Abstract
Randomized Controlled Trials (RCTs) are currently considered ‘gold standard’ for evaluating psychosocial interventions, including psychodynamic psychotherapies (PDTs). The aim of this review is to summarize all available RCTs involving PDTs. A thorough search yielded 298 studies published between 1967 and 2022. The number of studies has increased over time with 123 (41.2%) published in the last 10 years. Most studies have been conducted in western countries, evaluating PDTs of brief duration (<40 sessions) for adults with mood (k = 67, 22.5%), psychosomatic (k = 38, 12.8%), anxiety (k = 35, 11.7%), or personality disorders (k = 29, 9.7%). The studies have utilized comparative (k = 233, 78.2%), additive (k = 33, 11.1%), parametric (k = 30, 10.1%) and dismantling designs (k = 2, 0.7%) and includes a total of 374 comparisons. Categorization of outcomes suggests that PDTs typically outperforms inactive controls, while comparisons with active treatments, inclugding Cognitive-Behavior Therapy (CBT), typically indicate no statistical difference. While the evidence-base for PDTs is growing, there are still major limitations and many research questions yet to be addressed. There is a pressing need for disseminating the existing research for PDTs to policy makers and the general public, as well as integrating findings in psychodynamic training curriculums.
Introduction
The efficacy of psychoanalysis and psychodynamic psychotherapies (PDTs)Footnote1 has been challenged and debated for more than 100 years and is still a significant concern for the future of the psychoanalytic tradition (Leuzinger-Bohleber et al., Citation2020). At the heart of the debate, critics have claimed that there exists little controlled outcome research in PDTs; alternatively, that when such research exists, it indicates that PDTs are less effective than other treatments in general and Cognitive-Behavioral Therapy (CBT) in particular (e.g., Eysenck, Citation1952; Hofmann, Citation2016; Marcus et al., Citation2014; Salkovskis & Wolpert, Citation2012; Tolin, Citation2010, Citation2014). In contrast, proponents of PDTs have argued that comparative trials and meta-analytic studies typically find that PDTs are more effective than controls and no less effective than other established treatments (e.g., Barber et al., Citation2021; Fonagy, Citation2015; Leichsenring & Klein, Citation2014; Leichsenring et al., Citation2013; Steinert et al., Citation2017).
While this debate may be regarded an expression of the current state of ‘normal science’ (Kuhn, Citation1962) within psychotherapy research, its recursions have had a major impact on the field in recent decades. The growing influence of the Evidence-Based Medicine (EBM) movement has led to an increased focus on the critical evaluation of research findings and development of clinical practice guidelines to support health-care organizations, as well as individual treatment providers, in their every-day decision-making. Although the development of such guidelines has improved medical practice and increased the use of effective and life-saving treatments in many areas (Djulbegovic & Guyatt, Citation2017), the impact of EBM in the mental health field has been intensely debated, especially when it comes to the recommendation of different psychotherapies for specific disorders (Elliott, Citation1998; Norcross et al., Citation2006; Shedler, Citation2018; Wampold & Imel, Citation2015).
In several countries, PDTs have been given low priority, or even been omitted completely, in national treatment guidelines for common mental health problems (e.g., Abbass, Tasca, et al., Citation2020; Martindale, Citation2022; Okada, Citation2022; Plakun, Citation2020). While such omissions have been challenged as being based on biased views of PDT and its research base (e.g., Abbass et al., Citation2017; Leichsenring & Rabung, Citation2011; Leichsenring et al., Citation2022, Citation2023; McPherson et al., Citation2018; Tasca et al., Citation2018), efforts to change the notion that there is a lack of evidence for PDTs have so far had limited impact, and PDTs have generally become more and more marginalized in recent years (Yakeley, Citation2020, Citation2021). This marginalization is not only a concern when it comes to the provision of PDTs in the public health sector but also affects future training opportunities and research funding. Thus, the notion that there exists little research to support PDTs may become a ‘master narrative’ that feeds a vicious circle, which over time diminishes the likelihood that such research will ever be conducted (Shedler, Citation2018).
The debate regarding the efficacy of PDTs is strongly related to the study design known as the Randomized Controlled Trial (RCT). While this design is at least as old as the critique of PDTs (Nezu & Nezu, Citation2008), it has taken center stage since the mid 1990s when it became considered the ‘gold standard’ for testing effects of psychosocial interventions and psychotherapies (Backmann, Citation2017; Boutron et al., Citation2008; Chambless & Hollon, Citation1998; Guyatt et al., Citation1995; Sackett et al., Citation1996). The logic behind the RCT is to use an experimental methodology to eliminate alternative explanations in order to establish a causal connection between the independent variable (treatment) and dependent variable (outcome). A central feature is the random assignment of participants to treatment and control groups. Random assignment (when successful) ensures that differences that exists between participants before entering the treatment phase of the study are equally distributed between the groups. Thus, any observed differences between treatment and control at termination may logically be attributed to the therapy applied.
The view that the RCT-design is the ‘gold standard’ methodology for evaluating psychotherapies has also been questioned and debated intensely (e.g., Philips, Citation2020; Philips & Falkenström, Citation2021; Seligman, Citation1995; Shedler, Citation2018; Westen et al., Citation2004). Among other issues, critics have highlighted how certain features of the design itself (such as the use of random assignment, inclusion of DSM disorder homogenous patient samples, therapies of fixed duration, treatment manuals and adherence checks, etc.) limit the external validity of RCTs since such procedures are not part of everyday clinical practice. This debate has been central in nuancing exaggerated assertions about the value of RCTs, as well as highlighting the potential and importance of other research designs (Philips, Citation2020). Still, although the RCT methodology is far from ‘perfect’, most psychotherapy researchers of today would agree that it is the strongest design for establishing a causal link between treatment and outcome (Barber & Sharpless, Citation2015; Fonagy, Citation2015; Leichsenring & Klein, Citation2014; Lilienfeld et al., Citation2018; Philips & Falkenström, Citation2021).
It is sometimes overlooked that besides testing the ‘absolute’ or ‘relative’ efficacy of a treatment by contrasting it with an inactive (e.g., waitlist) or active control condition (e.g., medication or other therapy), the RCT methodology may also be used for examining other important research questions (Nezu & Nezu, Citation2008). For example, in so-called ‘additive designs’, all patients receive the same treatment, but a randomized half of the sample also receive another intervention in addition to the first. Such studies can help bring light on questions such as if adding a particular form of psychotherapy to medication or to treatment-as-usual (TAU) may yield additional benefits. Further, in ‘parametric designs’, the same treatment is modified and contrasted on some key parameters of interest. For example, the researchers may be interested in contrasting individual vs. group format, or short-term vs. long-term treatment, possibly providing evidence for the superiority of one of the modalities of a particular treatment. Finally, in ‘dismantling designs’, the researchers deliberately take away a specific component from a treatment that is thought to be responsible for change and test that version of the treatment against a ‘full package’ version. Results from dismantling studies may be considered an important first step towards establishing evidence-based mechanisms of change (Kazdin, Citation2007).
