Abstract
Objective
To compare the safety and efficacy of high-intensity focused ultrasound (HIFU) followed by hysteroscopic resection for different placenta accreta spectrum disorders.
Materials and methods
Thirty-four patients with placenta accreta, placenta increta, or placenta percreta were treated with USgHIFU from January 2016 to December 2019 and were retrospectively reviewed. The patients were classified into three categories according to the relationship between the trophoblastic villi and the myometrium, based on magnetic resonance imaging (MRI). Fifteen patients were classified as placenta accreta, 17 patients were classified as placenta increta, and 2 were classified as placenta percreta. All patients completed follow-up. Treatment efficacy and safety were evaluated.
Results
No significant differences in baseline characteristics and results of HIFU ablation were observed between the patients with placenta accreta and those with placenta increta. The return of HCG levels to normal was longer in patients with placenta accreta compared with patients with placenta increta, while no significant difference was observed in the amount of intraoperative blood loss, the return of normal menstruation and the length of hospital stay.
Conclusions
HIFU treatment followed by hysteroscopic resection is safe and effective in the treatment of patients with placenta accreta and placenta increta.
Introduction
Placenta accreta spectrum disorder is a clinical condition that occurs when the placental villi grow deeply into the myometrium. It is one of the most dangerous obstetric complications which results in hemorrhage after delivery and this can result in multiorgan failure and even death [Citation1]. Based on the relationship between the placental villi and the myometrium, placenta accreta spectrum disorder is classified into three categories: (1) placenta accreta: the villi simply attach to the myometrium; (2) placenta increta: the villi invade into the myometrium; (3) placenta percreta: the villi invade the full thickness of the myometrium [Citation2]. The incidence of placenta accreta spectrum disorder has been increasing owing to the rising number of cesarean section deliveries and abortions. Several studies have shown that placenta accreta occurred in approximately 1 in 4000 deliveries in the 1970s [Citation3], 1 in 2500 deliveries in the 1980s [Citation4], and recently, 1 in 272 (0.37%) deliveries [Citation5]. In China, the incidence of placenta accreta was even higher than that in western countries because of the high cesarean section rate [Citation6].
The treatment of placenta accreta, placenta increta, and placenta percreta remains a major challenge. The invasion of chorionic villi into the myometrium will result in severe obstetric hemorrhage if a dilation and curettage (D&C) is performed, especially in those who have signs of marked blood flow between the myometrium and the retained placenta. Thus, the optimal treatment for placenta accreta, placenta increta, and placenta percreta remains uncertain [Citation7]. Recently, conservative treatments have been more widely used in the management of placenta accreta. Methotrexate (MTX) injection and/or oral mifepristone have been used for patients with placenta accreta before hysteroscopic resection, but the effectiveness is controversial [Citation7]. Another option for patients with placenta accreta is uterine artery embolization (UAE) followed by hysteroscopic resection; however, due to the severe complications, its use has been limited [Citation8]. As a non-invasive treatment, ultrasound-guided high-intensity focused ultrasound (USgHIFU) has been widely used in the treatment of benign uterine diseases [Citation9–11]. Recently, several groups have used this technique to treat placenta accreta and the results show that USgHIFU is safe for use in treating patients with placenta accreta [Citation12]. However, no study has compared the results of patients with placenta accreta, placenta increta and placenta percreta treated with USgHIFU. Therefore, the aim of this study was to compare the safety and efficacy of USgHIFU treatment for different placenta accreta spectrum disorders.
Materials and methods
The protocol for this retrospective study was approved by the Ethics Committee of the First Affiliated Hospital of Zunyi Medical University and the requirement for informed consent was waived
Patients
From January 2016 to December 2019, 34 patients with placenta accreta, placenta increta and placenta percreta, who were treated with USgHIFU, followed by hysteroscopic resection, were reviewed retrospectively. The diagnosis and classification of placenta accreta were confirmed by the history, clinical manifestations, ultrasonographic imaging and/or magnetic resonance imaging (MRI).
