Abstract
Tumor ablation has been widely applied in Asia, accounting for 44.65% of clinical studies worldwide. We reviewed 5853 clinical studies to provide insight on the advance of tumor ablation in Asia chronologically and geographically among different techniques and organs. Since 1998, tumor ablation application has dramatically evolved in Asia. All kinds of ablation techniques, including percutaneous ethanol injection (PEI), radiofrequency ablation (RFA), microwave ablation (MWA), laser ablation (LA), cryoablation (CA), high-intensity focused ultrasound (HIFU), and irreversible electroporation (IRE), have been applied, with the first application of PEI and the most popular application of RFA. Twenty-five countries and one district in Asia have applied tumor ablation in various organs, including liver, lung, uterus, thyroid, kidney, pancreas, bone, prostate, breast, adrenal gland, lymph node parathyroid, esophagus, etc. Due to the high incidence of tumors as well as advanced economy and technology, East Asia accounted for 93.87% of studies, led by China (45.00%), Japan (32.72%), South Korea (12.10%), and Taiwan (4.03%). With the enrichment of evidence from large-scale multicenter and randomized control studies, China and South Korea have issued several guidelines on tumor ablation for liver, lung, and thyroid, which provided recommendations for global standardization of tumor ablation techniques. Therefore, Asia has made active contribution to global tumor ablation therapy.
Key point 1: Asia accounted for 44.65% of clinical studies worldwide on tumor ablation.
Key point 2: Twenty-five countries and one district in Asia have used tumor ablation in various organs, and East Asia accounted for 93.87% of studies, led by China (45.00%), Japan (32.72%), South Korea (12.10%), and Taiwan (4.03%).
Key point 3: China and South Korea have issued several guidelines on tumor ablation for liver, lung, and thyroid, which provided recommendations for global standardization of tumor ablation techniques
Keypoints
Introduction
According to global cancer statistics [Citation1], Asia accounted for nearly half of new cancers and over half of the cancer-related deaths. Among the top ten cancers worldwide, liver, lung, and thyroid cancers were particularly prevalent in Asia. While surgery remains the gold standard for treating these cancers, most patients are unsuitable candidates for surgery [Citation2]. In this case, ablation as a minimally invasive technique can be an alternative treatment strategy.
Over the past 30 years, applying tumor ablation has exploded in popularity in Asia, particularly since 1998. All kinds of ablation techniques have been employed. The first international clinical reports on chemical and energy ablation were both published by a Japanese research group in the 1980s using percutaneous ethanol injection (PEI) [Citation3] and laser ablation (LA) to treat liver cancers. Since then, cryoablation (CA, 1988) [Citation4], microwave ablation (MWA, 1994) [Citation5], radiofrequency ablation (RFA, 1999) [Citation6], high-intensity focused ultrasound (HIFU, 2001) [Citation7], and irreversible electroporation (IRE) [Citation8] have been successfully introduced into clinical use in Asia. Tumor ablation has been extensively applied in various organs, including liver, lung, uterus, thyroid, kidney, pancreas, bone, prostate, breast, adrenal gland, lymph node parathyroid, esophagus, etc. Due to the high incidence of tumors as well as sophisticated economy and technology, tumor ablation was mainly applied in East Asia, particularly in China, Japan, South Korea, and Taiwan. With the enriched experience from large-scale multicenter and randomized control studies, China and South Korea have issued numerous guidelines on tumor ablation for liver [Citation9], lung [Citation10–12], and thyroid [Citation13–15]. These guidelines provided recommendations for the global standardization of tumor ablation techniques.
In 2004, Rhim H [Citation16] reviewed the Asian experience with thermal ablation techniques and clinical practice with a particular emphasis on treating hepatocellular carcinoma (HCC). They addressed how tumor ablation was mostly utilized to treat unresectable liver tumors with the most application of RFA in Asia. Over the years, tumor ablation has been greatly developed in techniques and application organs. Therefore, we designed this study to review clinical studies chronologically and geographically among different techniques and organs to provide insight on tumor ablation advancement in Asia.
Article search strategy
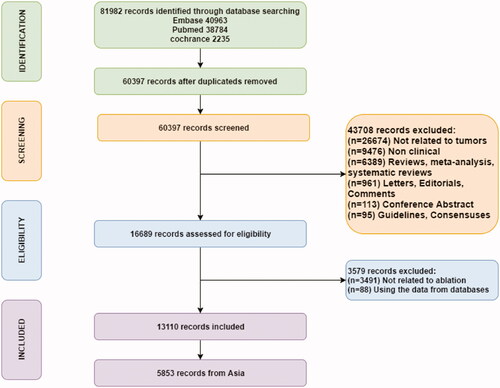
We conducted a comprehensive literature search of PubMed, EMBASE, and Cochrane databases, regardless of the beginning date. The deadline was set in data when searching databases (2 July 2020). The search terms included both Medical Subject Heading terms (MeSH) and free words, which were as follows: (‘radiofrequency ablation’) OR (‘radiofrequency’ AND ‘ablation’) OR (‘microwave ablation’) OR (‘microwave coagulation’) OR (‘microwave’ AND ‘ablation’) OR (‘microwave’ AND ‘coagulation’) OR (‘laser ablation’) OR (‘high-intensity focused ultrasound ablation’ OR ‘HIFU’) OR (‘high intensity focused ultrasound’) OR (‘ethanol ablation’ OR ‘percutaneous ethanol injection’) OR (‘ethanol injection’) OR (‘percutaneous’ AND ‘ethanol’ AND ‘injection’) OR (‘ethanol’ AND ‘ablation’) OR (‘cryoablation’) OR (‘cryosurgery’ AND ‘ablation’) OR (‘irreversible electroporation’ OR (‘irreversible’ AND ‘electroporation’) OR (‘Ablation Techniques’ OR ‘thermal ablation’) OR (‘chemical ablation’). The study type was restricted to clinical trials. After searching databases, 81,982 studies were retrieved. After excluding duplicated records, 60,397 publications were screened by reading the title, abstract or full text. The eligibility criteria were as follows: (1) clinical study on human beings; (2) research focused on tumor ablation, including benign, malignant/primary, secondary tumors, and atypical hyperplasia. The exclusion criteria were as follows: (1) review articles, meta-analyses, systematic reviews, letters, conference abstracts, editorials, comments, guidelines, and consensuses; (2) articles unrelated to tumor ablation; and (3) articles that used data from databases. Finally, 13,110 articles were enrolled, including 5853 articles from Asia. The article searching and screening process is summarized in .
