Abstract
Many patients referred for psychodynamic psychotherapy are also seen by other services. Due to the complex interplay between psychological distress, physical symptoms and care-seeking behaviour, engagement with a psychotherapy department has the potential either to increase or decrease use of other services. This service evaluation compared 268 patients’ service use in the year preceding and following contact with an NHS psychodynamic psychotherapy department using t-tests. There were no significant changes from before therapy to afterwards for the sample as a whole. However, for sub-groups who made regular use of services at baseline, a full course of psychotherapy (16+ sessions) was associated with a statistically significant reduction in outpatient contacts, both for mental health (N = 32, mean 11.69 appointment per year pre-therapy vs 5.16 post-therapy, p = 0.01) and medical services (N = 23, from mean 9.65 to 3.00, p < 0.01). No compensatory changes were found in either A&E or inpatient contacts, suggesting this represents an overall reduction in service use. Due to the study design, it was not possible to establish causality; there may be other reasons for this observed reduction such as natural illness course. These findings tentatively support the existing literature that psychodynamic psychotherapy is associated with a reduction in use of wider services.
Introduction
The indirect economic cost of mental health problems is estimated to be £70-£100 billion each year in the UK (Department of Health, Citation2014). In terms of the direct funding of services in Scotland, where the present study took place, in 2021–22 £1.1 billion (7%) was allocated for mental health services, out of £16 billion allocated for the overall health portfolio (Scottish Govenment, Citation2021). People who experience marked states of anxiety use general medical services more frequently than those without pronounced anxiety (Candilis & Pollack, Citation1997), as do patients with medically unexplained symptoms (Kleinstäuber et al., Citation2011).
Psychodynamic psychotherapy has been shown to be as efficacious as other forms of therapy in the treatment of people with a variety of mental health presentations (Steinert et al., Citation2017). It is hypothesised that these benefits may translate into a reduction in mental health service use. Given the focus of psychodynamic psychotherapy on interpersonal relationships, it is plausible that, as individuals become more aware of these dynamics, those who use healthcare services in order to meet their interpersonal needs may find other ways of doing so, as well as experiencing a reduction in somatic complaints. Conversely, psychotherapy may enable some individuals to ask for more help, leading to an increase or shift in service use. Understanding these effects is helpful for both service evaluation and service planning.
Several previous studies have shown that psychological therapies are cost-effective treatments, partly due to their effect in reducing overall healthcare utilization. A systematic review by Gabbard and Hornberger (Citation1997) concluded that psychotherapy (broadly defined) is associated with reduced duration (and frequency) of inpatient stays for patients with a variety of difficulties, but recommended more data be collected on both inpatient and outpatient care. A more recent Israeli study (Yonatan-Leus et al., Citation2020) showed an increase in health service use in the year prior to accessing psychodynamic psychotherapy, with a sustained reduction following cessation of treatment. A similar pattern of rising costs prior to a course of therapy (CBT, psychodynamic or psychoanalytic), followed by a sustained reduction in outpatient and inpatient service use, was found in Germany by Altmann et al. (Citation2016). Abbass et al. (Citation2015) also found an overall reduction in healthcare costs in the three years following a course of intensive short-term dynamic psychotherapy in Canada. In England, a cost-benefit analysis in 2007 estimated that the costs of fully implementing NICE guidance regarding access to CBT would be fully recovered within two to five years, although economic savings to the NHS were estimated using data from the USA (Layard et al., Citation2007). A similar Canadian study concluded that every $1 invested in psychological services would yield $2 in savings to society (Vasiliadis et al., Citation2017). However, other studies have not found any relation between psychotherapeutic treatment and healthcare utilization (Lazar et al., Citation2006).
These studies examined a wide range of psychotherapeutic modalities (e.g., CBT, psychodynamic therapy, family interventions), with varying durations, and used a variety of outcome measures (e.g., patient-reports, medication use, hospital admissions). Many did not distinguish between mental health and medical service use, or attempted to assess an overall economic saving (potentially masking compensatory effects). The majority of these studies were conducted in countries other than the United Kingdom, and results may therefore not be applicable due to differences in population demographics, cultural views, access to psychotherapy, or healthcare structures.
