Abstract
Background
High-intensity focused ultrasound (HIFU) is an important method for treating non-neoplastic epithelial disorders of the vulva (NNEDV), but the factors affecting the efficacy of HIFU for NNEDV treatment remain unclear.
Objective
To determine the factors influencing the clinical efficacy of HIFU in the treatment of NNEDV.
Methods
A retrospective observational study of 186 NNEDV patients treated with HIFU was performed to evaluate the therapeutic effect, and the relationship between treatment efficacy and clinicopathological factors was analyzed.
Results
NNEDV signs and symptoms were effectively improved and relieved after HIFU treatment. The total effective and recurrent rates were 95.16% and 4.52%, respectively. Younger patients with shorter disease courses, mild itching, or peri-vulvar lesions had better therapeutic effects, and patients with anxiety and/or depression had worse treatment outcomes.
Conclusion
The therapeutic effect of HIFU on NNEDV is not only related to the itching degree, age, or disease course but is also closely related to lesion location as well as anxiety and depression in patients.
Introduction
Non-neoplastic epithelial disorder of the vulva (NNEDV) is a common disease characterized with pigmentation and degeneration of the female mucosa and skin tissue of the vulva. It has been regarded as a ‘refractory disease’, with a prolonged disease course and severe symptoms. The symptoms can significantly affect the physical and mental health of patients, but its etiology and pathogenesis remain unclear. Although serval clinical treatments, including physiotherapy (such as microwave, frozen, and laser techniques), drugs (such as corticosteroids and herbal medications), and surgery, are available, the overall curative effect is poor and relapses are common. At present, there are many disputes about the choice of treatment, and the recognized ‘gold standard’ for treatment has not yet been established [Citation1]. High-intensity focused ultrasound (HIFU), as a new physiotherapy technique, has achieved remarkable results in the treatment of NNEDV. Many related studies have proved that HIFU is better than traditional drugs or treatment methods, and it has been favored by many patients and doctors. HIFU is favored for its short treatment course, quick effect, and noninvasive nature [Citation2]. However, in clinical observation, the effect of treatment varies greatly among different NNEDV patients receiving HIFU treatment. While current studies on HIFU have mostly focused on comparison between HIFU and other treatment options, only few studies have focused on factors affecting the therapeutic effects of HIFU. Such factors could include the lesion size and pathological type influencing the therapeutic effect of HIFU [Citation3,Citation4]. Therefore, it is necessary to conduct a study to clarify the relevant factors affecting the therapeutic effect. In this study, in addition to identifying the common factors affecting the therapeutic effect of HIFU in NNEDV patients, we also analyzed the relationship among lesion location and psychological factors, and prognosis. To the best of our knowledge, these relationships have not been reported in the literature to date.
Materials and methods
Patients and groups
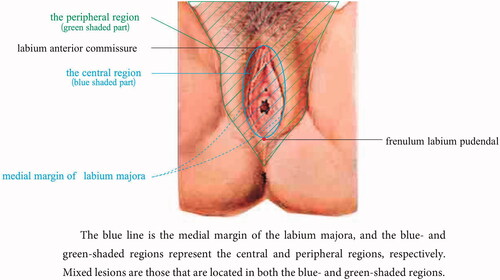
From January 2014 to June 2018, 186 patients with NNEDV, confirmed by pathological biopsy and treated with HIFU, were selected. Among them, 51 patients were diagnosed with lichen sclerosis of the vulva (LSV), 106 patients with lichen simplex chronicus (LSC), and 29 patients with lichen planus (LP). The mean age of these patients was 45.6 ± 11.0 years, and the median disease course was 5.7 ± 3.2 years. The anterior commissure of the labia and labia fourchette served as the top and bottom vertices and the medial margins of the left and right labia majora as the boundaries. The area between the boundaries was designated as the central region and the area outside the boundaries as the peripheral region (). The patients were divided into three groups according to the location of the lesions: central, peripheral, and mixed, with 15, 114, and 57 patients, respectively, in each group. In addition, patients were divided into two groups according to their depression and/or anxiety levels: 159 patients in the no or mild symptom group and 27 patients in the moderate or severe symptoms group. Patients with depression and anxiety were evaluated using the self-rating depression scale and self-rating anxiety scale when they received treatment. After evaluation, the patients were subsequently diagnosed and received intervention by a psychologist.
Exclusion criteria for patients were: (Citation1) vulvar intraepithelial neoplasia or vulvar cancer; (Citation2) serious heart, liver, or kidney diseases; (Citation3) severe diabetes; (Citation4) receiving other physical therapy within the past 3 months; and (Citation5) pregnancy, lactation, menstruation, and acute genital tract inflammation. This study strictly complied with the Helsinki Declaration and all patients provided written informed consent for clinical research. The research protocol for this retrospective study was assessed and approved by the Medical Ethics Committee at our institutes (IEC-LW022).
