Abstract
Background
To compare the short-term clinical outcomes of ultrasound-guided microwave ablation (MWA) and parathyroidectomy (PTX) for severe secondary hyperparathyroidism(SHPT).
Methods
In a prospective multi-center study, we compared the outcomes of MWA and PTX for severe SHPT. The outcome measures were case rate of successful treatment, improvement of clinical symptoms, incidence of complications, and differences in treatment parameters and costs between the two groups.
Results
A total of 167 eligible patients were included in the study, of which 79 underwent MWA and 88 underwent PTX. There was no significant difference in rate of successful treatment between the MWA and PTX groups (χ2=2.299, p = 0.125). However, the MWA group showed significantly lower range of intact parathyroid hormone (iPTH) decrease than the PTX group (t=−2.352, p = 0.023). Postoperative clinical symptoms improved in both groups, with no significant difference between the two groups (p > 0.05). Postoperative hypocalcemia was significantly more common in the PTX group (p < 0.05). The operative time, incision and postoperative pain of the MWA group were significantly better than those of the PTX group (p < 0.05), while postoperative recurrent laryngeal nerve injury and hematoma showed no significant difference between the two groups (p > 0.05). The cost of MWA was significantly less than PTX (p = 0.000).
Conclusions
Both MWA and PTX are effective and safe for severe secondary hyperparathyroidism. PTX is more thorough and traumatic, while MWA is minimally invasive and postoperative iPTH is more consistent with the Kidney Disease: Improving Global Outcomes (KDIGO) recommendation.
Introduction
End-stage renal disease (ESRD) is a global health problem, with the annual incidence rate of 1425 per million people [Citation1], and the prevalence rate is steadily increasing [Citation2,Citation3]. Secondary hyperparathyroidism (SHPT) is a common and serious complication of dialysis patients with chronic renal failure (CRF) [Citation4,Citation5], which can lead to multiple organ system involvement and death [Citation6]. Surgical treatment is necessary for patients with intractable hyperparathyroidism, and the reported surgical resection rate was 7–8 per 1000 person-years, which has remained unchanged for many years [Citation7]. In 2018, there were about 520,000 renal dialysis patients in China [Citation8]. About 60% of maintenance dialysis patients had different degrees of SHPT, and the compliance rate of intact parathyroid hormone (iPTH) control in these patients was only about 55%. Renal failure and its associated complications resulted in poor physical condition, such as cardiopulmonary dysfunction, and the patient's tolerance to surgery was poor, so the surgical rate of the remaining patients was only 2% (Dialysis Outcomes and Practice Patterns Study, DOPPS). Thermal ablation therapy has become a research hotspot since it is minimally invasive and has short operation time (more than 10 min). The preliminary results showed that microwave ablation (MWA) of SHPT has a significant effect [Citation9]. This study aimed to compare the outcomes of the two methods through a multi-center, prospective cohort study.
Materials and methods
The authors had complete control over the data and methods of the study. This prospective trial was approved by the ethics committee of the Beijing Friendship Hospital and registered at www.chictr.org.cn (ChiCTR1800018156) prior to patient recruitment. All patients provided signed informed consent before the study.
Participants
The patients presenting with SHPT to the Department of interventional ultrasound and surgical ward at the Beijing Friendship Hospital, China-Japan Friendship Hospital and People's Liberation Army General Hospital between June 2018 and May 2020 were enrolled in this study.
Inclusion and exclusion criteria
The inclusion criteria according to the consensus of clinical practice experts in surgical treatment of SHPT to CRF [Citation5] were:
iPTH >800 pg/ml;
Clinical manifestations: severe osteodynia, itchy skin and other symptoms affecting the quality of life, such as severe anemia and persistence of erythropoietin resistance;
Patients who met the diagnosis of SHPT, were resistant to calcium-sensitive receptor agonists, vitamin D and its analogues, hypercalcemia (serum calcium >4 mmol/L) or hyperphosphatemia (serum phosphorus >1.94 mmol/L);
Ultrasound indicated that at least one or more parathyroid glands had hyperplasia and diameter >1 cm, with abundant blood flow.
