Abstract
Objective
To evaluate the clinical outcomes of transvaginal ultrasound-guided (US-guided) radiofrequency ablation (RFA) combined with mifepristone for the treatment of large uterine fibroids.
Methods
Between June 2016 and December 2018, a total of 30 patients with symptomatic uterine fibroids (≥5cm) who underwent transvaginal US-guided RFA combined with mifepristone were included in this retrospective study. A matching cohort of 30 patients underwent transvaginal US-guided RFA without mifepristone as controls. The technical efficacy, complications and mid-term treatment effectiveness were assessed and compared with the controls.
Results
The mean volume of uterine fibroid was 168.3 ± 40.1 cm3. The mean ablation time was 23.5 ± 11.3 min in the combined treatment group, which was demonstrably less than that of the RFA group, which was 45.7 ± 6.8 min. The mean number of punctures was 2.2 ± 0.6 in the combined treatment group, which was significantly less than that of the RFA group. No major complications occurred. The mean percentages of regression of fibroid at 3 and 12 months after the course of the combined treatment were 73.3% and 90.1%, respectively, which were significantly more than those of the RFA group. Quality of life and symptom scores improved in both groups but to a greater extent in the combined treatment group.
Conclusions
US-guided RFA combined with mifepristone might be a simple, safe and effective alternative for the treatment of large uterine fibroids.
Introduction
Uterine fibroids are a common benign gynecological condition. Approximately, 50% of uterine fibroids cause symptoms that warrant therapy. Symptoms include abnormal uterine bleeding, heavy menstrual bleeding, bulk symptoms and other complications [Citation1]. In recent years, ultrasound-guided (US-guided) radiofrequency ablation (RFA) has been the focus of interest as a minimally invasive strategy for patients with symptomatic uterine fibroids. Previous studies have reported that RFA can provide symptomatic relief and significant improvement in the quality of life [Citation2–10]. However, optimal patients might be those with small fibroids (diameter <5 cm or volume < 180 cm3) [Citation2–5]. For larger fibroids, RFA may not be effective, and the risk of complications may also increase [Citation2–5].
Mifepristone is a synthetic steroid with both anti-progesterone and anti-glucocorticoid activities. Mifepristone can effectively reduce the uterine fibroid volume, however, its effect is transient, and it is unsuitable for long-term use [Citation11–14].
The aim of this study was to evaluate the feasibility, safety and outcomes of transvaginal US-guided RFA combined with mifepristone for the treatment of large, symptomatic uterine fibroids.
Materials and methods
Participants
This retrospective study was approved by the institutional review board of the Chinese PLA Rocket Force General Hospital, and all enrolled patients signed informed consent forms for the treatment and for any future use of the data collected.
Between June 2016 and December 2018, 517 premenopausal women with symptomatic uterine fibroids were treated with transvaginal US-guided RFA at our institution. A cohort of 30 patients who underwent transvaginal US-guided RFA combined with mifepristone was enrolled in the study. A separate cohort of 30 women who only underwent RFA served as controls. These patients were matched for initial fibroid diameter and type before the treatment. The two groups of patients met the following inclusion criteria: (1) symptomatic uterine fibroid, diagnosed by biopsy pathology; (2) single uterine fibroid ≥ 5 cm; (3)no desire for future childbirth; (4) declined to undergo surgery; (5) normal liver and kidney functions; (6) normal coagulation function and (7) normal ThinPrep cytology test results.
The exclusion criteria included pregnancy or lactation, suspected pelvic inflammatory disease, suspected malignancy, other treatment for uterine fibroids within the 3 months before the study or any contra-indication to mifepristone itself as hypersensitivity, severe renal or hepatic disorders.
Mifepristone treatment
Patients underwent three months of daily therapy with oral mifepristone (at a dose of 2.5 mg).Blood samples were taken for hepatic function at the initial consult and every month into treatment. It was decided beforehand that any subject presenting alterations in transaminases 3 times or more above their normal maximum limit, in line with FDA recommendations [Citation15], would be excluded from the treatment.
