?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
To evaluate the efficacy, feasibility and acceptability of microwave ablation (MWA) compared to uterine artery embolization (UAE) as treatment for uterine fibroids.
Method
A randomized controlled superiority trial, including premenopausal women 30–55 years, with symptomatic uterine fibroids without any single fibroid exceeding mean diameter of eight centimeters. Patients were randomized to receive microwave ablation, performed abdominally or vaginally, or to uterine artery embolization. The primary outcome was volume difference of the three largest fibroids at 6 months post treatment evaluated by magnetic resonance imaging (MRI) by a blinded radiologist analyzed by Mann–Whitney U-test. Secondary outcomes included symptom severity score (SSS), health related quality of life (HR-QoL), amount of menstrual bleeding, postoperative pain, length of hospitalization, need for additional treatment, adverse events and if patients would recommend the treatment to a friend.
Results
Patients were recruited from 30 January 2017 to 12 September 2019, with a total of 17 patients treated in each group from May 2017 to December 2019. Superiority of MWA could not be established. The volume reduction was 41.8% (Interquartile range, IQR, 14–63) in the MWA group compared to 62.2% (IQR 34.9–80.1) in the UAE group (p = 0.29). Effects on symptoms, HR-QoL and acceptability did not differ between groups. Days of hospitalization and sick leave were significantly fewer in the MWA group (p < 0.001 and p = 0.001).
Conclusions
Although superiority of MWA could not be established, it is a promising technique for treating uterine fibroids. It was well tolerated and associated with lower use of health care resources. Trial registration: NCT02942537, www.clincialtrials.gov
Introduction
Uterine fibroids are the most common benign pelvic tumor in women, reaching a lifetime incidence of up to 77% [Citation1,Citation2]. The main reasons for seeking medical care are heavy menstrual bleeding (HMB), pelvic pain, pressure symptoms or fertility disorders [Citation3]. Traditionally, fibroid symptoms have been treated with hysterectomy. Hysterectomy is an invasive surgical procedure carrying a risk of short term complications such as infections and organ damage as well as long-term side effects such as genito-vaginal prolapse. Myomectomy, another common surgical fibroid treatment, spares the uterus but is associated with a high recurrence rate [Citation4,Citation5] and the same short-term complications as hysterectomy at a lower incidence.
In recent years the interest in medical treatment and minimally invasive or noninvasive therapies with uterine preservation has increased. Minimally invasive treatments include uterine artery embolization (UAE), radiofrequency ablation, high intensity focused ultrasound and microwave ablation (MWA). UAE is an established method to decrease volume of fibroids and improve clinical symptoms [Citation6], however postoperative pain and post-embolization syndrome associated with the procedure have limited its use [Citation7]. There has been a concern that women are at increased risk of entering earlier menopause after UAE and previous studies have shown contradictory results [Citation8–10]. Studies of MWA do not report any effects on ovarian reserve nor an elevated risk of entering premature/earlier menopause [Citation11]. A retrospective comparison of high intensity focused ultrasound and MWA showed no difference in outcome but shorter treatment times in the MWA group [Citation12].
Ultrasound guided MWA is minimally invasive, has short time requirements and is easy to perform. It is used for the treatment of solid tumors in organs other than the uterus with favorable effects [Citation13]. For treatment of uterine fibroids, MWA has been used mainly in China and Japan [Citation14–16]. MWA utilizes electromagnetic microwaves to induce heat and coagulation necrosis, resulting in fibroid shrinkage and relief of symptoms. Safety, efficacy, and acceptability has been established in prospective observational studies [Citation14,Citation17]. To the best of our knowledge no randomized comparative studies of patients with uterine fibroids have been published in English. The objective of this study was to compare efficacy, safety, and acceptability of MWA compared to UAE in a randomized controlled trial.
Methods
The study was approved by the Regional Ethical Review Board of Stockholm (Ö14-2016 and amendments 2017/2130-32 for increase in fibroid size to 8 cm, addition of AMH, ferritin and hemoglobin at 1, 3 and 6 months, 2018/1650-52 for addition of vaginal approach and increased microwave energy in Watts). The trial was registered at clincialtrials.gov (NCT02942537).