Methods
All patients were subjected to routine history data collection, gynecological examination, auxiliary examination, and vulvar biopsy to confirm the diagnosis of NNEDV before treatment. HIFU treatment was performed 3–7 days after menstruation and when the biopsy wound had healed. The bladder was emptied, and the skin was prepped preoperatively. Thereafter, all patients were treated with a model CZF-focused ultrasound therapeutic device developed by Chongqing Haifu Medical Technology Co., Ltd., Chongqing, China. Sacral anesthesia or combined spinal-epidural anesthesia was used for the treatment. The operating parameters were as follows: frequency was 9.5–10.5 MHz, power was 4–5 W, and pulse was 1000–1100 Hz. Using an ultrasonic coolant as the conduction medium, the ultrasound probe was placed close to the skin of the lesion. A consecutive scan was performed at a uniform speed of 3–5 mm/s on the lesion area and normal tissues located around 5 mm of that area. The scanning lasted for 10–40 min according to the size of the lesion until the treatment area showed swelling, mild congestion, hyperthermia, and the wrinkled area became smooth and flat. Immediately after treatment, ice bags were intermittently applied to the skin treatment area for 24–48 h, and burn cream was applied locally for a week to promote the regression of edema.
Evaluation of clinical efficacy
Clinical efficacy was graded according to changes in the degree of itching and signs of the local skin (elasticity, color, lesion size, and tissue structure) before and after treatment (). The therapeutic index score [Citation5] was obtained as follows: [(scores before the treatment – scores after treatment)/scores before treatment] × 100%. The results were as follows: (Citation1) cured (therapeutic index ≥ 90%): patients’ symptoms and signs had completely disappeared, skin color and elasticity of the diseased area became normal, (Citation2) effective (therapeutic index 21%–89%): symptoms such as vulva pruritus and causalgia decreased, vulva skin color and elasticity partially recovered, (Citation3) ineffective (therapeutic index ≤ 20%): persistence of vulval pruritus and no change in skin lesion, or such signs and symptoms recurred within 6 months after treatment, and (Citation4) recurrent symptoms and signs 6 months after treatment. Patients were followed up at 1 week, 1 month, 3 months, 6 months, and 12 months after treatment in the first year. Patients were then followed up once a year to observe and record the clinical efficacy and side effects.
Table 1. Grading of clinical effect for NNEDV.
Statistical analysis
The software package SPSS 25.0 (IBM Corp., Armonk, NY, USA) was used to process the data and analyze the response rate. A chi-square test was used to compare the differences among groups, and the variables with statistical significance were included in the sequential logistic regression model for multivariate effectiveness analysis. Statistical significance was set at p < 0.05.
Results
Therapeutic effect
Swelling and congestion appeared immediately in the lesion area after treatment. One week later, all edema subsided, and the itching symptoms of some patients resolved. With time, the symptoms and signs improved gradually. At 12 months after treatment, the skin color, elasticity, and tissue structure of the lesion area returned to normal in most patients. Among the 186 patients, the treatment was curative in 94 (50.54%), effective in 83 (44.62%), and ineffective in 9 (4.84%); the total effectiveness rate was 95.16%. During a two-year follow-up after treatment, recurrence was observed in eight (4.52%) patients of all the patients with effective treatment. Only 13 patients had mild skin burns, characterized by blisters and a few ulcers in the corresponding area.
Comparison of therapeutic effect among patients with different lesion locations
The difference in cure rates among patients with different lesion locations was statistically significant (χ2 = 35.71, p < 0.01). There was no significant difference in therapeutic effect between patients with central and mixed lesions (χ2 = 0.06, p > 0.05). The discrepancy between peripheral patients and central and mixed patients was statistically significant (χ2 = 7.69, p < 0.01; χ2=17.84, p < 0.01) ().
Table 2. The effectiveness of HIFU treatment for NNEVD.
Comparison of the therapeutic effect on patients with different itching degrees
The cure rate among patients with different itching degrees was statistically significant (χ2=41.97, p < 0.01). There were significant differences in therapeutic effect when comparing score 1 patients with score 2 and 3 patients (χ2=8.68, p < 0.01;χ2=33.96, p < 0.01). A similar conclusion was obtained from the comparison between score 2 patients and score 3 patients (χ2=21.72, p < 0.01) ().
Comparison of therapeutic effect among patients with different ages
The difference in cure rates between the different age groups was statistically significant (χ2 = 10.91, p < 0.05). There was no significant difference in therapeutic effect between the age groups of 21-35 and 36-50 years (χ2 = 0.49, p > 0.05). The difference in therapeutic effect between the age groups of 21–35 and 51–66 years was statistically significant (χ2 = 6.79, p < 0.01), as was difference between the age groups of 36–50 and 51–66 years (χ2 = 7.29, p < 0.01) ().