The exclusion criteria were:
Severe skeletal deformity and osteoporosis;
Combined with systemic diseases such as severe cardiopulmonary and brain dysfunction;
Severe coagulation dysfunction;
Ultrasound or radionuclide scans suggested ectopic parathyroid glands behind the sternum.
Patients with hyperplasia of parathyroids less than 4.
All patients first met with the clinic general surgeon and ablation practitioner, and the patients who met the inclusion criteria were divided into the ablation group and surgery group based on their choice.
Data extraction and quality assessment
The following data were extracted: efficacy, adverse events/complications, cost analysis, and social experience.
Efficacy included changes in iPTH, alkaline phosphatase (ALP), serum calcium (Ca), phosphorous (P) and clinical symptoms after treatment. According to expert consensus on surgical practice of SHPT to CRF [Citation5], postoperative iPTH levels <80% before surgery are considered to be completely removed. As a reference, 80% reduction of iPTH after ablation is considered complete ablation, less than 80% and greater than 50%, considered effective ablation. Evaluation scales such as visual analogue scale (VAS) for pain (ranging from 1 to 10) [Citation10], Athens Insomnia Scale (AIS) (ranging from 0 to 24) [Citation11], Sinicization of Four-item Itch Questionnaire (FIIQ) (ranging from 3 to 19) [Citation12], Quality of life VAS (that includes 12 items related to physical health, economic status, psychological status, etc.) were used to evaluate the clinical symptoms and social experience.
Before the start of the project, three centers jointly studied and determined the Case Report Form (CRF) tables and standard data determination tables. Data were independently extracted by one investigator at each center using standard data extraction forms. The lead center researcher managed and analyzed the data in a unified way.
Cost analysis included the procedure (ablation or surgery) as well as pre-procedural and post-procedural exams. Direct costs were related to hospitalization for MWA or surgery plus any costs associated with adverse events. Pricing was obtained from the hospital database. Indirect costs were evaluated using the human capital approach according to the Chinese guidelines for cost-effectiveness studies, and using the standard formula as follows:
Indirect costs = Gross Domestic Product (GDP) per capita × day × productive weight
Where productive weight is based on the internationally weighted value [Citation13]. The value of GDP per capita was based on the Beijing, China regional value estimate of Yuan 292 per day.
Procedures
Pretreatment evaluation
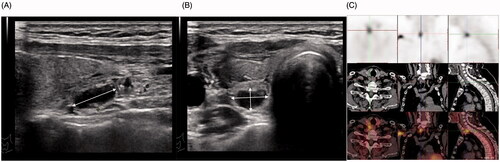
Pre-operative procedures included recording of disease history focusing on history of kidney disease and dialysis, symptoms. Laboratory tests of iPTH, ALP, Ca and P concentrations were performed. Routine blood work and clotting tests were also verified to be normal. Parathyroid ( and Citation2A) dimensions were measured with an ultrasound machine (Ascendus Color Doppler Ultrasound Diagnostic, Hitachi Medical Systems, Tokyo, Japan) using a 5–18 MHz linear matrix transducer to measure the length and diameter of the parathyroid. Radionuclide imaging (99mTc-MIBI; ) was used to confirm the number of parathyroid. Video laryngoscopy was used to check the vocal cords to judge the function of recurrent laryngeal nerve.
Figure 1. Sonogram of secondary hyperparathyroidism. A 45-year-old woman had been on dialysis for six years, and her ultrasound revealed an enlarged parathyroid gland, with (A) long parathyroid axis, (B) short parathyroid axis, and (C) radionuclide imaging.
