Abstract
Background
Percutaneous, ultrasound-guided laser ablation is a proven management approach for the treatment of Benign Thyroid Nodules (BTN), but only sporadic cases of treatment of large-volume nodules with laser ablation have been reported. The aim of this study was to evaluate the efficacy and safety of laser ablation in the treatment of very large (> 100 mL) thyroid nodules.
Methods
Between 2009 and 2016, 24 patients with very large, BTN received 2–3 sessions of laser ablation over the course of 12 months. Nodule volume was measured before treatment, and at 1 and 4 years.
Results
Prior to treatment, median nodule volume was 138 mL (range: 102–289 mL). At 1 year, technique efficacy was achieved in 75% of patients, with median nodule volume significantly reduced to 26 mL (range: 15–31 mL, p < 0.001 vs pretreatment). Volume reduction ratio (VRR) at 1 year was 81%. At 4-year follow-up, median nodule volume was 27 mL (range: 15–33 mL, p < 0.001 vs pretreatment), with a VRR of 80%. Two patients had nodule regrowth > 50% and went to surgery – one patient after 1 year and the other after 3 years. Treatment was well tolerated; there were no major complications, although transient fever occurred in 12% (3/24) of patients and mild-to-moderate pain was experienced by 8% (2/24) of patients.
Conclusions
In this patient series, percutaneous, ultrasound-guided laser ablation of very large thyroid modules provided long-term benefits and the treatment was well tolerated.
Introduction
Percutaneous, ultrasound (US)-guided laser ablation has become a proven management approach for the treatment of Benign Thyroid Nodules (BTN) and is acknowledged as such in recent management guidelines [Citation1–3]. This position reflects a growing evidence base gained over more than 20 years [Citation4,Citation5], with data obtained from randomized clinical trials, and prospective and retrospective studies [Citation6]. Laser ablation is the first of a range of image-guided thermal ablation techniques for thyroid-nodule treatment, which also includes radiofrequency ablation, microwave ablation, and high-intensity focused ultrasound (HIFU) ablation [Citation6].
In the literature, sporadic cases of treatment of large-volume nodules with laser ablation have been reported. For example, in the largest retrospective, multicenter evaluation of laser ablation that evaluated more than 1,500 nodules, the largest nodule volume treated was 216 mL; however, the mean ± SD nodule volume at baseline was 27 ± 24 mL, indicating an overall study population with relatively moderate nodule volumes [Citation7]. Similarly, in randomized clinical trials of laser ablation [Citation8–12], the mean baseline thyroid-nodule volume has ranged from 8.2 mL (largest nodule = 26.9 mL) [Citation8] to 24.7 ± 24 mL [Citation12], indicating study populations with predominantly small or medium-sized nodules.
To our knowledge, there are no published studies that have evaluated laser ablation specifically in a cohort of patients with very large nodules. Here, we report the results from 4 years of follow-up of a cohort of patients with very large BTN (defined in this study as a nodule volume > 100 mL) who underwent two or three sessions of ultrasound-guided laser ablation of a single nodule. In this retrospective study, conducted between January 2009 and December 2016, 24 subjects with nodules ranging in volume from 102 to 289 mL who underwent laser ablation were evaluated.
Materials and methods
This study was approved by the local ethics committee (protocol number: 102009) and fully informed consent was obtained in writing from all the subjects who met the inclusion criteria. Enrolled subjects had a high operative risk or had refused surgery. The inclusion criteria for this retrospective study were as follows: diagnosis of benignity obtained through fine-needle aspiration biopsy, solid nodule > 100 mL, normal levels of thyroid stimulating hormone (TSH), free triiodothyronine (FT3), and free thyroxine (FT4), negative anti-TSH receptor antibodies, negative anti-thyroperoxidase and anti-thyroglobulin antibodies, normal calcitonin levels, the presence of local compressive symptoms combined with the refusal of surgery or surgical ineligibility.
Between January 2009 and December 2016, 24 patients received outpatient laser-ablation treatment at Azienda Ospedaliero-Universitaria, Perugia. Percutaneous laser ablation was performed under sterile conditions, and US guidance was performed as described by Pacella et al. [Citation5], without anesthesia or sedation as we used the symptom of pain or burning as a guide to eventually stop or reduce energy delivery [Citation13]. Fourteen of these patients have previously been reported as part of a large multicenter study [Citation7].