Trend and geographical distribution of tumor ablation techniques
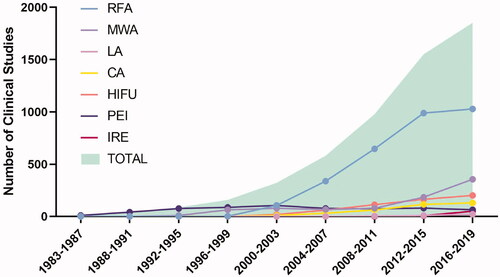
All kinds of ablation techniques have been employed in Asia. After the first application of chemical and energy ablation in Japan in the 1980s using PEI and LA to treat liver cancers, CA (1988), MWA (1994), RFA (1999), HIFU (2001), and IRE (2013) have been successfully introduced into clinical use in Asia. Japan also made the first international clinical study on MWA to treat liver cancers. Tumor ablation has exploded in popularity in Asia during the last three decades, particularly since the introduction of RFA in 1999. Since then, most (94.85%) studies have been published ().
RFA is the most popular technique for tumor ablation, accounting for nearly half of the total (56.30%, 3295/5853), followed by MWA (17.12%, 1002/5853), PEI (11.97%, 701/5853), HIFU (10.42%, 610/5853), CA (6.35%, 372/5853), IRE (1.17%, 68/5853), LA (0.81%, 47/5853), and chemical ablation (other than PEI, 0.36%, 21/5853).
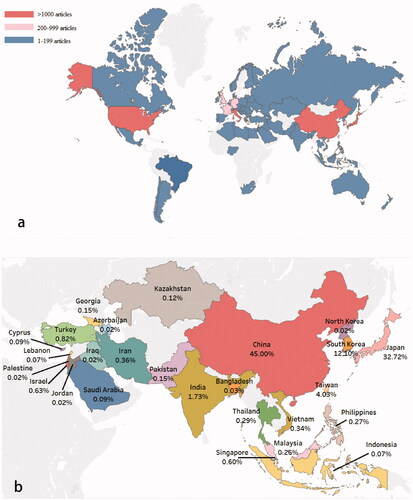
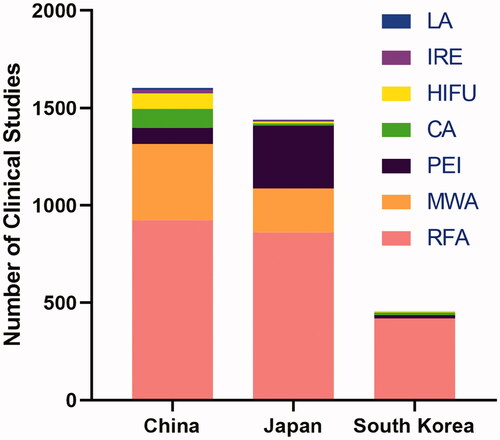
There are 73 countries and one district that have applied tumor ablation worldwide (). Most clinical studies were published by Asia (44.65% 5853/13110), followed by Europe (30.88%, 4049/13110), America (22.59%, 2961/13110), Oceania (1.05%, 137/13110), and Africa (0.84%, 110/13110). In Asia, 25 countries and one district have applied tumor ablation (). The number of clinical studies on tumor ablation varies across different regions. As a result of the high prevalence of tumors and sophisticated economy and technology, East Asia accounted for 93.87% (5494/5853) of studies with the top four regions as follows: China (45.00%, 2634/5853), Japan (32.72%, 1915/5853), South Korea (12.10%, 708/5853) and Taiwan (4.03%, 236/5853).
Figure 3. (a) Global distribution of clinical studies on tumor ablation. Red: >1000 articles; Pink: 200–999 articles; Blue: 1–199 articles. (b) Geographical distribution of clinical studies on tumor ablation in Asia. Only regions where tumor ablation has been applied are shown. The percentage represents the proportion of clinical studies published in the region.
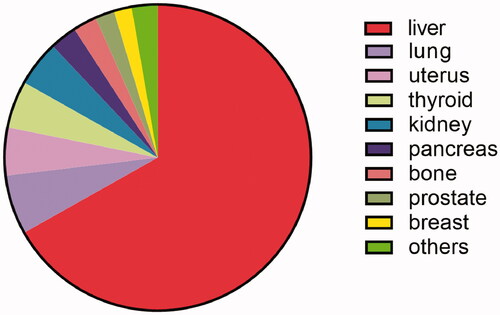
The extensive use of tumor ablation in various organs
Tumor ablation has been employed in 22 different organs in Asia, including liver (67.35%, 3942/5853), lung (6.31%, 370/5853), uterus (5.10%, 299/5853), thyroid (5.02%,294/5853), kidney (4.88%, 285/5853), pancreas (2.87%, 168/5853), bone (2.53%,148/5853), prostate (2.06%, 120/5853), breast (1.90%,111/5853), others (2.75%,161/5853, parathyroid, adrenal gland, esophagus, lymph node, soft tissue, etc.) (). We reviewed the Asian experience of tumor ablation in various organs, with a particular emphasis on the top few organs.