Given this dearth of specific evidence, we examined how the important issue of service usage applied to our local situation by evaluating how frequently patients used wider NHS services before and after attending the Psychotherapy Department in Edinburgh. The aim of this project was to examine any association between contact with the Psychotherapy Department and patients’ wider service use. Our main hypothesis was that a treatment course of psychotherapy would be associated with an overall reduction in service use.
Methods
Local service
We are a small department providing a psychodynamic psychotherapy service for NHS Lothian (the health board in which Edinburgh is located), which has a population of circa 900,000. The service has three core roles: reflective practice and consultation for staff; teaching and training; and a clinical service. This paper pertains to the latter role. Referrals are particularly invited for people seeking help with relational difficulties:
whose clinical presentation does not easily fall into a well-defined category; and/or
where it is felt that the ways in which they relate to offered care has interfered with their treatment; and/or
who are suitable for psychological therapy but have not benefited from other types of psychological therapies
Approximately two-thirds of patients are referred from secondary care mental health services, with the majority of the remainder from GPs. A previous study of a subset of 303 patients referred to the department who had a history of childhood sexual abuse, found that patients scored highly (i.e., severe) on the Symptom Checklist 90 for depression, interpersonal sensitivity, anxiety and obsessive-compulsive symptoms (Bak-Klimet et al., Citation2014).
Patients are initially seen for a psychodynamic consultation with an experienced psychotherapist, usually over two to three sessions. Through this interaction, patients have space to talk and think about themselves, their relationships, and their current predicament. A relational formulation of their difficulties is developed which is discussed with the patient. For some people, this experience can provide what they are looking for at this point in time and their care may be returned to their GP or referrer after consultation. If a psychodynamic therapeutic consultation is found not to be helpful or suitable, the patient is helped to think about other approaches that may be better suited to their needs.
Some patients go on to have a longer course of psychodynamic sessions. The majority of our further treatment is provided by doctors in training who deliver psychodynamically-oriented therapy under weekly supervision with a senior colleague. There is more limited availability for individual psychodynamic therapy or group psychotherapy delivered by Adult Psychotherapists or Consultant Psychiatrists in Psychotherapy. The standard length for further treatment in the department is six or 12 months. This may be longer in group therapy. Whilst the Psychotherapy Department does see in-patients for consultation, the vast majority of its direct clinical service work is with out-patients.
Data collection
Anonymized data were retrospectively provided by the NHS Lothian eHealth department for patients who had been offered appointments in the NHS Lothian psychotherapy department between July 2014 and December 2017. We were provided with each patient’s number of contacts with the psychotherapy department per quarter. This included patients treated by trainee psychiatrists and experienced psychotherapists, as well as patients in group therapy.
Anonymised information about these patients’ wider service use was provided between January 2012 and March 2018 in the form of number of contacts with each service per quarter (medical and mental health outpatient contacts; medical and mental health inpatient admissions; A&E presentations). These figures included all contacts with secondary care, excluding psychodynamic psychotherapy appointments.
Data were extracted for patients who met these eligibility criteria:
Contact with the psychotherapy department commenced after 1st October 2014 and ended before 31st March 2017. This ensured a full data set for wider service use for one year preceding first contact with the department and one year following final contact. A change in computer system for psychiatric services during July-September 2014 meant some of the psychotherapy department contact data were ambiguous, and this period was therefore excluded from the psychotherapy data set.
Attendance for at least one psychotherapy appointment during the study period
For patients included in the study, service use data were collected for the year prior to contact with the department, the period during contact (converted to per annum for comparison) and the year following the end of their contact with the department. Regular contact with services at baseline was defined as 4+ mental health or medical outpatient appointments within that year. A full course of therapy was defined as 16+ sessions: this was felt to represent realistic attendance for someone receiving regular therapy for six months or longer. In addition, structured psychodynamic therapies (eg. Dynamic Interpersonal Therapy) have protocols of this duration (Lemma et al., Citation2011, p. 63).