Aims
Since the RCT methodology is considered the strongest test of treatment efficacy and is central to EBM, there is a need to examine the available research for PDTs based on such methodology. Thus, the aim of this paper is to provide a comprehensive overview of all the available RCTs involving PDTs. Importantly, the aim here is not to statistically aggregate and meta-analyze results of studies, but rather provide a descriptive, ‘birds-eye’, perspective of the current state of the field. Such an overview may help address common misconceptions regarding the alleged lack of research on PDTs, as well as correct overstated claims of the available research in certain areas. An overview of the available RCTs may also assist the research community by identifying gaps and limitations in the existing research literature, as well as point out potential areas for future studies and meta-analyses. A comprehensive overview may also be helpful for psychodynamic clinicians, supervisors and educators wanting to integrate results from controlled research in their practice and teaching.
Materials and methods
Search strategy
This review is part of the author’s ongoing project to assemble all RCTs ever conducted on PDTs (for a current update see https://www.researchgate.net/publication/317335876_Comprehensive_compilation_of_randomized_controlled_trials_RCTs_involving_psychodynamic_treatments_and_interventions). The project started in January 2014 and this review includes results of searches that were conducted until the end of December 2022.
In order to find all relevant studies, an additive search strategy has been used. The author started with extracting references to RCTs included in (or excluded from) meta-analyses of PDTs published before 2014. The original studies of these meta-analyses were then read and checked for references to additional studies. Since January 2014, the author has conducted recurrent manual searches in major data bases (e.g., PubMed, PsycINFO and Cochrane Library) using a combination of search terms such as ‘psychodynamic’, ‘psychoanalytic’, ‘randomized’ and ‘trial’ to find additional and newly published studies. Further, newly published studies and meta-analyses have been read and checked for references to previously undetected studies. Finally, leading researchers within the PDT research community has been probed repeatedly for knowledge of any less well-known or unpublished studies.
Inclusion and exclusion criteria
All studies that used a randomized design and involved at least one intervention described as being based on psychodynamic theory and treatment principles have been included. Thus, the studied treatment may be some form of Short-Term Psychodynamic Psychotherapy (STPP), Long-Term Psychodynamic Psychotherapy (LTPP), psychoanalysis or other form of PDT and be delivered in individual, group or other format (e.g., couples therapy). Studies of eclectic or integrative treatments with a major psychodynamic component, such as for example Brief Eclectic Psychotherapy (BEP; Gersons & Schnyder, Citation2013) and Emotional Awareness and Expression Therapy (EAET; Lumley & Schubiner, Citation2019), have also been included. However, studies of established treatments that overlap with PDTs to some extent but are typically not considered psychodynamic, such as Interpersonal Therapy (IPT; Markowitz et al., Citation1998), Eye Moment and Desensitization Reprocessing (EMDR; Shapiro & Laliotis, Citation2011), Schema-Focused Therapy (SFT; Arntz & Van Genderen, Citation2021), Compassion-Focused Therapy (CTF; Gilbert, Citation2014) or Cognitive-Analytic Therapy (CAT; Ryle & Kerr, Citation2020) have been excluded. No restrictions in terms of the targeted patient population or condition treated has been used.
Coding
All collected studies were retrieved, read in full text and coded by the author. For studies published in a language other than English (i.e., German, k = 1; Italian, k = 1; Spanish, k = 1; Russian, k = 1; Farsi, k = 13), only the English abstract was used. For the purpose of this review, information in the following domains was extracted and coded:
Study characteristics
Besides the year of publication and country of origin, the main design of each study was coded. The code ‘Comparative’ was used when PDT was tested against either an inactive control group (such as no treatment, waitlist, etc., see below for details on coding of comparison groups) and/or an active treatment comparison (e.g., medication or CBT). ‘Additive’ was used for studies in which PDT was used as an add-on to treatment-as-usual (TAU) or medication, or if medication was added to PDT and tested against PDT alone. ‘Parametric’ was used for studies that compared two (or more) PDTs with contextual factors manipulated, such as for example treatment format (e.g., individual vs. group), length (e.g., LTPP vs. STPP), or mode (e.g., expressive vs. supportive). Studies that tested a full-package PDT versus PDT without a particular component (e.g., transference work) were coded as ‘Dismantling’. If elements from several designs were present in the same study (e.g., contrasting two variations of PDT in a parametric design, but also including a waitlist), the study was coded in accordance with the main research question stated by the authors.
Sample characteristics
The total number of participants included for randomization was extracted as well as the mean age and percentage of female participants when available. The targeted age group of the study was also coded ‘Children’ (<12 years), ‘Adolescents’ (12–18 years), ‘Adults’ (18–64 years), ‘Older adults’ (>65 years) or ‘Mixed age groups’ when participants could belong to several categories. The primary targeted condition was coded in eight diagnostic categories, i.e., ‘Mood disorders’, ‘Anxiety disorders’, ‘Personality disorders’, ‘Psychosomatic disorders’, ‘Eating disorders’, ‘Substance abuse disorders’, ‘Trauma/stress related disorders’ and ‘Psychotic disorders’, based on the definition used in each study. When studies included participants with different primary diagnoses, the category ‘Mixed diagnoses’ was used. For studies that did not target a particular diagnosis, the category ‘Other defined problem’ was used. Studies were also coded if they reported using some version of DSM or ICD diagnostics as inclusion criteria for their sample.
Treatment characteristics
Based on the available information in each study, treatment format was coded ‘individual’, ‘Group’, ‘Parent-infant’ or ‘Couple’. When the treatment intervention included several formats (e.g., individual and group therapy), the code ‘Multi-modal’ was used.
Treatment type was coded ‘STPP’ when 1) the treatment was less than 40 sessions, 2) the study authors used terms such as ‘short-term’, ‘brief’, ‘time-limited’ or ‘focal’ to describe the treatment, and/or 3) there was a clear reference to well-known STPP literature. The code ‘LTPP’ was used for treatments that were not described as STPP (according to the above criteria) and involved more than 40 sessions. Treatments were coded ‘Psychoanalysis’ when authors used that term and the treatment involved 3–5 sessions a week with a couch setting. The code ‘Internet-based self-help’ was used for guided self-help programs based on PDT theory delivered via the Internet. Treatments were coded ‘Integrative’ when authors described them as involving techniques derived from several theoretical orientations besides PDT. When a treatment could not be categorized in any of these categories, they were coded as ‘Other’. This category included, for example, multi-modal day clinic treatments, music- or movement-oriented treatments, psychoeducational programs for parents, work counseling, etc., that were described as being based psychodynamic theory and treatment principles.
Treatment setting was coded ‘Outpatient’ or ‘Inpatient/day care’ and treatment length was coded for the planned number of sessions of the intervention (e.g., <12, 12–40, or >40 sessions) in each study. Further, treatments were also coded for manual use: ‘Clear reference’ was used when there was a reference to a specific book on psychodynamic technique or a specific manual, ‘Unclear reference’ when there were references to several books or manuals and ‘No manual’ when there was either no information or clear information that no particular manual was used.