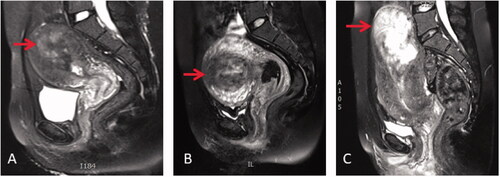
Inclusion criteria were as follows: (1) patients with placenta accreta, placenta increta or placenta percreta whose diagnosis was confirmed by ultrasound and MRI (); (2) patients with placenta accreta or placenta increta who wish to maintain fertility or preserve their uterus;(3) patients two weeks post vaginal delivery, cesarean section, induced labor or incomplete abortion; (4) no active vaginal bleeding or infection; (5) normal liver and renal function, and hemoglobin higher than 7.0 g/L. Exclusion criteria were as follows: (1) large surgical scar on the lower abdominal wall; (2) delivery complications; (3) acute pelvic infection.
Figure 1. T2 weighted MRI of patients with different placenta accreta spectrum disorders. (A) placenta accreta: the villi simply attach to the myometrium (red arrow); (B) placenta increta: the villi invade into the myometrium (red arrow); (C) placenta percreta: the villi invade the full thickness of the myometrium (red arrow).
USgHIFU ablation
USgHIFU treatment was performed using the Model-JC-200 focused ultrasound tumor therapeutic system (Chongqing Haifu Medical Technology Co., Ltd., Chongqing, China). Therapeutic ultrasound energy was produced by a mono-element transducer measuring 20 cm in diameter, with a focal length of 12 cm, and operating at a frequency of 1.0 MHz. The dimensions of focus were 5 mm × 3 mm (beam axis × transverse direction). An ultrasound imaging probe (My-Lab70, Esaote, Italy), situated in the center of the transducer was used to monitor the response of the residual placenta to HIFU during the procedure.
Each patient was asked to perform the following routine bowel preparation for 2 days prior to HIFU treatment: instructions were given to patients to ingest a semi-liquid diet on day 1 and liquid food on day 2, and then fast for 12 h before the USgHIFU procedure. On the morning of the treatment, an enema was given, and the skin was shaved, degreased, and degassed, from the level of the umbilicus to the upper margin of the pubic symphysis. A urinary catheter was inserted to release urine and/or filling the bladder with normal saline to control the bladder volume and improve the therapeutic acoustic pathway.
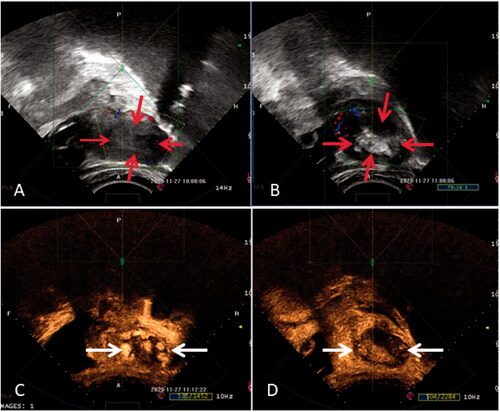
The patients were placed in a prone position on the HIFU table, and a degassed water balloon was placed between the anterior abdominal wall and the transducer to help compress and push the bowel out of the acoustic pathway. HIFU ablation was performed under conscious sedation (fentanyl at 1 mg/kg, midazolam hydrochloride at 0.02 mg/kg, repeated administration every 20 ∼ 30 min intervals if needed). The sagittal view of the ultrasound scanning mode was selected and a treatment plan was made by dividing the target region of the placenta into different slices each with a thickness of 5 mm. During the HIFU procedure, a sonication power of 300–400 W (acoustic power) was used. The exposure time for each sonication was 1 or 2 s. The sonication power or the exposure time was adjusted based on feedback from the patient and changed grayscale on ultrasonographic imaging (). For example, if the patients could not tolerate a sonication of 400 W for 2 s or if a significant grayscale change was observed, we could decrease the power or the exposure time. This process was repeated on a slice-by-slice basis. Once the entire targeted placenta had a hyperechoic appearance or the contrast-enhanced ultrasound showed no blood supply (), the treatment was terminated. During the procedure, the patients were required to report any discomfort and vital signs such as heart rate, blood pressure, respiration and oxygen saturation were monitored.
