Abstract
Objective
To compare the postoperative hypocalcemia between ultrasound-guided microwave ablation (MWA) and total parathyroidectomy (TPTX) for secondary hyperparathyroidism (SHPT).
Methods
The retrospective study reviewed 286 SHPT patients (171 received MWA and 115 underwent TPTX) between March 2018 and May 2019. Propensity-score matching was used to assemble a cohort of patients with similar baseline characteristics. A total of 184 SHPT patients (92 in each group) were finally enrolled, the occurrence and prognosis of postoperative hypocalcemia were compared. And the risk factors associated with severe hypocalcemia (SH) in each group were analyzed.
Results
Hypocalcemia encountered in 95cases (49 in the MWA group and 46 in the TPTX group). SH occurred in 76 cases (40 in the MWA group and 36 in the TPTX group). There were no statistically significant differences in the detection time, incidence, minimum value of serum calcium and symptomatic hypocalcemia between MWA and TPTX group (all p values > 0.05). Of patients developing hypocalcemia, serum calcium did not recover to normal range in 5 cases (10.2%) in the MWA group, while 13 cases (28.3%) were still hypocalcemia at 6 months follow-up in TPTX group (p = 0.035). The time to recovery from hypocalcemia in the TPTX group (mean 30 days, range 3–180 days) was longer than the WA group (mean 14 days, range 3–126 days) (p = 0.000). High serum alkaline phosphatase (ALP) level and low serum calcium level were the main risk factors of postoperative SH.
Conclusion
There was no difference in hypocalcemia between MWA and TPTX group. Hypocalcemia in the TPTX group might need a longer time to recover.
Introduction
Secondary hyperparathyroidism (SHPT) is a common complication of end-stage renal disease (ESRD) which causes disorders in mineral and bone metabolism and results in cardiovascular diseases or even death [Citation1,Citation2]. Parathyroidectomy (PTX) is recommended in most practical guidelines for SHPT patients who are refractory to medical therapy [Citation2–4]. It can effectively decrease parathyroid hormone (PTH), relieve symptoms, improve quality of life and reduce complications and mortality [Citation5,Citation6]. Recently, as a new effective surgical approach for SHPT, ultrasound (US)-guided percutaneous microwave ablation (MWA) has been preliminarily applied in clinical practice and demonstrated its superiority [Citation7–9].
However, with the removal or inactivation of hyperplastic parathyroid glands, the level of PTH sharply decreases. Intestinal absorption of calcium reduces, while bone deposition accelerates, leading to hypocalcemia [Citation10,Citation11]. Hypocalcemia further increases the difficulty of SHPT treatment and affects the outcome of the disease. Severe hypocalcemia (SH) could lead to low blood pressure, convulsions, fractures, seizures, cardiac arrhythmia and even sudden death.
According to the previous studies, the incidence of postoperative hypocalcemia and SH in SHPT patients ranges from 70% to 90% and from 37% to 57%, respectively [Citation12,Citation13]. Hypocalcemia and SH were also common in 37.6% and 22.1% SHPT patients after MWA [Citation14,Citation15]. As the principles and strategies of these two surgical methods are completely different, the occurrence of postoperative hypocalcemia will have their own characteristics. However, investigators in previous studies have mainly focused on comparing the feasibility and therapeutic effectiveness of these two methods. A meta-analysis indicated that thermal ablation reduced the risk of hypocalcemia compared with PTX, because the PTH value remained relatively high after thermal ablation [Citation9]. However, there might be some bias and heterogeneity because the comparison of hypocalcemia involved a variety of thermal ablation methods and multiple PTX produces. As far as we know, there has been no such comparative study to systematically analyze the occurrence and prognosis of hypocalcemia after one kind of thermal ablation method or surgical procedure. Therefore, the purpose of this study was to compare the postoperative hypocalcemia between ultrasound-guided MWA and TPTX for SHPT.
Materials and methods
Patients
This retrospective study protocol was approved by the Human Ethics Review Committee of the China-Japan Friendship Hospital (2015-GZR-77). Written informed consent for treatment procedures was obtained from each patient.
