ABSTRACT
Burnout has garnered considerable attention from occupational health specialists for nearly 50 years. In this paper, we discuss three beliefs about burnout that remain ill-supported despite their popularity among researchers and their importance for burnout research. The three beliefs are the following: (a) work-related factors are the prime predictors of burnout; (b) burnout is a condition of epidemic magnitude in contemporary society; (c) burnout is not a depressive condition. As we examine these widely held views, we outline possible paths to clarification to aid future research. We close our commentary by recommending that researchers be vigilant about the risk of drawing premature conclusions about burnout.
Burnout has elicited increasing interest among occupational health specialists since the introduction of the construct in the mid-1970s. As we write these lines, the keyword “burnout” generates nearly 20,000 hits in PsycINFO. In addition to being a popular indicator of job-related distress in academic research, burnout has resonated with contemporary sociocultural concerns and gained traction among the general public (Maslach et al., Citation2001; Schaufeli et al., Citation2009). Today, burnout is commonly presented as a global crisis (The Lancet, Citation2019).
Burnout has been generally defined as “a state of exhaustion in which one is cynical about the value of one’s occupation and doubtful of one’s capacity to perform” (Maslach et al., Citation1996, p. 20). The World Health Organization (Citation2019, Citation2022) incorporated this definition of burnout in the latest edition of the International Classification of Diseases (ICD-11). The ICD-11 does not classify burnout as a medical condition but includes the entity among the “factors influencing health status or contact with health services.” Burnout has been regarded as a syndrome resulting from insurmountable work-related adversity (Demerouti et al., Citation2021; Maslach et al., Citation2001; Shirom, Citation2005). The ICD-11 stipulates that burnout “refers specifically to phenomena in the occupational context and should not be applied to describe experiences in other areas of life.”
Although burnout has become a focal concern in occupational health science, substantial discrepancies exist between what can be considered established knowledge about the phenomenon and what can be regarded as prenotions or published opinions (Bianchi & Schonfeld, Citation2023; Enzmann, Citation2005; Schwenk & Gold, Citation2018; Weber & Jaekel-Reinhard, Citation2000). In this paper, we discuss three beliefs about burnout that remain ill-supported despite their popularity among researchers and their importance for burnout research. The three beliefs are the following: (a) work-related factors are the prime predictors of burnout; (b) burnout is a condition of epidemic magnitude in contemporary society; and (c) burnout is not a depressive condition. As we scrutinise these widely held views, we outline possible paths to clarification that may aid future research.
Raising awareness about the ill-supported beliefs that surround burnout is of scientific value for fostering knowledge accumulation and guiding research efforts (Taris, Citation2006). Such awareness is also important from an applied standpoint. For example, unduly assuming that work-related factors are the principal predictors of burnout may lead investigators to disregard significant (work-unrelated) etiological factors when planning interventions for mitigating burnout, thereby limiting the effectiveness of these interventions (Dreison et al., Citation2018; Lambreghts et al., Citation2023; Sen, Citation2022). Claiming that burnout is a ubiquitous condition without compelling evidence may be confusing to public health decision-makers who need to base policies on solid research findings (Bianchi & Laurent, Citation2018; Rotenstein et al., Citation2018). Failing to appreciate the overlap of burnout with depression may lead working individuals to be misdiagnosed and receive inappropriate treatment, with potentially lethal consequences such as work-related suicide (Schonfeld, Citation2018; Sen, Citation2022). In sum, clarifying our understanding of burnout is crucial to accomplishing our goal of supporting and protecting our workforce.
Belief 1: Work-related factors are the prime predictors of burnout
The idea that work-related factors are the core determinants of burnout has been an integral part of the syndrome’s conceptualisation (Maslach, Citation1976; Maslach et al., Citation2001; Schaufeli & Enzmann, Citation1998). In the research literature, one commonly reads statements such as “job variables and the organisational context are the prime predictors of burnout” (Maslach & Leiter, Citation2016, p. 355). Such views have been embraced by the World Health Organization (Citation2019), which currently characterises burnout as a syndrome “resulting from chronic workplace stress.”
