in the analysis. (C) Forest plot of postoperative pain. Forest plot of postoperative pain analyzed by odds ratio (OR) with 95% confidence intervals. The size of the data markers indicates the weight in the analysis.
Efficacy
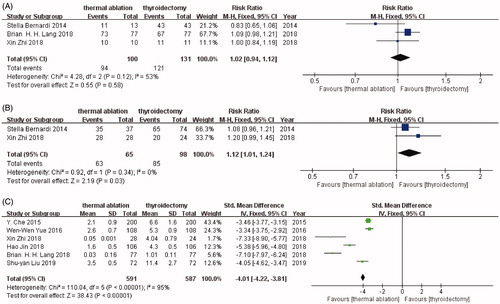
In terms of symptom improvement, the difference between thermal ablation and conventional thyroidectomy was not statistically significant [RR 1.02, 95% CI (0.94, 1.12)] (p = 0.58). The chi-square test and I2 statistic indicated moderate heterogeneity (I2 = 53%, p = 0.12) (). However, thermal ablation yielded significantly better postoperative cosmetic effects [RR 1.12, 95% CI (1.01, 1.24)] and was associated with a shorter hospitalization time [SMD −4.01, 95% CI (−4.22, −3.81)] than conventional thyroidectomy (p < 0.05) (). The chi-square test and I2 statistic indicated no heterogeneity (I2 = 0%, p = 0.34) in postoperative cosmetic effects but significant heterogeneity (I2 = 95%, p < 0.00001) in hospitalization time. The results of the sensitivity analysis for hospitalization time were stable. Subgroup analyses of hospitalization time were conducted according to the publication year, study type and ablation method, but no source of heterogeneity was found.
Figure 3. (A) Forest plot of symptom improvement. Forest plot of symptom improvement analyzed by relative risk (RR) ratio with 95% confidence intervals. The size of the data markers indicates the weight in the analysis. (B) Forest plot of postoperative cosmetic effect. Forest plot of postoperative cosmetic effect analyzed by relative risk (RR) ratio with 95% confidence intervals. The size of the data markers indicates the weight in the analysis. (C) Forest plot of hospitalization time. Forest plot of hospitalization time analyzed by standard mean difference (SMD) with 95% confidence intervals. The size of the data markers indicates the weight in the analysis.
Publication bias
A funnel plot suggested that publication bias of the included literature was less likely.
Discussion
This systematic review and meta-analysis of 1289 patients provides strong evidence through a comparison between thermal ablation and conventional thyroidectomy for the treatment of benign TNs. This study shows that, for benign TNs, ultrasound-guided thermal ablation may offer potential advantages in terms of safety, cosmetic effects and reduced hospitalization time compared with conventional thyroidectomy, while symptom improvement is the same.
Conventional thyroidectomy is the standard therapy for benign TNs requiring treatment, but it is not always the best choice. This method may lead to complications, cosmetic concerns, long hospital stays and other problems [Citation24–26]. Whether it is worthwhile for patients to experience these problems in the course of treatment for benign disease is controversial [Citation27]. Additionally, some patients’ poor health conditions make them unfit for thyroidectomy. Ultrasound-guided thermal ablation may be an excellent potential alternative treatment for benign TNs. The efficacy of thermal ablation for benign TNs has been demonstrated [Citation28–30]. However, for benign TNs, it remains unknown whether thermal ablation is equivalent or even superior to conventional thyroidectomy. To our knowledge, no systematic reviews or meta-analyses evaluating the differences in safety and efficacy between ultrasound-guided thermal ablation and conventional thyroidectomy for benign TNs have been conducted.
