Abstract
Purpose
This study aimed to investigate the safety and efficacy of High-Intensity Focused Ultrasound (HIFU) treatment for vaginal intraepithelial neoplasia(VaIN).
Methods
Retrospective analysis was conducted on clinical, pathological, and follow-up data of 43 patients who underwent HIFU treatment for VaIN at Xiangya Third Hospital of Central South University between January 2018 and December 2022. The preliminary efficacy and safety of HIFU in treating VaIN were discussed.
Results
The 36 patients were analyzed, and the average age was 50.09 ± 12.06 years, including 24 patients with VaIN I and 12 patients with VaIN II. Five cases had a history of hysterectomy (4 due to cervical lesions, 1 due to hysteromyoma), and 2 cases had conization of cervical intraepithelial lesions (CIN). All 36 cases were complicated by human papillomavirus (HPV) infection, with 3 cases also having grade I-II CIN and undergoing cervical HIFU treatment. All patients successfully completed the HIFU treatment, with an average treatment time of 5.99 ± 1.25 min, treatment power of 3.5 W, and average total treatment dose of 1118.99 ± 316.20 J. Patients tolerated the treatment well, experiencing only slight pain with VAS score of 3. There was a mild postoperative burning sensation, which resolved within approximately 10-20 min. After 6 follow-up visits, 33 patients (91.66%) achieved cure, 1 patient (2.77%) showed persistence, 2 patients (5.55%) exhibited progression, and 27 patients (75%) tested negative for HPV. At 12 months of follow-up, the results were consistent with those of 6 months. No complications occurred during the procedure and the follow-up period.
Conclusion
HIFU is a safe and effective treatment for VaIN. However, this study had a small sample size, a relatively short follow-up period, and lacked a control group, requiring further investigation.
Introduction
Vaginal intraepithelial neoplasia (VaIN) refers to abnormal cell growth within the vaginal epithelium, ranging from mild to severe dysplasia. VaIN is primarily considered a precancerous condition preceding vaginal invasive cancer, and its development is often associated with persistent infection of high-risk human papillomavirus (HPV) [Citation1]. The incidence of VaIN is relatively low, with reported rates ranging from 0.2 to 2 per 100,000 women per year. However, with the increasing availability of cervical lesion screening and diagnostic techniques, the detection rate of VaIN has been steadily rising, leading to increased attention toward its diagnosis and treatment. Currently, there is no standardized clinical protocol for the management of VaIN, and treatment can be challenging, particularly when lesions are located in proximity to the bladder and rectum, resulting in high recurrence rates. Surgical interventions, especially for wide-ranging lesions, can cause significant damage and impact vaginal function. Therefore, there is an urgent need for minimally invasive and effective treatment modalities in clinical practice. High-Intensity Focused Ultrasound (HIFU) technology has emerged as a noninvasive treatment approach widely employed in gynecology. Its applications include the treatment of cervical erosion, genital HPV infection, vulvar intraepithelial neoplasia, and other lower genital tract diseases. However, there is currently no literature available regarding the use of HIFU in the treatment of VaIN. This retrospective analysis examines the clinical data of 36 VaIN patients treated with HIFU to explore the efficacy and safety of HIFU in managing VaIN.
Information and methodology
Study subjects
Thirty-six patients diagnosed with VaIN I or VaIN II at Xiangya Third Hospital of Central South University between January 2018 and December 2022 were selected as study subjects. Clinical, pathological data, and follow-up results were collected.
Inclusion criteria:
All patients underwent Thinprep Cytologic Test(TCT) and HPV screening before the operation, followed by colposcopy biopsy for pathological diagnosis of VaIN I or VaIN II.
Prior to treatment, patients had a comprehensive understanding of their condition and various treatment options, agreed to receive HIFU treatment, and signed informed consent forms.
Patients with complete clinical, pathological, and follow-up data.
Patients who did not receive other VaIN or cervical intraepithelial lesions(CIN) physical therapies within the past 3 months.
Exclusion criteria:
Patients who were unable to complete follow-up due to severe illness or accidents.
Patients who were lactating or pregnant during the follow-up period.