Liver
The incidence of liver cancer remains high in Asia, particularly in the East and South-East [Citation1,Citation17]. Consistent with cancer incidence, the liver is the most commonly targeted organ for tumor ablation, accounting for over half of the total (67.35%) according to our analysis.
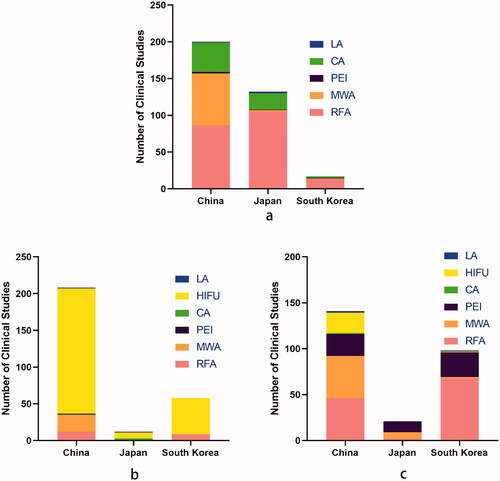
In Asia, 22 countries and one district have applied ablation techniques to treat liver cancers. China, Japan, and South Korea are the top three regions having the most clinical trials on liver ablation (). China is the only region where all seven ablation techniques have been applied to treat liver cancers.
Figure 5. The top three regions with the most clinical studies published on liver ablation using each technique. PEI: percutaneous ethanol injection; LA: laser ablation; CA: cryoablation; MWA: microwave ablation; RFA: radiofrequency ablation; HIFU: high-intensity focused ultrasound; IRE: irreversible electroporation.
PEI was initially reported by Japan in the 1980s as the first ablation technique to treat liver cancers [Citation3,Citation18]. Over the past 30 years, 11 regions in Asia have applied PEI to treat liver cancers, of which Japan published most studies (). Japan reported the largest sample size clinical experience with PEI in treating HCCs. The overall survival rates were 83–90%, 52–65% and 27–40% at 1 year, 3 years, and 5 years, respectively [Citation19]. A randomized trial from China demonstrated that PEI appeared to be as effective as resection in treating small HCCs [Citation20]. However, due to the non-uniform penetration of ethanol in the targeted tissue, the treatment efficacy was limited in larger tumors [Citation21]. As a result, with the development of energy ablation techniques, PEI is mainly used as an auxiliary of other techniques in recent years [Citation22,Citation23].
The first clinical study on MWA treating liver cancers was reported by Japan in 1994 [5]. Seki T et al. first performed microwave coagulation in 18 patients with a single unresectable HCC with a diameter of 2 cm or less. Since then, six Asian regions have successively employed MWA to treat liver cancers, of which China published most studies. A Chinese research group designed the largest multicenter clinical study. Liang P. et al. [Citation24] analyzed the MWA efficacy in treating 1363 treatment-naïve lesions of 1007 patients with primary liver tumors. The overall survival rates were 91.2%, 72.5%, and 59.8% at 1 year, 3 years, and 5 years respectively. Besides, several long-term follow-up studies revealed favorable survival rates of MWA in treating liver cancers [Citation25–28] (). Additionally, a Chinese research group revealed a low risk of neoplastic seeding after MWA by analyzing 14-year experience with 1462 patients [Citation40].
Table 1. Summary of clinical studies on liver ablation.
The first clinical RFA experience in treating liver cancers worldwide was reported by Italian physicians in 1993 [Citation41]. In Asia, RFA was first used to treat liver cancers in 1998. Japanese physicians first evaluated the efficacy of combined RFA and arterial infusion chemotherapy in treating liver metastases from colorectal cancer [Citation6]. Since then, most physicians have switched their treatment strategy from PEI and MWA to RFA [Citation16,Citation42,Citation43]. By now, 19 Asian regions have employed RFA to treat liver cancers, of which China published most studies. Three large sample size studies with a ten-year follow-up from Japan and South Korea revealed that RFA patients achieved favorable survival rates (59.7–83.7% and 27.3–74.2% at five and ten years, respectively, ) [Citation29–31]. A Japanese research group evaluated RFA complications for HCCs by analyzing 16,346 treated nodules in 13,283 patients in a multicenter study. The complication rate was 3.54%, confirming that RFA was a low-risk treatment for HCC [Citation44]. Technique efficacy was evaluated in comparative studies (). Several large randomized control studies from Asia exhibited comparable survival outcomes between RFA and surgical resection in treating small HCCs [Citation32,Citation34–36]. However, Huang J. et al. [Citation33] demonstrated that resection provided better survival outcomes than RFA for HCC conforming to the Milan criteria (single HCC ≤5 cm or up to 3 nodules <3 cm). The contradictory outcomes may result from differences in technology and physician experience. Besides, numerous randomized control studies compared RFA with other ablation techniques, as displayed in . The results revealed that RFA was superior to PEI in treating small HCCs, as evidenced by higher survival rates and similar adverse events [Citation37–39]. This may also result in PEI replacement to treat liver cancers in Asia. MWA and RFA have similar clinical values regarding long-term survival and complications [Citation25,Citation27].
China was the first to apply HIFU in liver ablation. In 2001, Fang W. et al. investigated the pathologic changes in liver cancers after HIFU [Citation7]. This was the first clinical study that revealed the effectiveness and feasibility of HIFU in treating liver cancers. Over the past 20 years, only 5 Asian regions have employed HIFU to treat liver cancers with limited studies for its relatively low thermal efficiency.
IRE was first reported as an emerging ablation technique in 2011 by an Australian research group [Citation45]. In 2013, Huang et al. reported the pilot experience of IRE for liver cancers in Asia [Citation8]. Over the past seven years, six Asian regions have introduced IRE to liver ablation. Compared to western countries, applying IRE, CA, and LA was limited in Asia.