We performed a single center randomized superiority trial with blinded primary outcome assessment comparing MWA to UAE treatment in patients with symptomatic uterine fibroids. All patients were recruited and treated at Danderyd Hospital, a tertiary teaching hospital affiliated to Karolinska Institutet. The inclusion criteria were (1) Women with presence of fibroids without any single fibroid exceeding mean diameter of eight centimeters evaluated by transvaginal or transabdominal ultrasound, (2) age 30–55, (3) premenopausal status, (4) symptoms including bleeding, pressure symptoms or urgency, and (5) willing to comply with protocol. The exclusion criteria where (1) desire for future fertility, (2) Body Mass Index >35, (3) treatment with anticoagulant or bleeding disorder and, (4) any contraindication for UAE or general anesthesia. To be included patients had to agree to discontinue any hormonal treatment at least two months prior to planned treatment. Patients were provided with written and oral information about the study by an investigator. All patients thereafter signed informed consent forms. No patients or patient organizations were involved in the conceivement of the trial.
An MRI was performed after informed consent was obtained, and if patients still fulfilled inclusion criteria, randomization was performed at a ratio of 1:1 in permuted blocks of 2–6 to either MWA or UAE by consecutive opening of numbered opaque sealed envelopes containing the allocation. The envelopes were prepared by staff not involved in the study following a computer-generated randomization list (www.sealedenvelope.com). In total, 36 patients with symptomatic uterine fibroids were randomized to MWA or UAE. It was not deemed feasible to blind patients nor providers.
All patients filled in a validated questionnaire for evaluation of uterine fibroid symptoms (UFS-QoL) [Citation18–20]. UFS-QoL generates a symptom severity score (SSS) where high scores indicate more severe symptoms, and a score on health-related quality of life (HR-QoL) where high scores indicate a higher quality of life.
Patients filled in the validated Pictorial Bleeding Assessment Chart (PBAC) for assessment of menstrual bleeding [Citation21,Citation22] during the menstruation closest to treatment. PBAC creates a score based on numbers of pads and tampons used, the degree of soaking of pads and tampons, clots passed, and flooding episodes during a menstrual period. In addition, a full blood panel, ferritin, and Anti-Müllerian Hormone (AMH) was evaluated.
All patients in both treatment groups were required to stay in hospital over night the day of the procedure, in order to objectively evaluate pain and adverse events at least 24 h post operatively.
We used an Emprint™ Ablation Generator with Thermosphere™ Technology (Medtronic, Minneapolis, USA) with a 13-gauge antenna. The generator operates at a frequency of 2.45 GHz ± 50 MHz with an output power range of 5–100 Watts. There are many different ablation generators available in the market, with slight differences in performance. We used the Emprint™ Ablation Generator with Thermosphere™ Technology (Medtronic, Minneapolis, USA), as it was well known by the interventional radiologists executing the ablations. At the time of the study, the Emprint system was one of the systems used in our clinic that enabled spherical ablation zones [Citation23], which was assumed to be beneficial when treating round lesions like fibroids. Ultrasound (LOGIQ™ 10, GE Healthcare) was used for imaging and needle guidance. Contrast enhanced ultrasound was used to assess size and vascularization of the fibroids, with the administration of 2.4 ml of SonoVue® medium (Bracco, Milan, Italy) before and immediately after MWA.