The medical records of all patients with SHPT who underwent ultrasound-guided MWA or TPTX between March 2018 and May 2019 in our hospital were reviewed. Demographics, relative clinical symptoms, laboratory indicators, imaging findings and treatment variables were recorded. Propensity-score matching was used to assemble a cohort of patients with similar baseline characteristics. The incidence, severity, clinical manifestations and outcome of hypocalcemia were compared between MWA and TPTX group. Other complications were recorded and compared between these two groups as well. Clinical parameters, laboratory indices and parathyroid gland characteristics were analyzed to assess risk factors associated with SH in the two groups.
Inclusion and exclusion criteria
The inclusion criteria were (1) patients with maintenance hemodialysis complicated with SHPT. (2) symptomatic patients (e.g. bone pain, pruritus and other relative symptoms affecting the quality of life). (3) SHPT patients who were resistant to medication, with uncontrolled hypercalcemia or/and hyperphophatemia. (4) Intact PTH > 800 pg/mL. (5) Hyperparathyroidism > 6 months, and (6) at least one enlarged parathyroid gland with a sharp margin and complete capsule that was clearly shown on ultrasound.
The exclusion criteria were (1) previous PTX or thermal ablation; (2) history of parathyroid or other neoplasms in the neck region, (3) prothrombin time longer than 18 s, prothrombin activity lower than 60%, and platelet count less than 60 × 109 cells/L, or (4) intractable coexisting morbidity, such as cardiac insufficiency or severe hypertension.
Patients meeting all the above inclusion criteria were enrolled. Surgery was the first-line therapy choice for enrolled SHPT patients. MWA was performed for patients who refuse or were not suitable for surgery.
Microwave equipment and technique
A microwave generator and a 17-gauge internally cooled applicator antenna with a 0.3-cm tip (Intelligent Basic Microwave Tumor Ablation System; Nanjing ECO Microwave System, Nanjing, China) were applied. LOGIQ E9 US system (GE Healthcare, Waukesha, WI) equipped with a 6–15 MHz linear-array transducer was used.
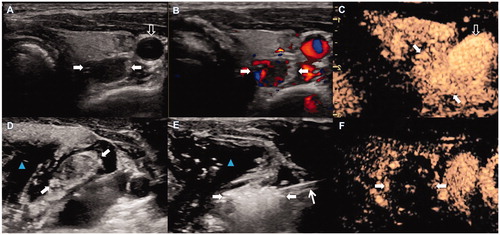
Patients were placed in a supine position with neck extended. After the neck was sterilized, 40–60 ml of normal saline (NS) was first injected into the area around the parathyroid nodule to provide hydrodissection. Then, a lidocaine and NS mixture (1:3) was injected close to the peri-parathyroid capsule for local anesthesia. The antenna was inserted freehand into the parathyroid gland under US guidance. A multipoint ablation strategy was adopted, where the power was 30 W and the radiation time was 15–25 s at each ablation point [Citation16]. The therapy was terminated when the hyperechoic zone covered the entire nodule. After ablation, contrast-enhanced US (SonoVue; Bracco, Milan, Italy) was used to evaluate the efficacy of ablation. If a non-enhanced zone covered the ablated nodule, complete ablation was achieved; if there was enhancement inside the ablation zone, an additional ablation was performed immediately. After complete ablation on one side, the procedure continued on the contralateral side if there was no voice change and no abnormal vocal cord movement on the US ().
Figure 1. Percutaneous MWA of SHPT nodule in a 56-year-old man. Routine US showed a hypoechoic SHPT nodule (white arrows) behind left lobe of thyroid and on right side of carotid artery (black arrow). B. Color Doppler US showed abundant blood flow signals in the nodule (arrows). C. Uniform hyperenhanced SHPT nodule (white arrows) was beside carotid artery (black arrow) in arterial phase on CEUS. D. Injection of hydrodissection (blue arrowhead) around SHPT nodule (white arrows) before MWA. E. MWA procedure of SHPT nodule: hyperechoic area emerging inside nodule (arrows)-which surrounded by hydrodissection (blue arrowhead), around antenna (white arrowhead). F. After MWA, nonenhancement area covered SHPT nodule (arrows) in CEUS image. CEUS: contrast-enhanced US; MWA: microwave ablation; SSHPT: secondary hyperparathyroidism; US: ultrasound.