MWA procedure
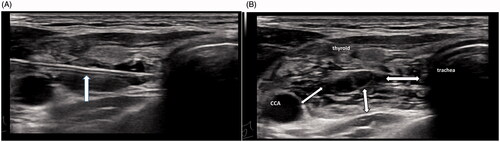
MWA was performed in an outpatient setting by an experienced physician, as previously reported [Citation9]. Microwave therapeutic equipment (KY-2000; Kangyou Medical, Nanjing, China) was used to administer microwave energy at a frequency of 2450 MHz. The microwave generator is capable of producing up to 100 W of power (30 W power was used in the study), with an antenna diameter of 2 mm, a total length of 100 mm and transmit segment length of 5 mm. Before ablation, intravenous access was achieved via the antecubital vein, and the patient’s partial pressure of oxygen (PO2), heart rhythm, respiratory rate and blood pressure were continuously monitored. SonoVue (Bracco, Italy) was used as the ultrasound contrast agent. The parathyroid blood supply was confirmed with contrast-enhanced ultrasound (CEUS) () and the ablation pathway was decided. Patients were placed in the supine position with their necks fully exposed. Routine neck disinfection was performed and 2% lidocaine was used for topical anesthesia. Key aspects of MWA technique included the following [Citation1]: To protect the carotid artery, recurrent nerve and other adjacent structures, a liquid insulation zone was used as a hydrodissection technique. Specifically, physiological saline refrigerated at 4–7 °C was injected into the area around the parathyroid as an isolation fluid to create a heat insulation layer (), so that the parathyroid glands exist as “an island” (). During ablation, the isolation liquid was continuously injected to ensure that the width of the isolation band was >1 cm, and the low-temperature isolation liquid could offset the diffusion of the ablation heat and ensure the safety of ablation [Citation2]. After creating the isolation zone, ablation process was started (). Mobile ablation method was used. The ablation was conducted from deep to shallow, and from far to near. The ablation needle tip began to move when hyperechoic bubbles appeared. When the ablation bubble high echo completely covered the parathyroid gland, the ablation was terminated. The patient’s voice was monitored during the operation, and the procedure was halted if dysphonia occurred [Citation3]. CEUS was performed, and if there was no enhancement of the entire parathyroid gland (), the procedure was discontinued.
Figure 2. Ultrasonography before and after parathyroid ablation of a 56-year-old man on dialysis for seven years. (A) Ultrasonography of secondary hyperparathyroidism. (B) Ablation bubbles filled the entire parathyroid gland during ablation. (C) Preoperative CEUS showed high enhancement of the parathyroid gland. (D) Postoperative CEUS showed no enhancement of the parathyroid.
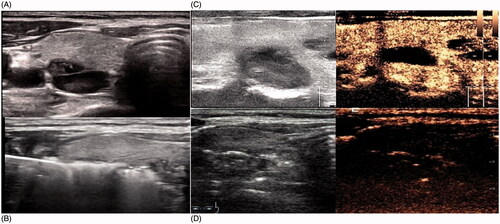
Figure 3. Ultrasonography of parathyroid isolation fluid. (A) The isolation needle was placed between the parathyroid gland and the trachea, then the isolation fluid was injected to widen the space between the parathyroid gland and the trachea. (B) The isolation band between the parathyroid gland and the surrounding should be >1 cm, so that the parathyroid gland can exist as a solitary island.
Surgical procedures
Three surgical options are available for parathyroidectomy as follows: subtotal parathyroidectomy (sPTX), total parathyroidectomy with autotransplantation (tPTX + AT), and total parathyroidectomy (tPTX). Currently, there is no consensus among endocrine surgeons on which operation is superior [Citation14,Citation15]. tPTX + AT involves removing all parathyroid tissue and re-implanting small pieces of tissue at a distance in well-vascularized muscular structures [Citation16,Citation17], which was performed in this study.
The surgeries were performed under general anesthesia. As a general principle, we constantly dissected and protected the recurrent laryngeal nerves in the procedures. If four parathyroid glands were definitively identified, the thymectomy was not performed. The parathyroid tissue was completely removed and non-nodular parathyroid tissues 30–60 mg (cut into 1 mm3) were implanted in 3–4 "muscle sacs" of sternocleidomastoid muscle that did not have hematoma. The transplantation site was marked with metal clip or other non-absorbable materials. All parathyroid glands were weighed, measured, and sent for pathological testing.
Follow-up evaluation
Laboratory tests of iPTH, ALP, Ca and P were performed at 2 h, 1 week, 1 month, and 3 months after the operation. Clinical symptoms, such as bone pain and itching, were reassessed at 2 h, 1 week, 1 month and 3 months, and insomnia and social experience that improved slowly were reassessed at 3 months after treatment. Each complication was recorded during and after treatment.