The ablations were performed under general anesthesia in supine position. The microwave antenna was inserted under ultrasound guidance by an experienced interventional radiologist for percutaneous approach or by gynecologists in the presence of an experienced interventional radiologist for vaginal approach. The shortest and safest route was chosen depending on the fibroid localization. If the percutaneous route was used, a skin incision corresponding to the size of the tip of the microwave antenna was made. For the vaginal route the needle was inserted without prior incision through the posterior or frontal fornix of the vagina. The antenna was inserted into the fibroid until the tip of the antenna was 0.5–1 cm from the distal end of the fibroid depending on surrounding tissue, as heat can spread 3–5 mm beyond the tip of the antenna according to the manufacturer. In the study, the microwave effect used was 50–80 Watts depending on the size and composition of the fibroid treated. During ablation, the ablation effect on the fibroid was monitored by real-time ultrasound and the MWA was stopped when the microbubbles that roughly represent the ablation zone covered the whole fibroid. In larger fibroids the antenna was pulled back and/or reinserted for a new ablation. If the contrast enhanced ultrasound showed remaining vascularization in the treated fibroid, the procedure was repeated if possible. A typical image of the post ablation evaluation with contrast enhanced ultrasound is shown in Supplementary Figure 1. Post-operative pain was managed according to a standardized protocol for all MWA patients with pre-operative medication of 1.5 g acetaminophen (paracetamol), 400 mg celecoxib, and 5 mg oxycodone. If additional pain medication was needed, intravenous morphine was administered as needed in the post-operative care unit.
UAE was carried out by experienced interventional radiologists under fluoroscopic guidance (AlphenixTM, INFX-8000V, Canon Medical System Corporation, Askim, Sweden). A unilateral groin approach was used for bilateral, selective embolization of the uterine artery. Through a microcatheter (Embocath® Plus, Merit Medical, Stockholm Sweden) tris-acryl polymer microspheres 500–700 µm (Embosphere®, Merit Medical, Stockholm, Sweden) were injected until flow in the artery ceased. UAE was performed with an epidural anesthesia placed pre-operatively using sufentanil and ropivacaine as per clinical practice in our clinic. The day after UAE patients received 400 mg celecoxib, 1 g acetaminophen and 10 mg oxycodone according to a standardized post-operative pain protocol. Two hours after having received medication the epidural was turned off and pain was continuously evaluated using a Visual Analogue Scale (VAS). If the patient could not tolerate the pain, the epidural was re-activated without sufentanil and the procedure was repeated every morning until the woman could leave the hospital with per oral analgesia.
A second MRI was performed at 6 months post treatment (±15 days) and evaluated by a blinded radiologist. Patients filled in UFS-QoL at the 6 months visit and PBAC at menstruation number 5 postoperatively. Post-operative maximum pain was evaluated on a VAS on the treatment day. Pain at 9 am every following day in hospital and the maximum pain during the day at bedtime for the first seven days at home was evaluated on a VAS. Length of hospitalization for both groups was noted. Follow-up visits were scheduled 1, 3, and 6 months after first post-treatment menstruation (±2 weeks). Patients were asked about post-operative pain, use of pain medication, and how long it took before they could resume normal daily activities.
At the follow up visits, acceptability was assessed by asking patients if they would recommend the treatment to a friend using a scale from 1 (very unlikely) to 7 (very likely). Hemoglobin, ferritin and Anti-Müllerian Hormone (AMH) were measured. Information on adverse events was collected continuously.
The primary outcome was difference in fibroid volume 6 months post treatment according to the formula:
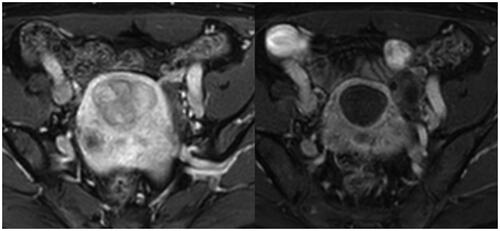
The pre- and post-operative MRI evaluation at 6 months of the same patient as above is shown in and . The primary outcome was based on present literature of fibroid treatment with MWA at study start [Citation14].
Figure 1. Sagittal MRI of fibroid at baseline (craniocaudal measurement 34.7 mm) and at 6 months post treatment (26.7 mm).
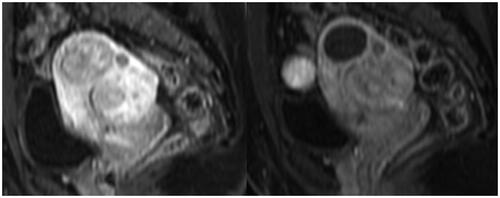
Figure 2. Axial MRI of fibroid at baseline (36.1 × 47.4 mm) and at 6 months post treatment (33 × 35.8 mm).