A large body of research has documented associations between work-related factors and burnout (Aronsson et al., Citation2017; Halbesleben, Citation2006; Schonfeld & Chang, Citation2017; Seidler et al., Citation2014). Such factors have often been approached in terms of job demands (e.g. workload) and job resources (e.g. social support). They have also been conceived of in terms of the reciprocity between what workers give to their job and what they get from it (e.g. in the effort-reward imbalance model). The associations of burnout with work-related factors have recently been summarised by Guthier et al. (Citation2020) in a sophisticated meta-analysis. The authors investigated the links between job stressors (e.g. workload, time pressure, role conflict) and burnout across 48 longitudinal studies representing 26,319 participants. In addition to considering reciprocal effects between job stressors and burnout, the study team took into account between-study variations in time intervals and evaluated various sources of bias. Consistent with past research, Guthier et al.’s (Citation2020) meta-analysis did find a link between job stressors and burnout. The authors, however, found that the link was modest and likely biased upward. Moreover, post hoc statistical power analyses revealed that the detection of an effect of job stressors on burnout had mainly been a matter of chance. Looking into the directionality of the effects, Guthier et al.’s (Citation2020) observed that the evidence that burnout predicts exposure to job stressors is more solid (e.g. less affected by small-sample bias and HARKing) than the evidence that exposure to job stressors predicts burnout. All in all, such findings suggest that work-related factors may not explain most of the variance in burnout. The magnitude of the link between job stressors and burnout (or vice versa) might be further inflated by the exclusive use of self-report measures in the studies of interest (Podsakoff et al., Citation2024). Reliance on more diversified and “objective” indicators of stress and health may result in even smaller links.
In their 48-study meta-analysis, Guthier et al. (Citation2020) marshalled what might be the best of the evidence accumulated over the past five decades, and the authors’ conclusions are quite clear: “The present results show that job stressors such as workload have only small effects on burnout. Therefore, many other causes of burnout are likely to exist” (p. 1165). However, one might contend that job stressors do constitute the main determinants of burnout and that past studies simply failed to capture this link because (a) job stressors were not properly measured, (b) burnout was not properly measured, and/or (c) longitudinal studies were not designed in a way that allowed the temporal ordering of X (job stressors) and Y (burnout) to be nailed down. While the importance of such measurement and design issues is difficult to overstate, the evidence base and rationale for contending that job stressors constitute the main determinants of burnout would remain to be presented. Taking a clinical perspective on burnout, van Dam noted that stressors from virtually any domain of life can be expected to contribute to the development of a syndrome such as burnout. This view stems from the observation that the bodily stress response does not discriminate job stressors from stressors encountered in other spheres of life. The hypothalamic–pituitary–adrenal (HPA) and sympathetic-adrenal-medullary (SAM) axes are context-agnostic.
Guthier et al.’s (Citation2020) findings comport with those of an earlier meta-analysis conducted by Lesener et al. (Citation2019). Lesener et al. (Citation2019) focused on the (reciprocal) relationships between job demands and resources, on the one hand, and burnout, on the other. In an examination of 29 high-quality longitudinal studies (N = 14,486), these authors found that job demands and resources explained little variance in burnout. In line with Guthier et al.’s (Citation2020) results, Lesener et al. (Citation2019) found that burnout had a greater effect on job demands than vice versa. Importantly, that job demands and resources explain little variance in burnout does not render the finding trivial. The finding allows us to identify contributing factors, which is valuable from the standpoint of fundamental knowledge and may be of practical significance at the population level (Faragher et al., Citation2005). It remains, however, that if the impact of job demands and resources on burnout is small, other factors are likely to be involved in the development of burnout (e.g. stress factors unrelated to the job, dispositional factors, physical health). By implication, focusing only on job demands and resources may considerably limit our ability to address burnout. Lesener et al.’s (Citation2019) and Guthier et al.’s (Citation2020) results are consistent with the finding that vast proportions of individuals do not consider their work to be the main cause of their burnout symptoms (e.g. Bianchi & Brisson, Citation2019).
Though at the heart of burnout’s conceptualisation from inception, the idea that job-related stressors are the main drivers of burnout’s development emerged from crude observations. Maslach (Citation1976) attributed burnout symptoms to the action of job-related stressors at a time when no systematic research had been conducted on the syndrome. Now that burnout research has developed, rich meta-analytic findings are available (Guthier et al., Citation2020; Lesener et al., Citation2019). By pointing out lots of unknowns, these meta-analytic findings invite us to be cautious in how we approach burnout’s etiology. It may be premature to conclude that burnout is preponderantly or specifically induced by job stress and consider the case closed. Hakanen and Bakker (Citation2017) recommended that stress factors unrelated to the job (e.g. negative life events) be paid much more attention in burnout research as they may have direct and moderating effects of significant importance. Similar recommendations can be made for personality traits such as neuroticism (Bianchi, Citation2018; Swider & Zimmerman, Citation2010) and physical disorders that can give rise to burnout-like symptomatology (e.g. sleep-wake disorders or thyroid disorders). To develop effective interventions, it is crucial that researchers expand their knowledge of the factors involved in the development of burnout.