Statistical analysis
Data were analyzed using Excel for Windows, and statistical analysis was performed using SPSS version 22. Continuous variables were presented as mean ± SD or median (interquartile range), and categorical variables were presented as frequencies. The Student’s t-test (for normal distribution data) or Mann–Whitney U test (for skewed data) was used to compare numerical data, and chi-square analysis was used to compare categorical data. A p-value <0.05 was considered statistically significant, unless stated otherwise. Data were expressed as mean ± SEM for all continuous variables.
Results
Clinical data
A total of 167 eligible patients were included in the study, of which 79 underwent MWA and 88 underwent PTX. The study included 69 males and 98 females, with an age range of 25–79 years. The average period of hemodialysis was 7.92 years, with a range of 3.512 years. The operation was smoothly performed in all cases ().
Table 1. General information of the patients.
Efficacy comparison
The successful treatment cases in the MWA group was 86.08%, and that in the PTX group was 93.18%, with no statistical difference between the two groups (χ2=2.299, p = 0.125). However, the range of iPTH decline two hours after the operation in the MWA group was significantly lower than that in the PTX group (t=−2.352, p = 0.023) ( and ).
The symptoms of bone pain, itching and insomnia in the two groups were significantly improved after the operation, with no significant difference between the two groups (p > 0.05).
Table 2. The successful treatment cases.
Table 3. Postoperative follow-up data.
Comparison of complications and treatment procedures between the ablation group and the surgery group
Hypocalcemia
There were 21 cases of postoperative hypocalcemia in the ablation group and 45 cases in the surgery group, and the difference was statistically significant (p < 0.01) ().
Table 4. Complications and treatment procedures of the two groups.
Recurrent laryngeal nerve palsy (RLNP)
Regardless of TRLNP or PRLNP, there was no significant difference in RLNP between the ablation group and the surgery group (p > 0.05).
Postoperative hematoma
There was no case of postoperative bleeding in the ablation group, and five cases of postoperative hematoma in the surgical group, but the difference was not statistically significant (p > 0.05).
Postoperative pain
The ablation group had a surgical incision of about 0.2 cm and a pain score of about 1.8points (1 d after treatment), while the surgical group had a surgical incision of 5 cm and a pain score of 8.00, with a statistical difference (p < 0.01).
Treatment procedures
The duration of hospitalization and operation time of MWA group was shorter than that of the surgery group (p < 0.01). The postoperative scar length of the MWA group was smaller than that of the surgery group (p < 0.01).
Patient's sense of social experience (Quality of life VAS) and treatment cost
Postoperative quality of life VAS were significantly improved, with no statistical difference between the two groups (p > 0.05). However, there was significant difference in treatment costs between the two groups (p = 0.001) ().
Table 5. Quality of life VAS and treatment costs.
Discussion
Refractory hyperparathyroidism seriously affects patients' quality of life and increases mortality [Citation18]. Numerous studies have shown that hyperplastic parathyroidectomy can significantly improve clinical symptoms and reduce the risk of death [Citation19,Citation20], which was also recommended by KDIGO and Kidney Disease Outcomes Quality Initiative (KDOQI). But many dialysis patients suffer from cardiopulmonary dysfunction due to basic diseases, they cannot tolerate the trauma of surgery. Thermal ablation is widely used because of its advantages of less trauma, simple operation, and repeatability. Radiofrequency ablation, laser ablation and microwave ablation had been reported for the treatment of secondary hyperparathyroidism, and the efficacy were significant [Citation9,Citation21, Citation22]. Our data also showed that MWA could reduce iPTH and improve clinical symptoms as effectively as PTX + AT.