Secondary outcomes were symptom severity score (SSS) and health related quality of life (HR-QoL) evaluated by UFS-QoL questionnaire at 6 months post treatment (±2 weeks), amount of menstrual bleeding during the 5th menstruation post-treatment, post-operative pain, length of hospitalization, need for additional treatment, adverse events, and if patients would recommend the treatment to a friend.
Power calculation: The power calculation was based on results from a previous study by Zhang et al [Citation14] for MWA effects and from the literature for UAE. To be able to show a difference between the groups in fibroid volume reduction at 6 months of 75% in MWA and 50% in the UAE group with a standard deviation of 25% with an alpha of 0.05 and a power of 80%, 16 patients were needed in each group. To compensate for loss to follow up we aimed to randomize 18 patients in each group.
Comparisons between groups for differences in baseline values and values at 6 months were analyzed by Mann–Whitney U-test. Comparisons between groups for continuous variables with a single measurement were analyzed by Mann–Whitney U-test. We calculated 95% confidence intervals (CI) for the population median using the exact method based on the binomial distribution. For acceptability with treatment the values of 1–3 were categorized as “would not recommend”, 4–5 as “would neither recommend nor discourage” and 6–7 as “would recommend”. Categorical variables were analyzed using Chi2-test or Fisher´s exact test as appropriate.
Pain levels over time were analyzed by a linear mixed model with pain on the VAS as a dependent variable and allocation (MWA or UAE) and timepoints as factors. In a fixed model, allocation, timepoint and an interaction variable of allocation*timepoint were used. All statistical analyzes were performed using the Statistical Package for Social Sciences (SPSS) version 26 (IBM corporation, Armonk, New York, US).
Results
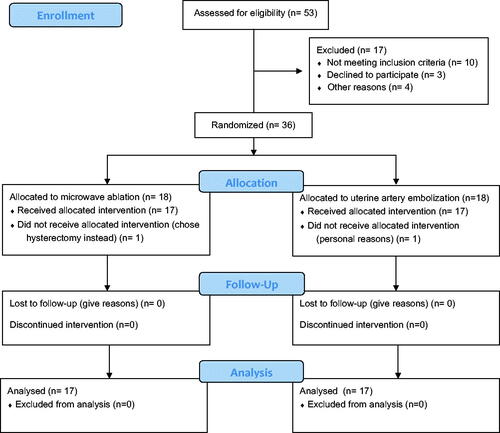
Patients were recruited from 30 January 2017 to 12 September 2019, with a total of 17 patients treated in each group from May 2017 to December 2019 at Danderyd Hospital. The flow of patients is presented in the Consort Flow Chart ().
Baseline characteristics of both groups are presented in . There were no cross overs. For the largest fibroid of 7.7 × 7.6 × 6.7 cm, a total ablation time of 1,260s was needed. Vaginal treatment was performed in two women in the MWA group. There was no significant difference in the primary outcome of fibroid volume reduction between the groups (p = 0.29). Graphical representations of the change in volume after treatment in both groups are shown in (line plot) and (Box plot).
Figure 4. Line plot of volume change (ml) before and after treatment. MWA: Microwave ablation; UAE: Uterine artery embolization.
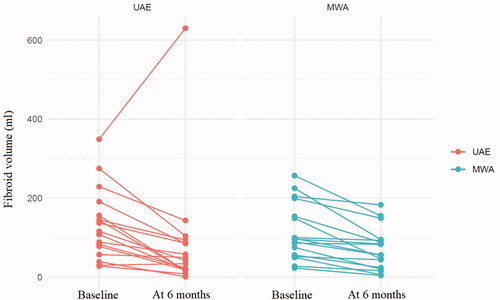
Table 1. Baseline characteristics.
