Abstract
Purpose
To explore the clinical outcomes and safety of ultrasound-guided microwave ablation (MWA) for treating thyroid benign solid nodules during a three-year follow-up.
Methods
A total of 53 patients with thyroid benign solid nodules with the largest diameter exceeding 2 cm were treated with US-guided MWA between January 2015 and December 2017. Nodule volume, the cosmetic score, and the symptom scores were evaluated before ablation and 1, 2, and 3 years after the operation. The characteristics of MWA and complications were also evaluated.
Results
The thyroid nodule volume at each time point after ablation was significantly smaller than that before ablation (p < .05). The Symptom and Cosmetics score were significantly improved (p < .05). Hoarseness was the major complication, with an incidence of 1.89%. The original nodules volume was 7.28 ± 11.42 mL; the isolating fluid was 34.36 ± 13.35 mL; the ablation time was 188.77 ± 89.13s.
Conclusions
MMA is an effective and safe approach for reducing nodule volume and symptoms in patients with benign thyroid solid nodules.
Background
Thyroid nodules (TNs) are a mass of thyroid tissue, solid- or fluid-filled lumps that form within a thyroid after the abnormal proliferation of thyroid cells. With the application and promotion of ultrasound diagnostic technology, the detection rate of TNS has drastically increased. Most patients are detected with benign nodules [Citation1–2] that usually do not require special treatment [Citation3]. Yet, this type of TNs lumps can cause local pressure symptoms such as choking or dull pain or cosmetic concerns, which may require additional treatment [Citation4]. Symptomatic TNs are often resolved surgically; however, some patients reject surgery due to scar formation and large trauma.
Ultrasound (US)-guided thermal ablation (TA) is a minimally invasive and fast approach and a good alternative to surgery for those concerned about scar formation and large trauma. Thermal ablation of benign TNs is also used in clinical practice. According to the 2020 European Thyroid Association Clinical Practice Guideline for the Use of Image-Guided Ablation in Benign Thyroid Nodules, TA should be mainly considered for patients with nodules with a maximum diameter ≥30 mm that keep growing steadily during US follow-up and who start complaining of local discomfort [Citation5]. Papini et al. also suggested that progressive growth of benign thyroid lesions that reach 12 mL was especially suited for minimally invasive procedures [Citation6]. Nevertheless, defining a nodule volume cutoff is not straightforward because symptoms and cosmetic problems are influenced by the location of the thyroid lesions and the cervical circumference, in addition to factors that cannot be objectively assessed. In the reports, radiofrequency ablation has been widely used [Citation2,Citation7–10] and has achieved positive results, even with proven of long-term efficacy [Citation3,Citation11], while there were few reports of the long-term follow-up results of microwave ablation (MWA) of benign TNs, especially for benign solid nodules.
In this study, we retrospectively evaluated the clinical outcomes of MWA for patients with thyroid benign solid nodules (TBSNs) over a three-year follow-up in our hospital and provided evidence to select a better and more appropriate device for ablation of TBSNs for clinicians or patients.
Materials and methods
Participants
A total of 53 patients with thyroid nodules were treated with US-guided MWA at the department of ultrasound of Beijing Friendship Hospital between January 2015 and December 2017.
All patients were selected with the following inclusion criteria: (1) reported pressure symptoms and/or cosmetic problems; (2) with only one nodule in the thyroid gland; (3) largest diameter of solid nodule > 2 cm; (4) confirmation of benignancy with repeated fine-needle aspiration (FNA) cytology; (5) serum thyroid hormone and thyrotropin levels within normal ranges; (6) patient underwent one-time MWA treatment. The exclusion criteria were: (1) substernal nodules or nodules that were difficult to monitor during the MWA procedure; (2) serious coagulopathy; (3) pregnancy.; (4) patients with incomplete imaging data or follow-up time < 36 months.
All patients were informed of the pros and cons of MWA and signed informed consent. The study was approved by Medical Ethics Committee of Beijing Friendship Hospital, Capital Medical University (2015-P2-021-01).
Pretreatment assessment
All patients were evaluated by US examination, FNA, laboratory, and clinical examinations.
US data
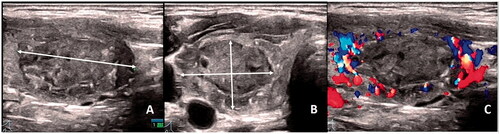
US, US-guided FNA, and MWA were performed using a 5 to 18-MHz linear matrix transducer and a real-time ultrasound system (Ascendus Color Doppler Ultrasound Diagnostic, Hitachi Medical Systems, Tokyo, Japan). Each thyroid nodule was measured (), and the volume of each nodule was calculated according to the following formula: V = π × (a × b × c)/6, where V is the volume, (a) the largest diameter, (b) and (c) the two other perpendicular diameters. The nodule location and the blood flow were also identified () and classified using a four-point scale. They were benign (Bethesda class II) at two consecutive cytological assessments performed [Citation5].
