Abstract
Objective
To compare the re-intervention rates of myomectomy, uterine artery embolization (UAE) and magnetic resonance-guided focused ultrasound surgery (MRgFUS) for uterine fibroids (UFs) in different follow-up time.
Methods
Two investigators searched PubMed for clinical studies published in English from 1 Jan 2000 to 31 Dec 2020, and independently examined the paper to select qualified studies, extracted relevant information and assessed the risk of bias. Meanwhile, a meta-analysis of 31 studies containing totally 42103 patients was conducted to compare the re-intervention rate of myomectomy, UAE and MRgFUS.
Results
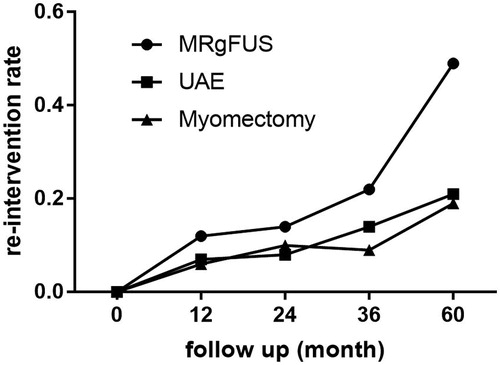
In the meta-analysis of 42103 patients, the 12-month re-intervention rates of myomectomy, UAE and MRgFUS for UFs were 0.06 (95%CI, 0.01–0.11), 0.07 (95%CI, 0.06–0.09), and 0.12 (95%CI, 0.04–0.20) respectively. The 24-month re-intervention rates were 0.10 (95%CI, 0.04–0.16), 0.08 (95%CI, 0.01–0.17), and 0.14 (95%CI, 0.07–0.21) respectively. The 36-month re-intervention rates were 0.09 (95%CI, 0.05–0.13), 0.14 (95%CI, 0.05–0.23), and 0.22 (95%CI, 0.11–0.32) respectively. Additionally, the 60-month re-intervention rates were 0.19 (95%CI, 0.15–0.24), 0.21 (95%CI, 0.17–0.25), and 0.49 (95%CI, 0.21–0.77) respectively.
Conclusions
The myomectomy has the lowest re-intervention rate of the three regimens in short time and long time while the MRgFUS has the highest. The rate of MRgFUS increased rapidly in the 60th month after the treatment.
1. Introduction
Uterine fibroids (UFs) are considered as the most common benign uterine tumors in women of childbearing age, and a large number of women with UFs are probably to schedule a uterus-conserving treatment [Citation1]. The patients who wish to preserve the uterus had the options of myomectomy, uterine artery embolization (UAE) and magnetic resonance-guided focused ultrasound (MRgFUS) [Citation2]. Although there was a large body of literature on the efficacy of various uterine-sparing interventions, the outcome still remained controversial [Citation3]. For example, the lowest 24-month re-intervention rate of myomectomy was reported by Michal Mara et al. as 3% and the highest was reported by S Subramanian et al. as 17% [Citation4,Citation5]. Therefore, it was of great significance to evaluate the short-time and long-time efficacy of the different regimens.
Disease status after uterine-sparing treatment is a crucial factor for clinical management of UFs, and the re-intervention risk of each option should be evaluated in different endpoints [Citation1]. For example, the 12-month re-intervention rate of UAE was reported by Matthew R Davis et al. as 7% and the 36-month re-intervention rate was reported by Scott C Goodwin et al. as 14% [Citation6,Citation7]. However, the longitudinal data of the common uterine-sparing regimens still remained fragmentary [Citation8]. As a result, we conducted this meta-analysis to 1) compare the re-intervention rate between myomectomy, UAE and MRgFUS groups and 2) estimate a clinically meaningful re-intervention rate for UFs in different follow-up time.
2. Methods
2.1. Search strategy
PubMed, Embase and Cochrane databases were systematically searched for relevant published articles with the following terms: (uterine fibroids OR fibroids OR UFs OR leiomyoma OR myoma) and (uterine artery embolization OR UAE OR magnetic resonance-guided focused ultrasound OR MRgFUS OR High-Intensity Focused Ultrasound OR HIFU OR myomectomy). The date were from 1 Jan 2000 to 31 Dec 2020. In addition, the search was restricted to human subjects and English-language studies.