Figure 2. Ultrasound images obtained during HIFU treatment for placenta accreta. (A) pre-HIFU ultrasound image showed hypoechoic area in the uterus (read arrows); (B) post-HIFU utrasound image showed grey scale changes in the treated region (read arrows); (C) pre-HIFU contrast-enhanced ultrasound image showed perfusion in the placenta accreta (white arrows); (d) post-HIFU contrast ultrasound image showed no perfusion in the placental tissue (white arrows)
Hysteroscopic resection
Hysteroscopic resection of placental tissue was performed under general anesthesia. The patient was placed in a dorsal lithotomy position. After routine disinfection of the operative field, the depth of the uterus was measured. Next, a cervical dilator was used to dilate the cervix to 10 mm, and a 30° diagnostic hysteroscope (Olympus 9.0 mm) was used to visualize the uterine cavity and to locate the site of the placental tissue. Then, hysteroscopic resection was performed to remove the implanted placental tissue. During the procedure, normal saline was used to expand the uterine cavity. All removed placental tissues were sent for pathological examination.
Statistical analysis
SPSS 20.0 software (SPSS, Inc., Chicago, IL, USA) was used for statistical analysis. Normally distributed data were depicted as mean ± standard deviation, and skew distribution data were depicted as median and interquartile range, Chi-square test and Mann–Whitney U test were used to compare the data between the two groups.
Results
Baseline characteristics
Based on MRI, 15 patients were classified as placenta accreta, 17 were classified as placenta increta, and 2 patients were classified as placenta percreta. Since the number of patients with placenta percreta was minimal, they were not included in the statistical analysis. Of these patients, 16 had a vaginal delivery, 4 had a cesarean section delivery, 5 had a miscarriage, and 7 had an abortion.
As shown in , the average age was 29.8 ± 6.2 in the group of patients with placenta accreta, while it was 30.2 ± 4.6in the group of patients with placenta increta. The median BMI was 25.4 in the group of patients with placenta accreta, and it was 23.5 in the group of patients with placenta increta. The median number of previous pregnancies was 4 in the group of patients with placenta accreta and 3 in the group of patients with placenta increta. The median number of previous deliveries was 2 in patients with placenta accreta and placenta increta. The level of β-HCG before HIFU was 109.6 U/L in the group of patients with placenta accreta, and it was 172.1 U/L in patients with placenta increta. The median residual placental volume was 93.6 cm3 in the group of patients with placenta accreta, while it was 112.7 cm3 in the group of patients with placenta increta. No significant difference was observed in age, BMI, history of previous pregnancy, nor the number of previous deliveries between the two groups.
Table 1. Comparison of baseline characteristics of patients with placenta accrete and patients with placenta increta.
Assessment of HIFU ablation
All patients completed HIFU treatment in one session. As shown in , grayscale change was observed in real-time ultrasound monitoring images and a non-perfused area was observed in contrast-enhanced ultrasound after HIFU (). The median interval between post-pregnancy and HIFU treatment was 16.8 ± 2.96 days in the group of patients with placenta accreta, and it was 11.71 ± 1.59 days in the group of patients with placenta increta. The median HIFU treatment time was 50 min (interquartile range: 24–71) and the median sonication time was 400 s (interquartile range: 300–730) in the group of patients with placenta accreta, while they were 69 min (interquartile range: 49–85) and 655 s (interquartile range: 450–950) in the group of patients with placenta increta. The median HIFU treatment energy was 160 (interquartile range: 117–292) KJ in the group of patients with placenta accreta, while it was 262 (interquartile range: 180–380) KJ in the group of patients with placenta increta. The median non-perfused volume (NPV) ratio, which was defined as NPV divided by the placenta volume immediately after HIFU treatment, was 87% in the group of patients with placenta accreta, while it was 90% in the group of patients with placenta increta. No significant difference was observed in the interval between post-pregnancy and HIFU, HIFU treatment time, acoustic energy generated during treatment, sonication time, and NPV ratio between the two groups ().