TPTX procedure
After successful general anesthesia, the patient took a supine position, shoulder pillow, head back and routine sterilized. Two transverse fingers were taken from the sternal notch, and the transverse neck incision along the dermatoglyphic direction was about 5–8 cm. Skin, subcutaneous tissue and muscle were cut layer by layer to fully dissociate, and bilateral sternohyoid and thyroid muscles were separated to detect parathyroid glands and perform PTX. The ipsilateral recurrent laryngeal nerve (RLN) was explored by nerve monitor to protect it intraoperatively. Hemostasis was fully achieved and the incision was sutured layer by layer. All patients underwent bilateral neck exploration with an attempt to identify all parathyroid glands. All identifiable parathyroid glands were removed without doing any autotransplantation.
Definition of hypocalcemia
Hypocalcemia, indicated by a serum calcium concentration below 2.0 mmol/L (normal range, 2.0–2.75 mmol/L), was further classified as mild-moderate (total serum calcium 1.875–2.0 mmol/L) and severe (total serum calcium <1.875 mmol/L) [Citation11].
Perioperative treatment strategy
All patients started on oral administration of elemental calcium (1.8 g/d) and calcitriol (0.5 μg/d) one week before the operation. Hemodialysis was performed the day before the operation. After operation, serum calcium was monitored at 2 h, once a day within 1 week, 1 month and then at 3 months intervals. Patients received a high calcium dialysis bath (1.5 mmol/L or 1.75 mmol/L) according to the level of serum calcium. If serum calcium was less than 1.8 mmol/L or symptoms of hypocalcemia were present, intravenous calcium was initiated. If serum calcium level was between 1.8–2.1 mmol/L, elemental calcium (1–2 g/d) and calcitriol (1.5–3μg/d) were given. If serum calcium level was 2.1 mmol/L or above, intravenous calcium was stopped, calcium and active vitamin D were gradually reduced.
Outcomes
The primary outcome of the study was the incidence, clinical symptoms and recovery time of hypocalcemia in MWA and TPTX groups. Various secondary outcomes were also assessed, including complications deriving from the two treatments and the risk factors associated with SH.
Statistical analysis
All statistical analyses were performed using SPSS software (version 20.0 for Windows; IBM, Armonk, NY) and Stata version 15.0 (StataCorp, College Station, TX, USA). Continuous data were presented as the mean ± standard deviation or median and interquartile range. Differences among categorical variables were analyzed with a chi-square test, and a t-test was used for continuous variables. Propensity-score matching was used to identify a cohort of patients with similar baseline characteristics and a reduction rate of iPTH 2 h after operation. Matching was performed with the use of a 1:1 matching protocol without replacement (greedy-matching algorithm), with a caliper width equal to 0.2 of the standard deviation of the logit of the propensity score. Logistic stepwise regression with the forward selection of variables was adopted to explore the risk factors of SH. p < 0.05 was considered statistically significant.
Results
Patient characteristics
A total of 286 SHPT patients were reviewed, of whom 171 patients underwent ultrasound-guided MWA (MWA group) and 115 patients underwent TPTX (TPTX group). Before propensity-score matching, there were differences between the two groups in ureanitrogen, serum iPTH, phosphorus, alkaline phosphatase and volume of hyperplastic parathyroid glands. With the use of propensity – score matching, 92 patients who underwent MWA were matched with 92 patients who underwent TPTX. After matching, the baseline characteristics of patients were comparable between the two groups ().
Table 1. Baseline characteristics of patients undergoing MWA and TPTX before and after propensity-score matching.