2.2. Eligibility criteria
Inclusion criteria were as follows: (1) The study participants were human beings. (2) Original research papers with 30 or more patients were written in English. (3) Studies provide sufficient data on uterine-sparing treatment, and re-intervention. The re-intervention was defined as all additional treatment necessary during the follow-up period to control persistent or recurrent fibroid-related symptoms (such as hysterectomy, myomectomy and endometrial ablation) [Citation9]. (4) Studies with randomized controlled trials (RCTs), prospective or retrospective design. (5) Studies published between 1 Jan 2000 and 31 Dec 2020. (6) The patients underwent initial myomectomy, UAE or MRgFUS. (7) A follow-up period of 12, 24, 36 and (or) 60 months were required after treatment.
The studies were excluded according to the following criteria: (1) Abstracts, case reports, case series, meeting summaries, comments, letters, reviews or studies not related to human subjects. (2) Repeated studies including the same patients. (3) Insufficient sample size of less than 30 patients. (4) Studies with a lack of relevant outcome data and (5) Studies published before 1 Jan 2000 or after 31 Dec 2020.
2.3. Data extraction and quality assessment
Two investigators (Fan Xu and Lihong Deng) independently extracted the data from the studies. All data were confirmed by internal consistency, and disagreements were resolved by discussion between the two investigators. The present study was approved by the Ethics Committee of Nanchong Central Hospital, the Second Clinical Medical College, North Sichuan Medical University. The current meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (known as PRISMA) statement [Citation10]. The Newcastle-Ottawa Scale (NOS) was employed to evaluate the study quality. Each study considered to be a suitable candidate for inclusion in the meta-analysis was awarded a ‘star’. A high-quality study was defined as a study with five or more stars in total.
2.4. Statistical analysis
All data were analyzed using STATA software version 12.0 (StataCorp, College Station, TX), with p < 0.05 being considered to be statistically significant. In the meta-analysis, the unit of analysis was the re-intervention rate of myomectomy, UAE or MRgFUS. Heterogeneity was assessed using the chi-square test and I2 statistic. Heterogeneity was defined as a p value less than 0.10 or I2 greater than 50%. A fixed-effects model was suitable for data with no or low heterogeneity (I2<50%). Otherwise, a randomeffects model was used. Publication bias was assessed with Egger's test. Sensitivity analysis was performed in order to identify the influence of an individual study on pooled estimates by removing one study at a time.
3. Results
3.1. Literature search
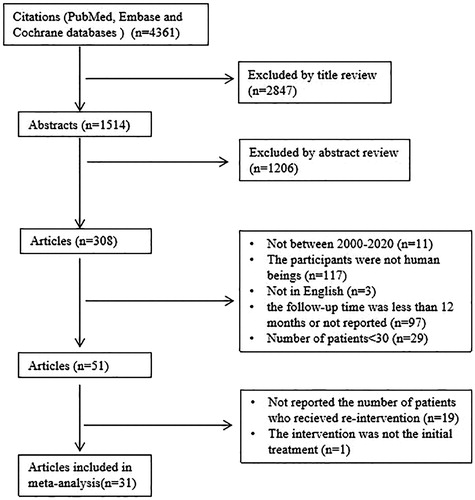
Initially, totally 4361 records were identified in the target database. Full texts of more than 300 articles were reviewed because the re-intervention risk was usually not a primary outcome in studies. A total of 31 studies were included in the final analysis (). Among the included studies, six were randomized controlled studies [Citation4,Citation11–15] and 25 were cohort studies [Citation5–7,Citation9,Citation16–36]. In addition, 18 from Europe (58.1%), 9 originated from USA (29.0%), 3 from Japan (9.7%), and 1 from Israel (3.2%). We evaluated the quality of the studies based on the Newcastle-Ottawa scale, and all studies had a score that ranged from 6 to 9 ().
Table 1. Characteristics of the included studies.
Due to the re-intervention data, the patients treated by ultrasound image-guided focused ultrasound surgery (USgFUS) were not involved. Some studies presented more than one treatment. Therefore, the total number was not the same as the sum of subgroups. These studies compared the re-intervention case following myomectomy, UAE and MRgFUS in the treatment of UFs. The main outcome was the re-intervention rate of these regimens. lists the baseline characteristics of the patients included in these studies.