The primary outcome and secondary outcomes are presented in . Fibroid characteristics and individual treatments results are shown in . For two patients in the UAE group treatment resulted in amenorrhea and menopausal vegetative symptoms which were confirmed by post-menopausal levels of follicle stimulating hormone. For these patients the secondary outcomes of SSS, HR-QoL and PBAC could not be evaluated. Both methods led to improvements in SSS, and in HR-QoL without significant differences between groups. There were no significant differences between groups in hemoglobin, ferritin or AMH levels. The pattern of postoperative pain is shown in . There were no significant differences in pain levels over time between groups (p = 0.071).
Table 2. Primary and Secondary outcomes.
In the MWA group patients stayed in hospital significantly fewer days (p < 0.001) and had significantly fewer days of sick leave (p = 0.001). Both methods were highly acceptable, measured as a recommendation of the method to a friend. In the UAE group, 2 patients would not recommend the treatment to a friend, compared to none in the MWA group. Fourteen patients in the MWA group would recommend the treatment compared to ten patients in the UAE group. Overall, there were no significant differences in acceptability between groups (p = 0.097). Three patients in the UAE group required additional treatment due to insufficient relief of fibroid symptoms after the 6 months follow up visit whereof two had a hysterectomy and one had a transcervical resection of myoma within 1 month after the 6 month follow up. In the MWA group there were no additional treatments required due to fibroid symptoms.
There were more adverse events in the UAE group (). One patient in the UAE group had temporary menopausal symptoms that subsided after 3 months and two patients in the UAE group entered menopause after the treatment at the age of 45 and 48 respectively, compared to none in the MWA group.
Discussion
Both MWA and UAE led to a reduction of fibroid volume and clinical symptoms. We could not establish superiority for efficacy of MWA over UAE. MWA results did not differ significantly from UAE results in fibroid volume reduction, symptom alleviation, quality of life improvement, post-operative pain levels or acceptability. Length of hospitalization and days of sick leave did however differ significantly between the groups in favor of MWA. In addition, no patients in the MWA group required additional treatment due to uterine fibroid symptoms.
In this study patient reported outcomes such as bleeding, pain and acceptability were compared between MWA and UAE. There are few published studies comparing patient reported outcomes with MWA to other established treatments. A previous randomized study compared MWA to radiofrequency ablation for treatment of adenomyosis [Citation24]. However, radio frequency ablation is not commonly used for adenomyosis nor for uterine fibroids. We therefore chose comparison to UAE which is the most established and commonly used minimally invasive treatment with uterine preservation.
In the MWA group all treated fibroids decreased in size. This may have reduced the need for additional treatment due to persisting symptoms of uterine fibroids in MWA group. Predictable treatment result facilitates information prior to surgery as patients can be reassuringly informed about expected treatment outcomes. In the UAE group, complete embolization failed in one patient despite microspheres being injected until visible flow in the artery ceased. Recanalization of the arteries or prominent nonuterine artery collateral supply can result in fibroid growth and worsening of symptoms [Citation25]. This patient subsequently had a hysterectomy.
Although we could not show superiority of MWA in fibroid volume or symptom reduction, we consider microwave ablation a promising minimally invasive treatment of symptomatic uterine fibroids, considering the low need for hospitalization, sick leave, and the high acceptability of the procedure. Using an ultrasound guided needle is common practice in gynecology and introduction and implementation of the method is therefore feasible. Furthermore, we do not see any indication of negative effects on ovarian reserve post-treatment, in conjunction with previous reports [Citation11]. Thus, MWA has the potential of becoming a promising treatment for patients who desire fertility sparing treatment. For the UAE group two women entered permanent menopause and one woman has transient menopausal symptoms. The women who entered menopause after UAE were above 45 years- a well-known risk factor [Citation26]. Moreover, the sample size is small and these results may be due to chance.
More comparative as well as prospective observational multicenter studies are needed to establish which patients are most likely to benefit from MWA for uterine fibroids. Based on our experience, we speculate that MWA is more suitable for women with one to a few large fibroids, especially if submucosal in location, while women with multiple fibroids might benefit more from UAE. This is due to technical aspects of MWA where treatment of multiple lesions is more time consuming, and many antenna insertions entails increased risk of complications. Long term follow-up data is also needed prior to broad implementation to determine the need for repeated or additional treatment and to establish whether the treatment is effective until patients reach menopause.