Comparisons
In comparative designs, the control conditions were coded ‘No treatment’, ‘Waitlist’, ‘Medical placebo’ or ‘TAU’ (e.g., treatment or care as usual) based on the study descriptions. Comparison conditions that included some active elements (e.g., psychoeducation, brief relaxation training, non-specific support, etc.) but were of shorter duration and with limited therapist contact compared to the treatment tested were coded as ‘Limited treatment’ controls. ‘Medication’ was used when the comparison condition involved medication that followed some protocol or regime. Comparative psychotherapies that were described as based on cognitive therapy, behavior therapy or a combination of cognitive and behavior components were all coded as ‘CBT’, while active treatments based on other theoretical foundations (e.g., systemic and humanistic) were coded as ‘Other psychotherapies’. Comparisons that involved manualized supportive therapy of approximately equal duration as the main treatment tested were coded ‘Supportive Therapy’.
Studies with additive designs were coded so that the additive element compared to the group without the additive element (e.g., add PDT to TAU, add PDT to medication or add medication to PDT). Comparison groups in parametric designs were coded according to which parameter was tested (e.g., individual vs. group, outpatient vs. inpatient, etc.), while dismantling studies were coded based on the particular element dismantled (e.g., transference work vs. no transference work).
Main outcome
In order to provide a descriptive overview of results of PDTs in comparison to different control conditions, studies were also coded for their main outcome on the primary outcome measure of each study. If the study authors did not specify a particular measure as primary, a measure targeting the primary sample diagnostic (e.g., BDI for depression, LSWQ for social phobia, etc.) was selected by the author of this review. Results for comparisons with controls or alternative treatments were then coded ‘Favoring PDT’, ‘No statistical difference’ or ‘Favoring comparison’ based on the result of the statistical test used in each study. Only results directly at termination of treatments was coded. Same procedure was used for additive, parametric and dismantling designs. Thus, no effect sizes were calculated or synthesized for this review since the aim was to provide an overall view of the literature rather than meta-analysis.
Results
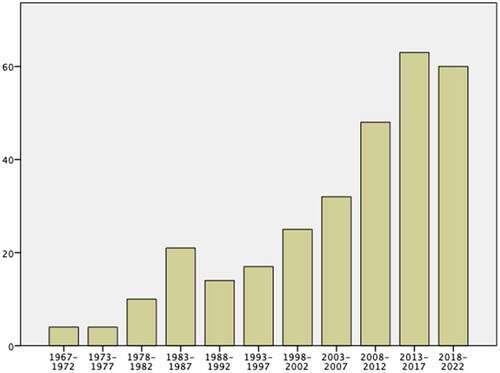
A total of 298 independent studies were identified through the searches. The studies were published between 1967 and 2022 and there was evidence of an increase in publications over time (see ), with just over 40% of the studies (k = 123, 41.2%) published in the last decade.
The overall characteristics of the included studies are displayed in . Most studies were conducted in Europe (k = 166, 55.7%), followed by North America (k = 77, 25.8%) and Asia (k = 43, 14.4%). Only seven studies (2.3%) were conducted in South America, and no study of PDT has yet been conducted on the African continent. In terms of specific countries, most studies have been conducted in USA (k = 59, 19.8), followed by UK (k = 42, 14.1%) and Germany (k = 34, 11.4%). Of the total 298 studies, 233 (78.2%) used a comparative design, 33 (11.1%) an additive design and 30 (10.1%) a parametric design. Only two studies (0.7%) utilized a dismantling design.
Table 1. Study characteristics (k = 298).
Sample and treatment characteristics are summarized in . Across all 298 studies, the average sample size was 91.4 (SD = 83.6, range 8–570). The distribution was positively skewed with most studies (k = 206, 69.1%) having less than 100 participants. Median sample size was 68.5. In terms of gender distribution, the average study had 66.6% female participants and 47 studies (15.8%) had female participants only. The mean age of participants across all samples was 34.1 (SD = 12.3) years, and a clear majority of studies have targeted adults (k = 252, 84.6%).
Table 2. Sample characteristics (k = 298).
In terms of diagnostic categories, the most studied area is mood disorders (k = 67, 22.5%), followed by psychosomatic conditions (k = 38, 12.8%), anxiety disorders (k = 35, 11.7%), and personality disorders (k = 29, 12.8%). A fairly large number of studies (k = 56, 18.8%) were categorized as focusing on ‘other defined problem’, which included samples with psychological and interpersonal issues such as aggression, self-harm, alexithymia, fear of intimacy, couple distress, etc., without patients necessarily fullfilling criteria for any specific psychiatric diagnosis. Of the studies that focused on a specific diagnostic sample, 184 (76.0%) reported using some version of DSM or ICD criteria for inclusion.
summarizes treatment characteristics. Because some studies tested several variations of PDT, the total number of studied PDT interventions was k = 314. Most commonly, treatment was delivered in individual format (k = 227, 72.2%), followed by group (k = 50, 15.9%) and multi-modal format (k = 26, 6.9%). There currently exist nine studies of parent-infant PDTs (2.4%), but only two studies of PDTs for couples (0.1%). In terms of treatment type, most studies tested some form of STPP (k = 229, 70.0%), followed by LTPP (k = 40, 12.6%) and integrative treatments (k = 14, 4.5%). There are currently nine RCTs (2.8%) of Internet-based self-help programs based on PDT principles, but only two studies of psychoanalysis proper (<0.1%). The treatments were typically delivered in an outpatient setting (k = 294, 93.6%) and involved 12–40 sessions (k = 198, 63.1%). About two-thirds of studies (k = 196, 62.4%) reference a specific manual or book describing the treatment used.
Table 3. Treatment characteristics (k = 314).
Comparison conditions and categorization of the main outcomes are displayed in . The 298 studies involved a total of 374 comparisons across the different study designs. In comparative designs, the most common control condition was waitlist (k = 47), followed by TAU (k = 46), and limited treatment (k = 37). Only two studies have tested a PDT against a medical placebo. The most common active treatment comparator is CBT (k = 86), followed by other psychotherapy (k = 30). In terms of the categorizations of main outcomes in comparative designs, most studies suggest PDTs outperform no treatment (k = 20, 90.1%), waitlist (k = 39, 83.0%), TAU (k = 36, 78.3%), and limited treatment controls (k = 21, 56.8%). Studies comparing PDTs with CBT typically find no statistically significant differences (k = 59, 69.6%), but about one-fourth of comparisons suggest possible advantage for CBT at post treatment (k = 21, 24.4%). The most common result when PDTs are compared with medication (k = 9, 75.0%), other psychotherapies (k = 21, 70.0%) and manualized supportive therapy (k = 7, 58.3%) is also that of no statistical difference.
Table 4. Comparison conditions (total k = 374) and categorization of main outcome.