This study shows that thermal ablation is safer than conventional thyroidectomy. Safety is a very important consideration when choosing a treatment for benign TNs. Serious complications resulting from the treatment of benign disease make the loss outweigh the gain. When the efficacy of different treatments is similar, we prefer to adopt thermal ablation. This view is consistent with some published guidelines and recommendations [Citation31–33] on the treatment of TNs by thermal ablation. In a consensus [Citation33] published by 29 physicians, based on literature review and consensus opinion of interdisciplinary experts, the possibility of thermal ablation as a first-line treatment for benign TNs was clearly proposed. In this study, we compare the safety of thermal ablation and conventional thyroidectomy in terms of three aspects: hoarseness, hypothyroidism and postoperative pain. Based on the previous systematic review of Mainini et al. [Citation3] and Ha et al. [Citation34], thermal ablation performed well in terms of safety. The incidence of major complications (including hoarseness and hypothyroidism) ranged from 0% (0/65) to 3.9% (9/233), and the incidence of minor complications (including postoperative pain) ranged from 0% (0/20) to 38.3% (224/584), which is consistent with our findings. In our study, the incidence of hoarseness was 1.56% (7/448) in the thermal ablation group and 4.78% (23/481) in the conventional thyroidectomy group; for hypothyroidism, it was 0% (0/520) and 31.10% (172/553); for postoperative pain, it was 32.24% (79/245) and 62.59% (174/278), respectively. Our study showed that thermal ablation was superior to conventional thyroidectomy in the above aspects.
Hoarseness is a common major complication after thyroidectomy that may seriously affect the quality of life of patients. Our study showed that thermal ablation was superior to conventional thyroidectomy in terms of hoarseness, and the absence of heterogeneity indicated that the results were reliable. When thermal ablation is used to treat benign TNs, hydrodissection can be used to protect important blood vessels and nerves adjacent to TNs. Those who have difficulty implementing the hydrodissection technique can also choose to forego the treatment of dangerous areas adjacent to important blood vessels or nerves and instead only perform thermal ablation in relatively safe areas. Therefore, the incidence of hoarseness caused by thermal ablation is reasonably low.
Our study shows that the incidence of hypothyroidism in the thermal ablation group was significantly lower than that in the conventional thyroidectomy group. The impact on thyroid function is another important consideration in the treatment of benign TNs. Some patients may have hypothyroidism after surgery and will require lifelong levothyroxine, which will not only increase the financial burden but also cause long-term problems. Hypothyroidism occurred in none of the 520 patients in our study who underwent thermal ablation. However, the chi-square test and I2 statistic indicated significant heterogeneity (I2 = 100%, p < 0.00001). Subgroup analyses and a sensitivity analysis showed that the source of heterogeneity was the study by CHE [Citation19]. This may be because of the large proportion (151/200) of patients who underwent total thyroidectomy, resulting in a relatively large proportion (143) of hypothyroidism in the conventional thyroidectomy group, which was much more than the proportion in the other studies. Since removing the study of CHE [Citation19] had no effect on the results, we consider the results to be valid. Thermal ablation is a delicate treatment performed under ultrasound guidance, and this technique causes less damage to normal thyroid tissue around TNs. Therefore, patients with normal thyroid function rarely experience hypothyroidism after ablation. We believe that this is the most important advantage of thermal ablation.
Although postoperative pain is not a serious complication, it is still an indicator of great concern to patients. In this study, the incidence of postoperative pain in the thermal ablation group was significantly lower than that in the conventional thyroidectomy group. The chi-square test and I2 statistic for postoperative pain indicated significant heterogeneity (I2 = 95%, p < 0.00001). A sensitivity analysis showed that the source of heterogeneity was the study by YUE [Citation18]. We suspect that this finding might be related to the pain grading method, the timing of pain assessment or the anesthetic method used for thermal ablation; however, these factors were not elaborated in the articles, so our hypotheses cannot be verified. Although the heterogeneity of postoperative pain was significant, removing the study of YUE [Citation18] had no effect on the results, so we propose that the results are valid. Since thermal ablation is a minimally invasive treatment compared with thyroidectomy, it is reasonable that this approach will cause less postoperative pain.