Figure 1. Ultrasonographic measurement and color Doppler sonography of thyroid solid nodule. Ultrasonography of a 28-year-old woman with solid nodules in the right lobe of the thyroid gland. (A) Solid nodule in the right lobe of the thyroid; the length diameter of the nodules was measured in the longitudinal section. (B) The left and right diameters and anteroposterior diameters of the nodules were measured in cross section. (C) Color Doppler sonography of solid thyroid nodules.
Laboratory examinations
Laboratory examinations included the levels of thyroid-stimulating hormone (TSH), thyrotropin, free triiodothyronine (FT3), and free thyroxin (FT4); blood routine examination; and coagulation time determination.
Symptom and cosmetic scores
Symptom and cosmetic scores were assessed by the physician, as described in a previous consensus statement [Citation12].
MWA procedure
MWA was performed in an outpatient setting by an experienced physician [Citation13–14], Microwave therapeutic equipment (KY-2000; Kangyou Medical, Nanjing, China) was used to administer microwave energy at a frequency of 2450 MHz. The microwave generator can produce up to 100 W of power (only 30 W power was used in this research) with an antenna diameter of 2 mm, a total length of 100 mm, and a transmit segment length of 5 mm.
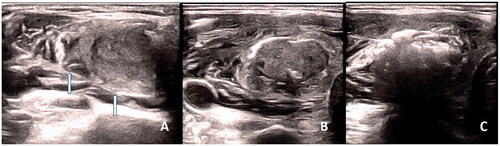
Briefly, patients were placed in the supine position with their necks fully exposed. Based on our experience, we recommend lateral cervical approach (LCA) and ‘water- isolation’ technology. Before ablation, isolation fluid was injected into three sides of the thyroid gland lobes to protect the parathyroid tissues (). It was recommended that the width of the isolation band should be > 0.5 cm, and the width should be kept unchanged during the operation. The mobile ablation method was then applied. The tip of the antenna was kept inside the nodule and could touch the nodule edge when ablating the edge of the nodule. When the transient hyper-echoic bubbles completely covered all conceptual units of thyroid nodule (), the ablation was terminated. The patient’s voice was monitored during the operation, and the procedure was halted if dysphonia occurred. During ablation, the thyroid nodules could also be tilted away from the recurrent laryngeal nerve according to the lever principle.
Figure 2. Ablation of a benign solid thyroid nodule. (A) Isolation fluid was injected into the posterior margin of the thyroid, where the nodule was located, to increase the distance between the thyroid and the recurrent laryngeal nerve. (B) Isolation fluid was injected into three sides of the right thyroid lobe where the nodule was located, like an ‘island’. (C) A solid nodule in the right lobe of the thyroid was filled with ablation hyper echo after complete ablation.
Follow-up evaluation
Postprocedural follow-up was carried out at 1, 2, and 3 years after treatment. At each follow-up, US examination, thyroid serum tests, and symptoms/cosmetics scores were performed, and VRR of the treated nodule was calculated based on the formula: VRR = [(initial volume – final volume) × 100%]/initial volume. Complications of MWA were also assessed.
Statistical analysis
Data were analyzed using Excel for Windows, and Statistical analysis was performed using SPSS version 22. Continuous variables were presented as mean ± SD or median (interquartile range), and categorical variables were presented as frequencies. T-Test (for normal distribution data) or Mann–Whitney U-test (for skewed data) was used to compare numerical data, and chi-square analysis was used to compare categorical data. A p-value <.05 was considered statistically significant.
Results
General data
The baseline characteristics of the thyroid nodules are summarized in . A total of 53 patients with thyroid nodules underwent MWA. There were 13 male and 40 female patients with an average age of 48.92 ± 12.43 years.
Table 1. The baseline characteristics of the thyroid nodules.
The outcomes of treatment
At the end of follow-up, the therapeutic success rate (a reduction of more than 50% in nodule volume after ablation was considered as a successful treatment) was 96.22% (51/53), and the complete disappearance rate was 18.8% (10/53).
Nodule volume and VRR
The thyroid nodule volume at each time point of follow-up after ablation was significantly smaller than that before ablation (p < .05), and the difference between the volume at 2 years and that at 1 year was statistically significant (p < .05), while the difference between the volume at 3 years and that at 2 years was not statistically significant (p > .05) (). The mean ± SD of VRRs at 1, 2, and 3 years follow-up was 72.15 ± 22.01%, 83.40 ± 21.07%, 84.64 ± 18.11%, respectively ().