In additive designs, 23 comparisons were between adding PDT to TAU and TAU alone, 11 between adding PDT to medication and medication alone, and six involved adding medication to PDT and testing against PDT alone. Categorizations of the results suggest that adding PDT to TAU (k = 15, 65.2%) or medication (k = 8, 72.7%) may be associated with additional benefits, while the most common result of adding medication to PDT was no significant difference compared to PDT alone (k = 5, 83.3%).
The most common comparisons in parametric designs involved comparing expressive and supportive modes of PDT (k = 12), LTPP vs STPP (k = 6) and comparing PDT in individual format vs group format (k = 5). Categorizations of outcomes suggest expressive modes of PDT may be favorable over supportive (k = 8, 66.6%). Half of the available comparisons suggest that LTPP may outperform STPP (k = 3, 50%), while most comparisons suggest no significant differences between PDTs in individual and group format (k = 4, 80%). Studies comparing PDTs with manual vs. PDT without manual suggest no significant differences in outcome (k = 3, 100%). Only two studies utilized a dismantling design and both involved comparing PDT, which included transference work with PDT that did not focus on the transference relationship. No significant difference was found at post treatment in either of the studies.
Discussion
The aim of this review was to provide a comprehensive, descriptive overview of all existing randomized controlled trials of PDTs. Through an extensive search, almost 300 studies were identified. The publications span over 55 years and there was evidence of an increase over time. Interestingly, this contrasts with a recent study by Rief et al. (Citation2022) who report that the number of psychodynamic RCTs has decreased since 2010. The authors of that review found 53 published studies between 2010 and 2019, while 117 studies from the same period were included here, i.e., more than twice as many. It is possible that this discrepancy is a consequence of differences in search strategies and inclusion criteria, which highlights the importance of conducting broad literature searches in order to avoid incorrect conclusions.
This review found that about 40% of the controlled outcome research in PDTs has been published in the last decade. Given the typically slow process of research dissemination, this suggests a fair number of studies on PDTs are likely not very well known in the community. Further, much of this research has not yet been included in meta-analyses or integrated in guideline recommendations. Thus, the psychodynamic community needs to continue to be attentive to future developments in the field and actively work towards a fair representation of the evidence-base for PDTs for policy makers, as well as the general public.
Clearly, with almost 300 published RCTs, the notion that ‘there is no controlled outcome research on PDTs’ is not valid. Still, compared to other active treatments in the mental health field (such as, for example, anti-depressive medication or CBT), the database is still quite small, and the results of this review point to several areas where there are important gaps and limitations to be addressed in future studies.
For example, the existing evidence-base is skewed towards adult patient populations, and there are relatively few studies of children and adolescents. While this in part may reflect general problems with funding and ethical complications when conducting research with underaged participants, the field of psychodynamic child and adolescent psychotherapy has also been slow in adopting to the demands of modern outcome research (Midgley et al., Citation2021). Thus, despite a rich theoretical and clinical tradition, there is a strong need for further evaluations of PDTs targeting children and adolescents. Also, older adults (e.g., >65 years) appears to be an understudied population considering PDTs may be particularly well-suited for this age group based on both theoretical and clinical notions (Choudhury et al., Citation2020).
In terms of diagnostic categories, most studies have targeted mood disorders (i.e., depression). Since bona-fide psychotherapies tend to have similar effects for mild-to-moderate depression (Cuijpers, Citation2017), researchers may consider focusing on more challenging patient presentations (e.g., chronic, treatment resistant or recurrent depression), as well as contrasting different modes, intensities or treatment lengths to see what may augment effects for this population, in future studies of PDTs for mood disorders. Also, to the author’s knowledge, no study has yet evaluated PDT for bipolar disorder or tested PDT as a relapse prevention intervention in depression.
Perhaps somewhat surprisingly, the second largest diagnostic category targeted was psychosomatic conditions with 38 identified studies. While this area is complex and researchers are still in search of consensus regarding diagnostic classifications, meta-analytic findings suggest PDTs are effective for many patients with functional somatic symptoms (Abbass, Town, et al., Citation2020). Still, there is a need for larger, high-quality studies, as well as studies that examine treatment mechanisms in more detail. There has also been an increased interest in PDTs for anxiety disorders in recent years, and encouragingly this review found 35 studies in this area. Still, while the evidence-base is growing, there are few studies for certain anxiety diagnoses such as OCD or PTSD (Barber et al., Citation2021). Similarly, the evidence-base for PDTs in personality disorders is promising but currently limited to cluster C and borderline (Keefe et al., Citation2019). In other important areas, such as eating disorders, substance abuse disorders and psychotic disorders, controlled studies of PDTs are still quite scarce. At this point, these areas may benefit from systematic reviews of the clinical and research literature (including results of non-RCTs and process research) in order to provide theoretical and empirical ground work for the future development and testing of PDTs.
When it comes to treatment characteristics, it is important to acknowledge that the majority of studies evaluate short-term versions of PDT (i.e., STPPs), while the evidence-base for LTPP is more limited and psychoanalysis proper has rarely been subjected to controlled outcome research at all. This probably reflects a number of practical and ethical issues associated with testing longer therapies in RCT designs (e.g., Seligman, Citation1995). It is also true that even though many patients with personality disorders or other complex psychiatric conditions likely need longer treatments, controlled studies of long-term therapies (including long-term CBT) are scarce in general (Leichsenring et al., Citation2013). The categorization of results from parametric designs in suggests that when LTPP and STPP have been compared directly, half of the studies find LTPP superior. Thus, LTPP may be preferable in some patient populations, and there is a need to continue to identify factors that predict poorer outcome in short-term treatments and evaluate LTPP as a possible alternative. Since RCTs are very expensive and complicated to conduct (although evidently not impossible) for longer treatments, panel data/cohort designs with repeated measurements may be a more pragmatic alternative to consider (Philips & Falkenström, Citation2021).
One area that has gained a lot of research attention in the last decade is that of therapist-guided self-help interventions delivered through the Internet (Andersson et al., Citation2019). While there are now hundreds of trials of Internet-based Cognitive-Behavior Therapy (ICBT), research on Internet-based Psychodynamic Therapy (IPDT) has also gained some momentum (nine studies were included here) and the results appear quite promising (Lindegaard et al., Citation2020). This type of intervention may challenge the psychodynamic community since the here-and-now therapeutic relationship may seem less important in such treatments. However, newly conducted qualitative research (e.g., Lindqvist et al., Citation2022; Mortimer et al., Citation2022) indicates that patients value the therapeutic relationship highly in IPDT and clinical experience suggests psychodynamic treatment principles and interventions may be both useful and important in this context (Maroti et al., Citation2023). IPDTs should be evaluated further, and one prospect would be to compare IPDT with face-to-face PDT in order to examine possible differences in efficacy, as well as examine the impact of different treatment processes in each format.
The aim of this review was to provide a descriptive overview rather than to aggregate and meta-analyze effect sizes from primary studies. Thus, the categorization of outcomes in should be interpreted with caution. In particular, studies finding ‘no significant difference’ between PDT and comparators may simply reflect lack of statistical power in some of the individual studies. Still, the simple categorization of outcomes was included in this review in order to consider some tentative implications.