Lung
Lung cancer is the leading cause of death among men in most Asian countries, particularly in China [Citation1]. Our study enrolled 370 clinical studies (6.31%, 370/5853) () on lung ablation. A great inclination has been made in selecting the ablation technique (). The largest proportions are exhibited by RFA (216 studies, 216/370, 58.38%), followed by MWA (79 studies, 79/370, 21.35%), CA (66 studies, 66/370, 17.84%), LA (5 studies, 5/370, 1.35%) and PEI (4 studies, 4/370, 1.08%).
Figure 6. The top three regions with the most clinical studies published on (a) lung, (b) uterine, (c) thyroid using different ablation techniques. PEI: percutaneous ethanol injection; LA: laser ablation; CA: cryoablation; MWA: microwave ablation; RFA: radiofrequency ablation; HIFU: high-intensity focused ultrasound; IRE: irreversible electroporation.
In 2000, an American research team firstly reported RFA use in treating three cases of lung tumors [Citation46]. In 2002, a Japanese research team conducted a pilot study in Asia on the clinical feasibility and safety of RFA therapy for inoperable lung tumors [Citation47]. The follow-up CT revealed no noticeable tumor regrowth in any patients without observing severe complications or side effects. Over the past 20 years, 11 regions in Asia have applied lung ablation, among which China is the region with the most studies published. We summarized the long-term follow-up clinical studies on lung ablation, two of which were multicenter researches (). The survival rates range was 66.7–97%, 41.1–82%, and 24.6–74% at 1 year, 2 years, and 3 years respectively. Most studies applied CT as an image guiding method [Citation48–51]. The US is exclusively indicated for treating peripheral lung neoplasms [Citation52].
Table 2. Summary of clinical studies on lung ablation.
Uterus
Image-guided ablation has been used frequently utilized to treat uterine disease in Asia (). Our study enrolled 299 studies. HIFU (245 studies, 245/299, 81.94%) was the most widely used technique for uterine ablation, followed by MWA (25 studies, 25/299, 8.36%), RFA (22 studies, 22/299, 7.36%), CA (4 studies, 4/299, 1.34%), LA (2 studies, 2/299, 0.67%), and PEI (1 study, 1/299, 0.33%) (). The first commercial HIFU device to treat solid tumors was designed in Asia (ExAbalte 2000, InSightec-TxSonics Ltd., Haifa, Israel) and was approved by FDA to treat uterine fibroid patients. The first clinical HIFU experience to treat uterine fibroids worldwide occurred in China in 2002 [Citation53]. Over the past 20 years, seven Asian regions have used ablation to treat uterine fibroids, adenomyosis, and cervical intraepithelial neoplasia. China is the region with the most studies published (). Three large sample size clinical studies [Citation54–56] conducted in China revealed the effectiveness of HIFU and MWA in treating uterine fibroids. The median tumor reduction rates (volume before therapy – volume after therapy)/volume before therapy × 100%) was 21.2–22.2%, 29.6–63.5%, 44.8–78.5%, and 48.7–86.7% at 1 month, 3 months, 6 months and 12 months respectively.
Thyroid
Thyroid cancer is highly prevalent in Asia, particularly in South Korea, where the incidence was the highest globally for both genders [Citation1]. Fourteen Asian regions have used thyroid ablation, with China publishing the most studies (). Six kinds of ablation techniques have been employed in thyroid ablation, including RFA (126 studies, 126/294, 42.86%), PEI (83 studies, 83/294, 28.23%), MWA (55 studies, 55/294, 18.71%), HIFU (25 studies, 25/294, 8.50%), LA (3 studies, 3/294, 1.02%), CA (2 studies, 2/294, 0.68%) ().
The first international clinical study on RFA and MWA in treating thyroid nodules was from Asia. In 2006, a research group in South Korea published the first clinical experience using RFA in treating benign cold thyroid nodules [Citation57]. In 2012, a Chinese research group first addressed the feasibility of MWA to treat benign thyroid nodules [Citation58]. Currently, thyroid ablation has been utilized in various thyroid nodule types, including benign thyroid nodules, papillary thyroid microcarcinomas (PTMC), and recurrent thyroid cancers. We summarized clinical studies on thyroid ablation with a minimum follow-up of six months [Citation59–64] (). These studies included benign and malignant thyroid nodules. The thyroid nodules in all studies had a mean volume reduction rate of 71.0–98.8%. No major complications were observed in all cases. Two South Korean randomized controlled trials [Citation65,Citation66] examined whether RFA and PEI were equally effective in treating cystic and predominantly cystic thyroid nodules.
Table 3. Summary of clinical studies on thyroid ablation.
Other organs
In Asia, ablation techniques have been deployed to treat tumors of various organs, although the number of studies on specific organs is limited. The first international clinical study of HIFU in treating pancreatic cancers was reported in 2005 by a Chinese research group [Citation67]. Besides, a Chinese research group published the largest sample size clinical study comparing MWA and laparoscopic partial nephrectomy for cT1a renal cell carcinoma, revealing comparable oncologic outcomes and complications between two treatments [Citation68]. Additional research in additional regions is urgent in the future to expand the application of ablation in various organs.
Guidelines issued on tumor ablation in Asia
In the last decades, with evidence from large-scale multicenter or randomized control studies has accumulated, various guidelines on tumor ablation have been issued on liver, lung, and thyroid.
The Asian Society on Tumor Ablation (ASTA) was founded in 2014 and has hosted yearly conferences since then (ACTA: Asian Conference on Tumor Ablation). The ASTA has a multicenter trial committee and published several multicenter studies on liver ablation [Citation69–71]. In addition, ASTA has a guideline committee and issued ASTA guidelines on the thyroid [Citation72], kidney (in press), and adrenal (in press) ablation.