Patients were treated via a 1064 nm continuous-wave laser (EchoLaser ModìLiteTM, Elesta, Calenzano, Florence, Italy) as recently described [Citation14], with the exception that each patient received a course of treatment of two or three sessions of laser ablation, and it was planned that each session would be performed using 2–4 fibers, according to the volume of the nodule. The number of illuminations carried out per treatment depended on the initial volume of the nodule, heat diffusion, and compliance of the patient. The EchoLaser system is an integrated device that consists of an ultrasound machine (MyLab70XVG, Esaote, Genova, Italy) and a multisource laser device (Echolaser x4, Elesta SpA, Calenzano). The planning of the treatment, the insertion of the needles/fibers and the monitoring are all carried out under ultrasound guidance. To facilitate the insertion maneuver, the system has a dedicated multi-applicator Guiding System for specific probes with related PLA (Percutaneous Laser Ablation) software in the ultrasound scanner. This software displays the guidelines on the screen and a graphical representation of the safety distance area that takes into account the safety distance to maintain from the fiber tip to the capsule and vital structures. To avoid complications, the fiber tip is positioned according to the graphical representation of the Planning Software, which assures a safety distance of at least 10 mm laterally and 15 mm frontally from the vital structures of the neck (blood vessels, recurrent laryngeal nerve, trachea, and esophagus). Once the introducer needles are inserted in the target tissue, an optical fiber is introduced into each needle with its tip protruding 5 mm from the needle tip to be in contact with thyroid nodule tissue.
The minimum interval between one session of laser ablation and the next was 6 months. This interval was chosen because the definitive results, in terms of volume reduction, are obtained after 6 months from the laser ablative treatment [Citation13,Citation15]. For each patient, the decision to use two or three sessions was governed by the persistence of compressive symptoms, i.e., the third session of laser ablation was administered if the patient still had compressive symptoms after receiving their second session.
Compressive symptoms and cosmetic effects were evaluated at day 0 and after 1, 6, 12, 24 and 36 months. Compressions were assessed using a 4-point scale: 0 = asymptomatic; 1 = mild pressure complaint; 2 = neck constraint; 3 = neck constraint with swallowing difficulty [Citation16]. After clinical and US control, patients were asked to complete a structured visual analog questionnaire concerning treatment tolerability. Periprocedural pain was scored from 1 (absence of pain) to 10 (intolerable pain) [Citation9]. The complications and side-effects, as well as the terminology used, were evaluated in agreement with the International Working Group on Image-Guided Tumor Ablation [Citation17] and the Technology Assessment Committee of the Society of Interventional Radiology [Citation18].
Nodule volume was calculated using the ellipsoid formula [Citation19] before treatment and at 1 and 4 years. Volume reduction ratio (VRR) – the percentage reduction in nodule volume – was calculated with the following equation: VRR = [(initial volume – final volume)/initial volume × 100]. Technique efficacy was defined as a volume reduction ≥ 50% at a 1-year follow-up [Citation20]. Statistical analyses were performed using SPSS version 22.0 (SPSS, Chicago, IL). Quantitative variables are reported as median and range. A p-value < 0.05 was deemed to be statistically significant.
Results
A total of 24 patients with very large nodule volumes received 2–3 sessions of laser ablation. summarizes the characteristics of the patients. The duration of each procedure ranged from 30 to 60 min. Twenty-one patients received two sessions of laser ablation. Three sessions were performed on 7 patients with a pretreatment nodule volume > 157 mL. In all patients, the initial session was performed using 3 fibers. For the second session, 70.8% (17/24) were performed using 3 fibers and 29.2% (7/24) were done using 2 fibers. In the 7 patients who received the third session, all of these were done using 2 fibers.
Table 1. Patient characteristics.
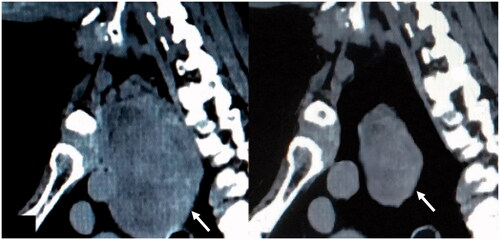
All patients received all of their sessions in the first year after their first ablation. At 1 year, technique efficacy was achieved in 75% (18/24) of patients. Median nodule volume was significantly reduced from 138 mL (range: 102–289 mL) at pretreatment assessment to 26 mL (range: 15–31 mL) at 1 year (p < 0.001 vs pretreatment). At a 4-years follow-up, the median nodule volume was 27 mL (range: 15–33 mL, p < 0.001 vs pretreatment). VRRs after one and two sessions of laser ablation were 48% and 78%, respectively. The VRRs at 1 year and at 4 years were 81% and 80%, respectively (). Two patients experienced nodule regrowth > 50% and went to surgery – one patient after 1 year and the other after 3 years. shows the CT scans obtained in the same patient before and at 6 months after the last laser treatment.