Overall, the categorizations are in line with a number of systematic reviews and meta-analyses finding that PDTs outperform inactive controls and generally show small or no differences with other active treatments (e.g., Abbass, Tasca, et al., Citation2020; Barber et al., Citation2021; Leichsenring & Klein, Citation2014; Steinert et al., Citation2017). Still, it should be recognized that PDTs do not invariably outperform inactive comparison conditions, not even no treatment or waitlist controls. Further, only two studies have compared PDT with a medical placebo and show conflicting results. While some ‘false negatives’ are to be expected simply due to chance, studies with unexpected results should be examined closely in order to identify factors in treatment delivery and/or study context that may help explain the lack of effects.
This review found 86 direct comparisons between some form of PDT and some form of CBT and the typical finding was that of no statistical difference. Still, given the recurrent debate concerning PDTs relative efficacy to CBT, the fact that about a quarter of the comparisons indicated advantage for CBT warrant some further elaboration. First, this finding may help explain conflicting results of meta-analyses if authors selectively examine only a portion of the available research (Wampold et al., Citation2017). Further, among the studies that show advantage for CBT, some may be considered controversial and have been criticized for misrepresenting PDTs (e.g., Leichsenring & Leibing, Citation2007; Shedler, Citation2018; Wittmann et al., Citation2011; Yeomans, Citation2007). It should also be kept in mind that results were only coded at termination for this review, and several studies suggest that significant advantage for CBT at termination may disappear at follow-up (e.g., Leichsenring et al., Citation2014; Svensson et al., Citation2020).
Still, these caveats aside, there are also well-executed trials that point to possible advantages for CBT. Rather than ignoring, discarding or ‘forgetting’ such results, the psychodynamic community should study and learn from the studies since they may inform future development of PDTs. For example, consider PDT for bulimia for which Poulsen et al. (Citation2013) found a clear advantage of CBT compared to a long-term psychoanalytic therapy (42% remission rate compared to 15%). However, in another study, Stefini et al. (Citation2017) found no significant differences in remission rates for CBT and PDT for bulimia (33% vs. 31%, respectively). In the second study, an STPP manual that specifically targeted bulimia was used, while to the first study tested, a more ‘generic’ LTPP approach. Thus, in terms of treating patients with specific disorders, PDTs may be enhanced by developing approaches that target specific symptoms or problem areas (e.g., Busch, Citation2021). Such results may be very informative for clinical practice and should be discussed and integrated in psychodynamic trainings.
Results from parametric and dismantling studies may also be informative for clinical practice since they help clarify under what conditions PDTs are effective and evaluate important treatment components. Still, there are few such studies of PDTs, and while there is some indication that expressive modes of PDTs may outperform more supportive modes, results are mostly inconclusive. This points to the need of further high-quality studies that evaluate theoretically derived mechanisms of change in PDTs. However, using parametric or dismantling RCT designs may not be the most fruitful way forward since such studies do not provide direct support for a mediator or mechanism (Kazdin, Citation2007). What is needed is larger RCTs in specific areas that include repeated measurements of both outcome and well-defined process variables enabling the use of state-of-the-art statistical methods in order to illuminate the complex interactions leading to outcome (Philips & Falkenström, Citation2021; Zilcha-Mano, Citation2019).
Turning to some implications for training, the present-day evidence-base for PDTs should be actively taught and integrated in psychodynamic training programs (Aafjes van Doorn & Prout, Citation2022; Busch et al., Citation2009; Pretsky, Citation2020). In addition to skills in critical evaluation of studies, future psychodynamic practitioners should have sound knowledge of this body of research, including its current limitations. Further, specific STPP and LTPP models that have been subjected to controlled research, such as for example Supportive-Expressive Therapy (SET; Luborsky, Citation1984), Intensive Short-Term Dynamic Psychotherapy (ISTDP; Abbass, Citation2015), Panic-Focused Psychodynamic Psychotherapy (PFPP; Milrod et al., Citation1997); Dynamic-Interpersonal Therapy (DIT; Lemma et al., Citation2011), Transference-Focused Psychotherapy (TFP; Clarkin & Kernberg, Citation2015) and Mentalization-Based Treatment (MBT; Bateman & Fonagy, Citation2006), should be introduced and integrated with teaching in general psychodynamic concepts and treatment principles. This puts pressure on psychodynamic teachers and supervisors who, in addition to having deep knowledge in the rich theoretical and clinical literature, needs to keep updated with the growing body of research in PDTs; still, if the aim of the community is to truly become ‘evidence-based’, this is the way forward.
Limitations
There are several limitations with this overview that should be kept in mind. First, although a very thorough search strategy was used, there may still exist undetected studies. In particular, there may be trials published in other languages than English as well as unpublished studies not included here. Second, all coding was done by the author alone which increases the risk of bias and error. Some studies were difficult to code due to limited data in the original article, and it is possible that a group of coders would have reached other categorizations in some cases; however, it seems unlikely that the overall picture of this overview would change. Future meta-analyses focusing on more specific research questions should use multiple coders to assess inclusion and exclusion criteria as well as the extraction of data from primary studies.
Also, the quality of the studies was not assessed. In a previous review, Thoma et al. (Citation2012) found that RCTs of PDTs had similar average quality compared to RCTs of CBT for depression. Their review included 94 RCTs of PDTs published up till 2010, and the authors found a significant increase in study quality over time; however, it is not clear if this increase has continued beyond 2010. Likewise, the authors’ allegiance was not coded for this review. Allegiance has been found to have a robust moderate association with study outcome (Munder et al., Citation2013) and considering the demands of conducting RCTs, it is likely that most studies testing PDTs have been done by researches with allegiance to that type of treatment. Thus, future meta-analyses focusing on outcomes for PDTs in particular areas should assess and consider both study quality and author allegiance as co-variates in analyses.
Lastly, as already mentioned above, the aim of this review was descriptive, and I did not calculate study effect sizes or conduct formal meta-analyses. Thus, the categorizations of outcomes should be interpreted cautiously and only be viewed as general indicators. Future meta-analyses should examine outcomes in more detail and also extract data for several measures and assessment points in order to evaluate the effects of PDTs in specific areas.
Conclusion
PDTs have been around for more than 100 years and are still widely practiced around the world. This review suggests that there is a growing body of controlled outcome research in PDTs that generally indicate that these are effective treatments. However, there are still significant limitations and areas that need to be investigated further. Thus, the debate over the efficacy of PDTs is not likely to settle any time soon, and there is a risk of further marginalization of PDTs unless the evidence-base continues to be expanded and disseminated to policy makers and the general public. There is also a need to assimilate research findings in psychodynamic training, clinical practice and academic settings in order to continue to develop and evaluate PDTs for the future.