In 2013, the Society of Chinese Interventional Ultrasound issued the guidelines for ultrasound-guided percutaneous MWA of liver malignancy [Citation9]. In 2014, the Minimally Invasive and Comprehensive Treatment of Lung Cancer Branch, Professional Committee of Minimally Invasive Treatment of Cancer of the Chinese Anti-Cancer Association organized multidisciplinary experts and developed guidelines for thermal ablation of primary and metastatic lung tumors [Citation10]. In 2015, the Chinese Society of Thoracic and Cardiovascular Surgery Lung Cancer Study Group released the expert consensus on image-guided RFA of lung tumors [Citation12], followed by the 2018 guidelines issued after detailed refinement of the old edition [Citation11].
In 2012, the Korean Society of Thyroid Radiology published RFA guidelines of benign thyroid nodules and recurrent thyroid cancers [Citation13]. Five years later, such guidelines were updated with a new edition in 2017 [14]. In 2018, the Korean Society initiated the consensus statement on ethanol ablation in managing symptomatic thyroid nodules [Citation15]. These guidelines recommended standardized thermal ablation procedures, indications for treatment candidates, post-ablation outcome assessment, and complication control.
Novel progression of tumor ablation in Asia
As medical technology advances, various novel technologies have emerged to assist or combine with traditional ablation therapy to optimize ablation procedures and improve efficiency. Additionally, numerous clinical investigations on these novel techniques were published in Asia.
Image fusion navigation in tumor ablation
The effectiveness of ablation is highly dependent on the image guiding technique such as ultrasound, CT, or MRI. The image fusion technology can simultaneously apply multiple guiding modalities, overcoming the limitations of each technique. Image fusion navigation has been introduced as a promising method for tumor ablation. China, Japan, and South Korea have applied image fusion to assist their tumor ablation procedures. The fusion image in these clinical studies was achieved by overlaying images from multiple imaging modalities such as ultrasonography (US)+CT/MR, US + US, CEUS (contrast-enhanced ultrasound) +CT/MR, and CEUS + CECT (contrast-enhanced computed tomography) [Citation73–79].
Molecular targeted and immune therapy in combination with tumor ablation
Systemic therapy for cancers has markedly advanced since the survival benefit of molecularly targeted agents. Numerous large sample sizes and multicenter studies from China revealed that combining molecularly targeted agents, sorafenib, with RFA was superior to RFA or sorafenib alone in improving survival outcomes for treating liver cancers [Citation80–83].
Besides, adoptive immunotherapy is considered to help reduce the recurrence and metastasis rates of cancers. Cellular immunity is critical for antitumor immunity. In the last decade, several clinical studies were conducted on combining adoptive immunotherapy and ablation in treating tumors in Asia. Most studies [Citation84–91] adopted one single immunocyte such as cytokine-induced killer (CIK), RetroNectin activated killer cells (RAK), and natural killer cells (NK cells). Two studies applied multiple successively-administered immunocytes infusion, which was more representative of the native immune response [Citation92,Citation93]. In 2017, a Chinese research group published the first international clinical trial of allogeneic NK cells combined with CA or IRE for treating renal cell cancers [Citation90], advanced non-small-cell lung cancers [Citation84], and metastatic pancreatic cancers [Citation88].
The recent development of immune checkpoint inhibitors has greatly altered the landscape of cancer therapy. In the future, we expect clinical research on combining anti-programmed cell death protein-1 (PD-1) and ablation therapy.
In this review, we only used the number of publications to evaluate tumor ablation advancement. However, there must be a gap from the real status of ablation practices because we cannot acquire the real data on procedure numbers in each country. Future research with more extensive investigations may compensate for this limitation.
This review demonstrated that tumor ablation was widely applied in Asia over the past 30 years in extensive organs. In the next few decades, we should develop multiple novel techniques such as multimodal image navigation, artificial intelligence, nano-material to assist ablation for improving the efficiency of minimally invasive and precise treatment of tumors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
- Petrowsky H, Busuttil RW. Resection or ablation of small hepatocellular carcinoma: what is the better treatment? J Hepatol. 2008;49(4):502–504.
- Sugiura N, Takara K, Ohto M, et al. Percutaneous intratumoral injection of ethanol under ultrasound imaging for treatment of small hepatocellular carcinoma. Acta Hepatologica Japonica. 1983;24:920.
- Zhou XD, Tang ZY, Yu YQ, et al. Clinical evaluation of cryosurgery in the treatment of primary liver cancer. Report of 60 cases. Cancer. 1988;61(9):1889–1892.
- Seki T, Wakabayashi M, Nakagawa T, et al. Ultrasonically guided percutaneous microwave coagulation therapy for small hepatocellular carcinoma. Cancer. 1994;74(3):817–825.
- Kainuma O, Asano T, Aoyama H, et al. Combined therapy with radiofrequency thermal ablation and intra-arterial infusion chemotherapy for hepatic metastases from colorectal cancer. Hepatogastroenterology. 1999;46(26):1071–1077.
- Wu F, Chen WZ, Bai J, et al. Pathological changes in human malignant carcinoma treated with high-intensity focused ultrasound. Ultrasound Med Biol. 2001;27(8):1099–1106.
- Huang K. The pilot experience of irreversible electroporation for medium-size liver cancers in the Asia. J Vasc Interv Radiol. 2013;24(759):e30.
- Liang P, Yu J, Lu MD, et al. Practice guidelines for ultrasound-guided percutaneous microwave ablation for hepatic malignancy. World J Gastroenterol. 2013;19(33):5430–5438.
- Ye X, Fan W, Chen JH, et al. Chinese expert consensus workshop report: guidelines for thermal ablation of primary and metastatic lung tumors. Thorac Cancer. 2015;6(1):112–121.
- Ye X, Fan W, Wang H, et al. Expert consensus workshop report: guidelines for thermal ablation of primary and metastatic lung tumors (2018 edition). J Cancer Res Ther. 2018;14(4):730–744.