The lack of a core outcome set for trials on treatment of uterine fibroids has been acknowledged [Citation27]. We aimed to include patient reported outcomes as well as previously used outcomes for MWA. We based our primary outcome on treatment results available at the time when the power calculation was performed. We were unable to demonstrate the same level of fibroid volume reduction as in previous studies [Citation14–17,Citation28]. It cannot be excluded that this is due to a learning curve with potential improvement with increased MWA experience in treating uterine fibroids.
The strengths of the study include the randomized design with the blinded assessment of the primary outcome. In addition, secondary outcomes included both objectively evaluated outcomes such as hemoglobin levels and AMH in addition to patient reported outcomes on symptoms and acceptability.
The limitations include that this was a single center study with a small sample size. The single center design was due to lack of equipment and competence for MWA in other sites that were approached. The sample size was sufficient to show the difference postulated in the power calculation which was based on a conservative estimation of previous results. It was not deemed feasible to blind patients as treatments had different methods of anesthesia and entry methods. Several MWA treated patients actively asked to be discharged on the day of the procedure but were asked to stay overnight due to protocol requirements. Our trial protocol may thus have affected the difference in hospital stay between groups in favor of UAE and yet a significant difference was seen favoring MWA treatment. According to our experience in this trial, we have subsequently scheduled, and treated, all patients in our currently ongoing prospective observational trial of MWA for uterine fibroids as out-patients.
Microwave ablation is a promising minimally invasive method for treating uterine fibroids. It carries high tolerability and lower use of health care resources compared to UAE.
Supplemental Material
Download PDF (271.4 KB)Acknowledgments
The authors extend our sincere thanks and gratitude to Professor Jing Zhang at the Department of Interventional Ultrasound, Chinese PLA General Hospital, Beijing, China, for introducing us to microwave ablation of uterine disease, for her hospitality and for so generously sharing her extensive knowledge and expertise. The authors thank Anju Zhang, obstetrician gynecologist at Danderyd Hospital, for invaluable enthusiasm, knowledge and expertise in addition to interpretation in communication and during travels.
Disclosure statement
The authors report the following potential conflicts of interest: Kopp Kallner reports personal fees from pharmaceutical companies outside the submitted work (presentations and advisory boards). Beermann, Cronsioe, Hasselrot and Kopp Kallner have participated in symposia on microwave ablation sponsored by Medtronic. Jonsdottir reports no conflicts of interest.
Data availability statement
Will individual participant data be available (including data dictionaries)? Yes- upon reasonable request.
What data in particular will be shared? All available data in the database will be made available.
What other documents will be available? No other information will be made available.
When will data be available (start and end dates)? Data is saved for 10 years and is then destroyed.
By what access criteria will data be shared. (including with whom, for what types of analyses, and by what mechanism)? Data will be made available upon reasonable request as judged by the research group.
Additional information
Funding
References
- Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95–114.
- Viswanathan M, Hartmann K, McKoy N, et al. Management of uterine fibroids: an update of the evidence. Evid Rep Technol Assess (Full Rep). 2007;154:1–122.
- Divakar H. Asymptomatic uterine fibroids. Best Pract Res Clin Obstet Gynaecol. 2008;22:643–654.
- Ming X, Ran XT, Li N, et al. Risk of recurrence of uterine leiomyomas following laparoscopic myomectomy compared with open myomectomy. Arch Gynecol Obstet. 2020;301:235–242.
- Kotani Y, Tobiume T, Fujishima R, et al. Recurrence of uterine myoma after myomectomy: Open myomectomy versus laparoscopic myomectomy. J Obstet Gynaecol Res. 2018;44:298–302.
- Keung JJ, Spies JB, Caridi TM. Uterine artery embolization: a review of current concepts. Best Pract Res Clin Obstet Gynaecol. 2018;46:66–73.
- Ganguli S, Faintuch S, Salazar GM, et al. Postembolization syndrome: changes in white blood cell counts immediately after uterine artery embolization. J Vasc Interv Radiol. 2008;19:443–445.