Table 2. Nodule volume and VRR of thyroid benign solid nodules 1, 2, and 3 years after ablation.
Symptom score and cosmetics score
The Symptom score and Cosmetics score were significantly reduced at 1 year and were stable at 3 years post operation (p < .05) ().
Table 3. The Symptom score and Cosmetics score at 1, 2, and 3 years after ablation.
Complications and safety
All of the complications and side effects were summarized. Hoarseness resulted as a serious complication following the operation, having an incidence of 1.89%. The incidence of minor complications such as pain, neck swelling, and fever was 60.38%, 49.06%, and 1.89%, respectively. No patients experienced a life-threatening or delayed complication during follow-up ().
Table 4. Complications and side effects after WMA.
Characteristics of ablation
The preoperative volume of the nodule was 7.28 ± 11.42 mL, the volume of the intraoperative isolation fluid was 38.23 ± 29.65 mL, and the ablation time was 188.77 ± 89.13 s ().
Table 5. Characteristics of ablation.
Comparison of factors between different TNs volumes after ablation
(1) All nodules were divided into three groups (<10mL, 10–30 mL, >30mL) according to the TNs volumes before ablation (). The VRR of nodules was 71.03%, 72.19%, and 72.86% in group with <10mL, group with 10–30 mL, and group with >30mL, respectively, without statistical difference.
Table 6. Comparison of factors between different TNs volumes after ablation.
(2) The median delivered energy per volume in the nodules group with <10mL, group with 10–30 mL, and group with >30mL was 971.61 J/mL, 892.90 J/mL, 751.15 J/mL, respectively, without statistical difference.
Discussion
The thyroid gland is an essential organ of the human body that regulates and controls normal life activities. Surgical excision is the standard treatment procedure for benign thyroid nodules. TA can reduce complications after surgical thyroidectomy, including lifelong thyroxine replacement therapy, neck tissue adhesion, and scarring.
Compared with other thermal ablation, microwave treatment can produce higher temperatures, a larger ablation region in a short time and the ablation region is larger and more stable [Citation15–16]. To ensure that local nodules in situ are inactivated, corresponding measures need to be applied to guarantee the operation safety. For example, cool saline should be administrated to prevent thermal damage to surrounding tissues. Previous studies have recommended MWA with LCA and ‘water-isolated’ technique to treat benign solid nodules, even previous research believed that LCA and ‘water-isolated’ technique could reduce the complication rate of MWA surgery [Citation17]. MWA of benign thyroid nodules may lead to increased stress symptoms and cosmetic problems in patients with moderate or large nodules. Many short- and medium-term studies have reported on the stable improvement until the end of the study period [Citation18–20]. In this study, the outcomes of three years after ablation (even a few cases were followed up to 4–5 years, which were not analyzed due to the small number of cases and incomplete data) have been analyzed and summarized. We found a significant improvement in symptoms, cosmetic procedures and nodule volumes. In addition, the VRR after two years of follow-up were larger than 70% and remained stable until the end of the study period (3 years after the operation) just like RFA for the treatment of benign thyroid nodules in the report [Citation3].
In this study, all the nodules were ablated one time, and the size of the nodules significantly decreased in two years of follow-up, but not significantly at three years. There were even two cases with striated blood flow signals at the edge of the nodules, which suggested that some large nodules could be ablated again after two years if necessary.
The most common complication in this study was a sense of swelling in the neck caused by the ‘water-isolation’ which was a limitation of this method; yet, the symptom disappeared within 24 h after surgery, without affecting the patients' health. Another complication was hoarseness, which occurred in only one case with an incidence of 1.88%. In this case, the size of the nodule was about 7.0 × 6.4 × 3.5 cm, and the inferior margin of the nodule reached behind the sternum. Due to its large volume, the distance between the nodules and the recurrent laryngeal nerve was difficult to be separated by ‘water-isolation’, and due to the large volume, the patient had difficulty swallowing. However, the patient was resistant to surgical resection, so the surgeon decided to perform ablation after careful evaluation. One year later, the nodule volume was reduced by 77.55%, and the symptoms were significantly relieved. Postoperative fever was also a common complication, and there was only one case in this study, which occurred in the above patient. No further complications, such as bleeding, were found in this study.
This study has a few limitations. This was a single-center retrospective study with small sample size. Moreover, this approach has not been widely carried out in clinical practice as it requires surgeons to have a clear understanding of thyroid anatomy and skilled operation.