Although the postoperative iPTH in MWA was higher than that in PTX, it met the KDIGO recommendation that the iPTH of CKD-5 patients should be maintained at 2–9 times the upper limit of normal iPTH (0–65 pg/ml) [Citation23]. This was different from the surgery group wherein the parathyroid tissue was completely excised under direct vision, and the ablation was only to inactivate the parathyroid tissue. Although the CEUS showed no enhancement of the nodules, some residual nodules may have been present at the edges that could not be detected by ultrasound since the surrounding structures and organs could not be damaged. However, the research team found that with the proficiency and improvement of the ablation technology, the ablation effect was significantly improved compared to before, especially in the same institution [Citation24,Citation25]. KDOQI suggests not to reduce PTH to twice or less of the upper limit of iPTH detection (grade 2C), because over-inhibition of iPTH can lead to an increase in the prevalence of adynamic bone disease (ABD) [Citation26]. Many patients with ABD are asymptomatic, but some patients can have bone pain [Citation27], and these patients have an increased risk of fracture (possibly caused by the impairment of the ability to repair micro-injury), hypercalcemia and vascular calcification (visible on imaging), which are associated with increased mortality [Citation28,Citation29]. In this study, 80% of PTX cases were lower than the normal two-fold level, and SPTX was reported to have a high incidence of hypoparathyroidism [Citation30,Citation31], while some studies showed that the risk was the lowest when the PTH concentration was about 300 pg/ml [Citation32]. Based on these results, ablation treatment was recommended.
MWA and PTX are effective in the treatment of severe SHPT, but each operation has its complications or limitations. Hypocalcemia is a common complication of PTX and MWA. In patients with surgically removed or thermally ablated parathyroid glands, circulating iPTH suddenly drops, and the digestive tract shows insufficient calcium absorption, while the bones of SHPT patients are in the state of "bone hunger", so a large amount of calcium and phosphorus need to be absorbed from the blood for component compensation, resulting in the rapid transfer of a large amount of blood calcium to the previously decalcified bone, and the blood calcium level decreases rapidly. Our findings revealed that hypocalcemia occurred earlier and more seriously in the PTX group, especially in the older patients and those with higher iPTH before operation, and this phenomenon was related to the complete removal of parathyroid tissue by PTX.
Hoarseness is another common complication of treatment. Temporary hoarseness was caused by the compression of the nerves by the isolation fluid or temporary paralysis of lidocaine in the ablation group, and intraoperative nerve pulling in the surgical group. Generally, no treatment was required and both groups recovered within three months. Permanent hoarseness was caused by negative nerve damage leading to more than one year of hoarseness due to heat damage to the recurrent laryngeal nerve in the ablation group, and unintended cutting of the nerve in the surgery group. Transient hoarseness is more common in the ablation group, because the recurrent laryngeal nerve cannot be identified by ultrasound, in order to clearly separate the nerve from the parathyroid gland. So when the isolation fluid is injected, the nerve is affected by compression and traction, and lidocaine will also flow into the interstitial anesthesia nerve. Therefore, there is transient hoarseness in many cases, but no substantial damage to the nerve. There was no difference in the incidence of hoarseness between the two groups in this study.
Postoperative hemorrhage did not occur in the ablation group, while there were five cases in the surgery group, including two cases of hemostasis after compression, two cases of compression-induced hemostasis after suction under the guidance of ultrasound, one case continued to increase after aspiration and hemostasis was treated after surgical incision. The positive pain, numbness and appearance of the wound were much better in the ablation group than in the surgery group, and there was no psychological impact on the patients. Recurrent hyperparathyroidism after treatment was a serious complication related to clinical efficacy [Citation33]. Given the short follow-up time in this study, no recurring cases were seen in the two groups, but we will continue to follow-up the patients.
In terms of treatment costs, we found that the cost of MWA was less than that of surgical resection. Perhaps, the occasional medical expense had no significant impact on the quality of life for most families. However, for long-term dialysis patients, treatment costs accounted for a certain proportion of family income, and led to a heavy economic burden. In this study, there were 36 low-income patients (Ministry of Civil Affairs of the People's Republic of China 2019 standard, the monthly income per person in Beijing was less than 1,100 RMB, and in Hebei and other provinces it was about 600 yuan), of which 23 were in the ablation group, which indicated that the patients also considered economic costs in the selection of treatment.
This study had some limitations. Although both methods were proven to be effective for severe SHPT, the study did not follow the randomization principle, which inevitably led to certain deviations in the results. In addition, the ablation technique has relatively high requirements for surgeons to master the operational skills, which limits its widespread use.
