Abstract
Objective: Adenomyosis is a common gynecological disease, which occurs in women in reproductive age and is characterized by the presence of endometrial glands and stroma within the myometrium. Abnormal uterine bleeding, pelvic pain as well as infertility can be associated with adenomyosis. There are two main types of adenomyosis: diffuse and focal. Previously, adenomyosis was diagnosed only upon histopathological examination after hysterectomy and/or adenomyomectomy. However, the development of imagining techniques such as transvaginal ultrasound and magnetic resonance imaging enables the diagnosis of adenomyosis (diffuse and focal) without any surgical intervention. When medical therapy is contraindicated or ineffective, or if patients have a fertility desire, a surgical treatment may be necessary.
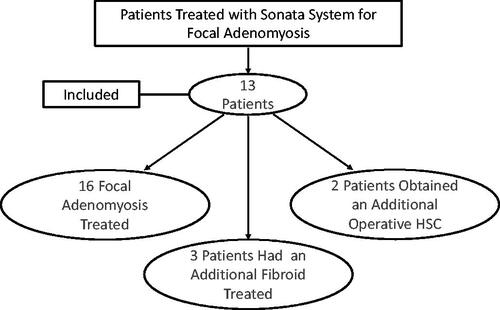
Methods: In this study, a total of 13 patients with 16 areas of focal adenomyosis were treated. All patients provided their informed consent to undergo transcervical adenomyosis ablation treatment with the Sonata System, aware that the safety and effectiveness of transcervical radiofrequency (RF) ablation for the treatment of adenomyosis has not been established. Follow-up was performed six months after Sonata treatment.
Results: The positive results relating to the improvement of symptoms and reduction of adenomyosis lesion size were observed in our study.
Conclusion: Transcervical RF ablation with the Sonata System may be a promising therapeutic alternative method to conventional procedures such as hysterectomy for the treatment of focal adenomyosis, disease which has limited therapeutic approach, and may enable a minimally invasive, uterine preserving option.
Introduction
Adenomyosis is a common gynecological disease, which occurs in women in reproductive age and is characterized by the presence of endometrial glands and stroma within the myometrium [Citation1]. Abnormal uterine bleeding, pelvic pain as well as infertility can be associated with adenomyosis; although, it is believed that as many as 30% may be asymptomatic [Citation2]. The true prevalence of adenomyosis remains unclear, and histopathologic and imaging diagnostic criteria remain to be standardized [Citation3]. There are two main types of adenomyosis: diffuse and focal. When focal adenomyosis is entirely surrounded by hyperplastic/hypertrophic smooth muscle, it is referred to as an adenomyoma, and such true adenomyomata are uncommon [Citation4,Citation5]. The first description of adenomyoma was in 1896 [Citation6]. With adenomyosis, the border of the lesion is indistinct from the adjacent myometrium [Citation7]. Adenomyosis is generally not considered to be premalignant, although rare cases of malignancy in association with adenomyosis have been reported [Citation8,Citation9]. Previously, adenomyosis was diagnosed only upon histopathological examination after hysterectomy and/or adenomyomectomy [Citation1]. However, the development of imagining techniques such as transvaginal ultrasound and magnetic resonance imaging enables the diagnosis of adenomyosis (diffuse and focal) without any surgical intervention [Citation10,Citation11]. Symptoms attributable to adenomyosis may be treated with a medical therapy [Citation12]. When medical therapy is contraindicated or ineffective, or if patients have a fertility desire, a surgical treatment may be necessary [Citation13]. The most used technique is either laparoscopic or open abdominal approach; however, currently new surgical methods are being tried for treatment of adenomyosis [Citation14].
Transcervical radiofrequency (RF) ablation with the Sonata® System is a focal, volumetric image-guided RF procedure. The Sonata System combines intrauterine sonography with the delivery of RF energy in a single integrated device. The system provides a real-time visualization of fibroids with graphical imaging demonstrating the location of the ablation as well as a thermal safety border beyond which, there is no material thermal effect. Depending on the ablation size, the duration of ablation ranges between 1 and 7 min [Citation14].
The Sonata System is FDA-cleared and CE-marked for treatment of uterine fibroids [Citation15]. Transcervical adenomyosis ablation (TAA) with the Sonata System has not been previously reported. This case series is the first to report the outcomes of TAA with the Sonata System in patients with adenomyoma. For this reason, this case series was undertaken.