Statistical analysis
We compared the number of outpatient contacts (both mental health and medical) in the year before therapy with the year following therapy for patients who undertook a course of psychodynamic therapy with the psychotherapy department. We repeated this comparison with a sub-group of patients in regular contact with services at baseline.
We also compared the number of contacts for both hospital admission and A&E attendance before and after psychodynamic therapy, to examine if any change in either of the primary measures is associated with compensatory effects elsewhere in the system. Finally, for patients who attend for a consultation only (defined as three sessions or fewer), we observed their use of wider services pre and post consultation.
Data were entered into MS Excel and analysed using paired, two-tailed t-tests to compare an individual’s service contact before and after their psychotherapy experience. A small number of outliers were noted with particularly high figures for mental health outpatient contact (>100 per annum) and a sensitivity analysis was performed excluding these patients.
Ethical approval
As all data were anonymised, non-identifiable, and routinely collected, and no changes were made to patients’ treatment, formal ethical approval and participant consent were not required for this service evaluation. The project was registered with the local quality improvement team for governance and oversight purposes.
Results
Of the 746 patients for whom data was initially provided, 268 met these criteria. Of the patients not included in the sample, 94 did not attend appointments offered to them and 384 had contact which started and/or ended outwith the study period. Due to the fully anonymised nature of the sample, no clinical or demographic are available for this specific sample. General characteristics of patients referred to the service have been mentioned above.
Descriptive statistics
A total of 119 patients attended the department for consultation only (1–3 sessions), 64 patients for a partial course of therapy (4–15 sessions), and 85 patients for a full course of therapy (16+ sessions). The mean [SD] durations of therapy for these groups were: consultation only, 1.66 [0.70] sessions over 1.46 [0.78] quarters; partial course of therapy, 9.99 [3.78] sessions over 3.88 [1.55] quarters; full course of therapy, 26.11 [13.16] sessions over 5.26 [1.70] quarters.
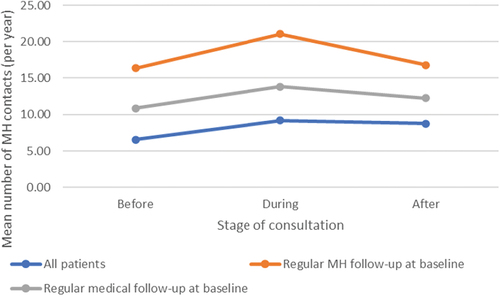
Ninety-seven patients (36%) were in regular contact with mental health services in the year prior to contact with the department and seventy-two (27%) were in regular contact with medical services during this period. These groups appeared comparable in terms of proportion of patients who received partial or full treatment courses ().
Table 1. Proportion of patients undertaking a consultation only, a partial course of therapy, or a full course of therapy.
Comparing service use before and after psychotherapy
There were no statistically significant changes in patients’ use of mental health or medical outpatient services from pre- to post-therapy, for either full or partial courses of therapy ().
Table 2. Mean outpatient contacts before and after therapy with the psychotherapy department.
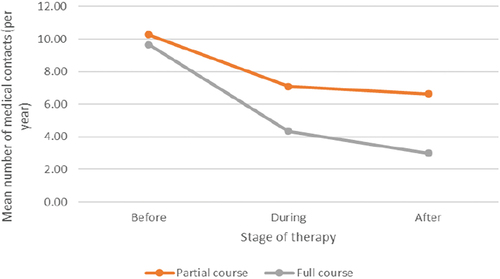
Examining the sub-group who had regular contact with outpatient mental health services at baseline, those who attended for a full course of therapy (n = 32) showed a statistically significant (p = 0.01) reduction in outpatient mental health contacts from mean 11.69 per year (95% CI 8.4–15.0) to mean 5.16 (0.35–9.96) ( and ). For those attending a partial course of therapy, there was no statistically significant change from pre- to post-therapy. However, on visual inspection of the data, the number of mental health contacts appeared to reduce during therapy (from mean 12.55 (95% CI 7.74–17.35) to 7.93 (3.65–12.21); p = 0.03), before rising slightly post-therapy (albeit not as high as pre-therapy) ().