In addition to safety, another important concern in the treatment of benign TNs is efficacy. Since patients with benign TNs mainly undergo treatment due to symptoms of compression and cosmetic problems, we mainly compared the efficacy of thermal ablation and conventional thyroidectomy in terms of symptom improvement, postoperative cosmetic effects and hospitalization time. Previous studies [Citation35–39] have shown that the volume of benign TNs can be significantly reduced within 12 months after treatment with any kind of thermal ablation, and this reduction in size will continue during long-term follow-up. Some recent meta-analyses [Citation40,Citation41] have indicated that thermal ablation can not only significantly reduce the volume of benign nonfunctioning solid TNs, but also be effective for autonomous functioning TNs. Therefore, both conventional thyroidectomy and thermal ablation can significantly improve the patient’s symptoms. Our included clinical trials showed that the benign TN volume decreased significantly after thermal ablation, and the nodules continued to shrink over time. The difference between thermal ablation and conventional thyroidectomy was not statistically significant in terms of symptom improvement (p = 0.58). Therefore, the efficacy of thermal ablation can be considered to be the same as that of thyroidectomy. We also compared the postoperative cosmetic effects and hospitalization time of the two treatments. As thermal ablation is a minimally invasive treatment, patients may experience better cosmetic satisfaction and shorter hospitalization times. These findings were confirmed in our study. Thermal ablation performed better in terms of the postoperative cosmetic effects and showed no heterogeneity (I2 = 0%, p = 0.34), which indicated that the results were reliable. As thermal ablation is a minimally invasive treatment (the surgical incision is only 1–2 mm for laser, radiofrequency and microwave ablation, and there is no wound for high-intensity focused ultrasound ablation), the cosmetic effects after thermal ablation are significantly better than those after conventional thyroidectomy. Furthermore, because of the rapid recovery after minimally invasive treatment, the hospitalization time of patients treated with thermal ablation is considerably shorter than that of patients treated with conventional thyroidectomy.
Although thermal ablation is superior to conventional thyroidectomy in many aspects, it should be noted that the pathological results before thermal ablation were obtained by fine-needle aspiration (FNA) or core needle biopsy (CNB), which could yield false negative or false positive results. Therefore, we believe that patients should undergo thermal ablation only when the TN is confirmed to be benign by at least two FNAs or CNBs. Moreover, for some benign TNs that are located behind the sternum, the effect of thermal ablation is often unsatisfactory, in which case, conventional thyroidectomy should be the first-choice treatment [Citation42]. Consequently, we believe that a comprehensive preoperative evaluation should be performed that includes a reliable preoperative diagnosis and assesses the feasibility of thermal ablation. Only when these two conditions are simultaneously satisfied is thermal ablation preferred for benign TNs.
To our knowledge, our study is the first systematic review and meta-analysis to compare the safety and efficacy of thermal ablation and conventional thyroidectomy in terms of multiple parameters, including hoarseness, hypothyroidism, postoperative pain, symptom improvement, postoperative cosmetic effects and hospitalization time. The strengths of the review include the multilevel article screening system, the comprehensive and up-to-date search, the scientific assessment of evidence risk and publication bias and rigorous data extraction and analysis. Overall, our study had a low risk of bias. Although some results were heterogeneous, and sensitivity and subgroup analyses were performed, the results were still reliable.
It should be emphasized that inhomogeneity still exists in how the information of thermal ablation is presented and reported among different studies, which have not only caused some difficulties to our analysis, but also created barriers to academic exchanges between different institutions and doctors. The proposal of the Italian working group [Citation43] on the standardization of terminology and reporting criteria is really helpful to avoid such problems, which also reminds us of our future research.
There were some limitations in our study. First, because of some practical difficulties, such as patient recruitment, physical condition and subjective intention, there was not a sufficient number of RCTs for inclusion, which may have led to selection bias. Second, the selection of different surgical methods, including total thyroidectomy and hemithyroidectomy, may have led to bias. Third, to compare two completely different therapies, surgery and thermal ablation, we pooled several types of thermal ablation together for the analysis, which presented a meaningful hypothesis but may have led to bias. Finally, the included studies showed that the maximum follow-up period was up to one year after treatment, and there were not enough long-term follow-up data for further study.
Conclusion
This study shows that for benign TNs, ultrasound-guided thermal ablation may have potential advantages in terms of safety, cosmetic effects and shorter hospitalization time compared with conventional thyroidectomy, while symptom improvement is the same.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Sui WF, Li JY, Fu JH. Percutaneous laser ablation for benign thyroid nodules: a meta-analysis. Oncotarget. 2017;8(47):83225–83236.
