Abstract
Objective
To study long-term effects in patients treated with microwave ablation (MWA) for symptomatic uterine fibroids and investigate fibroid characteristics predictive of successful treatment.
Method
Women who received MWA treatment for uterine fibroids in a previous study were included. A total of 16 patients underwent contrast enhanced MRI before treatment, postoperatively at 6 months and at long-term follow-up, to assess volumes of treated fibroids (n = 42). Long-term MRI was performed between 16 and 36 months after treatment [median 22 months, interquartile range (IQR) 18.5–27]. Validated questionnaires for evaluation of uterine fibroid symptoms and menstrual bleeding (UFS-QoL and PBAC) were used to assess long-term effects on symptoms. The degree of shrinkage was correlated to vascularization and T2 signal intensity (SI) at preoperative MRI and location of fibroids according to the FIGO classification, using the Mann–Whitney U test.
Results
Most patients (82%) reported improvement up to 3 years after treatment. Out of 42 treated fibroids, 35 (83%) continued to shrink over time with median relative volume reduction of 77% (IQR 39–95). For eight fibroids (19%) which showed low vascularization on the pretreatment MRI, there was less shrinkage compared to well-vascularized fibroids (p = 0.01). Most fibroids (79%) showed iso- to hyperintense T2 signal on preoperative MRI and showed a higher grade of shrinkage than hypointense fibroids (p = 0.02).
Conclusion
After microwave treatment improvement is maintained for most patients up to 36 months and most fibroids showed continuous shrinkage. Preoperative vascularization, high T2 SI and submucosal location predicted continuous volume reduction. However, to confirm this, larger studies are needed.
Background
Uterine fibroids are common in women of reproductive age, reaching a lifetime incidence of up to 70% [Citation1]. Although benign, they may cause severe symptoms of heavy menstrual bleeding, pain and infertility [Citation2]. If medical treatment fails, hysterectomy is curative but may lead to short- and long-term complications such as infections, organ damage and genito-vaginal prolapse [Citation3,Citation4]. Since many patients desire uterine preservation, the interest for minimally invasive treatments such as high-intensity focused ultrasound (HIFU), uterine artery embolization (UAE), radiofrequency ablation (RFA) and percutaneous microwave ablation (MWA) is increasing [Citation2].
MWA is a well-established method for treating malignant tumors in solid organs such as liver, kidney and lung but has also been used for the treatment of uterine fibroids mainly in China and Japan. Used correctly, it is safe, fast and easy to perform, and patient acceptability is high [Citation5–8]. Zhang et al. [Citation8,Citation9] among others have reported continuous shrinkage of fibroids after MWA for up to 12 months after ablation, but long-term effects are less well studied.
Also, the literature suggests that fibroid characteristics visualized by Magnetic Resonance Imaging (MRI) may affect outcome of MWA [Citation10], but comprehensive studies are missing.
We have previously published results of a trial including patients with symptomatic fibroids randomized to treatment with either MWA or UAE, where volume reduction at 6 months evaluated by contrast enhanced MRI was the primary outcome [Citation11]. We here present a long-term follow-up of symptoms. In addition, an MRI follow-up was performed to study fibroid volume, regrowth and to investigate if fibroid characteristics such as preoperative vascularization, T2 signal intensity (SI) and location of the fibroid predict treatment effect.
Methods
The study was approved by the Swedish Ethical review Authority (permit no 2019-04273 with amendment 2020-00200 and 2020-01157).
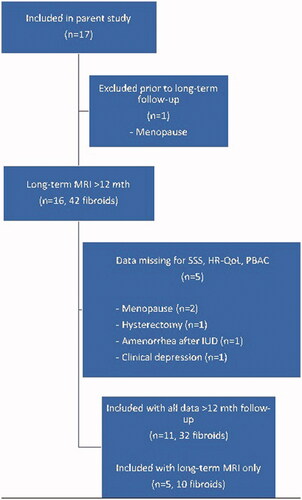
All 17 patients treated with MWA in our previous study [Citation11] were offered inclusion during a planned follow up visit according to protocol of the randomized controlled trial. One patient had entered menopause and was therefore excluded from the study, as menopause may affect fibroid volume [Citation12]. A total of 16 patients signed a new informed consent to have an MRI >12 months after treatment (flow chart of inclusion is shown in ). The follow-up MRI was performed 16-36 months after the MWA treatment [median 22 months, interquartile range (IQR) 18.5–27]. The volume of the treated fibroids (n = 42) was compared to the volume preoperatively and at 6 months.