US-guided RFA procedure
In the combined treatment, RFA was performed one month after the withdrawal of mifepristone. The radiofrequency generator used in this study (Ban Bian Tian Medical Apparatus and Instruments Company, Xi An City, China) was operated at 50 Hz with a transmitting power of 300 W. The radiofrequency electrode used (Ban Bian Tian Medical Apparatus and Instruments Company) was 35 cm long with a 1.5 cm exposed distal tip. The output energy was set at 30–50 W.A. The procedure was performed under intravenous conscious sedation. Patients were placed in the lithotomy position. In all the cases, a biopsy of the lesion was performed with an 18-gauge core needle for pathological diagnosis before ablation. A radiofrequency electrode was introduced transvaginally under transabdominal ultrasound guidance. The electrode was penetrated through the endometrium and was inserted into the lesion. Once the hyperechogenic signal covered nearly 80–90% of the entire lesion on real-time ultrasound, the ablation was discontinued [Citation16]. Absence of vascularization was confirmed at the end by contrast-enhanced ultrasound. All patients received oral antibiotic prophylaxis for 3 d after the treatment. The doctors who performed RFA were blinded to mifepristone use.
Follow-up assessment
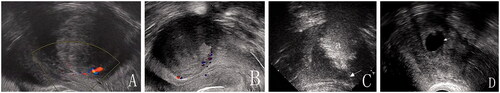
Ultrasound was performed immediately before treatment (baseline), prior to RFA and at 3 and 12 months after RFA (). The uterine fibroid volume was evaluated by ultrasound and calculated using the following formula: 0.5233 × superoinferior diameter × anteroposterior diameter × transversal diameter. The doctors who performed the imaging data acquisition and entry were blinded against all clinical data.
Figure 1. (A) Transvaginal sonographic image before treatment. (B) Three months after mifepristone treatment. The fibroid volume reduction is 45%; (C) RFA procedure (a = hyperechogenic zone arrow = electrode); (D) Twelve months after the procedure. (Arrow = the secondary cystic changes); The fibroid volume reduction is 85%.
All patients underwent a thorough clinical evaluation that included the uterine fibroid symptom and health-related quality of life questionnaire (UFS-HRQoL). This instrument includes a symptom severity score (SSS) and a HRQoL score [Citation17].
Statistical analysis
Statistical analysis was performed using SPSS for Windows version 26.0 (SPSS Inc., Chicago, IL). Means were compared by t-tests, and proportions were compared by chi-square or Fisher’s exact tests. Paired t-tests were used to analyze changes in each score from baseline. A value of p < .05 was considered statistically significant.
Results
Baseline characteristics
The average age of the patients was 37.7 ± 5.0 years (range, 32–50 years), and the mean volume of uterine fibroid was 168.3 ± 40.1 cm3 (range, 67.5–286.7 cm3). The baseline characteristics of the two groups are given in , which shows no significant differences in the baseline data between the study group and the control group.
Table 1. Baseline information.
Post-procedural evaluation of combined treatment
RFA combined with mifepristone was successfully performed for all 30 patients in this group. The mean percentage reduction of fibroids was 41.6% after mifepristone treatment. In the patients who presented with anemia before treatment, the hemoglobin levels were significantly increased from 8.4 ± 1.5 to 11.1 ± 2.1 g/L after 3 months of mifepristone treatment.
The mean ablation time was 23.5 ± 11.3 min (range, 15–32 min). The mean number of punctures was 2.2 ± 0.6 (range, 1–3). The mean percentage reduction of fibroid was 73.3% and 90.1% at 3 and 12 months post-ablation, respectively. The SSS was reduced at 12 months post-ablation, from a mean of 32.5 ± 5.1 to 6.7 ± 5. The UFS-QoL HRQoL score improved at 12 months post-ablation, from a mean of 53.1 ± 12.6 to 89.4 ± 7.1.
Comparison of the results of combined treatment vs. RFA
The single RFA procedure was successfully performed for all 30 patients in this group. The mean ablation time was 45.7 ± 6.8 min (range, 32–47 min), which was demonstrably longer than that of the combined treatment group. The mean number of punctures was 3.7 ± 0.6 (range, 2–5), which was significantly more than that of the combined treatment group. The mean percentages of fibroid regression at 3 and 12 months after the course of treatment were 48.9% and 72.5%, respectively, which was significantly less than that of the combined treatment group. The improvement in the SSS was significantly better after the combined treatment than after RFA. The improvement in HRQoL scores was better after the combined treatment than after RFA, but the difference was not significant (p > .05) ().