- Liu BD, Zhi XY. Expert consensus on image-guided radiofrequency ablation of pulmonary tumors–2015 edition. Chin Clin Oncol. 2015;4:27.
- Na DG, Lee JH, Jung SL, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012;13(2):117–125.
- Kim JH, Baek JH, Lim HK, et al. 2017 Thyroid radiofrequency ablation guideline: Korean society of thyroid radiology. Korean J Radiol. 2018;19(4):632–655.
- Hahn SY, Shin JH, Na DG, et al. Ethanol ablation of the thyroid nodules: 2018 consensus statement by the Korean society of thyroid radiology. Korean J Radiol. 2019;20(4):609–620.
- Rhim H. Review of Asian experience of thermal ablation techniques and clinical practice. Int J Hyperthermia. 2004;20(7):699–712.
- Petrick JL, Florio AA, Znaor A, et al. International trends in hepatocellular carcinoma incidence, 1978–2012. Int J Cancer. 2020;147(2):317–330.
- Shiina S, Yasuda H, Muto H, et al. Percutaneous ethanol injection in the treatment of liver neoplasms. AJR Am J Roentgenol. 1987;149(5):949–952.
- Teratani T, Ishikawa T, Shiratori Y, et al. Hepatocellular carcinoma in elderly patients: beneficial therapeutic efficacy using percutaneous ethanol injection therapy. Cancer. 2002;95(4):816–823.
- Huang GT, Lee PH, Tsang YM, et al. Percutaneous ethanol injection versus surgical resection for the treatment of small hepatocellular carcinoma - a prospective study. Ann Surg. 2005;242(1):36–42.
- Ahmed M, Brace CL, Lee FT, et al. Principles of and advances in percutaneous ablation. Radiology. 2011;258(2):351–369.
- Yang B, You X, Yuan ML, et al. Transarterial ethanol ablation combined with transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus. Hepat Mon. 2016;16(8):e37584.
- Zhou P, Liu X, Li R, et al. Percutaneous coagulation therapy of hepatocellular carcinoma by combining microwave coagulation therapy and ethanol injection. Eur J Radiol. 2009;71(2):338–342.
- Liang P, Yu J, Yu XL, et al. Percutaneous cooled-tip microwave ablation under ultrasound guidance for primary liver cancer: a multicentre analysis of 1363 treatment-naive lesions in 1007 patients in China. Gut. 2012;61(7):1100–1101.
- Lu MD, Xu HX, Xie XY, et al. Percutaneous microwave and radiofrequency ablation for hepatocellular carcinoma: a retrospective comparative study. J Gastroenterol. 2005;40(11):1054–1060.
- Dong B, Liang P, Yu X, et al. Percutaneous sonographically guided microwave coagulation therapy for hepatocellular carcinoma: results in 234 patients. AJR Am J Roentgenol. 2003;180(6):1547–1555.
- Ding J, Jing X, Liu J, et al. Comparison of two different thermal techniques for the treatment of hepatocellular carcinoma. Eur J Radiol. 2013;82(9):1379–1384.
- Xu J, Zhao Y. Comparison of percutaneous microwave ablation and laparoscopic resection in the prognosis of liver cancer. Int J Clin Exp Pathol. 2015;8:11665–11669.
- Shiina S, Tateishi R, Arano T, et al. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol. 2012;107(4):569–577; quiz 578.
- Kim YS, Lim HK, Rhim H, et al. Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol. 2013;58(1):89–97.
- Lee MW, Kang D, Lim HK, et al. Updated 10-year outcomes of percutaneous radiofrequency ablation as first-line therapy for single hepatocellular carcinoma < 3 cm: emphasis on association of local tumor progression and overall survival. Eur Radiol. 2020;30(4):2391–2400.
- Chen MS, Li JQ, Zheng Y, et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg. 2006;243:321–328.
- Huang J, Yan L, Cheng Z, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg. 2010;252(6):903–912.
- Feng K, Yan J, Li X, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol. 2012;57(4):794–802.
- Fang Y, Chen W, Liang X, et al. Comparison of long-term effectiveness and complications of radiofrequency ablation with hepatectomy for small hepatocellular carcinoma. J Gastroenterol Hepatol. 2014;29(1):193–200.
- Ng KKC, Chok KSH, Chan ACY, et al. Randomized clinical trial of hepatic resection versus radiofrequency ablation for early-stage hepatocellular carcinoma. Br J Surg. 2017;104(13):1775–1784.
- Shiina S, Teratani T, Obi S, et al. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology. 2005;129(1):122–130.
- Lin SM, Lin CJ, Lin CC, et al. Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut. 2005;54(8):1151–1156.
- Lin SM, Lin CJ, Lin CC, et al. Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma < = 4cm. Gastroenterology. 2004;127:1714–1723.
- Yu J, Liang P, Yu XL, et al. Needle track seeding after percutaneous microwave ablation of malignant liver tumors under ultrasound guidance: analysis of 14-year experience with 1462 patients at a single center. Eur J Radiol. 2012;81(10):2495–2499.
- Rossi S, Di Stasi M, Buscarini E, et al. Percutaneous radiofrequency interstitial thermal ablation in the treatment of small hepatocellular carcinoma. Cancer J Sci Am. 1995;1(1):73–81.
- Shiina S. Image-guided percutaneous ablation therapies for hepatocellular carcinoma. J Gastroenterol. 2009;44(Suppl.19):122–131.
- Shiina S, Teratani T, Obi S, et al. Nonsurgical treatment of hepatocellular carcinoma: from percutaneous ethanol injection therapy and percutaneous microwave coagulation therapy to radiofrequency ablation. Oncology. 2002;62(Suppl.1):64–68.