The incidence of hypocalcemia and SH
Hypocalcemia episodes occurred in 95 patients (95/184, 51.6%), including 49 (49/92, 53.3%) patients in MWA group and 46 (46/92, 50%) patients in TPTX group. SH occurred in 76 cases (76/184, 41.3%), including 40 (40/92, 43.5%) patients in MWA group and 36 (36/92, 39.1%) patients in TPTX group. There was no significant difference of hypocalcemia and SH between MWA and TPTX (p = 0.768, p = 0.653). In the MWA group, hypocalcemia occurred within 1–7 days after treatment, and the mean minimum value of serum calcium was 1.68 ± 0.13 mmol/L. In the TPTX group, hypocalcemia occurred within 1–14 days after treatment, and the mean minimum value of serum calcium was 1.65 ± 0.24 mmol/L. There was no significant difference in the occurrence time of hypocalcemia and the minimum value of serum calcium between the two groups ().
Table 2. Comparison of hypocalcemia between MWA and TPTX group after propensity-score matching.
Symptoms associated with hypocalcemia
In the MWA group, symptomatic hypocalcemia accounted for 32.6% (15/49), including 13 cases of numbness, 1 case of palpitation, and 1 case of dyspnea. The patient with bilateral recurrent laryngeal nerve injury had post-MWA SH and presented with dyspnea. Symptoms were relieved after the correction of SH and oxygen intake. In the TPTX group, 16 patients (16/46, 34.8%) had symptomatic hypocalcemia. Eleven patients complained varying degrees of hand and foot numbness, 1 patient had palpitations, 2 patients manifested abdominal pain and diarrhea, and 2 cases developed symptoms like heart failure (clammy skin, hypotension, increased heart rate and rale). The above manifestations were improved after adequate supplementation of element calcium and calcitriol. The incidence of symptomatic hypocalcemia was not statistically significant between the two groups.
In the MWA group, skin necrosis occurred in two other SH patients due to the infusion of calcium gluconate. These two patients had skin grafts. One patient had an arteriovenous internal fistula blockage due to hypotension caused by hypocalcemia within 1 week after TPTX. Local urokinase thrombolysis was administered within 24 h.
Recovery of hypocalcemia
At 6 months of follow-up, serum calcium did not recover to normal range in 5 cases (10.2%) in the MWA group, while 13 cases (28.3%) were still hypocalcemia at follow-up in the TPTX group (p = 0.035). The recovery time of hypocalcemia in the TPTX group (mean 30 days, range 3–180 days) was longer than that of the MWA group (mean 14 days, range 3–126 days) (p = 0.000).
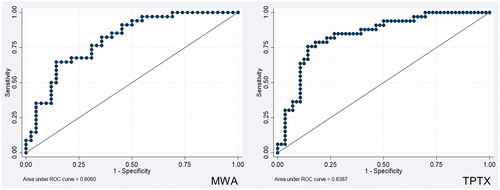
Risk factors of SH in MWA and TPTX group
In the MWA group, high ALP and ALB level, low serum calcium levels were risk factors for developing SH. In the TPTX group, high ALP level, low serum calcium levels and large gland volume were risk factors for developing SH (). The efficacy of the SH prediction model was promising in MWA (0.806) and TPTX (0.839) groups ().
Table 3. Factors influenced the development of SH in the two groups.
Complications in MWA and TPTX group
The complications occurred in the MWA and TPTX group were outlined in . The incidence of complications was comparable between the MWA group and the TPTX group (17.4% vs. 15.2%, p = 0.842). One patient in the MWA group sustained a permanent injury to a unilateral recurrent laryngeal nerve (RLN) and the patient who experienced external carotid artery pseudoaneurysm underwent local Thrombin injection (100 IU/mL, Pfizer Inc, New York). The remaining patients recovered without sequelae.
Table 4. Complications in SHPT patients who underwent MWA and TPTX.
Discussion
Hypocalcemia is the most common medical complication following PTX or thermal ablation. Our study showed that hypocalcemia usually occurred one week after MWA [Citation15]. However, in patients undergoing TPTX, although the serum calcium level tended to fall immediately after the operation, there might be a delay up to 2 weeks before it reached its lowest level. This was consistent with previous studies [Citation17]. It suggested that the severity of hypocalcemia and demand of calcium replacement resulting from accelerated bone formation might not be fully reflected by the serum calcium level early after operation. For some patients in the TPTX group, postoperative monitoring of hypocalcemia could be appropriately prolonged to provide guidance of calcium supplementation.