Figure 1. Mean number of mental health contacts before, during and after partial and full courses of therapy for sub-group with regular mental health appointments at baseline.
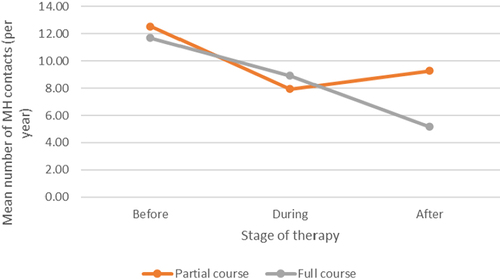
Table 3. Mean outpatient contacts before and after therapy with the psychotherapy department for sub-groups with regular mental health or medical appointments at baseline.
Examining the sub-group who had regular contact with outpatient medical services at baseline, those who attended for a full course of therapy (n = 23) showed a statistically significant (p < 0.01) reduction in medical outpatient appointments from mean 9.65 (6.4–12.9) to 3.00 (0.8–5.3) ( and ). There was a smaller non-significant reduction for those attending for a partial course ().
Hospital admission and A&E attendance
No significant changes in A&E presentations or inpatient admissions were associated with any changes in the primary measures ().
Table 4. Mean numbers of A&E presentations and inpatient admissions before and after therapy with the psychotherapy department.
There was also no statistically significant change in patients’ use of services from pre- to post- consultation for patients who had a consultation only ( and supplementary data).
Sensitivity analysis
A small number of outliers were noted (n = 3) had particularly high mental health outpatient contact either before or after contact with the department. Repeat analyses excluding these patients did not change our findings. There were no outliers noted with particularly high medical outpatient contacts.
Discussion
The main finding of this project was that a full course of psychodynamic psychotherapy (defined as 16+ weekly sessions) was associated with a statistically significant reduction in outpatient contacts (both mental health and medical) for those who made regular use of services at baseline. The fact that these reductions were not mirrored by increased contact elsewhere in the system suggests this represents a genuine reduction in overall service use. Due to the design of the study, it is not possible to establish causality, and there may be other reasons for this observed reduction (e.g., concomitant medication treatment or natural illness course).
Although these findings were not replicated when examining the study group as a whole, this may be, at least in part, due to the whole sample including a high proportion of patients who were referred directly from primary care, and therefore had no or minimal contact with secondary care services in the year prior to their course of therapy (i.e., a ‘floor effect’). It is possible that this population has had significant contact with primary care during this time, but these data were not available to us.
The data also tentatively suggest that the pattern of service use for patients undertaking a partial course of therapy may be different compared to those receiving a longer course. For people who had regular mental health follow-up at baseline, we observed a statistically significant reduction in mental health contacts during a partial course of therapy, with these slightly increasing again towards (but not reaching) baseline in the year following cessation of therapy. It is possible that, for some patients at least, a shorter duration of contact provided temporary containment without necessarily deeper psychological change, which they then sought to replicate elsewhere once therapy ended. This would be in keeping with the broader literature which suggests that longer courses of psychodynamic therapy are more effective (Leichsenring & Rabung, Citation2008) and that effects may increase in the post-termination phase (Fonagy et al., Citation2015).
In the secondary objective which pertained to people who had a consultation only, we noted that in the raw data, the mean frequency of service use was higher post-consultation. However, the change was not statistically significant so there is insufficient evidence to support this as a genuine finding. A more specific research project would be needed to explore this further and investigate any causal relationship which may exist (see further research, below). Our clinical observation is that patients who have a ‘consultation only’ constitute a more distressed group, often presenting in an emergent crisis, and who are not in a position to undertake longer term psychodynamic work at the time of referral. If so, it would not be surprising if this group required additional support and containment from wider services. Equally, a more detailed research project could explore whether, for a proportion of patients, a psychodynamic consultation might bring about increased service use elsewhere. This might be due to patients becoming more aware of psychological components of their difficulties for which they then pursue other psychiatric or psychological treatments.