Conclusion
MWA is an effective minimally invasive option for reducing nodule size and symptoms in patients with benign solid thyroid nodules without the risks associated with surgery. However, multi-center research with a larger sample size needs to be carried out to further confirm these findings.
Informed consent statement
Informed consent was obtained from all the study participants.
Acknowledgments
Thanks are due to Junfeng Zhao, Linxue Qian, Yujiang Liu, Xiaoqu Tan for assistance with the study and valuable discussion.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Availability of data and materials
The data set supporting the results of this article are included within the article.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Moon WJ, Baek JH, Jung SL, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011;12(1):1–14.
- Cesareo R, Manfrini S, Pasqualini V, et al. Laser ablation versus radiofrequency ablation for thyroid nodules: 12-month results of a randomized trial (Lara II study). J Clin Endocrinol Metab. 2021;106(6):1692–1701.
- Bernardi S, Giudici F, Cesareo R, et al. Five-year results of radiofrequency and laser ablation of benign thyroid nodules: a multicenter study from the Italian minimally invasive treatments of the thyroid group. Thyroid. 2020;30(12):1759–1770.
- Shin JH, Baek JH, Ha EJ, et al. Radiofrequency ablation of thyroid nodules: basic principles and clinical application. Int J Endocrinol. 2012;2012:919650.
- Papini E, Monpeyssen H, Frasoldati A, et al. 2020 European thyroid association clinical practice guideline for the use of image-guided ablation in benign thyroid nodules. Eur Thyroid J. 2020;9(4):172–185.
- Papini E, Pacella CM, Hegedus L. Diagnosis of endocrine disease: thyroid ultrasound (US) and US-assisted procedures: from the shadows into an array of applications. Eur J Endocrinol. 2014;170(4):R133–R146.
- Yao Z, Wu T, Zheng B, et al. A novel strategy for single-session ultrasound-guided radiofrequency ablation of large benign thyroid nodules: a pilot cohort study. Front Endocrinol. 2020;11:560508.
- Bernardi S, Stacul F, Michelli A, et al. 12-month efficacy of a single radiofrequency ablation on autonomously functioning thyroid nodules. Endocrine. 2017;57(3):402–408.
- Jung SL, Baek JH, Lee JH, et al. Efficacy and safety of radiofrequency ablation for benign thyroid nodules: a prospective multicenter study. Korean J Radiol. 2018;19(1):167–174.
- Cesareo R, Pacella CM, Pasqualini V, et al. Laser ablation versus radiofrequency ablation for benign non-functioning thyroid nodules: six-month results of a randomized, parallel, open-label, trial (Lara trial). Thyroid. 2020;30:847–856.
- Deandrea M, Trimboli P, Garino F, et al. Long-term efficacy of a single session of rfa for benign thyroid nodules: a longitudinal 5-year observational study. J Clin Endocrinol Metab. 2019;104(9):3751–3756.
- Na DG, Lee JH, Jung SL, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012;13(2):117–125.
- Zhao J, Qian L, Zu Y, et al. Efficacy of ablation therapy for secondary hyperparathyroidism by ultrasound guided percutaneous thermoablation. Ultrasound Med Biol. 2016;42(5):1058–1065.
- Liu YJ, Qian LX, Liu D, et al. Ultrasound-guided microwave ablation in the treatment of benign thyroid nodules in 435 patients. Exp Biol Med. 2017;242:1515–1523.
- Morelli F, Sacrini A, Pompili G, et al. Microwave ablation for thyroid nodules: a new string to the bow for percutaneous treatments? Gland Surg. 2016;5(6):553–558.
- Klebe J, Happel C, Grünwald F, et al. Visualization of tissue alterations in thyroid nodules after microwave ablation: sonographic versus scintigraphic imaging. Nucl Med Commun. 2015;36(3):260–267.
- Yue W-W, Wang S-R, Lu F, et al. Radiofrequency ablation vs. microwave ablation for patients with benign thyroid nodules: a propensity score matching study. Endocrine. 2017;55(2):485–495.
- Wu W, Gong X, Zhou Q, et al. US-guided percutaneous microwave ablation for the treatment of benign thyroid nodules. Endocr J. 2017;64(11):1079–1085.
- Hu K, Wu J, Dong Y, et al. Comparison between ultrasound-guided percutaneous radiofrequency and microwave ablation in benign thyroid nodules. J Cancer Res Ther. 2019;15(7):1535–1540.
- Yue W, Wang S, Wang B, et al. Ultrasound guided percutaneous microwave ablation of benign thyroid nodules: safety and imaging follow-up in 222 patients. Eur J Radiol. 2013;82(1):e11–e16.