3.2. Primary outcome
Meta-analysis of the 12-month, 24-month, 36-month and 60-month re-intervention rate of MRgFUS, UAE and myomectomy for UFs was shown in . Among the short-time efficacy of this regimens, for 12-month re-intervention rate, estimations of the pooled rates of MRgFUS, UAE, and myomectomy were 0.12 (95%CI, 0.04–0.20; I2=89.1%; p = 0.000), 0.07 (95%CI, 0.06–0.09; I2=14.2%; p = 0.324), and 0.06 (95%CI, 0.01–0.11; I2=95.1%; p = 0.000), respectively. In terms of the 24-month re-intervention rate, estimations of the pooled rates of MRgFUS, UAE, and myomectomy were 0.14 (95%CI, 0.07–0.21), 0.08 (95%CI, 0.01–0.17; I2=75.7%; p = 0.016), and 0.10 (95%CI, 0.04–0.16; I2=76.0%; p = 0.002), respectively.
Table 2. Meta-analysis of the 12-month, 24-month, 36-month and 60-month re-intervention rate of MRgFUS, UAE and myomectomy for UFs.
Among the long-time efficacy of this regimen, for the 36-month re-intervention rate, estimations of the pooled rates of MRgFUS, UAE, and myomectomy were 0.22 (95%CI, 0.11–0.32; I2=86.3%; p = 0.002), 0.14 (95%CI, 0.05–0.23; I2=94.7%; p = 0.000), and 0.09 (95%CI, 0.05–0.13; I2=0.0%; p = 0.508), respectively. Regarding the 60-month re-intervention rate, estimations of the pooled rates of MRgFUS, UAE, and myomectomy were 0.49 (95%CI, 0.21–0.77; I2=96.5%; p = 0.000), 0.21 (95%CI, 0.17–0.25; I2=84.1%; p = 0.000), and 0.19 (95%CI, 0.15–0.24; I2=53.7%; p = 0.071), respectively. presents the longitudinal data of re-intervention rate.
3.3. Publication bias and sensitivity analyses
The publication bias analyses were quantified with Egger’s test. No obvious asymmetry or p > 0.05 was detected, suggesting that there was no evidence of publication bias. A sensitivity analysis was employed to assess the reliability of the results. When one study was deleted at a time, the heterogeneity and the results still presented no difference.
4. Discussion
In recent decades, success has been achieved in the management of UFs after uterine-sparing treatment. Nevertheless, the real efficacy of this regimen still remained unknown [Citation37]. The meta-analysis of re-intervention rate after treatment for UFs was conducted to demonstrate that, the efficacy of the common uterine-sparing treatment including myomectomy, UAE, and MRgFUS, was satisfactory in the 12th month, the 24th month and the 36th month. However, the re-intervention rate of MRgFUS increased rapidly in the 60th month after treatment. To the best of our knowledge, this is the first study to report re-intervention rate meta-analysis after the treatment for UFs.
UFs are the extremely common benign tumors of female genital tract, causing substantial physical and psychological damages to patients. For women desiring uterine conservation, the re-intervention risk after treatment was the main factor affecting the clinical decision making [Citation38]. However, the short-time and long-time re-intervention rate of the uterine-sparing regimens was still debated [Citation1]. Some previous studies have reported the efficacy of different regimens. For example, Isaac T Manyonda et al. reported that [Citation12], both UAE and myomectomy contributed to significant and equal improvements in QoL. Meanwhile, UAE allowed a shorter hospital stay but with a higher rate of reintervention. In our meta-analysis, the re-intervention rate of UAE was higher than myomectomy but lower than MRgFUS.
Myomectomy, including laparoscopic, hysteroscopic, abdominal or transvaginal myomectomy, is a widely used procedure for removing leiomyomas [Citation23]. A longitudinal retrospective cohort study including 35631 patients demonstrated that the re-intervention rate of myomectomy was 4% [Citation6]. In our meta-analysis, estimations of the pooled 12-month, 24-month, 36-month and 60-month re-intervention rates of myomectomy were respectively 6%, 10%, 9% and 19%, which were the lowest of the three regimens. According to the results, less than one fifth patients with UFs suffered re-intervention during the five years following myomectomy. The reason of myomectomy with the lowest re-intervention rate may be related to the surgery, while in myomectomy procedure, the tumors had removed. Therefore, the re-intervention event happened only due to new fibroids development.