Figure 1. Median nodule volume over 4 years of follow-up. *p < 0.001 vs pretreatment nodule volume. Percentage values indicate the VRRs at each timepoint. The number of patients who underwent nodule-volume assessment at the different time points was as follows: pretreatment and 1 year, 24; 4 years, 23.
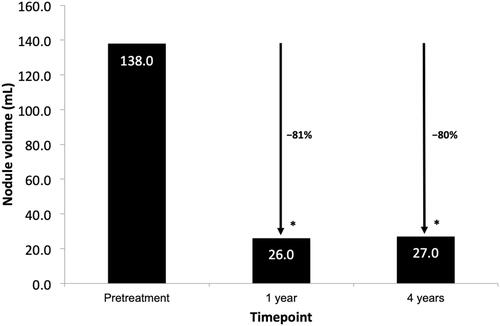
Figure 2. Example of CT scans before (left) and 6 months after (right) the last laser treatment. The thyroid nodule is indicated by the white arrows.
All patients maintained normal thyroid function during follow-up. At the end of treatment and follow-up, compressive symptoms were improved; 12 patients (50%) had a score of 0, 10 patients (41.7%) had a score of 1, and two (8.3%) had a score of 2. No patients had a compressive symptom score of 3 after treatment. No major complications of laser ablation occurred in this patient series. Transient fever (< 38 °C) occurred in 12% (3/24) of patients and local, mild-to-moderate pain (rated between 1 and 4 on the 10-point visual analog scale) was experienced by 8% (2/24) of patients.
Discussion
According to recent proposals for standardization of terminology for image-guided thyroid ablation, thyroid nodules should be classified as ‘small’ if they have a volume ≤ 10 mL, ‘medium’ if the volume is 11–30 mL, and ‘large’ if the volume is > 30 mL [Citation20]. In our cohort of 24 patients, the median nodule volume was 138 mL (range: 102–289 mL), indicating that these patients had very large thyroid nodules, and required relatively large ablation volumes.
In percutaneous laser ablation, amplification of the photocoagulated volume transversal to the direction of needle insertion can be achieved by the simultaneous illumination of more than one optical fiber, spaced 10–15 mm apart [Citation21]. Furthermore, enlargement of the ablation volume in the needle-insertion direction can be achieved using a pull-back maneuver and re-illumination. The use of these approaches, combined with repeat sessions of laser ablation, produced very good technical results, with a technique efficacy at 1 year of 75% and a VRR at 1 year of 81%. The effect of treatment was durable, with long-term benefit persisting at 4 years after the initial treatment; VRR at 4 years was 80%. Previous studies have indicated that an energy dose exceeding 500 J per mL of nodular tissue is required to produce good results [Citation5,Citation13,Citation22,Citation23]. In this patient series, the median energy delivered was 461 J per mL of tissue. However, for very voluminous nodules, it is acceptable to deliver less energy per mL because otherwise, the duration of treatment would be unacceptably long.
Despite all of the patients in our series receiving two or three sessions of laser ablation, the treatment was well tolerated and was achieved without major complications. As seen in previous studies of laser ablation, cases of transient fever and local pain were noted, but the absolute numbers and percentages of patients reporting these side effects were small (fever: 3 patients [12%]; pain: 2 patients [8%]). While these percentages are calculated from a relatively small number of patients, they are in broad agreement with values obtained in previous studies [Citation13,Citation15,Citation24,Citation25]. Lack of complications, although in such a small number of cases, confirms the Planning Software (available on Esaote US scanner and on a stand-alone device called ESI – EchoLaser Smart Interface, compatible with almost all commercial US scanners) as a useful tool in the needle positioning procedure for percutaneous laser ablation of BTN.