- Koda M, Murawaki Y, Hirooka Y, et al. Complications of radiofrequency ablation for hepatocellular carcinoma in a multicenter study: an analysis of 16 346 treated nodules in 13 283 patients. Hepatol Res. 2012;42(11):1058–1064.
- Thomson KR, Cheung W, Ellis SJ, et al. Investigation of the safety of irreversible electroporation in humans. J Vasc Interv Radiol. 2011;22(5):611–621.
- Dupuy DE, Zagoria RJ, Akerley W, et al. Percutaneous radiofrequency ablation of malignancies in the lung. AJR Am J Roentgenol. 2000;174(1):57–59.
- Nishida T, Inoue K, Kawata Y, et al. Percutaneous radiofrequency ablation of lung neoplasms: a minimally invasive strategy for inoperable patients. J Am Coll Surg. 2002;195(3):426–430.
- Yamakado K, Hase S, Matsuoka T, et al. Radiofrequency ablation for the treatment of unresectable lung metastases in patients with colorectal cancer: a multicenter study in Japan. J Vasc Interv Radiol. 2007;18(3):393–398.
- Lu Q, Cao W, Huang L, et al. CT-guided percutaneous microwave ablation of pulmonary malignancies: results in 69 cases. World J Surg Oncol. 2012;10:80–80.
- Gobara H, Arai Y, Kobayashi T, et al. Percutaneous radiofrequency ablation for patients with malignant lung tumors: a phase II prospective multicenter study (JIVROSG-0702). Jpn J Radiol. 2016;34(8):556–563.
- Li X, Wang J, Li W, et al. Percutaneous CT-guided radiofrequency ablation for unresectable hepatocellular carcinoma pulmonary metastases. Int J Hyperthermia. 2012;28(8):721–728.
- He W, Hu XD, Wu DF, et al. Ultrasonography-guided percutaneous microwave ablation of peripheral lung cancer. Clin Imaging. 2006;30(4):234–241.
- Wang W, Liu W, Zhou J, et al. High intensity focused ultrasound treatment for symptomatic uterine fibroids: preliminary results. Zhonghua Chao Sheng Ying Xiang Xue Za Zhi. 2002;11:161–163.
- Ren XL, Zhou XD, Zhang J, et al. Extracorporeal ablation of uterine fibroids with high-intensity focused ultrasound: imaging and histopathologic evaluation. J Ultrasound Med. 2007;26(2):201–212.
- Ren XL, Zhou XD, Yan RL, et al. Sonographically guided extracorporeal ablation of uterine fibroids with high-intensity focused ultrasound: midterm results. J Ultrasound Med. 2009;28(1):100–103.
- Liu H, Zhang J, Han ZY, et al. Effectiveness of ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroids: a multicentre study in China. Int J Hyperthermia. 2016;32(8):876–880.
- Kim YS, Rhim H, Tae K, et al. Radiofrequency ablation of benign cold thyroid nodules: initial clinical experience. Thyroid. 2006;16(4):361–367.
- Feng B, Liang P, Cheng Z, et al. Ultrasound-guided percutaneous microwave ablation of benign thyroid nodules: experimental and clinical studies. Eur J Endocrinol. 2012;166(6):1031–1037.
- Yue W, Wang S, Yu S, et al. Ultrasound-guided percutaneous microwave ablation of solitary T1N0M0 papillary thyroid microcarcinoma: initial experience. Int J Hyperthermia. 2014;30(2):150–157.
- Teng D, Sui G, Liu C, et al. Long-term efficacy of ultrasound-guided low power microwave ablation for the treatment of primary papillary thyroid microcarcinoma: a 3-year follow-up study. J Cancer Res Clin Oncol. 2018;144(4):771–779.
- Turtulici G, Orlandi D, Corazza A, et al. Percutaneous radiofrequency ablation of benign thyroid nodules assisted by a virtual needle tracking system. Ultrasound Med Biol. 2014;40(7):1447–1452.
- Hong MJ, Baek JH, Choi YJ, et al. Radiofrequency ablation is a thyroid function-preserving treatment for patients with bilateral benign thyroid nodules. J Vasc Interv Radiol. 2015;26(1):55–61.
- Sung JY, Baek JH, Kim YS, et al. One-Step ethanol ablation of viscous cystic thyroid nodules. AJR Am J Roentgenol. 2008;191(6):1730–1733.
- Kim YJ, Baek JH, Ha EJ, et al. Cystic versus predominantly cystic thyroid nodules: efficacy of ethanol ablation and analysis of related factors. Eur Radiol. 2012;22(7):1573–1578.
- Sung JY, Baek JH, Kim KS, et al. Single-session treatment of benign cystic thyroid nodules with ethanol versus radiofrequency ablation: a prospective randomized study. Radiology. 2013;269(1):293–300.
- Baek JH, Ha EJ, Choi YJ, et al. Radiofrequency versus ethanol ablation for treating predominantly cystic thyroid nodules: a randomized clinical trial. Korean J Radiol. 2015;16(6):1332–1340.
- Wu F, Wang ZB, Zhu H, et al. Feasibility of US-guided high-intensity focused ultrasound treatment in patients with advanced pancreatic cancer: initial experience. Radiology. 2005;236(3):1034–1040.
- Yu J, Zhang X, Liu H, et al. Percutaneous microwave ablation versus laparoscopic partial nephrectomy for cT1a renal cell carcinoma: a propensity-matched cohort study of 1955 patients. Radiology. 2020;294(3):698–706.
- Lee DH, Kim JW, Lee JM, et al. Laparoscopic liver resection versus percutaneous radiofrequency ablation for small single nodular hepatocellular carcinoma: comparison of treatment outcomes. Liver Cancer. 2021;10(1):25–37.