Acknowledgments
I would like to thank all colleagues in the psychodynamic research community who have helped me identify studies and manage my list of psychodynamic RCTs. Particular thanks to professors Allan Abbass, Falk Leichsenring, Marc Diener, Christian Roesler and Jaques Barber. I would also like to thank professors Andrzej Werbart and Rolf Sandell for persistent encouragement and inspiration to engage in the field of psychodynamic research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Notes
1. The term ‘psychodynamic psychotherapies’ (PDTs) will be used in this article to describe all psychological interventions based on principles derived from the broad psychoanalytic tradition. More specific terms, such as Long-Term Psychodynamic psychotherapy (LTPP), Short-Term Psychodynamic Psychotherapy (STPP) and psychoanalysis, will be used when discussing specific treatment formats and models.
References
- Aafjes van Doorn, K. & Prout, T. A. (2022). Changing attitudes toward evidence-based psychodynamic psychotherapy. Psychoanalytic Psychology, 39(3), 217–225. https://doi.org/10.1037/pap0000397
- Abbass, A. (2015). Reaching through resistance: Advanced psychotherapy techniques. Seven Leaves Press.
- Abbass, A., Luyten, P., Leichsenring, F., & Steinart, C. (2017). Bias toward psychodynamic therapy: Framing the problem and working toward a solution. Journal of Psychiatric Practice, 23(5), 361–365. https://doi.org/10.1097/PRA.0000000000000256
- Abbass, A., Tasca, G. A., Vasiliadis, H. M., Spagnolo, J., Kealy, D., Hewitt, P. L., Hébert, C., Drapeau, M., & Doidge, N. (2020). Psychodynamic therapy in Canada in the era of evidence-based practice. Psychoanalytic Psychotherapy, 34(2), 78–99. https://doi.org/10.1080/02668734.2020.1803390
- Abbass, A., Town, J., Holmes, H., Luyten, P., Cooper, A., Russell, L., Kisley, S., & Kisley, S. (2020). Short-term psychodynamic psychotherapy for functional somatic disorders: A meta-analysis of randomized controlled trials. Psychotherapy and Psychosomatics, 1–8. https://doi.org/10.1159/000507738
- Andersson, G., Titov, N., Dear, B. F., Rozental, A., & Carlbring, P. (2019). Internet‐delivered psychological treatments: From innovation to implementation. World Psychiatry, 18(1), 20–28. https://doi.org/10.1002/wps.20610
- Arntz, A. & Van Genderen, H. (2021). Schema therapy for borderline personality disorder (2nd ed.). Wiley Blackwell.
- Backmann, M. (2017). What’s in a gold standard? In defence of randomised controlled trials. Medicine, Health Care, and Philosophy, 20(4), 513–523. https://doi.org/10.1007/s11019-017-9773-2
- Barber, J. P., Muran, C., McCarthy, K. S., Keefe, J. R., & Zilcha-Mano, S. (2021). Research on dynamic psychotherapies. In M. Barkham, W. Lutz, & L. G. Castonguay (Eds.), Bergin and Garfield’s handbook of psychotherapy and behavior change (6th ed., pp. 387–419). Wiley.
- Barber, J. P. & Sharpless, B. A. (2015). On the future of psychodynamic therapy research. Psychotherapy Research, 37–41. https://doi.org/10.1080/10503307.2014.996624
- Bateman, A. & Fonagy, P. (2006). Mentalization-based treatment for borderline personality disorder: A practical guide. Oxford University Press.
- Boutron, I., Moher, D., Altman, D. G., Schulz, K. F., & Ravaud, P. (2008). Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: Explanation and elaboration. Annals of Internal Medicine, 148(4), 295. https://doi.org/10.7326/0003-4819-148-4-200802190-00008
- Busch, F. N. (2021). Problem-Focused psychodynamic psychotherapies. Psychiatric Services, 72(12), 1461–1463. https://doi.org/10.1176/appi.ps.202000887
- Busch, F. N., Milrod, B. L., & Sandberg, L. S. (2009). A study demonstrating efficacy of a psychoanalytic psychotherapy for panic disorder: Implications for psychoanalytic research, theory, and practice. Journal of the American Psychoanalytic Association, 57(1), 131–148. https://doi.org/10.1177/0003065108329677
- Chambless, D. L. & Hollon, S. D. (1998). Defining empirically supported therapies. Journal of Consulting and Clinical Psychology, 66(1), 7–18. https://doi.org/10.1037/0022-006X.66.1.7
- Choudhury, T. K., John, K. C., Garrett, R. K., & Stagner, B. H. (2020). Considering psychodynamic therapy for older adults. Psychodynamic Psychiatry, 48(2), 152–162. https://doi.org/10.1521/PDPS.2020.48.2.152
- Clarkin, J. F. & Kernberg, O. F. (2015). Transference-focused psychotherapy for borderline personality disorder: A clinical guide. American Psychiatric Publication.
- Cuijpers, P. (2017). Four decades of outcome research on psychotherapies for adult depression: An overview of a series of meta-analyses. Canadian Psychology/Psychologie Canadienne, 58(1), 7–19. https://doi.org/10.1037/cap0000096
- Djulbegovic, B. & Guyatt, G. H. (2017). Progress in evidence-based medicine: A quarter century on. The Lancet, 390(10092), 415–423. https://doi.org/10.1016/S0140-6736(16)31592-6
- Elliott, R. (1998). Editor’s introduction: A guide to the empirically supported treatments controversy. Psychotherapy Research, 8(2), 115–170. https://doi.org/10.1093/ptr/8.2.115
- Eysenck, H. J. (1952). The effects of psychotherapy: An evaluation. Journal of Consulting Psychology, 16, 319–324. https://doi.org/10.1037/h0063633
- Fonagy, P. (2015). The effectiveness of psychodynamic psychotherapies: An update. World Psychiatry, 14(2), 137–150. https://doi.org/10.1002/wps.20235
- Gersons, B. P. R. & Schnyder, U. (2013). Learning from traumatic experiences with brief eclectic psychotherapy for PTSD. European Journal of Psychotraumatology, 4(1), 1–6. https://doi.org/10.3402/ejpt.v4i0.21369
- Gilbert, P. (2014). The origins and nature of compassion focused therapy. British Journal of Clinical Psychology, 53(1), 6–41. https://doi.org/10.1111/bjc.12043
- Guyatt, G. H., Sackett, D. L., Sinclair, J. C., Hayward, R., Cook, D. J., & Cook, R. J. (1995). Users’ guides to the medical literature: IX. A method for grading health care recommendations. JAMA, 274(22), 1800–1804. https://doi.org/10.1001/jama.274.22.1800
- Hofmann, S. G. (2016). Psychodynamic therapy: A poorly defined concept with questionable evidence. Evidence-Based Mental Health, 19(2), 63–63. https://doi.org/10.1136/eb-2015-102211
- Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3(1), 1–27. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432
- Keefe, J. R., McMain, S. F., McCarthy, K. S., Zilcha-Mano, S., Dinger, U., Sahin, Z., Graham, K., & Barber, J. P. (2019). A meta-analysis of psychodynamic treatments for borderline and cluster C personality disorders. Personality Disorders: Theory, Research, and Treatment, 11(3), 157–169. https://doi.org/10.1037/per0000382
- Kuhn, T. (1962). The structure of the scientific revolution. Chicago University Press.