Belief 2: Burnout is a condition of epidemic magnitude
Research aimed at estimating the prevalence of burnout has grown in recent years (McCammon et al., Citation2023; Rotenstein et al., Citation2018). Many studies have concluded that burnout is alarmingly widespread (e.g. Banerjee et al., Citation2017). A recent Gallup (Citation2020) survey estimated that burnout prevalence might be as high as 76% in the U.S. workforce. At the level of specific occupations, a broadly relayed figure is that about 50% of U.S. physicians suffer from burnout (Shanafelt et al., Citation2017; The Lancet, Citation2019). Addressing burnout among Canadian healthcare workers, Leiter mentioned a dramatic increase in burnout prevalence from 14% to 23% in relation to the COVID-19 pandemic (see Lievens, Citation2021). Based on such numbers, investigators have concluded that burnout has reached epidemic levels in contemporary life (e.g. Lemaire & Wallace, Citation2017). But what, exactly, do we know about burnout prevalence?
The answer to the question of whether burnout is widespread or not is straightforward: Nobody knows. In effect, research on burnout prevalence has been hindered by the absence of established criteria for diagnosing the condition (Brisson & Bianchi, Citation2017; Rotenstein et al., Citation2018; Schwenk & Gold, Citation2018). Diagnostic criteria enable investigators to identify and characterise a given entity. The availability of a clearly defined, clinically valid diagnosis for burnout is a prerequisite for identifying cases and counting them in an effort to calculate prevalence estimates.
Studies of burnout prevalence have relied on identification criteria that have been arbitrary, in the sense that the criteria lack a sound clinical and theoretical basis (Rotenstein et al., Citation2018). Many of these studies have employed the Maslach Burnout Inventory (MBI), capitalising on cut-offs published in the MBI Manual (Maslach et al., Citation1996). These cut-offs, however, merely reflect tercile splits of convenience samples of workers recruited during early MBI research. As underscored by Schaufeli et al. (Citation2009, p. 212):
“ … such cutoffs are based on frequency distributions and therefore do not refer to an external criterion. For example, a score at the 70th percentile on exhaustion is relatively high, but it may not be associated with subjective distress, health disorders, or poor performance.”
“The MBI authors realized that the cut-offs were problematic and a ‘mistake’. For this reason, the cut-offs were not published in the MBI Manual fourth edition and were removed from all associated MBI materials.”
The plausibility of the sky-high prevalence estimates reported in numerous burnout studies has been questioned. Many investigators suspect that such estimates pathologise ordinary variations in stress, fatigue, or motivation and fail to circumscribe clinically relevant levels of symptoms (Bianchi et al., Citation2015; Fargen, Citation2022; Friedman, Citation2019; Rotenstein et al., Citation2018; Sethi et al., Citation2015). The health and social hazards of such “diagnosis creep” have been increasingly recognised (e.g. Hofmann, Citation2022), including the problem of harm trivialisation and the risk of promoting a sense of weakness and helplessness in the population (Dakin et al., Citation2023; Haslam, Citation2016). These hazards call for greater caution on how the issue of burnout prevalence is handled.
We recommend that investigators wishing to estimate burnout prevalence first perform the groundwork required to generate and validate clear diagnostic criteria for the condition. Establishing diagnostic criteria would involve a specification of (a) a consistent pattern of co-occurring symptoms and signs to be considered in clinical assessments, (b) the minimum required duration, frequency, and severity of the experienced symptoms, (c) the expected impact of the exhibited symptoms on the affected individual’s (working) life, (d) a description of the condition’s course, and (e) differential diagnosis procedures allowing the condition to be accurately delimited, not only from other psychological conditions but also from physical diseases that may implicate “mimicking” symptoms (American Psychiatric Association, Citation2013; Robins & Guze, Citation1970). Interestingly, the Swedish and Dutch medical classifications include diagnosable conditions that bear resemblance to burnout (GGZ Standaarden, Citation2018; Lindsäter et al., Citation2022). These conditions, however, diverge in significant ways from what the syndrome is supposed to be according to researchers such as Maslach or the World Health Organization. First, the diagnosis of these conditions does not require an etiological link to work. Second, the symptoms specified do not match the symptoms reflected in the MBI and incorporated by the World Health Organization. Adding a layer of complexity, the diagnostic criteria in Sweden and The Netherlands differ from each other.