Table 2. Comparison of HIFU ablation results of placenta accreta and placenta increta.
During HIFU treatment, all patients complained of mild lower abdominal or sacrococcygeal pain; the pain score ranged from 1 to 4 points on a 0–10 point scale. After HIFU treatment, 26 patients experienced mild pain on the day of the treatment with a pain scale from 1 to 2 points, while the remaining 8 patients experienced pain with a pain scale from 3 to 4 points. One patient had deep second-degree skin burns. The burned tissue was removed by surgical resection one day after HIFU treatment. No other serious complications were observed in these patients after HIFU treatment.
Evaluation of hysteroscopic procedure
The patients underwent the hysteroscopic procedure after a median of 4–5 days post HIFU treatment. The non-implanted portion of the placenta was removed, while the deeply implanted placenta was left in situ. No serious surgical complications, such as severe sepsis, gas embolism, nor uterine perforation occurred. No significant difference was found between the two groups in intraoperative blood loss and hospital stay. No patient received a blood transfusion, and no uterine perforation occurred in any of the patients in this study ().
Table 3. Comparison of hysteroscopic treatment results of placenta accreta and placenta increta.
Follow-up results
As shown in , no significant difference was observed in-hospital stay, duration of vaginal bleeding, and normal menstruation return between the two groups of patients. The average hospital stay was 16.8 ± 3.0 days in the group of patients with placenta accreta, and 11.71 ± 1.1 days in the group of patients with placenta increta. The median duration of a small amount of vaginal bleeding was 16 days (range: 10–30 days) in the group of patients with placenta accreta, and it was 10 days (range: 7–18 days) in the group of patients with placenta increta. The median for return to normal menstruation after the hysteroscopic resection was 2 months in both patients with placenta accreta and patients with increta. The median time for HCG to return to normal levels was 10 days in the group of patients with placenta accreta, while it was 5 days in the group of patients with placenta increta (p < 0.05). During the follow-up period, no hemorrhage, infection, or other complications occurred. Three patients with placenta accreta had a pregnancy within 2 years after the hysteroscopic procedure, two had an abortion for personal reasons, and the other delivered a healthy baby at term. One patient with placenta increta delivered a healthy baby during the follow-up.
Table 4. Comparison of follow-up results of patients with placenta accreta and placenta increta.
Discussion
Forcibly removing an invasive placenta increases the risks of massive obstetric hemorrhage. The goal of HIFU treatment in the management of placenta accreta is to reduce the risk of severe hemorrhage during D&C [Citation13]. Several studies with a small number of subjects have demonstrated the efficiency and safety of HIFU treatment for placenta accreta after vaginal delivery [Citation14–18]. The results from these studies showed that the blood supply of the residual placental tissue either significantly decreased or disappeared after HIFU (). The treated residual placental tissue was removed hysteroscopically, followed by D&C. The uterus was preserved, and menstruation returned to normal.
Among the 34 patients we treated, 15 had placenta accreta, 17 had placenta increta, and 2 had placenta percreta. In our study, we did not find any significant differences in baseline characteristics between the patients with placenta accreta and the patients with placenta increta (). In this study, only one patient had deep second-degree skin burns, but no other serious complications were encountered in the patients with placenta accreta or placenta increta. The deep second-degree skin burns occurred in a patient with a prior abdominal surgical scar. Less blood supply for scar tissue and skin sensory loss increased the risk of skin burns. This incidence can be decreased by often checking the skin during HIFU; moving down the transducer in the water tank to let the cold degassed water in contact with skin. Thus, HIFU treatment is safe for the management of placenta accreta and placenta increta.