Treatment methods
The treatment equipment used was the CJF300 ultrasonic focusing therapeutic instrument manufactured by Chongqing Haifu Medical Technology Co., Ltd. After the diagnosis of vaginal biopsy under colposcopy, treatment was scheduled during a clean period of menstruation (postmenopausal patients could be treated at any time). Vaginal secretions were examined to exclude acute inflammation of the genital tract before treatment. The patient emptied their bladder prior to the procedure and assumed the bladder lithotomy position. The vulva and vagina were disinfected with an iodine complex. The vaginal speculum exposed the vagina and cervix. Based on the colposcopy results, the vaginal wall and cervix were coated alternately with 3%-5% acetic acid solution and iodine solution to determine the extent of the lesions. Local infiltration anesthesia was performed using a 1:1 dilution of 2% lidocaine. If the lesion was located on the anterior and posterior walls of the vagina, adjacent to the rectum and bladder, approximately 10-30ml of normal saline could be injected under the mucosa to create a water cushion before treatment. The treatment parameters were as follows: power 3.5 W, frequency 9.5 MHz, pulse 1000 Hz. A special coupling agent was utilized as the conduction medium, and the treatment head was positioned close to the pathological area of the vaginal wall. The scanning speed was set at 5-10 mm/s. The treatment range extended 0.5-1 cm beyond the pathological area and its edges. The treatment duration depended on the size and severity of the pathological area. Treatment was terminated when the vaginal wall mucosa exhibited slight congestion and edema, and the vaginal wall wrinkles became slightly shallow. Following treatment, the vaginal wall was locally cooled with gauze for 5 min. Vulvar hygiene was emphasized within 1 month after treatment, and activities such as sexual intercourse and bathing were to be avoided.
Figure 1. Endoscopic images of patients with VaIN I before and after treatment are shown in . (a) Represents the appearance of the lesion site before treatment when 3% glacial acetic acid was applied. (b) Shows the lesion site before treatment when Lugol’s iodine solution was applied for recurrent staining. (c) Displays the lesion site after 6 months reexamination following treatment when 3% glacial acetic acid was applied. Finally, (d) demonstrates the lesion site after half a year’s reexamination following treatment when Lugol’s iodine solution was applied. The blue arrow indicates the location of the lesion in the images.
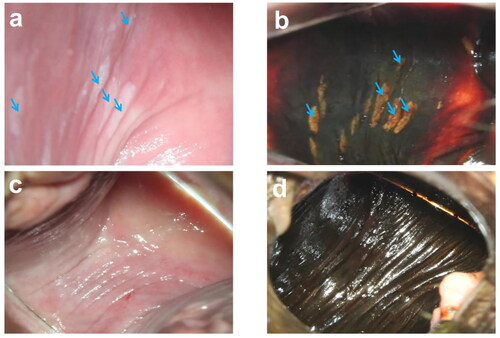
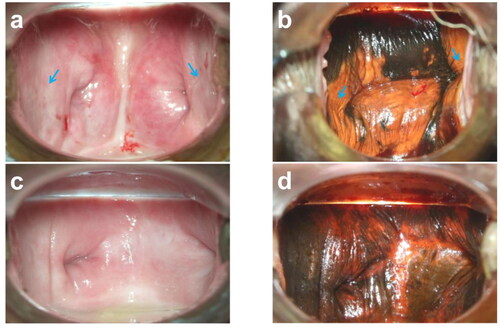
Figure 2. Endoscopic images of patients with vaginal stump VaIN I before and after treatment are presented in . (a) Shows the appearance of the lesion site before treatment when 3% glacial acetic acid was applied. (b) Displays the lesion site before treatment when Lugol’s iodine solution was applied for recurrent staining. After half a year’s reexamination following treatment, (c) exhibits the lesion site when 3% glacial acetic acid was applied. Finally, (d) demonstrates the lesion site after half a year’s reexamination following treatment when Lugol’s iodine solution was applied. The blue arrow indicates the location of the lesion in the images.
Observation and follow-up
During treatment, the treatment time, total power, patient pain (measured using the VAS score), and adverse reactions were observed and recorded. Short-term and long-term complications were assessed during follow-up visits at one month, three months, six months, and twelve months after treatment. Each visit involved evaluating abnormal symptoms such as vaginal bleeding, vaginal secretions, and the healing of vaginal wall wounds. HPV and TCT examinations were conducted at the six-month and twelve-month follow-up visits. If abnormalities were detected, colposcopy and biopsy were performed if necessary.