There are few data from prospective, randomized controlled trials comparing laser ablation with other image-guided ablation techniques. Laser ablation was compared with radiofrequency ablation in a randomized, single-center study in 58 patients with solid or predominantly solid BTNs. At 12 months, radiofrequency achieved a significantly larger nodule volume reduction; however, the technical success rate was similar in the two groups, and the two groups had similar, statistically significant improvements in compressive symptoms and symptom scores [Citation26]. Laser ablation was retrospectively compared with microwave ablation in a propensity-matched analysis of 320 BTN in 320 patients. While the overall VRRs of the microwave and laser groups were comparable, for nodules with a volume ≥ 13 mL, the VRRs associated with laser ablation at 6 months and beyond were significantly greater than those obtained with microwave ablation [Citation27]. To our knowledge, there are no head-to-head comparisons of laser ablation and HIFU in the published literature. However, a recent retrospective study of HIFU reported a 3-years follow-up in 65 patients with single BTNs. The median VRR at 12 months was 31.5%, and improvement in compressive symptoms or cosmetic complaints occurred in less than 15% of patients at 12, 24 and 36 months; these are lower percentages when compared with the other image-guided ablation techniques [Citation28]. An advantage of laser ablation compared with radiofrequency ablation is the reduced invasiveness; the Chiba needles used for laser ablation are 21 gauge, as opposed to the 18 gauge electrode needles used for radiofrequency ablation.
Certain strengths and limitations of the present study deserve mention. To our knowledge, our study is the first work to specifically evaluate laser ablation in a cohort of patients with very large nodule volumes. The 4-year duration of follow-up compares favorably with most other studies in the literature; until recently when we reported 10-follow-up after a single session of laser ablation in 171 patients [Citation14], the longest reported follow-up after laser ablation was 5 years [Citation25,Citation29]. However, our study was relatively small (n = 24 patients) and lacked a comparator group. In conclusion, in this cohort of patients with very large, BTN, treatment with two or three sessions of percutaneous, ultrasound-guided laser ablation produced a long-term reduction in nodule volume and was well tolerated.
Acknowledgments
Editorial support for the preparation of this article was provided by George Clarkson Ph.D., funded by Elesta SpA.
Disclosure statement
The authors confirm that there are no relevant financial or non-financial competing interests to report.
Additional information
Funding
References
- Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical Guidelines for clinical practice for the diagnosis and management of thyroid modules – 2016 update. Appendix. Endocrin Pract. 2016;22(Suppl 1):1–60.
- Papini E, Pacella CM, Solbiati LA, et al. Minimally-invasive treatments for benign thyroid nodules: a Delphi-based consensus statement from the Italian Minimally-Invasive Treatments of the Thyroid (MITT) group. Int J Hyperthermia. 2019;36(1):376–382.
- Papini E, Monpeyssen H, Frasoldati A, et al. 2020 European Thyroid Association clinical practice guideline for the use of image-guided ablation in benign thyroid nodules. Eur Thyroid J. 2020;9(4):172–185.
- Pacella CM, Bizzarri G, Guglielmi R, et al. Thyroid tissue: US-guided percutaneous interstitial laser ablation-a feasibility study. Radiology. 2000;217(3):673–677.
- Pacella CM, Bizzarri G, Spiezia S, et al. Thyroid tissue: US-guided percutaneous laser thermal ablation. Radiology. 2004;232(1):272–280.
- Papini E, Guglielmi R, Persichetti A, et al. Benign thyroid nodule laser ablation. In: Pacella CM, Jiang T, Mauri G (eds.) Image-guided laser ablation. Cham, Switzerland: Springer Nature Switzerland AG; 2020. pp 61–73.
- Pacella CM, Mauri G, Achille G, et al. Outcomes and risk factors for complications of laser ablation for thyroid nodules. A multicenter study on 1531 patients. J Clin Endocrinol Metab. 2015;100(10):3903–3910.
- Gambelunghe G, Fatone C, Ranchelli A, et al. A randomized controlled trial to evaluate the efficacy of ultrasound-guided laser photocoagulation for treatment of benign thyroid nodules. J Endocrinol Invest. 2006;29(9):RC23–RC26.
- Papini E, Rago T, Gambelunghe G, et al. Long-term efficacy of ultrasound-guided laser ablation for benign solid thyroid nodules. Results of a three-year multicenter prospective randomized trial. J Clin Endocrinol Metab. 2014;99(10):3653–3659.