Table 2. Comparison of results between combined treatment and single RFA.
Safety
Upon termination of mifepristone treatment, all the subjects were amenorrheic. Five women complained of fatigue; however, side effects, such as nausea, vomiting, rash and fever from mifepristone were not reported by any of the 30 women. There were no major complications in either group. The common minor complications after RFA were abdominal pain, vaginal discharge and low-grade fever (<38 °C), which were self-limited. They were classified as grade A or B according to the unified standardized Society of Interventional Radiology (SIR) grading system. Five patients complained of abdominal pain in the study group after ablation. In contrast, 12 patients presented with abdominal pain in the control group. Four cases of low-grade fever were observed in the study group after ablation. In contrast, ten cases of low-grade fever were observed in the control group. Eleven patients in the study group and fifteen in the control group presented with vaginal discharge after ablation (). No symptoms lasted more than 2 weeks. All patients had a menstrual cycle in the month following RFA.
Table 3. Complications after procedure.
Discussion
This study showed promising results of the combined transvaginal US-guided RFA and mifepristone protocol in terms of lesion volume reduction and symptom improvement for large uterine fibroid (>5 cm) treatment. The mean reduction in fibroid volume was 41% at the end of 3 months with a 25 mg dose of mifepristone, which is comparable to previous studies [Citation11–14]. In previous studies, the one-year uterine volume reduction rate of RFA ranged from 60% to 90% [Citation2–10]. Our results are within the previously reported ranges. However, it is difficult to compare the present results with previous studies due to differences in the characteristics of uterine fibroids and the types of electrodes. The RF device in this study used a monopolar electrode. There are various types of electrodes, and the type of electrode used clearly influences the extent of ablation [Citation18].
The mean lesion volume decreased by 91% at one year after combined treatment, which was greater than the corresponding values for the RFA group. In this study, scores assessed by the UFS-QoL questionnaire showed a significant improvement in both groups at the 12-month follow-up compared with baseline. Combined treatment was more effective than RFA treatment on its own. Based on the above comparisons, we speculate that combined treatment may provide a superior clinical effect compared to single RFA.
The results of our study demonstrate that mifepristone provides pre-ablation benefits in the short term. The pre-ablation use of mifepristone made RFA simpler in terms of a reduced number of punctures and ablation time. The primary reason for these differences in results was likely related to the fact that mifepristone diminished the volume of uterine fibroids. In addition, mifepristone could decrease blood flow to the uterus so that the cooling effect of blood flow during ablation is reduced [Citation14]. RFA destroys lesion by the heat generated from a high-frequency alternating current. As temperatures rise, increasing impedance limits further deposition of electricity into the tissue. This becomes even more pronounced if charring occurs. Therefore, small lesions where a single ablation is sufficient to cover the whole lesion while multiple overlapping ablations need to be planned to cover oversize lesions through a series of single probe ablations [Citation19].
No major complications were observed in the present groups of patients. The incidence of post-ablation abdominal pain and low-grade fever was significantly greater in the single RFA group than in the combined treatment group. The possible reasons for this difference were that the number of punctures and ablation time of the combined treatment group were demonstrably less than that of the RFA group. Five women in the combined treatment group complained of fatigue, which was one of the side effects of mifepristone. Future research should focus on cost-effectiveness and distinguish between groups of women with uterine fibroids who would most benefit.
This study presents several inherent limitations. First, we could not evaluate the true benefit of mifepristone prior to RFA because we could not perform a prospective randomized controlled study. In addition, for the purposes of this pivotal trial, uterine fibroids with a maximum diameter of 8.5 cm were selected. It is possible that even larger lesions (>10 cm) could be treated with multiple ablations [Citation20]. However, whether the application of mifepristone could diminish the sections of RFA for lesions (>10 cm) is unknown. Another limitation of the study was the use of ultrasound in the evaluation of the number, size, and morphological appearance of the fibroids, which is known to be an observer-dependent technique [Citation21]. Nevertheless, the efficiency of ultrasound compared with magnetic resonance imaging seems to be a sufficient technique when used with 1–4 fibroids [Citation22].
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Baird DD, Dunson DB, Hill MC, Cousins D, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188(1):100–107.