Our results showed that placenta accreta and placenta increta were sensitive to HIFU treatment. In this study, we found the sonication time was similar to a previous study [Citation17]. We further compared the treatment results and found that there was no significant difference in treatment time, sonication time, the acoustic energy used, and the NPV ratio between placenta accreta and placenta increta. Our results indicated that both placenta accreta and placenta increta are suitable for HIFU ablation. We noted that the median acoustic energy used for placenta increta was 262 KJ, while it was just 160 for placenta accreta. Can this phenomenon be explained by the placenta increta being more vascular than that of placenta accreta? It is needed to enroll more patients to validate this result in the future.
An earlier study showed that, in some cases, approximately 7 days after HIFU treatment, necrotic placental tissue could be delivered spontaneously [Citation15]. Therefore, some physicians proposed that D&C after HIFU is not mandatory. However, the treated residual placenta remains in the uterus and may increase the risk of hemorrhage or infection. In this regard, patients may experience severe emotional distress. Thus, HIFU, followed by hysteroscopic resection, was performed to remove retained placental tissue and prevent further complications [Citation14,Citation17].
In this study, 13 patients with placenta accreta and 8 with placenta increta underwent hysteroscopic resection after HIFU, while 2 patients with placenta accreta and 9 with placenta increta refused any additional treatment, for personal reasons. It is noted that the longer the interval between HIFU and hysteroscopic resection, the stronger the uterine wall becomes and there is a decrease in the blood supply of the placental tissue. However, with the longer interval between HIFU treatment and hysteroscopic surgery, the patients may potentially have a higher infection risk and associated emotional distress. In this study, we performed hysteroscopic resection around 4 days after HIFU. The median intraoperative blood loss was 70 ml in the group of patients with placenta accreta and 50 ml in the group of patients with placenta increta. The blood loss volume was much less than that of patients treated with hysteroscopic and laparoscopic resection alone[Citation19]. No uterine perforation or heavy hemorrhage was observed in either patient with placenta accreta or patients with placenta increta. The patients who were treated with HIFU and hysteroscopic resection or with HIFU alone completed follow-up. The follow-up results showed no significant difference in-hospital stay, vaginal bleeding time, normalization of menstruation, and changes in HCG levels. Our results indicated that HIFU followed by hysteroscopic resection around 4 days after HIFU is safe and effective for patients with placenta accreta and patients with placenta increta.
This study is limited because of the small number of subjects and because it is a retrospective study; several factors may cause a bias in the results. In this study, all patients had hysteroscopic resection around 4 days following HIFU. We did not have the results of patients who had hysteroscopic resection at different time points after HIFU. Therefore, a prospective study with a larger number of patients is needed to validate the findings. At the same time, we need to explore the best time for hysteroscopic resection following HIFU. Conclusions need to be reached regarding how long to wait between HIFU treatment and hysteroscopic resection. This then needs to be compared to the number of spontaneous deliveries of placental tissue following HIFU treatment in patients within different types on the placenta accreta spectrum, so as to reduce the risk of adverse effects caused by the procedure. This study is also limited because there was no control group for HIFU. Therefore, a further prospective study with a control group to assess if HIFU is better than other treatment modalities is needed.
Conclusion
Based on the results of this study, HIFU combined with hysteroscopic resection is safe and effective in the management of placenta accreta and placenta increta. Future studies with a larger number of subjects are needed to validate the findings and further investigate the optimal interval between HIFU and hysteroscopic resection.
Disclosure statement
Lian Zhang is a senior consultant to Chongqing Haifu Medical Technology Co., Ltd. The other authors have no conflict of interest to declare.