Methods and materials
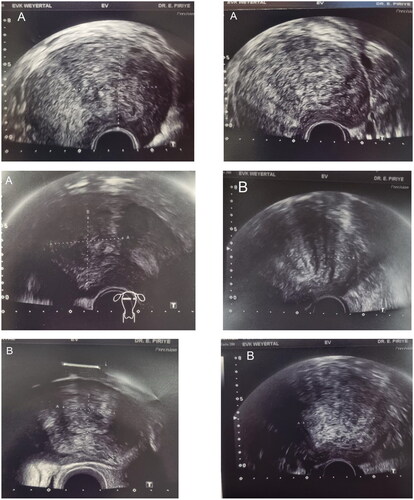
Transcervical fibroid ablation (TFA) is performed by a gynecologist. The instrument has a small ultrasound probe that is to be inserted intrauterine [Citation16]. Before the ablation, the fibroid is determined sonographically. Usually, a general anesthesia is required for TFA. The diameter of the device is 8.3 mm. The fibroid is represented due to graphical navigation. After graphical visualization of fibroid, the ablation is carried out. In this phase, a safety zone guaranteed no thermal injury in the surrounding organs (e.g., bladder and bowel). It is important especially for transmural fibroids that are also located near the bladder and bowels. The procedure allows for optimization of the ablated volume in the targeted fibroid. The puncture of serosa is not necessary. The measurements are registered graphically. The ablation time is 1–7 min depending on the fibroid size (the smallest size of fibroid is 2.0 × 1.3 cm). The temperature of the electrode is about 105 °C. A good knowledge of vaginal ultrasonography and confidence in all other endoscopic fibroid therapy are required, because they can be used at the same time in combination with TRF as needed [Citation15,Citation17]. TFA with the Sonata System has been performed in our department since 2011. In total, 220 patients were treated with Sonata® System in Academic Hospital Cologne Weyertal (Cologne, Germany). An ultrasound follow-up was the routine procedure in each case. In this retrospective case series, patients who were treated in our center with sonographic detected focal adenomyosis and heavy menstruation bleeding were included in this report (). Focal adenomyosis was differentiated from fibroid via transvaginal sonography. Compared with fibroids, adenomyosis lacks distinct margins as they lack pseudocapsules and other demarcations and may contain small cysts that are highly suggestive for adenomyosis [Citation11]. On Doppler imaging, vessels cross focal adenomyosis, while fibroids typically demonstrate peripheral flow [Citation11]. All these criteria were considered for the diagnosis of adenomyosis. We compared the largest diameter in the pre- and postoperative controls. If the findings were reduced and/or the symptoms improved, the ablation was rated as successful. All data are available by the corresponding author. In , some examples of preoperative and postoperative ultrasound imaging are represented.
Figure 2. Preoperative and postoperative ultrasound imaging. (A) Preoperative ultrasound imaging; (B) postoperative ultrasound imaging; DR. E. PIRIYEV: name of the first author; Weyertal: name of the hospital.
A total of 13 patients with 16 areas of focal adenomyosis were treated. We determined some criteria for this analysis: inclusion criteria were: (1) patients with bleeding disorder, (2) sonographic diagnosed focal adenomyosis, and (3) wish to organ preserving method. Exclusion criteria: patients with current fertility desire. All patients provided their standard informed consent for the surgery to undergo TAA treatment with the Sonata System, aware that this method is a safe and established method for fibroid treatment, but the safety and effectiveness of transcervical RF ablation for the treatment of adenomyosis have not been established.
The ablation of focal adenomyosis was performed in the same way as for fibroids and could be performed without any complications in all cases. After placement of the Sonata System, areas of focal adenomyosis were detected using the intrauterine sonography probe integrated within the Sonata handpiece. The central spike was introduced, the ablation zone and safety zone were adjusted and eventually the electrodes were inserted. After rechecking the safety zone, the ablation could be performed after reaching of 105 °C. The use of the Sonata System, in detail, has been explained in detail elsewhere [Citation15,Citation18]. All patients were discharged in good condition.
Ultrasound follow-up was done through six months after the procedure. The last follow-up regarding the improvement of bleeding symptoms was performed by phone contact 14.9 ± 6 month (8–24 month) after the procedure. Patients were asked about their subjective assessment of the improvement of bleeding symptoms and their satisfaction with this method of treatment.