Strengths and limitations
Unlike studies which attempt to review the effect of multiple different forms of psychotherapy on healthcare utilization, this project focuses exclusively on the provision of psychodynamic psychotherapy within one publicly-funded service. The breakdown of patient contacts by type of service also allows us to consider shifts in service use which may be masked by an overall cost-effectiveness study, but which are nonetheless important for healthcare service design and planning. The retrospective design of the study afforded a full data set, patients were included regardless of diagnosis or number of health problems, and therapy was provided by both experienced therapists and psychiatric trainees. All of this allows the results to be more easily applied to the ‘real world’ setting of a publicly funded psychodynamic psychotherapy service.
However, the advantages of these focused, real-world, routinely collected data also present some limitations. As this project was designed for service evaluation, there was no randomisation process or control group. Consideration was given to the comparison of those proceeding to treatment with those attending for consultation only; however, selection bias would likely render these groups incomparable. The fact that many of the observed differences in means were not statistically significant may reflect the relatively small sample sizes involved; this may be improved by a longer study period involving a greater number of patients. Thus, it is difficult to conclude whether a lack of change observed in the present study is a true lack of effect or whether it results from type-2 error.
Due to the anonymized nature of the data provided, we are unable to ascertain the reasons that individual patients did not continue to therapy from consultation or received a curtailed treatment course, nor are we able to establish whether patients received other treatment during this time (e.g., medication). The absence of demographic information available to us is likewise does not allow us to assess if the different subgroups are comparable. As mentioned above, we also recognise that our data do not include information from general practice, and we are therefore unable to establish whether psychotherapy was associated with any changes in how often patients attended primary care. Likewise, numbers of A&E presentations and inpatient admissions are too small to draw any firm conclusions regarding these services, although it is reassuring in terms of safety that no large increases in use of these services were observed.
Implications for clinical practice and research
These findings tentatively support the existing literature that psychodynamic psychotherapy contributes to a genuine reduction in service use. Greater sample sizes are needed to assess the impact of psychodynamic therapy on A&E and inpatient admissions.
In addition, this project has raised interesting questions about possible patterns of service use in people who have partial courses of therapy or undertake a psychodynamic consultation only. A more specific research study – as opposed to a service evaluation – would be required to investigate how the various non-statistically significant observations in this paper are borne out in larger, adequately powered, studies. Such a research study would have the ability to invite patients referred for psychodynamic therapy into an observational study aiming to track the influence of shorter versus longer durations of contact with a psychotherapy service and understand in more detail patients’ journeys through the healthcare system. Such a study could employ mixed methods, adding qualitative interviews with patients to quantitative outcome measures and data about service use, to try and piece together a person’s relationship with different parts of the healthcare system over time.
In conclusion, psychodynamic psychotherapy may be effective in reducing overall service use by patients who are regularly seen in medical or mental health outpatient departments, and should be considered as part of an overall treatment plan for this population. Further research is needed to quantify this effect and explore wider impacts and cost implications.