Comparison of the therapeutic effect on patients with different disease courses
There were significant differences in the cure rates among the different treatment groups (χ2 = 21.04, p < 0.01). The cure rates in the <3 years of disease course group and the 3-10 years of disease course group were significantly higher than that in the >10 years of disease course group (χ2 = 8.16, p < 0.01; χ2 = 7.26, p < 0.01). There was no significant difference in cure rates between the <3 years of disease course group and the 3–10 years of disease course group (χ2 = 0.79, p > 0.05) ().
Comparison of therapeutic effect among different pathological types of NNEDV
There were significant differences in the cure rates among different pathological types (χ2=10.44, p < 0.05), where the cure rate of LSC was higher than that of LSV. However, there was no significant difference in the effective and total effective rates among the three groups (p > 0.05) ().
Comparison of therapeutic effect among patients with different levels of anxiety and/or depression
The differences in cure and effectiveness rates between patients with different levels of anxiety and/or depression were significant (χ2=16.12, p < 0.01;χ2=11.81, p < 0.01) (). In the normal or mild group (159 patients, in which 21 patients with mild psychiatric symptoms), 14 patients with mild psychiatric symptoms showed a marked improvement after HIFU treatment. In the moderate or severe group (27 patients, in which 8 patients with severe psychiatric symptoms), the psychiatric symptoms improved or disappeared after HIFU treatment in 16 patients. There was no significant difference in the improvement of psychiatric symptoms between the two groups (χ2=0.28, p > 0.05).
Multivariant analysis of treatment effectiveness
Except for pathological type, the logistic regression multivariant analysis showed that disease course, itching degree, age, lesion location, anxiety, and depression levels were prognostic factors for effectiveness ().
Table 3. Multi-variant analysis of the effectiveness of HIFU treatment for NNEDV.
Discussion
At present, various clinical non-surgical treatments can partially alleviate symptoms, but the overall effect of such treatment is poor. The recurrence rate of patients undergoing surgery is as high at 50%. Scar contracture after surgery may cause pain and sexual difficulties, which have a great impact on the physical and mental health of patients [Citation6,Citation7]. In this context, HIFU, as an emerging physiotherapy technique, has been gradually applied to the treatment of NNEDV. It has been observed that because of its good tissue penetration and energy deposition, HIFU can improve local microcirculation; contribute to angiogenesis; promote the regeneration and repair of healthy tissue and the reconstruction of epidermis from deep to shallow; and gradually restore the color, shape, elasticity, and function of diseased tissues [Citation8]. In addition, HIFU has the advantages of low invasiveness, good safety, high effectiveness, and reusability. Therefore, it has been recognized and accepted by medical institutions worldwide, showing a tendency to gradually replace other treatment options [Citation9,Citation10]. Therefore, it is of great clinical significance to explore the factors influencing the therapeutic effect of HIFU treatment.
In this study, the total effectiveness and recurrence rates were 95.16% and 4.52%, respectively, and it was found that different disease courses or itching degrees had different therapeutic effects. The longer the course of the disease, the more severe the itching and the worse the efficacy. This conclusion is consistent with the findings of Ye et al. [Citation4]. The reason may be that the local skin structure is damaged or changed after repeated scratching due to the long course of the disease or severe itching. Consequently, during HIFU treatment, energy easily accumulates in the local area, which causes tissue damage and reduces the treatment effect [Citation11]. In addition, the prognosis of patients is closely related to their age. Under the same conditions, the younger the patient, the better the treatment effect, possibly because the healing and regeneration ability of the skin gradually decreases as the patient's age increases. and there are differences in the capacity of the skin for absorbing ultrasound in patients of different ages. The damaged skin of young patients has significant capacity for regeneration and healing, and the disease is easily controlled and reversed. Therefore, adolescent patients have the possibility of self-healing, and most of them do not require excessive treatment. However, timely and early diagnosis and intervention can avoid irreversible changes and increase the probability of self-healing [Citation11].
Our study also found that there were significant differences in the curative effects according to different lesion locations. We creatively proposed the concepts of central and peripheral regions and divided the lesions into three types: central, peripheral, and mixed. The results showed that the cure rate of patients with peripheral lesions was significantly higher than that of patients with central region or mixed lesions. This may be because the central area of the vulva, which mainly consists of the labia minora, clitoris, and pronaus, cannot be effectively flattened or fixed during treatment because of the irregular shapes and structures. Therefore, the ultrasound probe cannot be effectively scanned at a uniform speed close to the diseased skin, and the final treatment effect was discounted.