Conclusion
In summary, both MWA and PTX are effective and safe for SHPT. PTX can remove the parathyroid more thoroughly, but is more traumatic. MWA is less traumatic and postoperative IPTH is more consistent with the KDIGO recommendation, but cannot completely inactivate tissue. Based on the findings of this study, in the selection of treatment options, it is necessary to meticulously consider the individual differences of patients to make the most suitable treatment choice.
Ethical approval
Informed consent was obtained from all the study participants.
Author contributions
Junfeng Zhao,Linxue Qian did the traditional ultrasound, contrast enhanced ultrasonography examinations and the ablation for the patient in Beijing Friendship Hospital and Junfeng Zhao contributed to manuscript drafting; Yujiang Liu, Xiaoqu Tan assisted ablation operation completed; Mingan Yu was in China-Japan Friendship Hospital, and Fangyi Liu was in the General Hospital of the Chinese People's Liberation Army to complete the ablation of secondary hyperparathyroidism; Changsheng Teng undertaked the surgical resection of secondary hyperparathyroidism; Linxue Qian and Jianming Li were responsible for the revision of the manuscript; all authors issued final approval for the version to be submitted.
Acknowledgments
Thanks are due to Junfeng Zhao, Linxue Qian, Changsheng Teng, Mingan Yu, Fangyi Liu, Yujiang Liu, Xiaoqu Tan, Jianming Li for assistance with the study and valuable discussion.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data set supporting the results of this article are included within the article.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2017 Annual Data Report: Epidemiology of kidney disease in the United States. Am J Kidney Dis. 2018;71(3 Suppl 1):A7.
- Brück K, Stel VS, Gambaro G, et al. CKD prevalence varies across the European general population. JASN. 2016;27(7):2135–2147.
- Ebert N, Jakob O, Gaedeke J, et al. Prevalence of reduced kidney function and albuminuria in older adults: the Berlin initiative study. Nephrol Dial Transplant. 2017;32:997–1005.
- Tajbakhsh R, Joshaghani HR, Bayzayi F, et al. Association between pruritus and serum concentrations of parathormone, calcium and phosphorus in hemodialysis patients. Saudi J Kidney Dis Transpl. 2013;24(4):702–706.
- Thyroid Surgeons Committee SB, Chinese Medical Doctors Association. Expert consensus on surgical practice of hyperparathyroidism secondary to chronic renal failure. Chinese J Pract Surg. 2016;36:481–486.
- Nikodimopoulou M, Liakos S. Secondary hyperparathyroidism and target organs in chronic kidney disease. Hippokratia. 2011;15:33–38.
- Kim SM, Long J, Montez-Rath ME, et al. Rates and outcomes of parathyroidectomy for secondary hyperparathyroidism in the United States. CJASN. 2016;11(7):1260–1267.
- Weijing Bian GW, Yang L. An epidemiological analysis of secondary hyperparathyroidism in long-term hemodialysis patients. J China Japan Friendship Hosp. 2008;22:195–197.
- Zhao J, Qian L, Zu Y, et al. Efficacy of ablation therapy for secondary hyperparathyroidism by ultrasound guided percutaneous thermoablation. Ultrasound Med Biol. 2016;42(5):1058–1065.
- Hensley CP, Courtney CA. Management of a patient with chronic low back pain and multiple health conditions using a pain mechanisms-based classification approach. J Orthop Sports Phys Ther. 2014;44(6):403–c402.
- Liaveri PG, Dikeos D, Ilias I, et al. Quality of sleep in renal transplant recipients and patients on hemodialysis. J Psychosom Res. 2017;93:96–101.
- Xu Min XX, Wang X. Localization and the evaluation of reliability and validity of four item scale about pruritus. ChinJ Prac Nurs. 2015;31:1150–1153.
- Yue WW, Wang SR, Li XL, et al. Quality of life and cost-effectiveness of radiofrequency ablation versus open surgery for benign thyroid nodules: a retrospective cohort study. Sci Rep. 2016;6(1):37838.