Supplemental Material
Download MS Excel (11.8 KB)Disclosure statement
Adam Polnay currently works in the NHS Lothian Psychotherapy Department, where this service evaluation took place. Naomi Entwistle has previously worked in the Psychotherapy Department, and Tom Russ currently has links to the Department.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/02668734.2022.2147580
Additional information
Funding
References
- Abbass, A., Kisely, S., Rasic, D., Town, J. M., & Johansson, R. (2015). Long-term healthcare cost reduction with intensive short-term dynamic psychotherapy in a tertiary psychiatric service. Journal of Psychiatric Research, 64, 114–120. https://doi.org/10.1016/j.jpsychires.2015.03.001
- Altmann, U., Zimmermann, A., Kirchmann, H. A., Kramer, D., Fembacher, A., Bruckmayer, E., Pfaffinger, I., von Heymann, F., Auch, E., Steyer, R., & Strauss, B. M. (2016). Outpatient psychotherapy reduces health-care costs: A study of 22,294 insurants over 5 years. Frontiers in Psychiatry, 7. https://doi.org/10.3389/fpsyt.2016.00098
- Bak-Klimet, A., Karatzias, T., Elliot, L., Campbell, J., Pugh, R., & Laybourn, R. (2014). Nature of child sexual abuse and psychopathology in adult survivors: Results from a clinical sample in Scotland. Journal of Psychiatric Mental Health Nursing, 21(6), 550–557. https://doi.org/10.1111/jpm.12127
- Candilis, P. J. & Pollack, M. H. (1997). The hidden costs of untreated anxiety disorders. Harvard Review of Psychiatry, 5(1), 40–42. https://doi.org/10.3109/10673229709034724
- Department of Health. (2014). Annual Report of the Chief Medical Officer 2013 Public Mental Health Priorities: Investing in the Evidence. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/413196/CMO_web_doc.pdf
- Fonagy, P., Rost, F., Carlyle, J.-A., McPherson, S., Thomas, R., Pasco Fearon, R., Goldberg, D., & Taylor, D. (2015). Pragmatic randomized controlled trial of long-term psychoanalytic psychotherapy for treatment-resistant depression: The tavistock adult depression study (TADS). World Psychiatry, 14, 312–321. https://doi.org/10.1002/wps.20267
- Gabbard, G. O. & Hornberger, J. (1997). The economic impact of psychotherapy: A review. The American Journal of Psychiatry, 154(2), 147–155. https://doi.org/10.1176/ajp.154.2.147
- Kleinstäuber, M., Witthöft, M., & Hiller, W. (2011). Efficacy of short-term psychotherapy for multiple medically unexplained physical symptoms: A meta-analysis. Clinical Psychology Review, 31(1), 146–160. https://doi.org/10.1016/j.cpr.2010.09.001
- Layard, R., Clark, D., Knapp, M., & Mayraz, G. (2007). Cost-benefit analysis of psychological therapy. National Institute Economic Review, 202(1), 90–98. https://doi.org/10.1177/0027950107086171
- Lazar, A., Sandell, R., & Grant, J. (2006). Do psychoanalytic treatments have positive effects on health and health care utilization? Further findings of the Stockholm Outcome of Psychotherapy and Psychoanalysis Project (STOPPP). Psychotherapy Research, 16(1), 51–66. https://doi.org/10.1080/10503300500268094
- Leichsenring, F. & Rabung, S. (2008). Effectiveness of long-term psychodynamic psychotherapy: A meta-analysis. JAMA, 300(13), 1551–1565. https://doi.org/10.1001/jama.300.13.1551
- Lemma, A., Target, M., & Fonagy, P. (2011). Brief dynamic interpersonal therapy: A clinician’s guide (1st ed.). Oxford University Press.
- Scottish Govenment. (2021). Scottish Budget 2021 to 2022. https://www.gov.scot/publications/scottish-budget-2021-22/
- Steinert, C., Munder, T., Rabung, S., Hoyer, J., & Leichsenring, F. (2017). Psychodynamic therapy: As efficacious as other empirically supported treatments? A meta-analysis testing equivalence of outcomes. The American Journal of Psychiatry, 174(10), 943–953. https://doi.org/10.1176/appi.ajp.2017.17010057
- Vasiliadis, H.-M., Dezetter, A., Latimer, E., Drapeau, M., & Lesage, A. (2017). Assessing the costs and benefits of insuring psychological services as part of medicare for depression in Canada. Psychiatric Services, 68(9), 899–906. https://doi.org/10.1176/appi.ps.201600395
- Yonatan Leus, R., Strauss, A. Y., & Cooper-Kazaz, R. (2020). Psychodynamic psychotherapy is associated with sustained reduction in health care utilization and cost. Clinical Psychology & Psychotherapy, 28(3), 1–14. https://doi.org/10.1002/cpp.2527