Before treatment and at planned follow-up at set time points, patients filled in validated questionnaires for evaluation of uterine fibroid symptoms (The Uterine Fibroid Symptoms and Quality of Life questionnaire UFS-QoL) [Citation13,Citation14]. UFS-QoL generates a symptom severity score (SSS) where high scores indicate more severe symptoms, and a score on health-related quality of life (HR-QoL) where high scores indicate a better quality of life. Patients also filled in a validated Pictorial Bleeding Assessment Chart (PBAC) for assessment of menstrual bleeding [Citation15,Citation16].
Vascularization of fibroids (measured as contrast enhancement) and T2 SI at pretreatment MRI were correlated to volume reduction over time.
The International Federation of Gynecology and Obstetrics (FIGO) classification system for fibroid location was applied to all fibroids [Citation17]. In order to compare different FIGO classifications, we defined two groups which represent the clinical impact of the fibroid location: FIGO 0-2 = intracavitary/submucosal fibroids (n = 10) and FIGO 3-6 = intramural/subserosal fibroids (n = 32).
MRI
A series of standard T1-weighted, T2-weighted and contrast enhanced T1-weighted imaging were performed with a 3T IngeniaTM (Philips). The uterine fibroids were classified on contrast-enhanced MRI as showing (1) homogenous enhancement similar to or higher than myometrium, (2) inhomogeneous but distinct enhancement, (3) lower (or absent) enhancement when compared with myometrium. The fibroids were also classified on T2-weighted imaging into three groups depending on SI. (1) Hypointense; SI-like skeletal muscle, (2) Isointense; SI lower than myometrium but higher than skeletal muscle or (3) Hyperintense; SI the same or higher than myometrium. The classification was made by two senior radiologists and when the interpretation differed, consensus was reached by discussion. The follow-up MRI scans were performed with the same 3T IngeniaTM (before October 2019) or a 3T SIGNATM from GE Healthcare (after October 2019). The same protocol was used for all MRI scans.
Comparison between differences in baseline values and values at long-term follow-up were analyzed by Mann–Whitney U test. Statistical analyses were performed using SPSS version 26 (IBM Corporation, Armonk, New York, USA).
Results
We included 16 patients with a total of 42 fibroids previously treated with MWA.
Changes in SSS, HR-QoL and PBAC over time are shown in . The questionnaires filled in nearest in time of the long-term follow-up MRI were used for long-term evaluation of UFS-QoL (at least 12 months after treatment). Data are missing for 5 out of 16 patients for different reasons (menopause after MRI but before planned visit, hysterectomy after MRI but before planned visit, amenorrhea while use of hormonal IUD and clinical depression – could not bear to come). At long-term follow-up there was an increase in PBAC score for one patient, where the largest treated fibroid was avascular and showed no shrinkage over time. For this patient, the UFS-QoL scores showed worsening of symptoms and decreased quality of life. One additional patient had an isolated increase in the SSS score, but for all remaining patients there was an improvement at long-term follow-up compared to baseline. A total of 5 out of 11 patients had a decrease in the HR-QoL score and 8 out of 11 patients had an increase in the SSS score at long-term follow-up when compared with 6 months, but the scores were improved when compared with baseline (i.e., prior to MWA treatment). For the HR-QoL there was no difference in median score at the 6 months follow up (22, IQR 85–97) and at the long-term follow up (22, IQR 86–96), but for the SSS the median score worsened from 22 (IQR 21–35) to 34 (IQR 19–44).
Table 1. Base line characteristics and individual treatment results of uterine fibroids.
Out of the 42 fibroids, 35 (83%) continued to shrink between the 6 months and long-term follow-up MRI with a median relative volume reduction of 77% (IQR 39–95). The maximum number of treated fibroids in each individual was five. In seven patients with multiple fibroids the smallest ones were left without treatment and among these, one patient showed growth of untreated fibroids at long-term follow-up. In three fibroids (7%), size was increased compared to pretreatment volume due to regrowth of vascularized tissue, even though the immediate evaluation by contrast-enhanced ultrasound indicated technical success and there was a measurable volume reduction at 6 months for two-third of these fibroids. For eight fibroids (19%) which appeared to have very low vascularization on the pretreatment MRI there was none, or smaller, shrinkage compared to the preoperatively vascularized fibroids (showing distinct contrast enhancement on pretreatment MRI, groups 1–2). Median reduction rate was 27% (IQR 5.5–44) from baseline to long-term follow up compared to 84% (IQR 66–100) for the well-vascularized fibroids (p = 0.01).
The fibroids were also classified according to their T2 signal intensity (SI) on preoperative MRI. The majority of fibroids (32/42, 76%) were iso- to hyperintense and showed a higher grade of shrinkage than the fibroids classified as hypointense. Median volume reduction was 83.5% (IQR 53–100) compared to 43% (IQR 17.5–70.5), p = 0.02.
Our study did not show a significant correlation between T2 signal intensity and vascularization (p = 0.27).