UAE is less invasive, and associated with a shorter hospital stay and a quicker recovery regimen for UFs. Additionally, the currently available data on the likelihood of failure after UAE are inconsistent [Citation39]. For example, the lowest 60-month re-intervention rate of UAE was reported by Giovanna Tropeano et al. as 7% and the highest was reported by Annefleur M de Bruijn et al. as 35% [Citation15,Citation16]. In our meta-analysis, estimations of the pooled 12-month, 24-month, 36-month and 60-month re-intervention rates of UAE were respectively 7%, 8%, 14% and 21%, which were lower than MRgFUS but higher than myomectomy. The results proved that one fifth patients with UFs suffered re-intervention during the five years following UAE. Additionally, the reason of UAE having a higher re-intervention rate than myomectomy also lies in the procedure that the uterine fibroids has not been removed, and thus the fibroids left in suit may still have the risk of recurrence [Citation40].
High intensity focused ultrasound (HIFU), including MRgFUS and USgFUS, is a newly thermal ablation technique for UFs treatment, resulting in reduced toxicity compared with other ablation techniques [Citation41]. It is a no-invasive and low-cost procedure, which can cause minimal pain [Citation42]. However, the short-time and long-time efficacy still remained unknown [Citation43]. In our study, the re-intervention was defined as all additional intervention necessary after primary intervention (such as hysterectomy, myomectomy and UAE) [Citation9]. Due to the lack of re-treatment data of USgFUS, we only conducted a meta-analysis of MRgFUS. Estimations of the pooled 12-month, 24-month, 36-month and 60-month re-intervention rates of MRgFUS were respectively 12%, 14%, 22% and 49%, which were the highest of the three regimens. Based on the obtained results, MRgFUS was a satisfactory alternative to surgery or UAE for fibroids with a re-intervention lower than 30%. However, the rate increased rapidly in the 60th month. It can be explained by the theory that the efficacy of this technique was associated with none perfusion volume (NPV) ratio of fibroids after treatment. For MRgFUS procedure, the mean NPV% was 48.4 ± 25.0% [Citation35]. This part of fibroids without ablation may keep growing, which can cause the re-intervention.
However, the present study still had some limitations. Firstly, the main limitation of the present meta-analysis was the observed substantial heterogeneity. We are aware of that a lot of factors such as age, location of fibroids and menopause status might influence the re-intervention. However, further sub-analysis by this factor was not possible, because the information can not be obtained from the relevant studies. Nevertheless, this meta-analysis provides insights into current re-intervention rate and the obtained findings can be directly applicable in daily practice for counseling patients that are often eligible for over one treatment option. Secondly, there was not a sufficient number of RCTs for inclusion, which may have led to selection bias. In addition, our study has not included the patients with UFs who were treated by USgFUS due to the lack of data. The mean NPV% of USgFUS reported by Zhao WP et al. [Citation44] was 68.5 ± 24.1%, which was more than that of MRgHIFU, indicating that further studies are required to evaluate the re-intervention of USgFUS.
In conclusion, myomectomy, UAE, and MRgFUS are effective for the treatment of UFs. The re-intervention rates of myomectomy, UAE, and MRgFUS are lower than 30% those during the 12 months, 24 months and 36 months. However, the rate of MRgFUS increased fast (49%) in the 60th month.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Grube M, Neis F, Brucker SY, et al. Uterine fibroids - current trends and strategies. Surg Technol Int. 2019;34:257–263.
- Bulun SE. Uterine fibroids. N Engl J Med. 2013;369(14):1344–1355.
- Giuliani E, As-Sanie S, Marsh EE. Epidemiology and management of uterine fibroids. Int J Gynaecol Obstet. 2020;149(1):3–9.
- Mara M, Fucikova Z, Maskova J, et al. Uterine fibroid embolization versus myomectomy in women wishing to preserve fertility: preliminary results of a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2006;126(2):226–233.
- Subramanian S, Clark MA, Isaacson K. Outcome and resource use associated with myomectomy. Obstet Gynecol. 2001;98(4):583–587.