Additional information
Funding
References
- Silver R, Barbour K. Placenta accreta spectrum: accreta, increta, and percreta. Obstet Gynecol Clin North Am. 2015;42(2):381–402.
- Jauniaux E, Collins S, Burton GJ. Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am J Obstet Gynecol. 2018;218(1):75–87.
- Read J, Cotton D, Miller F. Placenta accreta: changing clinical aspects and outcome. Obstet Gynecol. 1980;56(1):31–34.
- Miller D, Chollet J, Goodwin T. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997;177(1):210–214.
- Mogos MF, Salemi JL, Ashley M, et al. Recent trends in placenta accreta in the United States and its impact on maternal-fetal morbidity and healthcare-associated costs, 1998-2011. Int Society of Perinatal Obstet. 2016;29:1077–1082.
- Zhang H, Dou R, Yang H, et al. Maternal and neonatal outcomes of placenta increta and percreta from a multicenter study in China. J Maternal-Fetal Neonatl Med. 2019;32(16):2622–2627.
- Sentilhes L, Kayem G, Chandraharan E, et al. FIGO consensus guidelines on placenta accreta spectrum disorders: conservative management. Int J Gynaecol Obstet. 2018;140(3):291–298.
- Diop AN, Chabrot P, Bertrand A, et al. Placenta accreta: management with uterine artery embolization in 17 cases. J Vasc Interv Radiolo. 2010;21(5):644–648.
- Zhang L, Zhang W, Orsi F, et al. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: a review of safety and efficacy. International journal of hyperthermia: the official journal of European Society for Hyperthermic Oncology. Int J Hyperthermia. 2015;31(3):280–284.
- Shui L, Mao S, Wu Q, et al. High-intensity focused ultrasound (HIFU) for adenomyosis: two-year follow-up results. Ultrason Sonochem. 2015;27:677–681.
- Zhu X, Deng X, Wan Y, et al. High-intensity focused ultrasound combined with suction curettage for the treatment of cesarean scar pregnancy. Medicine. 2015;94(18):e854.
- Zhang L, Chen W-Z, Liu Y-J, et al. Feasibility of magnetic resonance imaging-guided high intensity focused ultrasound therapy for ablating uterine fibroids in patients with bowel lies anterior to uterus. Eur J Radiol. 2010;73(2):396–403.
- Shaw C, ter Haar G, Rivens I, et al. Pathophysiological mechanisms of high-intensity focused ultrasound-mediated vascular occlusion and relevance to non-invasive fetal surgery. J R Soc Interface. 2014;11(95):20140029.
- Jiang J, Wang C, Xue M. High-intensity focused ultrasound versus uterine artery embolization for patients with retained placenta accreta. Eur J Obstet Gynecol Reprod Biol. 2020;252:82–86.
- Bai Y, Luo X, Li Q, et al. High-intensity focused ultrasound treatment of placenta accreta after vaginal delivery: a preliminary study. Ultrasound Obstet Gynecol. 2016;47(4):492–498.
- Lee J, Hong G, Park B, et al. High-intensity focused ultrasound combined with hysteroscopic resection to treat retained placenta accreta. Obstet Gynecol Sci. 2016;59(5):421–425.
- Ye M, Yin Z, Xue M, et al. High-intensity focused ultrasound combined with hysteroscopic resection for the treatment of placenta accreta. BJOG. 2017;124:71–77.
- Jiang X, Tang QLan, Yang B, et al. High-intensity focused ultrasound combined procedures treatment of retained placenta accreta with marked vascularity after abortion or delivery. International journal of hyperthermia: the official journal of European Society for Hyperthermic Oncology. North Am Hyperthermia Group. 2019;36(1):420–427.
- Legendre G, Zoulovits F, Kinn J, et al. Conservative management of placenta accreta: hysteroscopic resection of retained tissues. J Minim Invasive Gynecol. 2014;21(5):910–913.