Efficacy assessment
Cure: Normal TCT and HPV screening results were observed at 6 or 12 months after treatment, or colposcopy biopsy confirmed the absence of VaIN.
Persistent lesion: The lesion grade confirmed by colposcopy biopsy remained the same as before treatment.
Pathological progress: Colposcopy biopsy confirmed a higher pathological grade compared to the initial diagnosis.
Statistical analysis
Data analysis was performed using SPSS 25.0. Measurement data were described as (X ± s), and categorical data were presented as frequencies and rates.
Results
General data
A total of 43 patients were included, with 7 lost to follow-up.The study enrolled 36 patients diagnosed with VaIN through colposcopy biopsy. Among them, 24 cases were classified as VaIN I and 12 cases as VaIN II. Five patients had a history of total hysterectomy (4 due to cervical lesions and 1 due to uterine fibroids), and 2 patients had a history of cervical conization (see ). Among the lesions, 33 cases were classified as simple VaIN, and 3 cases were classified as CIN (all CIN I-II, and focused ultrasound treatment was performed simultaneously during the operation). All patients were found to have high-risk HPV infection ().
Table 1. Case data characteristics of VaIN patients.
Clinical efficacy
All patients successfully completed focused ultrasound treatment, with an average ablation time of 5.99 ± 1.25 min and an average ablation dose of 1118.99 ± 316.20 J. At the six-month follow-up, 36 patients completed the assessment, with 33 patients (91.66%) cured, including VaIN I 23(95.83%) and VaIN II 10(83.33%). 1 patient showing persistent disease, who was classified as VaINII.2 patients showing progressive disease, including VaIN I 1 and VaIN II 1.At the twelve-month follow-up, 36 patients completed the assessment, with 33 patients (91.66%) cured, including VaIN I 23(95.83%) and VaIN II 10(83.33%). 1 patient showing persistent disease, who was classified as VaINII, and then she received medication treatment and closely followed up for observation.2 patients showing progressive disease, including VaIN I 1 and VaIN II 1, and finally, they underwent surgical resection treatment.At twelve months after treatment, HPV turned negative in 27 patients. During the follow-up period, the cured cases showed no recurrence ().
Table 2. Effect of HIFU on VaIN.
Adverse reactions
The common adverse reactions during HIFU treatment include pain, ulceration, bleeding in the treated area, and damage to surrounding organs.Besides, in VaIN treatment, there may be vaginal discharge, vaginal infections, vaginal contracture, and impact on sexual activity.During treatment, VAS pain scores were 3 points and none of those adverse reactions occurred, as pertinent negatives.A slight burning sensation was experienced after the procedure, which subsided within 10-20 min. Throughout the follow-up period, none of the patients experienced those adverse reactions.
Discussion
VaIN, which is a precancerous lesion of vaginal cancer, as an intraepithelial lesion of the lower genital tract, has a significantly lower incidence compared to cervical intraepithelial neoplasia (CIN). The management of VaIN I often involves a conservative approach with follow-up observation due to its potential for disease reversal [Citation2]. However, this method is associated with a high recurrence rate, and some VaIN I patients may experience disease progression, leading to substantial psychological burden. On the other hand, vaginal high-grade squamous intraepithelial lesions (HSIL) and VaIN cases associated with CIN or squamous cell carcinoma (SCC) are considered high-risk conditions with a high likelihood of progressing to invasive cancer and a high recurrence rate.
Currently, various treatment modalities are available for VaIN. ①Laser ablation; Freitas et al. [Citation2] reported that laser ablation is suitable for multifocal lesions in sexually active young women with a cure rate up to 90% and recurrence rate up to 6.3%. ②Drug therapy, such as Imiquimod 5% and 5-Flouorouracil, have a good therapeutic effect, low pharmacological morbidity, and 25%-98% cure rate, 11.1%-75% persistence rate and 5.6%-94.4% recurrence rate. Drug therapy is commonly employed for young or multifocal VaIN cases and has shown positive results. However, it is associated with a lengthy treatment course, potential drug side effects, and poor patient compliance. ③Intravaginal radiotherapy can be 71.4%-90% efficient with and 20% of recurrence rate. ④Physical therapy, such as CO2 laser, cryotherapy, and electric ablation, have emerged. However, these methods still pose risks and may have a high recurrence rate. ⑤Surgical resection can be detrimental to vaginal health and impact normal vaginal function.There is an need for a safe and effective treatment approach for VaIN.