Our findings revealed that there was no difference between the two groups concerning the incidence of hypocalcemia and SH [Citation18], which was similar to the previous studies [Citation18,Citation19]. This indicated that MWA and TPTX were both effective surgical approaches for SHTP. The occurrence of hypocalcemia was not related to the surgical method itself, but mainly depended on the preoperative serum calcium and ALP levels, which were indicators of the bone metabolic status. High serum ALP indicated a high baseline bone-remodeling status before operation. The sudden decrease of the iPTH level could change the bone-remodeling status, from mainly bone resorption to mainly bone formation [Citation20,Citation21]. However, it was reported in a meta-analysis that the incidence of hypocalcemia after thermal ablation was lower than that of PTX [Citation9]. This could be attributed to thermal ablation methods and PTX procedures were rather variable in these studies. The majority underwent subtotal PTX or TPTX with autotransplantation while TPTX merely accounted for a minority.
Although the incidence of hypocalcemia was more than 50%, symptomatic hypocalcemia accounted for approximately 1/3 to 1/2 [Citation10,Citation22]. In this study, about 1/3 of the hypocalcemia patients had symptoms after MWA/TPTX, mainly manifested as hand-foot numbness, and a small number of patients presented with palpitations. Notably, individual patients show abdominal pain, diarrhea, and symptoms like heart failure. The above symptoms were improved after calcium and calcitriol supplement. In addition, the protection of recurrent laryngeal nerve was important as combined with SH could cause serious consequences. Therefore, for selected patients with high risk of SH, fractionated ablation might be planned [Citation14]. Cautions should also be given to arteriovenous internal fistula blockage related to hypocalcemia and skin necrosis caused by improper calcium supplementation. The adjustment of the dosage and pathway of calcium supplementation was very important.
Of the patients developing hypocalcemia, serum calcium did not recover to normal range in 28.3% patients in the TPTX group, while only in 10.2% patients in the MWA group at 6 months follow-up. It suggested that the recovery time of hypocalcemia was longer in TPTX than in MWA. As TPTX removes all four parathyroid glands to reduce the risk of secondary resection, ultrasound-guided MWA for SHPT completely inactivates the hyperplastic glands which can be displayed on ultrasound. Since the two surgical methods and treatment strategies are completely different, MWA sometimes requires multiple sessions to achieve the treatment purpose [Citation23]; the level of PTH may fluctuate during the follow-up, resulting in postoperative serum calcium value fluctuation. Persistence and/or recurrence SHPT was more common in thermal ablation [Citation9]. However, under the direct vision of TPTX, all hyperplastic glands were removed, the hungry bone symptoms lasted for a long time, and the recovery time of hypocalcemia was slow.
There are a few limitations to this study. First, this is a retrospective study, and a prospective study with more factors that may influence hypocalcemia is needed for more accurate results. Second, the study lacks model validation due to the relatively small number of SH subjects in both groups. Third, it is of significant clinical value to study the postoperative adjustment of medications used to treat calcium metabolism alterations due to renal failure.
Conclusions
The incidence of hypocalcemia has no significant difference between MWA and TPTX group. The recovery time of hypocalcemia was longer in the TPTX group. High serum ALP level and low serum calcium level were the main risk factors for developing SH.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379(9818):815–822.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2009;113:S1–130.
- Kestenbaum B, Andress DL, Schwartz SM, et al. Survival following parathyroidectomy among United States dialysis patients. Kidney Int. 2004; 66(5):2010–2016.
- Tominaga Y, Matsuoka S, Uno N. Surgical and medical treatment of secondary hyperparathyroidism in patients on continuous dialysis. World J Surg. 2009;33(11):2335–2342.
- Chen L, Wang K, Yu S, et al. Long-term mortality after parathyroidectomy among chronic kidney disease patients with secondary hyperparathyroidism: a systematic review and meta-analysis. Ren Fail. 2016;38(7):1050–1058.