- Rey VE, Labrador R, Falcon M, et al. Transvaginal radiofrequency ablation of myomas: technique, outcomes, and complications. J Laparoendosc Adv Surg Tech A. 2019;29(1):24–28.
- Iversen H, Dueholm M. Radiofrequency thermal ablation for uterine myomas: long-term clinical outcomes and reinterventions. J Minim Invasive Gynecol. 2017;24(6):1020–1028.
- Yin G, Chen M, Yang S, et al. Treatment of uterine myomas by radiofrequency thermal ablation: a 10-year retrospective cohort study. Reprod Sci. 2015;22(5):609–614.
- Garza-Leal JG. Long-term clinical outcomes of transcervical radiofrequency ablation of uterine fibroids: the VITALITY study. J Gynecol Surg. 2019;35(1):19–23.
- Brölmann H, Bongers M, Garza-Leal JG, et al. The FAST-EU trial: 12-month clinical outcomes of women after intrauterine sonography-guided transcervical radiofrequency ablation of uterine fibroids. Gynecol Surg. 2016;13(1):27–35.
- Carrafiello G, Recaldini C, Fontana F, et al. Ultrasound-guided radiofrequency thermal ablation of uterine fibroids: medium-term follow-up. Cardiovasc Intervent Radiol. 2010;33(1):113–119.
- Cho HH, Kim JH, Kim MR. Transvaginal radiofrequency thermal ablation: a day-care approach to symptomatic uterine myomas. Aust N Z J Obstet Gynaecol. 2008;48(3):296–301.
- Jiang X, Thapa A, Lu J, et al. Ultrasound-guided transvaginal radiofrequency myolysis for symptomatic uterine myomas. Eur J Obstet Gynecol Reprod Biol. 2014;177:38–43.
- Kim CH, Kim SR, Lee HA, et al. Transvaginal ultrasound-guided radiofrequency myolysis for uterine myomas. Hum Reprod. 2011;26(3):559–563.
- Kettel LM, Murphy AA, Morales AJ, et al. Clinical efficacy of the antiprogesterone RU486 in the treatment of endometriosis and uterine fibroids. Hum Reprod. 1994;9(1):116–120.
- Shen Q, Hua Y, Jiang W, et al. Effects of mifepristone on uterine leiomyoma in premenopausal women: a meta-analysis. Fertil Steril. 2013;100(6):1722.
- Murji A, Whitaker L, Chow TL, et al. Selective progesterone receptor modulators (SPRMs) for uterine fibroids. Cochrane Database Syst Rev. 2017; 4(4):CD010770.
- Reinsch RC, Murphy AA, Morales AJ, et al. The effects of RU 486 and leuprolide acetate on uterine artery blood flow in the fibroid uterus: a prospective, randomized study. Am J Obstet Gynecol. 1994;170(6):1623–1627.
- Guidance for Industry. Drug-induced liver injury: premarketting clinical evaluation. Washington (DC): US Department of Health and Human Services; 2009.
- Hai N, Hou Q, Ding X, et al. Ultrasound-guided transcervical radiofrequency ablation for symptomatic uterine adenomyosis. Br J Radiol. 2017;90(1069):20160119.
- Spies JB, Coyne K, Guaou Guaou N, et al. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol. 2002;99(2):290–300.
- Lee BB, Yu SP. Radiofrequency ablation of uterine fibroids: a review. Curr Obstet Gynecol Rep. 2016;5(4):318–324.
- Goldberg SN. Radiofrequency tumor ablation: principles and techniques. Eur J Ultrasound. 2001;13(2):129–147.
- Liu H, Zhang J, Han ZY, et al. Effectiveness of ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroids: a multicentre study in China. Int J Hyperthermia. 2016;32(8):876–880.
- Moshesh M, Peddada SD, Cooper T, et al. Intraobserver variability in fibroid size measurements: estimated effects on assessing fibroid growth. J Ultrasound Med. 2014;33(7):1217–1224.
- Dueholm M, Lundorf E, Hansen ES, et al. Accuracy of magnetic resonance imaging and transvaginal ultrasonography in the diagnosis, mapping, and measurement of uterine myomas. Am J Obstet Gynecol. 2002;186(3):409–415.