The fibroids were grouped according to clinical impact of location based on the FIGO classification: FIGO 0-2 = intracavitary/submucosal fibroids (n = 10) and FIGO 3-6 = intramural/subserosal fibroids (n = 32). There was a significant difference in shrinkage from baseline to long-term follow up between the groups, where the median relative volume reduction was 98% (IQR 75–100) for the submucosal fibroids and 67.5% (IQR 35.5–91) for intramural/subserosal fibroids (p = 0.02). Individual fibroid characteristics and volume change over time are shown in . Volume change over time is graphically depicted in , and shows pre- and postoperative MRI images of a patient treated with MWA.
Figure 2. Line plot showing per patient change of fibroid volume (ml) over time. Every line represents 1 patient (n = 16).
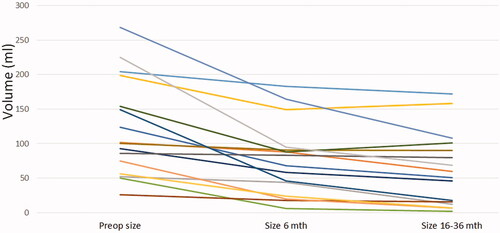
Figure 3. MRI images of a patient with two uterine fibroids. (a) before MWA, (b) 6 months after MWA and (c) at 19 months (sagittal view). At 19 months one fibroid is no longer visible.
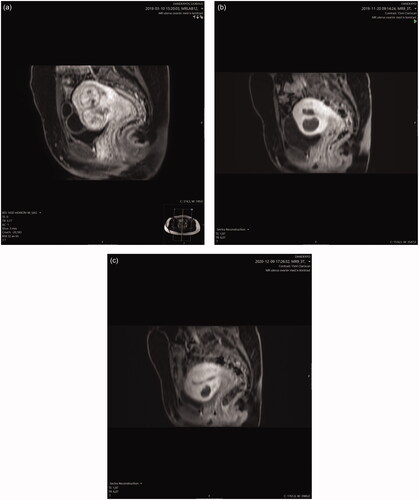
Table 2. Changes in SSS, HR-QoL and PBAC over time.
Discussion
The aim of this study was to evaluate the long-term effect of microwave ablation of uterine fibroids and to investigate fibroid characteristics predictive of outcome. Most patients (82%) reported an improvement of symptoms and quality of life and a decrease of menstrual bleeding at long-term follow-up compared to baseline. However, compared to the 6 months follow-up 8 out of 11 patients reported more symptoms related to uterine fibroids reflected by an increase in the SSS score. Although few fibroids grow back, small new fibroids that cause symptoms may develop. In other organs, MWA will often be repeated if there is local recurrence or new tumors, and this option should be further explored in studies of MWA for treatment of uterine fibroids. It is also noteworthy that the increase in SSS was not reflected by a simultaneous decrease in the HR-QoL scores. Thus, most likely the worsening of symptoms was not enough to cause a decrease in HR-QoL.
Even though most fibroids (83%) showed continuous shrinkage, the mean reduction rate at 6 months and long-term follow-up were 47% and 77%, respectively, which is less than what has been reported in the literature. There are several possible explanatory factors for these results. This was our first experience of MWA treatment for uterine fibroids. Because fibroids represent a benign disease the treatment is focused on symptom relief and the demand on safety is higher compared to treatment of malignant conditions. This might have led us to be more cautious of surrounding tissues than needed, as most fibroids have a pseudo-capsule that confines the heat and makes it possible to achieve satisfactory ablation volumes without undesirable thermal damage [Citation8]. We also accepted patients regardless of FIGO classification of the fibroids. The literature reports higher reduction rates for type 0-2 fibroids, as necrotic tissue can be completely discharged [Citation9]. These findings are supported by the results of this long-term follow up which showed a significant difference in volume reduction between submucosal fibroids and fibroids in other locations. For some fibroids the follow-up MRI showed signs of regrowth of vascularized tissue adjacent to, or filling out, the ablation zone. Regrowth after MWA treatment has not, to our knowledge, been previously described in the literature. Liu et al. [Citation9] reported partial ablation in some cases where the location of the fibroid was deemed to be too close to heat sensitive surrounding tissue but did not specify results for this group. When viable fibroid tissue is left in place, continued growth of this tissue is plausible. However, in our study small fibroids that were unlikely to have clinical significance were often left without treatment in patients with multiple lesions but only one patient showed growth of untreated fibroids on long-term follow-up. This could be due to lowered hormonal influence due to age or possibly other unknown factors. Further studies of partial MWA are needed.