- Yassa L, Cibas ES, Benson CB, et al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer. 2007;111(6):508–516.
- Mainini AP, Monaco C, Pescatori LC, et al. Image-guided thermal ablation of benign thyroid nodules. J Ultrasound. 2017;20(1):11–22.
- Efremidou EI, Papageorgiou MS, Liratzopoulos N, et al. The efficacy and safety of total thyroidectomy in the management of benign thyroid disease: a review of 932 cases. Can J Surg. 2009;52(1):39–44.
- Jin H, Fan J, Liao K, et al. A propensity score matching study between ultrasound-guided percutaneous microwave ablation and conventional thyroidectomy for benign thyroid nodules treatment. Int J Hyperthermia. 2018;35(1):232–238.
- Bayani M, Amani M, Moazezi Z. Efficacy of levothyroxine on benign thyroid nodule. Caspian J Intern Med. 2012;3(1):359–362.
- Bandeira-Echtler E, Bergerhoff K, Richter B. Levothyroxine or minimally invasive therapies for benign thyroid nodules. Cochrane Database Syst Rev. 2014;(6):CD004098. DOI:10.1002/14651858.CD004098.pub2
- Cervelli R, Mazzeo S, De Napoli L, et al. Radiofrequency ablation in the treatment of benign thyroid nodules: an efficient and safe alternative to surgery. J Vasc Interv Radiol. 2017;28(10):1400–1408.
- Korkusuz Y, Gröner D, Raczynski N, et al. Thermal ablation of thyroid nodules: are radiofrequency ablation, microwave ablation and high intensity focused ultrasound equally safe and effective methods? Eur Radiol. 2018;28(3):929–935.
- Lang BHH, Woo YC, Chiu KW. Sequential high intensity focused ultrasound (HIFU) ablation in the treatment of benign multinodular goitre: an observational retrospective study. Eur Radiol. 2018;28(8):3237–3244.
- Lang BHH, Woo YC, Chiu KW. Two-year efficacy of single-session high-intensity focused ultrasound (HIFU) ablation of benign thyroid nodules. Eur Radiol. 2019;29(1):93–101.
- Chen F, Tian G, Kong D, et al. Radiofrequency ablation for treatment of benign thyroid nodules: a PRISMA-compliant systematic review and meta-analysis of outcomes. Medicine. 2016;95(34):e4659.
- Chung SR, Suh CH, Baek JH, et al. Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J Hyperthermia. 2017;33(8):1–930.
- Higgins JPT, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(2):d5928.
- Melsen WG, Bootsma MCJ, Rovers MM, et al. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect. 2014;20(2):123–129.
- Higgins JP. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560.
- Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018;74(3):785–794.
- Yue W-W, Wang S-R, Lu F, et al. Quality of life and cost-effectiveness of radiofrequency ablation versus open surgery for benign thyroid nodules: a retrospective cohort study. Sci Rep. 2016;6(1):1–12.
- Che Y, Jin S, Shi C, et al. Treatment of benign thyroid nodules: comparison of surgery with radiofrequency ablation. AJNR Am J Neuroradiol. 2015;36(7):1321–1325.
- Bernardi S, Dobrinja C, Fabris B, et al. Radiofrequency ablation compared to surgery for the treatment of benign thyroid nodules. Int J Endocrinol. 2014;2014:1–10.
- Zhi X, Zhao N, Liu Y, et al. Microwave ablation compared to thyroidectomy to treat benign thyroid nodules. Int J Hyperthermia. 2018;34(5):644–652.
- Lang BHH, Wong CKH, Ma EPM, et al. A propensity-matched analysis of clinical outcomes between open thyroid lobectomy and high-intensity focused ultrasound (HIFU) ablation of benign thyroid nodules. Surgery. 2019;165(1):85–91.
- Liu S-Y, Guo W-H, Yang B, et al. Comparison of stress response following microwave ablation and surgical resection of benign thyroid nodules. Endocrine. 2019;65(1):138–143.
- Billmann F, Bokor-Billmann T, Lapshyn H, et al. Minimal-access video-assisted thyroidectomy for benign disease: a retrospective analysis of risk factors for postoperative complications. Int J Surg. 2014;12(12):1306–1309.