- Leichsenring, F., Abbass, A., Luyten, P., Hilsenroth, M., & Rabung, S. (2013). The emerging evidence for long-term psychodynamic therapy. Psychodynamic Psychiatry, 41(3), 361–384. https://doi.org/10.1521/pdps.2013.41.3.361
- Leichsenring, F. & Klein, S. (2014). Evidence for psychodynamic psychotherapy in specific mental disorders: A systematic review. Psychoanalytic Psychotherapy, 28(1), 4–32. https://doi.org/10.1080/02668734.2013.865428
- Leichsenring, F. & Leibing, E. (2007). Cognitive-behavioural therapy for avoidant personality disorder. British Journal of Psychiatry, 190(1), 80–80. https://doi.org/10.1192/bjp.190.1.80
- Leichsenring, F., Luyten, P., Abbass, A., & Steinert, C. (2022). In reply: Psychodynamic therapy of depression. Australian & New Zealand Journal of Psychiatry, 56(9), 1202–1204. https://doi.org/10.1177/00048674221108637
- Leichsenring, F. & Rabung, S. (2011). Double standards in psychotherapy research. Psychotherapy and Psychosomatics, 80(1), 48–51. https://doi.org/10.1159/000315365
- Leichsenring, F., Salzer, S., Beutel, M. E., Herpertz, S., Hiller, W., Hoyer, J., Leibing, E., & Leibing, E. (2014). Long-term outcome of psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder. The American Journal of Psychiatry, 171(10), 1074–1082. https://doi.org/10.1176/appi.ajp.2014.13111514
- Leichsenring, F., Steinert, C., Rost, F., Abbass, A., Heim, N., & Ioannidis, J. P. A. (2023). A critical assessment of NICE guidelines for treatment of depression. World Psychiatry, 22(1), 43–45. https://doi.org/10.1002/wps.21039
- Lemma, A., Target, M., & Fonagy, P. (2011). Brief dynamic interpersonal therapy: A clinician’s guide. Oxford University Press.
- Leuzinger-Bohleber, M., Solms, M., & Arnold, S. E. (Eds.). (2020). Outcome research and the future of psychoanalysis: Clinicians and researchers in dialogue (1st ed.). Routledge. https://doi.org/10.4324/9780429281112x
- Lilienfeld, S. O., McKay, D., & Hollon, S. D. (2018). Why randomised controlled trials of psychological treatments are still essential. The Lancet Psychiatry, 5, 536–538. https://doi.org/10.1016/S2215-0366(18)30-045-2
- Lindegaard, T., Berg, M., & Andersson, G. (2020). Efficacy of internet delivered psychodynamic psychotherapy: Systematic review and meta-analysis. Psychodynamic Psychiatry, 48(4), 437–454. https://doi.org/10.1521/pdps.2020.48.4.437
- Lindqvist, K., Mechler, J., Midgley, N., Carlbring, P., Carstorp, K., Neikter, H. K., Strid, F., Von Below, C., & Philips, B. (2022). “I didn’t have to look her in the eyes”—Participants’ experiences of the therapeutic relationship in internet-based psychodynamic therapy for adolescent depression. Psychotherapy Research. Advance online publication. https://doi.org/10.1080/10503307.2022.2150583
- Luborsky, L. (1984). A manual for supportive-expressive dynamic psychotherapy. Basic Books.
- Lumley, M. A. & Schubiner, H. (2019). Emotional awareness and expression therapy for chronic pain: Rationale, principles and techniques, evidence, and critical review. Current Rheumatology Reports, 21(7), 30. https://doi.org/10.1007/s11926-019-0829-6
- Marcus, D. K., O’Connell, D., Norris, A. L., & Sawaqdeh, A. (2014). Is the dodo bird endangered in the 21st century? A meta-analysis of treatment comparison studies. Clinical Psychology Review, 34(7), 519–530. https://doi.org/10.1016/j.cpr.2014.08.001
- Markowitz, J., Svartberg, M., & Swartz, H. (1998). Is IPT time-limited psychodynamic psychotherapy? The Journal of Psychotherapy Practice and Research, 7(3), 185. Retrieved from http://ukpmc.ac.uk/abstract/MED/9631340
- Maroti, D., Hallberg, H., Lindqvist, K., & Mechler, J. (2023). Using psychodynamic principles in guided internet-delivered therapy (IPDT). Psychoanalytic Psychotherapy, 37(1), 63–83. https://doi.org/10.1080/02668734.2022.2124441
- Martindale, B. (2022). Changes in psychoanalytic therapy in Europe over three decades. Then and now. Psychoanalytic Psychotherapy, 36(4), 383–436. https://doi.org/10.1080/02668734.2022.2124534
- McPherson, S., Rost, F., Town, J., & Abbass, A. (2018). Epistemological flaws in NICE review methodology and its impact on recommendations for psychodynamic psychotherapies for complex and persistent depression. Psychoanalytic Psychotherapy, 32(2), 102–121. https://doi.org/10.1080/02668734.2018.1458331
- Midgley, N., Mortimer, R., Cirasola, A., Batra, P., & Kennedy, E. (2021). The evidence-base for psychodynamic psychotherapy with children and adolescents: A narrative synthesis. Frontiers in Psychology, 12(April). https://doi.org/10.3389/fpsyg.2021.662671
- Milrod, B., Busch, F., Cooper, A., & Shapiro, T. (1997). Manual of panic-focused psychodynamic psychotherapy. American Psychiatric Publishing.
- Mortimer, R., Somerville, M., Mechler, J., Lindqvist, K., Leibovich, L., Guerrero-Tates, B., Edbrooke-Childs, J., Martin, P., & Midgley, N. (2022). Connecting over the internet: Establishing the therapeutic alliance in an internet-based treatment for depressed adolescents. Clinical Child Psychology and Psychiatry, 27(3), 135910452210811. https://doi.org/10.1177/13591045221081193
- Munder, T., Brütsch, O., Leonhart, R., Gerger, H., & Barth, J. (2013). Researcher allegiance in psychotherapy outcome research: An overview of reviews. Clinical Psychology Review, 33(4), 501–511. https://doi.org/10.1016/j.cpr.2013.02.002
- Nezu, A. M. & Nezu, C. M. (2008). Evidence-based outcome research: A practical guide to conducting randomized controlled trials for psychosocial interventions. Oxford University Press.
- Norcross, J. C., Beutler, L. E., & Levant, R. F. (Eds.). (2006). Evidence-based practices in mental health. Debate and dialogue on the fundamental questions. American Psychological Association.