- Sadideen HM, Taylor JD, Goldsmith DJ. Total parathyroidectomy without autotransplantation after renal transplantation for tertiary hyperparathyroidism: long-term follow-up. Int Urol Nephrol. 2012;44(1):275–281.
- Santos RO, Ohe MN, Carvalho AB, et al. Total parathyroidectomy with presternal intramuscular autotransplantation in renal patients: a prospective study of 66 patients. J Osteoporos. 2012;2012:631243.
- Zmijewski PV, Staloff JA, Wozniak MJ, et al. Mazzaglia PJ subtotal parathyroidectomy vs total parathyroidectomy with autotransplantation for secondary hyperparathyroidism in dialysis patients: short- and long-term outcomes. J Am Coll Surg. 2019;228(6):831–838.
- Hou J, Shan H, Zhang Y, et al. Network meta-analysis of surgical treatment for secondary hyperparathyroidism. Am J Otolaryngol. 2020;41(2):102370.
- Zhang L, Xing C, Shen C, et al. Diagnostic accuracy study of intraoperative and perioperative serum intact PTH level for successful parathyroidectomy in 501 secondary hyperparathyroidism patients. Sci Rep. 2016;6(1):26841.
- Chen L, Wang K, Yu S, et al. Long-term mortality after parathyroidectomy among chronic kidney disease patients with secondary hyperparathyroidism: a systematic review and meta-analysis. Ren Fail. 2016;38(7):1050–1058.
- Moldovan D, Racasan S, Kacso IM, et al. Survival after parathyroidectomy in chronic hemodialysis patients with severe secondary hyperparathyroidism. Int Urol Nephrol. 2015;47(11):1871–1877.
- Peng C, Zhang Z, Liu J, et al. Efficacy and safety of ultrasound-guided radiofrequency ablation of hyperplastic parathyroid gland for secondary hyperparathyroidism associated with chronic kidney disease. Head Neck. 2017;39(3):564–571.
- Shi Q, Sun Y, Tang S, et al. Ultrasound-guided percutaneous laser ablation for primary hyperparathyroidism. Oncoradiology. 2020;29(4):370–374.
- Ketteler M, Block GA, Evenepoel P, et al. Executive summary of the 2017 KDIGO chronic kidney disease-mineral and bone disorder (CKD-MBD) guideline update: what's changed and why it matters. Kidney Int. 2017;92(1):26–36.
- Cao Xiaojing H, Lili P. Clinical efficacy of microwave ablation in treatment of secondary hyperparathyroidism ineligible for surgical resection. Chin J Interv Imaging Ther. 2020;7:145–148
- Mingan Yu LZ, Lili P. Analysis of short-term efficacy of ultrasound-guided microwave ablation for secondary hyperparathyroidism. Chinese J Nephrol. 2015;31:303–304.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl (2011). 2017;7(1):1–59.
- Cozzolino M, Brancaccio D, Gallieni M, et al. Pathogenesis of parathyroid hyperplasia in renal failure. J Nephrol. 2005;18(1):5–8.
- Sherrard DJ, Hercz G, Pei Y, et al. The spectrum of bone disease in end-stage renal failure–an evolving disorder. Kidney Int. 1993;43(2):436–442.
- Malluche HH, Monier-Faugere MC. Monier-Faugere MC risk of a dynamic bone disease in dialyzed patients. Kidney Int Suppl. 1992;38:S62–S67.
- Schneider R, Slater EP, Karakas E, et al. Schlosser K initial parathyroid surgery in 606 patients with renal hyperparathyroidism. World J Surg. 2012;36(2):318–326.
- Conzo G, Perna AF, Sinisi AA, et al. Total parathyroidectomy without autotransplantation in the surgical treatment of secondary hyperparathyroidism of chronic kidney disease. J Endocrinol Invest. 2012;35(1):8–13.
- Danese MD, Kim J, Doan QV, et al. Chertow GM PTH and the risks for hip, vertebral, and pelvic fractures among patients on dialysis. Am J Kidney Dis. 2006;47(1):149–156.
- Gong L, Tang W, Lu J, et al. Thermal ablation versus parathyroidectomy for secondary hyperparathyroidism: a meta-analysis. Int J Surg. 2019;70:13–18.