- Davis MR, Soliman AM, Castelli-Haley J, et al. Reintervention rates after myomectomy, endometrial ablation, and uterine artery embolization for patients with uterine fibroids. J Womens Health (Larchmt). 2018;27(10):1204–1214.
- Goodwin SC, Spies JB, Worthington-Kirsch R, et al. Uterine artery embolization for treatment of leiomyomata: long-term outcomes from the FIBROID registry. Obstet Gynecol. 2008;111(1):22–33.
- Vilos GA, Vilos AG, Abu-Rafea B, et al. Interventional uterine-sparing therapies for leiomyomas: a commentary on myolysis. J Obstet Gynaecol Can. 2020;42(2):169–172.
- Froeling V, Meckelburg K, Schreiter NF, et al. Outcome of uterine artery embolization versus MR-guided high-intensity focused ultrasound treatment for uterine fibroids: long-term results. Eur J Radiol. 2013;82(12):2265–2269.
- Page MJ, McKenzie JE, Bossuyt PM, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. 2021;134:103–112.
- Edwards RD, Moss JG, Lumsden MA, et al. Uterine-artery embolization versus surgery for symptomatic uterine fibroids. N Engl J Med. 2007;356(4):360–370.
- Manyonda IT, Bratby M, Horst JS, et al. Uterine artery embolization versus myomectomy: impact on quality of life–results of the FUME (Fibroids of the Uterus: Myomectomy versus Embolization) trial. Cardiovasc Intervent Radiol. 2012;35(3):530–536.
- Moss JG, Cooper KG, Khaund A, et al. Randomised comparison of uterine artery embolisation (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG. 2011;118(8):936–944.
- van der Kooij SM, Hehenkamp WJ, Volkers NA, et al. Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroids: 5-year outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2010;203(2):105.e1-13.
- de Bruijn AM, Ankum WM, Reekers JA, et al. Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroids: 10-year outcomes from the randomized EMMY trial. Am J Obstet Gynecol. 2016;215(6):745.e1–745.e12.
- Tropeano G, Di Stasi C, Amoroso S, et al. Incidence and risk factors for clinical failure of uterine leiomyoma embolization. Obstet Gynecol. 2012;120(2 Pt 1):269–276.
- Joffre F, Tubiana JM, Pelage JP, et al. FEMIC (Fibromes Embolisés aux MICrosphères calibrées): uterine fibroid embolization using tris-acryl microspheres. A French multicenter study. Cardiovasc Intervent Radiol. 2004;27(6):600–606.
- Ikink ME, Nijenhuis RJ, Verkooijen HM, et al. Volumetric MR-guided high-intensity focused ultrasound versus uterine artery embolisation for treatment of symptomatic uterine fibroids: comparison of symptom improvement and reintervention rates. Eur Radiol. 2014;24(10):2649–2657.
- Lohle PN, Voogt MJ, De Vries J, et al. Long-term outcome of uterine artery embolization for symptomatic uterine leiomyomas. J Vasc Interv Radiol. 2008;19(3):319–326.
- Morita Y, Ito N, Hikida H, et al. Non-invasive magnetic resonance imaging-guided focused ultrasound treatment for uterine fibroids – early experience. Eur J Obstet Gynecol Reprod Biol. 2008;139(2):199–203.
- Scheurig-Muenkler C, Koesters C, Powerski MJ, et al. Clinical long-term outcome after uterine artery embolization: sustained symptom control and improvement of quality of life. J Vasc Interv Radiol. 2013;24(6):765–771.
- Sone M, Arai Y, Shimizu T, et al. Phase I/II multiinstitutional study of uterine artery embolization with gelatin sponge for symptomatic uterine leiomyomata: Japan Interventional Radiology in Oncology Study Group study. J Vasc Interv Radiol. 2010;21(11):1665–1671.
- Stewart EA, Faur AV, Wise LA, et al. Predictors of subsequent surgery for uterine leiomyomata after abdominal myomectomy. Obstet Gynecol. 2002;99(3):426–432.
- Walker WJ, Barton-Smith P. Long-term follow up of uterine artery embolisation–an effective alternative in the treatment of fibroids. BJOG. 2006;113(4):464–468.
- Duvnjak S, Ravn P, Green A, et al. Clinical long-term outcome and reinterventional rate after uterine fibroid embolization with nonspherical versus spherical polyvinyl alcohol particles. Cardiovasc Intervent Radiol. 2016;39(2):204–209.