The principle of high-intensity focused ultrasound (HIFU) therapy is based on the use of ultrasound as a mechanical vibration wave. Ultrasound, as an energy source, possesses the ability to penetrate living tissues without causing damage. HIFU utilizes the penetrative, localized, and focused properties of ultrasound to treat various diseases [Citation3]. The ultrasound beam generated by the ultrasound transducer can pass through the skin and soft tissues, focusing the energy beam onto the targeted lesion tissue. When the energy at the focal point is sufficiently high, thermal necrosis occurs in the lesion tissue, leading to irreversible cell death [Citation4]. HIFU is a noninvasive treatment modality known for its high maneuverability, making it widely used in surgery and gynecology, including the management of lower genital tract diseases. Studies have demonstrated that HIFU therapy achieves high efficacy rates ranging from 93% to 98% in the treatment of vulvar intraepithelial neoplasia [Citation5,Citation6]. Furthermore, focused ultrasound treatment has been established as an effective approach for chronic cervicitis. Clinical investigations have confirmed that HIFU therapy yields excellent results, with a 100% effective rate for mild cervical erosion, 95.2% for moderate erosion, and 91.7% for severe erosion, resulting in an overall effective rate of 94.7% [Citation7].
Furthermore, HIFU has also been utilized for the treatment of cervical intraepithelial neoplasia (CIN), particularly in patients with fertility requirements. Zeng et al. [Citation8] conducted a study on the efficacy of HIFU in 154 cases of CIN. The results showed a post-treatment efficacy of 96.8% at 3-6 months, with a disease persistence rate of 3.2%. No cases demonstrated disease progression during the 3-6 month post-treatment period, and the recurrence rate was 2.0% at 6-12 months. Notably, no significant side effects were observed following treatment. The mechanism of action of HIFU may be attributed to its ability to improve the local immune microenvironment of the cervix to some extent.Liu et al. [Citation9] reported on a prospective study involving 29 cases of CIN2/3 treated with HIFU. The study demonstrated a cure rate of 72.4% at 7 months post-treatment, 96.6% at 1 year post-treatment, and a 72.4% HPV negative rate at 6 months post-treatment. Since the pathogenesis of VaIN is similar to that of CIN, and HPV infection is one of its high-risk factors [Citation10], HIFU may be equally effective in the treatment of early-stage VaIN, particularly when coexisting with CIN. In our study involving 36 VAIN patients, all individuals were treated with HIFU. Follow up for 6 months, 33 cases were cured, and follow up for 12 months, 33 cases remained cured. During the follow-up period, no recurrences were observed, and 27 patients tested negative for HPV infection, providing preliminary evidence supporting the effectiveness of HIFU in treating VaIN. Additionally, due to the large treatment range of HIFU, it is possible to irradiate the surrounding area of the focal point, eliminating HPV infection even in areas without visible lesions, thus reducing the risk of recurrence.
In this study, all patients received outpatient treatment, experiencing minimal pain and requiring no hospitalization. The treatment was well-tolerated and showed good patient compliance. No complications, such as increased vaginal secretions, bleeding, infection, vaginal contracture, or adverse effects on sexual function or surrounding organs, were observed during or after the treatment.HIFU has the potential for thermal, cavitation, and mechanical effects that could cause tissue damage and necrosis [Citation11]. It’s important to keep in mind that the vaginal wall thickness varies in different segments [Citation4,Citation12], but HIFU should not cause scarring because the current treatment depth is thought to be approximately 4-6 mm below the mucosal surface [Citation3].
In cases where the lesion involves the anterior and posterior walls of the vagina, special attention should be given to the treatment time and power while combining the vaginal mucosa with a water cushion to minimize the risk of bladder and rectal damage. However, in postmenopausal patients, careful consideration should be given to the atrophy and thinning of the vaginal mucosa. It is important to fully form a water cushion and appropriately adjust the treatment time and power to ensure optimal outcomes while reducing the potential for adverse effects.