- Tsai WC, Peng YS, Yang JY, et al. Short and long-term impact of subtotal parathyroidectomy on the achievement of bone and mineral parameters recommended by clinical practice guidelines in dialysis patients: a 12-year single center experience. Blood Purif. 2013;36(2):116–121.
- Zhuo L, Peng LL, Zhang YM, et al. US-guided microwave ablation of hyperplastic parathyroid glands: safety and efficacy in patients with end-stage renal disease – a pilot study. Radiology. 2017;282(2):576–584.
- Gong L, Tang W, Lu J, et al. Thermal ablation versus parathyroidectomy for secondary hyperparathyroidism: a meta-analysis. Int J Surg. 2019;70:13–18.
- Diao Z, Wang L, Li D, et al. Efficacy of microwave ablation for severe secondary hyperparathyroidism in subjects undergoing hemodialysis. Ren Fail. 2017;39(1):140–145.
- Mittendorf EA, Merlino JI, McHenry CR. Post-parathyroidectomy hypocalcaemia: incidence, risk factors, and management. Am Surg. 2004;70(2):114–119.
- Floege J, Tsirtsonis K, Iles J, et al. Incidence, predictors and therapeutic consequences of hypocalcemia in patients treated with cinacalcet in the EVOLVE trial. Kidney Int. 2018;93(6):1475–1482.
- Sun X, Zhang X, Lu Y, et al. Risk factors for severe hypocalcemia after parathyroidectomy in dialysis patients with secondary hyperparathyroidism. Sci Rep. 2018;8(1):7743
- Tsa WC, Peng Ys Chiu Yl, et al. Risk factors for severe hypocalcaemia after parathyroidectomy in prevalent dialysis patients with secondary hyperparathyroidism. Int Urol Nephrol. 2015;47:1203–1207.
- Wei Y, Peng LL, Zhao ZL, Li Y, et al. Complications encountered in the treatment of primary and secondary hyperparathyroidism with microwave ablation – a retrospective study. Int J Hyperthermia. 2019;36(1):1264–1271.
- Wei Y, Peng LL, Zhao ZL, Li Y, et al. Risk factors of severe hypocalcaemia after us-guided percutaneous microwave ablation of the parathyroid gland in patients with secondary hyperparathyroidism. J Bone Miner Res. 2020;35(4):691–697.
- Yu MA, Yao L, Zhang L, et al. Safety and efficiency of microwave ablation for recurrent and persistent secondary hyperparathyroidism after parathyroidectomy: a retrospective pilot study. Int J Hyperthermia. 2016;32(2):180–186.
- Viaene L, Evenepoel P, Bammens B, et al. Calcium requirements after parathyroidectomy in patients with refractory secondary hyperparathyroidism. Nephron Clin Pract. 2008;110(2):80–85.
- Jiang B, Wang X, Yao Z, et al. Microwave ablation vs. parathyroidectomy for secondary hyperparathyroidism in maintenance hemodialysis patients. Hemodial Int. 2019;23(2):247–253.
- Liu FY, Yu XY, Liu ZL, et al. Comparison of ultrasound-guided percutaneous microwave ablation and parathyroidectomy for primary hyperparathyroidism. Int J Hyperthermia. 2019;36(1):835–840.
- Ho LY, Wong PN, Sin HK, et al. Risk factors and clinical course of hungry bone syndrome after total parathyroidectomy in dialysis patients with secondary hyperparathyroidism. BMC Nephrol. 2017;18(1):12.
- Yang M, Zhang L, Huang L, et al. Factors predictive of critical value of hypocalcemia after total parathyroidectomy without autotransplantation in patients with secondary hyperparathyroidism. Ren Fail. 2016;38(8):1224–1227.
- Puccini M, Carpi A, Cupisti A, et al. Total parathyroidectomy without autotransplantation for the treatment of secondary hyperparathyroidism associated with chronic kidney disease: clinical and laboratory long-term follow-up. Biomed Pharmacother. 2010;64(5):359–362.
- Zeng Z, Peng CZ, Liu JB, et al. Efficacy of ultrasound-guided radiofrequency ablation of parathyroid hyperplasia: single session vs. two-session for effect on hypocalcemia. Sci Rep. 2020;10(1):6206.