Our study showed a significant correlation between high vascularization and/or T2 hyperintensity on preoperative MRI and a more pronounced fibroid shrinkage. Previously, Xia et al. have studied the relationship between MRI signal intensity and energy required per unit volume of MWA [Citation10]. They report that fibroids with high vascularization and T2 hyperintensity require higher energy per volume (EPV = the total energy of MWA/MWA volume).They hypothesize that a high T2 signal reflects high vascularization and perfusion of the tissue which may lead to decreased heat accumulation during MWA. This information could affect planning of the ablation. However, the higher EPV does not necessarily reflect effect on shrinkage over time, and even though these fibroids might be more challenging to treat our results indicate a positive long-term outcome in fibroids with high vascularization.
Our study did not show a significant correlation between T2 signal intensity and vascularization, most likely due to lack of power for such a calculation. However, we agree that a correlation seems reasonable as our results show a significant correlation between both high T2 signal and shrinkage and high vascularization and shrinkage. Vascularization evaluated by contrast enhanced imaging seems to be a good predictor of outcome of MWA, but in its place T2 signal intensity on MRI might be of value. The number of treated patients in the literature is still small, and larger studies with imaging of vascularization and MRI signal intensity and the correlation to EPV as well as long-term outcome are needed for conclusive results.
A limitation to our study is the small number of participants. However, we find it important to report long-term effects of MWA even in a small group of patients as follow-up for more than 12 months is scarcely reported in the literature. Also, there was no loss to follow-up at 6 months and only one woman was excluded from long-term MRI due to menopause. A possible limitation is that time from treatment to long-term follow-up differed between patients. However, as the changes from 6 months follow-up are small, a more homogenous timeline might not have affected our results significantly.
In conclusion, clinical symptoms measured by UFS-QoL and PBAC remained considerably improved compared to baseline and most fibroids showed continuous shrinkage over time up to 36 months. Based on our results, we suggest that well vascularized, T2 hyperintense and submucosal fibroids would benefit the most from this minimally invasive, uterine preserving treatment. However, larger studies are needed to confirm this.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95–114.
- Donnez J, Dolmans MM. Uterine fibroid management: from the present to the future. Hum Reprod Update. 2016;22(6):665–686.
- Aarts JWM, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2015;2015(8):Cd003677.
- Clayton RD. Hysterectomy. Best Pract Res Clin Obstet Gynaecol. 2006;20(1):73–87.
- Arellano RS. What's new in percutaneous ablative strategies for hepatocellular carcinoma and colorectal hepatic metastases? 2020 update. Curr Oncol Rep. 2020;22(10):105.
- Izzo F, Granata V, Grassi R, et al. Radiofrequency ablation and microwave ablation in liver tumors: an update. Oncologist. 2019;24(10):e990–e1005.
- Shakeri S, Raman SS. Trends in percutaneous thermal ablation therapies in the treatment of T1a renal cell carcinomas rather than partial nephrectomy/radical nephrectomy. Semin Intervent Radiol. 2019;36(3):183–193.
- Zhang J, Feng L, Zhang B, et al. Ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroid treatment–a clinical study. Int J Hyperthermia. 2011;27(5):510–516.
- Liu H, Zhang J, Han Z-Y, et al. Effectiveness of ultrasound-guided percutaneous microwave ablation for symptomatic uterine fibroids: a multicentre study in China. Int J Hyperthermia. 2016;32(8):876–880.
- Xia M, Jing Z, Zhi-Yu H, et al. Feasibility study on energy prediction of microwave ablation upon uterine adenomyosis and leiomyomas by MRI. Br J Radiol. 2014;87(1040):20130770.
- Jonsdottir G, Beermann M, Lundgren Cronsioe A, et al. Ultrasound guided microwave ablation compared to uterine artery embolization treatment for uterine fibroids: a randomized controlled trial. Int J Hyperthermia. 2022;39(1):341–347.
- Wise LA, Laughlin-Tommaso SK. Epidemiology of uterine fibroids: from menarche to menopause. Clin Obstet Gynecol. 2016;59(1):2–24.
- Coyne KS, Margolis MK, Murphy J, et al. Validation of the UFS-QOL-hysterectomy questionnaire: modifying an existing measure for comparative effectiveness research. Value Health. 2012;15(5):674–679.
- Spies JB, Coyne K, Guaou Guaou N, et al. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol. 2002;99(2):290–300.
- Magnay JL, O'Brien S, Gerlinger C, et al. Pictorial methods to assess heavy menstrual bleeding in research and clinical practice: a systematic literature review. BMC Womens Health. 2020;20(1):24.
- Reid PC, Coker A, Coltart R. Assessment of menstrual blood loss using a pictorial chart: a validation study. BJOG. 2000;107(3):320–322.
- Gomez E, Nguyen M-LT, Fursevich D, et al. MRI-based pictorial review of the FIGO classification system for uterine fibroids. Abdom Radiol (NY). 2021;46(5):2146–2155.