- Kaump GR, Spies JB. The impact of uterine artery embolization on ovarian function. J Vasc Interv Radiol. 2013;24:459–467.
- Kim CW, Shim HS, Jang H, Song YG. The effects of uterine artery embolization on ovarian reserve. Eur J Obstet Gynecol Reprod Biol. 2016;206:172–176.
- El Shamy T, Amer SAK, Mohamed AA, et al. The impact of uterine artery embolization on ovarian reserve: a systematic review and Meta-analysis. Acta Obstet Gynecol Scand. 2020;99:16–23.
- Yang Y, Zhang J, Han ZY, et al. Ultrasound-guided percutaneous microwave ablation for adenomyosis: efficacy of treatment and effect on ovarian function. Sci Rep. 2015;5:10034.
- Zhao WP, Han ZY, Zhang J, et al. A retrospective comparison of microwave ablation and high intensity focused ultrasound for treating symptomatic uterine fibroids. Eur J Radiol. 2015;84:413–417.
- Arellano RS. What's new in percutaneous ablative strategies for hepatocellular carcinoma and colorectal hepatic metastases? 2020 update. Curr Oncol Rep. 2020;22:105.
- Zhang J, Feng L, Zhang B, et al. Ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroid treatment–a clinical study. Int J Hyperthermia. 2011;27:510–516.
- Yang Y, Hao Y, Zhang J, et al. Ultrasound-Guided percutaneous microwave ablation for subserosal uterine myomas. J Minim Invasive Gynecol. 2019;26(3):544–550.
- Wang F, Zhang J, Han ZY, et al. Imaging manifestation of conventional and contrast-enhanced ultrasonography in percutaneous microwave ablation for the treatment of uterine fibroids. Eur J Radiol. 2012;81(11):2947–2952.
- Liu H, Zhang J, Han ZY, et al. Effectiveness of ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroids: a multicentre study in China. Int J Hyperthermia. 2016;32:876–880.
- Coyne KS, Margolis MK, Murphy J, et al. Validation of the UFS-QOL-hysterectomy questionnaire: modifying an existing measure for comparative effectiveness research. Value Health. 2012;15:674–679.
- Harding G, Coyne KS, Thompson CL, et al. The responsiveness of the uterine fibroid symptom and health-related quality of life questionnaire (UFS-QOL). Health Qual Life Outcomes. 2008;6(1):99.
- Spies JB, Coyne K, Guaou Guaou N, et al. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol. 2002;99:290–300.
- Magnay JL, O'Brien S, Gerlinger C, et al. Pictorial methods to assess heavy menstrual bleeding in research and clinical practice: a systematic literature review. BMC Womens Health. 2020;20:24.
- Reid PC, Coker A, Coltart R. Assessment of menstrual blood loss using a pictorial chart: a validation study. Bjog. 2000;107:320–322.
- Vogl TJ, Basten LM, Nour-Eldin NA, et al. Evaluation of microwave ablation of liver malignancy with enabled constant spatial energy control to achieve a predictable spherical ablation zone. Int J Hyperthermia. 2018;34:492–500.
- Lin XL, Hai N, Zhang J, et al. Comparison between microwave ablation and radiofrequency ablation for treating symptomatic uterine adenomyosis. Int J Hyperthermia. 2020;37:151–156.
- Schirf BE, Vogelzang RL, Chrisman HB. Complications of uterine fibroid embolization. Semin Intervent Radiol. 2006;23:143–149.
- Hovsepian DM, Siskin GP, Bonn J, et al. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata. J Vasc Interv Radiol. 2009;20:S193–S9.
- Tran AP, Al Naber J, Tambor ES, et al. Addressing heterogenous outcomes in uterine fibroid research: a call to action. Am J Obstet Gynecol. 2020;223:75.e1–e5.
- Yang Y, Zhang J, Han ZY, et al. Ultrasound-guided percutaneous microwave ablation for submucosal uterine fibroids. J Minim Invasive Gynecol. 2014;21(3):436–441.