- Bauer PS, Murray S, Clark N, et al. Unilateral thyroidectomy for the treatment of benign multinodular goiter. J Surg Res. 2013;184(1):514–518.
- Nouraei SAR, Allen J, Kaddour H, et al. Vocal palsy increases the risk of lower respiratory tract infection in low-risk, low-morbidity patients undergoing thyroidectomy for benign disease: a big data analysis. Clin Otolaryngol. 2017;42(6):1259–1266.
- Gangappa RB, Kenchannavar MB, Chowdary PB, et al. Total thyroidectomy for benign thyroid diseases: what is the price to be paid? J Clin Diagn Res. 2016;10(6):PC04–PC07.
- Papini E, Rago T, Gambelunghe G, et al. Long-term efficacy of ultrasound-guided laser ablation for benign solid thyroid nodules. Results of a three-year multicenter prospective randomized trial. J Clin Endocrinol Metab. 2014;99(10):3653–3659.
- Mortensen LS, Smidt K, Jorgensen A, et al. Long-term parathyroid- and c-cell function after radioiodine for benign thyroid diseases. Basic Clin Pharmacol Toxicol. 2005;97(1):22–28.
- Deandrea M, Limone P, Basso E, et al. US-guided percutaneous radiofrequency thermal ablation for the treatment of solid benign hyperfunctioning or compressive thyroid nodules. Ultrasound Med Biol. 2008;34(5):784–791.
- Kim J-H, Baek JH, Lim HK, et al. 2017 Thyroid radiofrequency ablation guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018;19(4):632–655.
- Dietrich CF, Müller T, Bojunga J, et al. Statement and recommendations on interventional ultrasound as a thyroid diagnostic and treatment procedure. Ultrasound Med Biol. 2018;44(1):14–36.
- Papini E, Pacella CM, Solbiati LA, et al. Minimally-invasive treatments for benign thyroid nodules: a Delphi-based consensus statement from the Italian minimally-invasive treatments of the thyroid (MITT) group. Int J Hyperthermia. 2019;36(1):376–382.
- Ha EJ, Baek JH, Kim KW, et al. Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and bayesian network meta-analysis. J Clin Endocrinol Metab. 2015;100(5):1903–1911.
- Ji Hong M, Baek JH, Choi YJ, et al. Radiofrequency ablation is a thyroid function-preserving treatment for patients with bilateral benign thyroid nodules. J Vasc Interv Radiol. 2015;26(1):55–61.
- Ugurlu MU, Uprak K, Akpinar IN, et al. Radiofrequency ablation of benign symptomatic thyroid nodules: prospective safety and efficacy study. World J Surg. 2015;39(4):961–968.
- Feng B, Liang P, Cheng Z, et al. Ultrasound-guided percutaneous microwave ablation of benign thyroid nodules: experimental and clinical studies. Eur J Endocrinol. 2012;166(6):1031–1037.
- Valcavi R, Riganti F, Bertani A, et al. Percutaneous laser ablation of cold benign thyroid nodules: a 3-year follow-up study in 122 patients. Thyroid. 2010;20(11):1253–1261.
- Kovatcheva RD, Vlahov JD, Stoinov JI, et al. Benign solid thyroid nodules: US-guided high-intensity focused ultrasound ablation-initial clinical outcomes. Radiology. 2015;276(2):597–605.
- Trimboli P, Castellana M, Sconfienza LM, et al. Efficacy of thermal ablation in benign non-functioning solid thyroid nodule: a systematic review and meta-analysis. Endocrine. 2020;67(1):35–43.
- Cesareo R, Palermo A, Benvenuto D, et al. Efficacy of radiofrequency ablation in autonomous functioning thyroid nodules. A systematic review and meta-analysis. Rev Endocr Metab Disord. 2019;20(1):37–44.
- Chen AY, Bernet VJ, Carty SE, et al. American Thyroid Association statement on optimal surgical management of goiter. Thyroid. 2014;24(2):181–189.
- Mauri G, Pacella CM, Papini E, et al. Image-guided thyroid ablation: proposal for standardization of terminology and reporting criteria. Thyroid. 2019;29(5):611–618.