- Døssing H, Bennedbaek FN, Bonnema SJ, et al. Randomized prospective study comparing a single radioiodine dose and a single laser therapy session in autonomously functioning thyroid nodules. Eur J Endocrinol. 2007;157(1):95–100.
- Papini E, Guglielmi R, Bizzarri G, et al. Treatment of benign cold thyroid nodules: a randomized clinical trial of percutaneous laser ablation versus levothyroxine therapy or follow-up. Thyroid. 2007;17(3):229–235.
- Cesareo R, Pacella CM, Pasqualini V, et al. Laser ablation versus radiofrequency ablation for benign non-functioning thyroid nodules: six-month results of a randomized, parallel, open-label, trial (LARA Trial). Thyroid. 2020;30(6):847–856.
- Gambelunghe G, Bini V, Monacelli M, et al. The administration of anesthetic in the thyroid pericapsular region increases the possibility of side effects during percutaneous laser photocoagulation of thyroid nodules. Lasers Surg Med. 2013;45(1):34–37.
- Gambelunghe G, Stefanetti E, Avenia N, et al. Percutaneous, ultrasound-guided laser ablation of benign thyroid nodules: Results of 10-year follow-up in 171 patients. J Endocr Soc. 2021;5(7):1–7.
- Gambelunghe G, Stefanetti E, Colella R, et al. A single session of laser ablation for toxic thyroid nodules: three-year follow-up results. Int J Hyperthermia. 2018;34(5):631–635.
- Valcavi R, Riganti F, Bertani A, et al. Percutaneous laser ablation of cold benign thyroid nodules: a 3-year follow-up study in 122 patients. Thyroid. 2010;20(11):1253–1261.
- Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria-a 10-year update. J Vasc Interv Radiol. 2014;25(11):1691–1705.e4.
- Sacks D, McClenny TE, Cardella JF, et al. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14(9 Pt 2):S199–S202.
- Na DG, Lee JH, Jung SL, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012;13(2):117–125.
- Mauri G, Pacella CM, Papini E, et al. Image-guided thyroid ablation: proposal for standardization of terminology and reporting criteria. Thyroid. 2019;29(5):611–618.
- Heisterkamp J, Van Hillegersberg R, Sinofsky E, et al. Interstitial laser photocoagulation with four cylindrical diffusing fibre tips: Importance of mutual fibre distance. Lasers Med Sci. 1999;14(3):216–220.
- Gambelunghe G, Fede R, Bini V, et al. Ultrasound-guided interstitial laser ablation for thyroid nodules is effective only at high total amounts of energy: results from a three-year pilot study. Surg Innov. 2013;20(4):345–350.
- de Freitas RMC, Miazaki AP, Tsunemi MH, et al. Laser ablation of benign thyroid nodules: a prospective pilot study with a preliminary analysis of the employed energy. Lasers Surg Med. 2020;52(4):323–332.
- Gambelunghe G, Bini V, Stefanetti E, et al. Thyroid nodule morphology affects the efficacy of ultrasound-guided interstitial laser ablation: a nested case-control study. Int J Hyperthermia. 2014;30(7):486–489.
- Negro R, Greco G, Deandrea M, et al. Twelve-month reduction ratio predicts regrowth and time to regrowth in thyroid nodules submitted to laser ablation: a 5-year follow-up retrospective study. Korean J Radiol. 2020;21(6):764–772.
- Cesareo RR, Manfrini S, Pasqualini V, et al. Laser ablation versus radiofrequency ablation for thyroid nodules: 12-month results of a randomized trial (LARA II study). J Clin Endocrinol Metab. 2021;106(6):1692–1701.
- Shi F-Y, Zhou P, Liu W-G, et al. Microwave ablation compared with laser ablation for treating benign thyroid nodules in a propensity-score matching study. Front Endocrinol. 2019;10:874.
- Monpeyssen H, Hamou AB, Hegedüs L, et al. High-intensity focused ultrasound (HIFU) therapy for benign thyroid nodules: a 3-year retrospective multicenter follow-up study. Int J Hyperthermia. 2020;37(1):1301–1309.
- Bernardi S, Giudici F, Cesareo R, et al. Five-year results of radiofrequency and laser ablation of benign thyroid nodules: a multicenter study from the Italian minimally invasive treatments of the thyroid group. Thyroid. 2020;30(12):1759–1770.