Results
Thirteen patients with focal adenomyosis were treated with TAA ablation with Sonata System. Heavy menstrual bleeding was the main symptom. Eleven patients had one area of focal adenomyosis and three patients had additional at least one fibroid. In total, 20 findings (16 adenomyomas and four fibroids) were treated. In two cases, an operative hysteroscopy was performed: one patient obtained fibroid resection and another patient endometrium resection. The size of area of focal adenomyosis ranged from 2.3 cm to 7 cm in diameter, with average size of 4.2 cm. The patients’ characteristic and preoperative findings are presented in .
Table 1. Patient characteristic and preoperative findings.
All procedures were performed without intraoperative complications. Procedure times ranged from 18 to 56 min with average time of 29.4 min. One case lasted 56 min due to concomitant operative hysteroscopy with fibroid resection. In the majority of patients, more than one ablation cycle was necessary to completely ablate the lesion. Intraoperative parameters are presented in .
Table 2. Intraoperative parameters and postoperative outcomes.
Follow-up was performed after Sonata treatment. At the time of this report, 12 patients had returned for follow-up and one patient could not be reached. Out of 12, 83% of patients reported significant improvement of symptoms. Worsening of symptoms was not reported by any. The average focal lesion size was reduced from 4.2 cm at the time of procedure to 2.8 cm at 6 months post-procedure (). No postoperative complications were observed. All patients reported satisfaction with the procedure. Postoperative outcomes are shown in .
Discussion
The main goal of adenomyosis therapy includes symptom relief and preservation of fertility [Citation16]. A medical therapy is not always appropriate, so surgery can be required, especially in case of focal adenomyosis/adenomyoma. Many patients may desire a uterine preserving treatment option instead of hysterectomy even though hysterectomy is curative.
Regarding uterine preserving treatment of adenomyosis, magnetic resonance-guided focused ultrasound (MRgFUS) is a method that provides thermal ablation to soft tissue and has been used in trials involving relatively small numbers of patients with symptomatic adenomyosis [Citation19]. The results have been positive, particularly in the treatment of focal adenomyosis. However, the treatment time is typically long. Ferrari et al. reported the longest time of adenomyosis treatment with MRgFUS in their work of 3 h [Citation20]. Additionally, MRgFUS is not widely available as a treatment modality.
Transcervical fibroid ablation with Sonata System is a minimally invasive, incisionless, safe and effective method for the treatment of fibroids [Citation21]. Radiofrequency ablation incites coagulative necrosis, resulting in reduced symptoms while conserving the uterus in a safe outpatient manner [Citation15]. The use of TFA in women with symptomatic uterine fibroids has been reported to have a favorable safety profile [Citation17,Citation22]. Operative time of TAA, in contrast to laparoscopy, laparotomy, as well as MRgFUS, was shorter in our experience ().
To the best of our knowledge, this is the first analysis on transcervical RF ablation in patients with focal adenomyosis. In all our cases, the treatment with Sonata system could be performed without any complications. The patients were satisfied with the method. We used this method in patients with symptomatic focal adenomyosis. Improvement in symptoms was reported by the majority of patients (83%) with reduction of lesion size ().
The positive results relating to the improvement of symptoms and reduction of adenomyosis lesion size, both of which were observed in our study, make this method a potential therapeutic alternative in treatment of focal adenomyosis, disease which has limited therapeutic approach.
Limitations of this report include the small number of patients, absence of prespecified clinical protocol, the short follow-up, and absence of histological proof of adenomyosis. A prospect clinical trial to assess safety and effectiveness of TAA for treatment of focal adenomyosis is warranted.
Conclusion
Transcervical RF ablation with the Sonata System may be a promising therapeutic alternative method to conventional procedures, such as hysterectomy for the treatment of focal adenomyosis and may enable a minimally invasive, uterine preserving option.
Author contributions
EP: manuscript writing, data management and data analysis. SS and TR: project development and administration.
Ethical approval
This retrospective protocol was approved by the Ethics Committee of North Rhine Westphalia (protocol number 107/2023). The requirement for informed consent was waived because of the retrospective nature of the study. All patient data were anonymized for the purposes of reporting.
Disclosure statement
EP has no conflict of interest. SS and TR are consultants for the Sonata System. The authors report no other conflicts of interest in this work.
Additional information
Funding
References
- Bourdon M, Santulli P, Marcellin L, et al. Adenomyosis: an update regarding its diagnosis and clinical features. J Gynecol Obstet Hum Reprod. 2021;50(10):102228.