- Funaki K, Fukunishi H, Sawada K. Clinical outcomes of magnetic resonance-guided focused ultrasound surgery for uterine myomas: 24-month follow-up. Ultrasound Obstet Gynecol. 2009;34(5):584–589.
- Mindjuk I, Trumm CG, Herzog P, et al. MRI predictors of clinical success in MR-guided focused ultrasound (MRgFUS) treatments of uterine fibroids: results from a single centre. Eur Radiol. 2015;25(5):1317–1328.
- Narayan A, Lee AS, Kuo GP, et al. Uterine artery embolization versus abdominal myomectomy: a long-term clinical outcome comparison. J Vasc Interv Radiol. 2010;21(7):1011–1017.
- Popovic M, Berzaczy D, Puchner S, et al. Long-term quality of life assessment among patients undergoing uterine fibroid embolization. AJR Am J Roentgenol. 2009;193(1):267–271.
- Quinn SD, Vedelago J, Gedroyc W, et al. Safety and five-year re-intervention following magnetic resonance-guided focused ultrasound (MRgFUS) for uterine fibroids. Eur J Obstet Gynecol Reprod Biol. 2014;182:247–251.
- Walid MS, Heaton RL. Laparoscopic myomectomy: an intent-to-treat study. Arch Gynecol Obstet. 2010;281(4):645–649.
- Flyckt R, Soto E, Nutter B, et al. Comparison of long-term fertility and bleeding outcomes after robotic-assisted, laparoscopic, and abdominal myomectomy. Obstet Gynecol Int. 2016;2016:2789201.
- Sangha R, Katukuri V, Palmer M, et al. Recurrence after robotic myomectomy: is it associated with use of GnRH agonist? J Robot Surg. 2016;10(3):245–249.
- Gorny KR, Borah BJ, Brown DL, et al. Incidence of additional treatments in women treated with MR-guided focused US for symptomatic uterine fibroids: review of 138 patients with an average follow-up of 2.8 years. J Vasc Interv Radiol. 2014;25(10):1506–1512.
- Verpalen IM, de Boer JP, Linstra M, et al. The Focused Ultrasound Myoma Outcome Study (FUMOS); a retrospective cohort study on long-term outcomes of MR-HIFU therapy. Eur Radiol. 2020;30(5):2473–2482.
- Mohr-Sasson A, Machtinger R, Mashiach R, et al. Long-term outcome of MR-guided focused ultrasound treatment and laparoscopic myomectomy for symptomatic uterine fibroid tumors. Am J Obstet Gynecol. 2018;219(4):375.e1–375.e7.
- Vilos GA, Allaire C, Laberge PY, et al. The management of uterine leiomyomas. J Obstet Gynaecol Can. 2015;37(2):157–178.
- Stewart EA, Laughlin-Tommaso SK, Catherino WH, et al. Uterine fibroids. Nat Rev Dis Primers. 2016;2:16043.
- Kohi MP, Spies JB. Updates on uterine artery embolization. Semin Intervent Radiol. 2018;35(1):48–55.
- Keung JJ, Spies JB, Caridi TM. Uterine artery embolization: a review of current concepts. Best Pract Res Clin Obstet Gynaecol. 2018;46:66–73.
- Izadifar Z, Izadifar Z, Chapman D, et al. An introduction to high intensity focused ultrasound: systematic review on principles, devices, and clinical applications. JCM. 2020;9(2):460.
- Łoziński T, Filipowska J, Gurynowicz G, et al. The effect of high-intensity focused ultrasound guided by magnetic resonance therapy on obstetrical outcomes in patients with uterine fibroids - experiences from the main Polish center and a review of current data. Int J Hyperthermia. 2019;36(1):582–590.
- Szkodziak P, Szkodziak F, Trzeciak K, et al. Minimally invasive procedures in the management of uterine fibroids. Prz Menopauzalny. 2017;16(4):122–125.
- Zhao WP, Chen JY, Chen WZ. Dynamic contrast-enhanced MRI serves as a predictor of HIFU treatment outcome for uterine fibroids with hyperintensity in T2-weighted images. Exp Ther Med. 2016;11(1):328–334.