- Lee DH, Lee JM, Kim PN, et al. Whole tumor ablation of locally recurred hepatocellular carcinoma including retained iodized oil after transarterial chemoembolization improves progression-free survival. Eur Radiol. 2019;29(9):5052–5062.
- Lee DH, Lee JM, Yu MH, et al. Non-hypervascular hepatobiliary phase hypointense nodules on gadoxetic acid-enhanced MR can help determine the treatment method for HCC. Eur Radiol. 2019;29(6):3122–3131.
- Ha EJ, Baek JH, Che Y, et al. Radiofrequency ablation of benign thyroid nodules: recommendations from the Asian conference on tumor ablation task force. Ultrasonography. 2021;40(1):75–82.
- Ju JX, Zeng QJ, Xu EJ, et al. Intraprocedural contrast-enhanced ultrasound-CT/MR fusion imaging assessment in HCC thermal ablation to reduce local tumor progression: compared with routine contrast-enhanced ultrasound. Int J Hyperthermia. 2019;36(1):785–793.
- Li K, Su Z, Xu E, et al. Evaluation of the ablation margin of hepatocellular carcinoma using CEUS-CT/MR image fusion in a phantom model and in patients. BMC Cancer. 2017;17(1):61–61.
- Numata K, Fukuda H, Morimoto M, et al. Use of fusion imaging combining contrast-enhanced ultrasonography with a perflubutane-based contrast agent and contrast-enhanced computed tomography for the evaluation of percutaneous radiofrequency ablation of hypervascular hepatocellular carcinoma. Eur J Radiol. 2012;81(10):2746–2753.
- Lee JY, Choi BI, Chung YE, et al. Clinical value of CT/MR-US fusion imaging for radiofrequency ablation of hepatic nodules. Eur J Radiol. 2012;81(9):2281–2289.
- Song KD, Lee MW, Rhim H, et al. Percutaneous US/MRI fusion-guided radiofrequency ablation for recurrent subcentimeter hepatocellular carcinoma: technical feasibility and therapeutic outcomes. Radiology. 2018;288(3):878–886.
- Minami Y, Minami T, Takita M, et al. Radiofrequency ablation for hepatocellular carcinoma: clinical value of ultrasound-ultrasound overlay fusion for optimal ablation and local controllability. Hepatol Res. 2020;50(1):67–74.
- Liu FY, Yu XL, Liang P, et al. Microwave ablation assisted by a real-time virtual navigation system for hepatocellular carcinoma undetectable by conventional ultrasonography. Eur J Radiol. 2012;81(7):1455–1459.
- Peng Z, Chen S, Wei M, et al. Advanced recurrent hepatocellular carcinoma: treatment with sorafenib alone or in combination with transarterial chemoembolization and radiofrequency ablation. Radiology. 2018;287(2):705–714.
- Zhu K, Huang J, Lai L, et al. Medium or large hepatocellular carcinoma: sorafenib combined with transarterial chemoembolization and radiofrequency ablation. Radiology. 2018;288(1):300–307.
- Yuan H, Lan Y, Li X, et al. Large hepatocellular carcinoma with local remnants after transarterial chemoembolization: treatment by sorafenib combined with radiofrequency ablation or sorafenib alone. Am J Cancer Res. 2019;9:791–799.
- Feng X, Xu R, Du X, et al. Combination therapy with sorafenib and radiofrequency ablation for BCLC stage 0-B1 hepatocellular carcinoma: a multicenter retrospective cohort study. Am J Gastroenterol. 2014;109(12):1891–1899.
- Weng DS, Zhou J, Zhou QM, et al. Minimally invasive treatment combined with cytokine-induced killer cells therapy lower the short-term recurrence rates of hepatocellular carcinomas. J. Immunother. 2008;31(1):63–71.
- Ma H, Zhang Y, Wang Q, et al. Therapeutic safety and effects of adjuvant autologous RetroNectin activated killer cell immunotherapy for patients with primary hepatocellular carcinoma after radiofrequency ablation. Cancer Biol Ther. 2010;9(11):903–907.
- Liang S, Niu L, Xu K, et al. Tumor cryoablation in combination with natural killer cells therapy and herceptin in patients with HER2-overexpressing recurrent breast cancer. Mol Immunol. 2017;92:45–53.
- Lin M, Liang S, Wang X, et al. Percutaneous irreversible electroporation combined with allogeneic natural killer cell immunotherapy for patients with unresectable (stage III/IV) pancreatic cancer: a promising treatment. J Cancer Res Clin Oncol. 2017;143(12):2607–2618.
- Lin M, Liang S, Wang X, et al. Short-term clinical efficacy of percutaneous irreversible electroporation combined with allogeneic natural killer cell for treating metastatic pancreatic cancer. Immunol Lett. 2017;186:20–27.
- Lin M, Liang SZ, Wang XH, et al. Clinical efficacy of percutaneous cryoablation combined with allogenic NK cell immunotherapy for advanced non-small cell lung cancer. Immunol Res. 2017;65(4):880–887.
- Lin M, Xu K, Liang S, et al. Prospective study of percutaneous cryoablation combined with allogenic NK cell immunotherapy for advanced renal cell cancer. Immunol Lett. 2017;184:98–104.
- Yang Y, Qin Z, Du D, et al. Safety and short-term efficacy of irreversible electroporation and allogenic natural killer cell immunotherapy combination in the treatment of patients with unresectable primary liver cancer. Cardiovasc Intervent Radiol. 2019;42(1):48–59.
- Zhou P, Liang P, Dong B, et al. Phase I clinical study of combination therapy with microwave ablation and cellular immunotherapy in hepatocellular carcinoma. Cancer Biol Ther. 2011;11(5):450–456.
- Yu MA, Liang P, Yu XL, et al. Multiple courses of immunotherapy with different immune cell types for patients with hepatocellular carcinoma after microwave ablation. Exp Ther Med. 2015;10(4):1460–1466.