In conclusion, this study provides preliminary evidence supporting the effectiveness and safety of HIFU as a treatment option for VaIN. However, it is important to note that the study had a small sample size, lacked a control group, and had a relatively short follow-up period. Therefore, further extensive research is necessary to validate these findings. Firstly, we may need prospective clinical trials to explore more suitable HIFU treatment parameters for VaIN, for example, treatment depth. We need to follow up patients long term after treatment to observe the effectiveness of treatment and complications.Additionally, the cylindrical HIFU probe used for cervical lesion treatment did not fit perfectly with the surrounding vaginal wall, and the pathological changes in the vaginal wall were relatively superficial. Therefore, after confirming the safety and effectiveness of HIFU, if it is to be implemented as a standard clinical method for VaIN treatment, the development of a more suitable HIFU treatment probe is desirable to improve convenience and safety during the procedure.
Authors’ contributions
Susu Wu, study design, date collections, date analysis, writing. Xiang Li, date collections. Dabao Xu, study design. Mingzhu Ye, study design, writing.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data are made available by the authors on request without undue reservation. Data openly available in a public repository. The data that support the findings of this study are openly available in https://doi.org/10.6084/m9.figshare.24899691.v1
Additional information
Funding
References
- Serrano B, de Sanjosé S, Tous S, et al. Human papillomavirus genotype attribution for HPVs 6, 11, 16, 18, 31, 33, 45, 52 and 58 in female anogenital lesions. Eur J Cancer. 2015;51(13):1–5. doi: 10.1016/j.ejca.2015.06.001.
- Freitas G, Costa A. Non-Excisional therapeutic modalities in vaginal intraepithelial neoplasia. Eur J Obstet Gynecol Reprod Biol. 2023;284:175–179. doi: 10.1016/j.ejogrb.2023.03.014.
- Li C, Bian D, Chen W, et al. Focused ultrasound therapy of vulvar dystrophies: a feasibility study. Obstet Gynecol. 2004;104(5 Pt 1):915–921. PMID: 15516378. doi: 10.1097/01.AOG.0000139835.34168.b0.
- Huang M, Wang Y, Xu J, et al. Assessing vaginal wall indexes in premenopausal versus postmenopausal women by transrectal linear array high-frequency probe. Eur J Med Res. 2023;28(1):390. doi: 10.1186/s40001-023-01378-y.
- Feng T, Wang L, Zhu D, et al. Factors influencing the clinical efficacy of high-intensity focused ultrasound in the treatment of non-neoplastic epithelial disorders of the vulva: a retrospective observational study. Int J Hyperthermia. 2021;38(1):1457–1461. doi: 10.1080/02656736.2021.1985628.
- Wu C, Zou M, Xiong Y, et al. Short- and long-term efficacy of focused ultrasound therapy for non-neoplastic epithelial disorders of the vulva. BJOG. 2017;124 Suppl 3:87–92. PMID: 28856863. doi: 10.1111/1471-0528.14747.
- Xiao YB, Sun LJ. Therapeutic effects of focused ultrasound on chronic cervicitis and the influencing factors. Zhonghua Fu Chan Ke Za Zhi. 2007;42(1):14–17.
- Zeng H, Liu M, Xiao L, et al. Effectiveness and immune responses of focused ultrasound ablation for cervical intraepithelial neoplasia. Int J Hyperthermia. 2022;39(1):539–546. doi: 10.1080/02656736.2022.2052365.
- Liu Y, Wang W, Zhang M, et al. High-Intensity focused ultrasound for patients with cervical intraepithelial neoplasia 2/3: a prospective one-Arm study. Ultrasound Med Biol. 2023;49(1):375–379. doi: 10.1016/j.ultrasmedbio.2022.09.020.
- Zhang YY, Xia R, Chen D, et al. Analysis of related factors of cervical intraepithelial neoplasia complicated with vaginal intraepithelial neoplasia. Clin Transl Oncol. 2022;24(5):902–908. doi: 10.1007/s12094-021-02739-x.
- Bachu VS, Kedda J, Suk I, et al. High-Intensity focused ultrasound: a review of mechanisms and clinical applications. Ann Biomed Eng. 2021;49(9):1975–1991. doi: 10.1007/s10439-021-02833-9.
- Alcazar JL, Para E, Tomaizhe A, et al. Vaginal wall thickness as potential biomarker of vaginal health. A proposal for standardized ultrasound measurement using three-dimensional transvaginal ultrasound. J Clin Ultrasound. 2023;51(8):1366–1369. doi: 10.1002/jcu.23547.