Due to the unclear etiology of the disease, the long duration of the disease, and the lack of specific treatment, most patients experience long-term mental stress, accompanied by sleep and sexual disorders [Citation12]. In addition, patients may feel uncomfortable discussing such gynecological issues. It is easy for patients to develop negative emotions such as irritability, anxiety, and depression. Some scholars have reported that the incidence of anxiety or depression in patients with NNEDV is significantly higher than that in a control group [Citation13]. This suggests that in the process of treatment of NNEDV, the physical symptoms of patients should be improved as well as their adverse psychological problems should be treated. Most previous studies have reported that anxiety and depression resulted from NNEDV, but our study found that the cure rate of patients with anxiety and/or depression was significantly lower than that of patients with mild or no anxiety/depression. This indicated that anxiety and/or depression are closely related to the treatment effect of HIFU. The more anxiety and/or depression, the worse the treatment effect.
Therefore, this study suggests that clinicians should not ignore the impact of psychological factors on NNEDV treatment and should follow the model of bio-psycho-social medicine. While providing biological treatment to patients, they should also implement systematic psychotherapy and health education synchronously. Such treatments should include explaining relevant knowledge of NNEDV to increase patients’ confidence in treatment, care for patients, aid to adjust and relax their mood, timely psychological intervention, and anxiolytic and antidepressant prescription, if necessary.
This study had some limitations. One is that the follow-up time was relatively short; therefore, it needs to be extended in further research. Moreover, there are many factors that affect the therapeutic effect on patients, such as equipment parameters, operator manipulation and experience, and anesthetic methods, which need to be further summarized and discussed for clinical use in the future.
Conclusion
The therapeutic effect of HIFU on NNEDV is not only related to the degree of itch, age, and course of the disease, but is also closely related to the location of lesions, anxiety, and depression levels in patients.
Ethical approval
This study was approved by the ethics committee at Maternal and Child Health Hospital of Hubei Province.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Zhang L, Zhang W, Orsi F, et al. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: a review of safety and efficacy. Int J Hyperthermia. 2015;31(3):280–284.
- Zhou W, Zhu L, Zhou H, et al. The efficacy of high-intensity, focused ultrasound treatment for non-neoplastic epithelial disorders of the vulva. Cell Mol Biol (Noisy-le-Grand). 2016;62:111–115.
- Wu C, Zou M, Xiong Y, et al. Short- and long-term efficacy of focused ultrasound therapy for non-neoplastic epithelial disorders of the vulva. BJOG: Int J Obstet Gy. 2017;124 (Suppl 3):87–92.
- Ye M, Deng X, Mao S, et al. High intensity focused ultrasound treatment for non-neoplastic epithelial disorders of the vulva: Factors affecting effectiveness and recurrence. Int J Hyperthermia. 2015;31(7):771–776.
- Li C, Bian D, Chen W, et al. Focused ultrasoundtherapy of vulvar dystrophies: a feasibility study. Obstet Gynecol. 2004;104(5 Pt 1):915–921.
- Brodrick B, Belkin ZR, Goldstein AT. Influence of treatments on prognosis for vulvar lichen sclerosus: facts and controversies. Clin Dermatol. 2013;31(6):780–786.
- Madeleine MM, Johnson LG, Doody DR, et al. Natural antibodies to human papillomavirus 16 and recurrence of vulvar High-Grade intraepithelial neoplasia (VIN3). J Low Genit Tract Dis. 2016;20(3):257–260.
- Wallbillich JJ, Rhodes HE, Milbourne AM, et al. Vulvar intraepithelial neoplasia (VIN 2/3): comparing clinical outcomes and evaluating risk factors for recurrence. Gynecol Oncol. 2012;127(2):312–315.
- Shi HH, Zhu L, Yang Y, et al. Multicenter randomized clinical study of high-intensity focused ultrasound and cortical hormone in the treatment of non-neoplastic epithelial disorders of vulva. Zhonghua Yi Xue Za Zhi. 2013;93(41):3291–3293.
- Zhong X, Zhang M, Tian Z, et al. The study of enhanced high-intensity focused ultrasound therapy by sonodynamic N2O microbubbles. Nanoscale Res Lett. 2019;14(1):381.
- Nerantzoulis I, Grigoriadis T, Michala L. Genital lichen sclerosus in childhood and adolescence-a retrospective case series of 15 patients: early diagnosis is crucial to avoid long-term sequelae. Eur J Pediatr. 2017;176(10):1429–1432.
- Günthert AR, Duclos K, Jahns BG, et al. Clinical scoring system for vulvar lichen sclerosus. J Sex Med. 2012;9(9):2342–2350.
- Brauer M, van Lunsen RH, Laan ET, et al. A qualitative study on experiences after vulvar surgery in women with lichen sclerosus and sexual pain. J Sex Med. 2016;13(7):1080–1090.