- Okada, A. (2022). The health insurance system and psychoanalytic psychotherapy in Japan: The association with evidence-based practice. Psychoanalytic Psychotherapy, 36(4), 288–299. https://doi.org/10.1080/02668734.2021.1952648
- Philips, B. (2020). The quest for causality in psychotherapy research. Pragmatic Case Studies in Psychotherapy, 15(3), 271–280. https://doi.org/10.14713/pcsp.v15i3.2059
- Philips, B. & Falkenström, F. (2021). What research evidence is valid for psychotherapy research? Frontiers in Psychiatry, 11, 11. https://doi.org/10.3389/fpsyt.2020.625380
- Plakun, E. M. (2020). Access to psychoanalysis and psychotherapy in the US. Psychoanalytic Psychotherapy, 34(2), 100–110. https://doi.org/10.1080/02668734.2020.1750052
- Poulsen, S., Lunn, S., Daniel, S. I. F., Folke, S., Mathiesen, B. B., Katznelson, H., & Fairburn, C. G. (2013). A randomized controlled trial of psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia vervosa. The American Journal of Psychiatry, 171(1), 1–8. https://doi.org/10.1176/appi.ajp.2013.12121511
- Pretsky, J. (2020). Teaching empirical research in psychodynamic psychotherapy: How to make research really matter. In M. Leuzinger-Bohleber, M. Solms, & S. Arnold (Eds.), Outcome research and the future of psychoanalysis: Clinicians and researchers in dialogue (1st ed., pp. 238–248). Routledge. https://doi.org/10.4324/9780429281112
- Rief, W., Kopp, M., Awarzamani, R., & Weise, C. (2022). Selected trends in psychotherapy research: An index analysis of RCTs. Clinical Psychology in Europe, 42(2). https://doi.org/10.32872/cpe.7921
- Ryle, A. & Kerr, I. B. (2020). Introducing cognitive analytic therapy: Principles and practice of a relational approach to mental health (2nd ed.). John Wiley & Sons Ltd.
- Sackett, D. L., Rosenberg, W. M. C., Gray, J. A. M., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t. BMJ, 312(7023), 71–72. https://doi.org/10.1136/bmj.312.7023.71
- Salkovskis, P. & Wolpert, L. (2012). Does psychoanalysis have a valuable place in modern mental health services? BMJ, 344, e1188. https://doi.org/10.1136/bmj.e1188
- Seligman, M. E. P. (1995). The effectiveness of psychotherapy. The American Psychologist, 50(12), 965–974. https://doi.org/10.1037/0003-066X.50.12.965
- Shapiro, F. & Laliotis, D. (2011). EMDR and the adaptive information processing model: Integrative treatment and case conceptualization. Clinical Social Work Journal, 39(2), 191–200. https://doi.org/10.1007/s10615-010-0300-7
- Shedler, J. (2018). Where is the evidence for “evidence-based” therapy? The Psychiatric Clinics of North America, 41(2), 319–329. https://doi.org/10.1016/j.psc.2018.02.001
- Stefini, A., Salzer, S., Reich, G., Horn, H., Winkelmann, K., Bents, H., & Kronmüller, K. -T. (2017). Cognitive-behavioral and psychodynamic therapy in female adolescents with bulimia nervosa: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 56(4), 329–335. https://doi.org/10.1016/j.jaac.2017.01.019
- Steinert, C., Munder, T., Rabung, S., Hoyer, J., & Leichsenring, F. (2017). Psychodynamic therapy: As efficacious as other empirically supported treatments? A meta-analysis testing equivalence of outcomes. The American Journal of Psychiatry, 174(10), 943–953. https://doi.org/10.1176/appi.ajp.2017.17010057
- Svensson, M., Nilsson, T., Perrin, S., Johansson, H., Viborg, G., Falkenström, F., & Sandell, R. (2020, September). The effect of patient’s choice of cognitive behavioural or psychodynamic therapy on outcomes for panic disorder: A doubly randomised controlled preference trial. Psychotherapy and Psychosomatics, 90(2), 1–12. https://doi.org/10.1159/000511469
- Tasca, G. A., Town, J. M., Abbass, A., & Clarke, J. (2018). Will publicly funded psychotherapy in Canada be evidence based? A review of what makes psychotherapy work and a proposal. Canadian Psychology, 59(4), 293–300. https://doi.org/10.1037/cap0000151
- Thoma, N. C., McKay, D., Gerber, A. J., Milrod, B. L., Edwards, A. R., & Kocsis, J. H. (2012). A quality-based review of randomized controlled trials of cognitive-behavioral therapy for depression: An assessment and metaregression. The American Journal of Psychiatry, 169(1), 22–30. https://doi.org/10.1176/appi.ajp.2011.11030433
- Tolin, D. F. (2010). Is cognitive–behavioral therapy more effective than other therapies?a meta-analytic review. Clinical Psychology Review, 30(6), 710–720. https://doi.org/10.1016/j.cpr.2010.05.003
- Tolin, D. F. (2014). Beating a Dead Dodo Bird: Looking at signal vs. noise in cognitive-behavioral therapy for anxiety disorders. Clinical Psychology: Science and Practice, 21(4), 351–362. https://doi.org/10.1111/cpsp.12080
- Wampold, B. E., Flückiger, C., Del Re, A. C., Yulish, N. E., Frost, N. D., Pace, B. T., Goldberg, S. B., Miller, S. D., Baardseth, T. P., Laska, K. M., & Hilsenroth, M. J. (2017). In pursuit of truth: A critical examination of meta-analyses of cognitive behavior therapy. Psychotherapy Research, 27(1), 14–32. https://doi.org/10.1080/10503307.2016.1249433
- Wampold, B. E. & Imel, Z. E. (2015). The great psychotherapy debate: The evidence for what makes psychotherapy work (2nd ed.). Routledge/Taylor & Francis Group.
- Westen, D., Novotny, C. M., & Thompson-Brenner, H. (2004). The empirical status of empirically supported psychotherapies: Assumptions, findings, and reporting in controlled clinical trials. Psychological Bulletin, 130(4), 631–663. https://doi.org/10.1037/0033-2909.130.4.631
- Wittmann, L., Halpern, J., Adams, C. B. L., Orner, R. J., & Kudler, H. (2011). Prolonged exposure and psychodynamic treatment for posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 50(5), 521–522. https://doi.org/10.1016/j.jaac.2011.03.005
- Yakeley, J. (2020). Editorial. Psychoanalytic Psychotherapy, 34(2), 73–77. https://doi.org/10.1080/02668734.2020.1840858
- Yakeley, J. (2021). Editorial. Psychoanalytic Psychotherapy, 35(2), 85–88. https://doi.org/10.1080/02668734.2021.1939985
- Yeomans, F. (2007). Questions concerning the randomized trial of schema-focused therapy vs transference-focused psychotherapy. Archives of General Psychiatry, 64(5), 610–611. https://doi.org/10.1001/archpsyc.64.5.609-c
- Zilcha-Mano, S. (2019). Major developments in methods addressing for whom psychotherapy may work and why. Psychotherapy Research, 29(6), 693–708. https://doi.org/10.1080/10503307.2018.1429691