- Peric H, Fraser IS. The symptomatology of adenomyosis. Best Pract Res Clin Obstet Gynaecol. 2006;20(4):547–555.
- Loring M, Chen TY, Isaacson KB. A systematic review of adenomyosis: it is time to reassess what we thought we knew about the disease. J Minim Invasive Gynecol. 2021;28(3):644–655.
- Bergeron C, Amant F, Ferenczy A. Pathology and physiopathology of adenomyosis. Best Pract Res Clin Obstet Gynaecol. 2006;20(4):511–521.
- Novellas S, Chassang M, Delotte J, et al. MRI characteristics of the uterine junctional zone: from normal to the diagnosis of adenomyosis. AJR Am J Roentgenol. 2011;196(5):1206–1213.
- Von Recklinghausen F. Die adenomyome und cytadenome der uterus und tubenwandung, ihre abkunft von resten des wolffschen korpers. Berlin: Hirschwald; 1896.
- Gilks CB, Clement PB, Hart WR, et al. Uterine adenomyomas excluding atypical polypoid adenomyomas and adenomyomas of endocervical type: a clinicopathologic study of 30 cases of an underemphasized lesion that may cause diagnostic problems with brief consideration of adenomyomas of other female genital tract series. Int J Gynecol Pathol. 2000;19(3):195–205.
- Tahlan A, Nanda A, Mohan H. Uterine adenomyoma: a clinicopathologic review of 26 cases and a review of the literature. Int J Gynecol Pathol. 2006;25(4):361–365.
- Zouzoulas OD, Tsolakidis D, Efstratiou I, et al. Correlation between adenomyosis and endometrial cancer: 6-year experience of a single center. Facts Views Vis Obgyn. 2018;10(3):147–152.
- Chapron C, Vannuccini S, Santulli P, et al. Diagnosing adenomyosis: an integrated clinical and imaging approach. Hum Reprod Update. 2020;26(3):392–411.
- O'Shea A, Figueiredo G, Lee SI. Imaging diagnosis of adenomyosis. Semin Reprod Med. 2020;38(2-03):119–128.
- Wang PH, Su WH, Sheu BC, et al. Adenomyosis and its variance: adenomyoma and female fertility. Taiwan J Obstet Gynecol. 2009;48(3):232–238.
- Osada H. Uterine adenomyosis and adenomyoma: the surgical approach. Fertil Steril. 2018;109(3):406–417.
- Lindner LH, Roy K, Toub DB. Transcervical fibroid ablation (TFA) with the sonata system: updated review of a new paradigm for myoma treatment. Curr Obstet Gynecol Rep. 2022;11(3):238–248.
- Toub DB. A new paradigm for uterine fibroid treatment: transcervical, intrauterine sonography-guided radiofrequency ablation of uterine fibroids with the sonata system. Curr Obstet Gynecol Rep. 2017;6(1):67–73.
- Tsui KH, Lee WL, Chen CY, et al. Medical treatment for adenomyosis and/or adenomyoma. Taiwan J Obstet Gynecol. 2014;53(4):459–465.
- Römer T, Bends R, Christoffel L, et al. The significance of transcervical ultrasound-guided radiofrequency ablation in the treatment of symptomatic fibroids: results of an expert consensus from German-speaking countries. Arch Gynecol Obstet. 2022;306(1):1–6.
- Chudnoff S, Guido R, Roy K, et al. Ultrasound-guided transcervical ablation of uterine leiomyomas. Obstet Gynecol. 2019;133(1):13–22.
- Fukunishi H, Funaki K, Sawada K, et al. Early results of magnetic resonance-guided focused ultrasound surgery of adenomyosis: analysis of 20 cases. J Minim Invasive Gynecol. 2008;15(5):571–579.
- Ferrari F, Arrigoni F, Miccoli A, et al. Effectiveness of magnetic resonance-guided focused ultrasound surgery (MRgFUS) in the uterine adenomyosis treatment: technical approach and MRI evaluation. Radiol Med. 2016;121(2):153–161.
- Piriyev E, Schiermeier S, Bends R, et al. Transcervical radiofrequency ablation of fibroids that are 5 cm or larger in women with abnormal uterine bleeding. J Gynecol Obstet Hum Reprod. 2022;51(2):102303.
- Piriyev E, Bends R, Schiermeier S, et al. Transcervical intrauterine radiofrequency ablation of fibroids in high-risk patients with bleeding disorder. Ginekol Pol. 2022;93(8):614–619.