Scanning the research literature, one can find several attempts to adopt a diagnostic approach to burnout based on such putative “proxies” (e.g. Kleijweg et al., Citation2013; Lundgren-Nilsson et al., Citation2012; Schaufeli et al., Citation2001). To our knowledge, the most recent attempt was made by Schaufeli et al. (Citation2023) in a study that used the Burnout Assessment Tool (BAT), a measure reflecting an alternative definition of burnout (Schaufeli et al., Citation2020). The authors’ work resulted in tentative identification criteria for “burnout disorder” (Schaufeli et al., Citation2023, p. 300). Following these identification criteria, experiencing burnout symptoms “sometimes” is sufficient to be categorised as a clinical case and to be considered eligible for interventions. The notion that individuals who occasionally lack energy and motivation at work suffer from a disorder, require sick leave, and need treatment once more raises the issue of diagnosis creep. In addition to being medically questionable, such an extension of the domain of pathology may be detrimental to society and the economy. It may pose serious challenges for organisations, healthcare systems, and welfare states, including sustainability challenges (Hjörleifsson & Getz, Citation2023; Johansson et al., Citation2019). This BAT-related example illustrates the intricacies associated with addressing burnout diagnosis. These intricacies call for a broader and deeper discussion of diagnostic approaches to burnout.
Many researchers consider that binding diagnostic criteria for burnout are long overdue (e.g. Fargen, Citation2022; Rotenstein et al., Citation2018). For these investigators, a focus on the end state of the burnout process is crucial because it is where people’s health and ability to function are expected to be impaired (Schaufeli & Enzmann, Citation1998; Tyssen, Citation2018). A diagnosis is meant to differentiate individuals who have reached this clinically relevant stage from those who are experiencing benign (and inevitable) fluctuations in their levels of stress, fatigue, or motivation. The view favouring a diagnosis for burnout, however, is not unanimously shared among researchers. Maslach and Leiter (Citation2022), for instance, have expressed strong doubts regarding the benefit of approaching burnout diagnostically (see also Maslach & Leiter, Citation1997). From these authors’ standpoint, diagnostic approaches may lead to “victim-blaming” by instilling the idea that the worker, rather than the workplace, is “responsible” for burnout. Following this line of reasoning, diagnostic approaches would eventually lead to an over-individualization of job-related distress. While such concerns may not be unjustified, they have nontrivial implications. Without a diagnosis, it is not possible to ascertain whether someone suffers from burnout, differentiate someone with burnout from someone without burnout, or estimate the prevalence of burnout. These implications should be borne in mind when discussing the pros and cons of developing a diagnosis for burnout.
Belief 3: Burnout is not a depressive condition
Burnout was not introduced in the research literature after a systematic review of already identified stress-related conditions or in studies that empirically examined the construct’s (discriminant) validity (e.g. Maslach, Citation1976, Citation1978; Maslach & Pines, Citation1977). The issue of whether the burnout syndrome represented a “genuine phenomenon” thus elicited attention early on. As the outcome par excellence of experiences of intractable stress (Dohrenwend, Citation2000; Laborit, Citation1977; Pryce et al., Citation2011; Seligman, Citation1975; Wichers, Citation2014; Willner et al., Citation2013), depression emerged as a target of choice in research on burnout’s distinctiveness (e.g. Farber, Citation1983; Meier, Citation1984). Although skeptical voices have been heard here and there over the years (e.g. Firth et al., Citation1986; Kasl, Citation1998; Schonfeld, Citation1991), the view that burnout constitutes a standalone syndrome that is separate from depression has dominated the field (e.g. Maslach & Leiter, Citation2016; Melnick et al., Citation2017). Does the state of the art safely support this view?
Depressive conditions are primarily characterised by symptoms of anhedonia (i.e. loss of interest and pleasure, social withdrawal, loss of motivation, feeling of “not caring anymore”) and dysphoria – also known as depressed mood (e.g. feelings of helplessness and hopelessness, sadness, irritability, sense of frustration). Another cardinal feature of depression is exhaustion, considered both psychologically and physically. For the affected individual, “[e]ven the smallest tasks seem to require substantial effort” (American Psychiatric Association, Citation2022, p. 186). Fatigue and loss of energy are common presenting complaints of depressed individuals in clinical consultations. Other diagnostic symptoms include cognitive impairment, neuro-vegetative alterations (e.g. disrupted sleep), feelings of guilt or worthlessness (e.g. beliefs that one’s actions or contributions have no significance, ruminations about past failings), psychomotor disturbances, and suicidality (from fleeting thoughts of self-harm to suicide planning and attempts). Loss of emotional involvement, reduced empathy, and interpersonal distancing are frequent manifestations of the social impairment that afflicts depressed individuals (Beck & Alford, Citation2009; Kupferberg et al., Citation2016). The 12-month prevalence of major depressive disorder is estimated at 5% in Europe and 6%−7% in the U.S.A. (American Psychiatric Association, Citation2022; Paykel et al., Citation2005; Weinberger et al., Citation2018).
Depression involves an imbalance between positive and negative affect thought to reflect a gap between positive-rewarding and negative-punitive experiences (Gilbert, Citation2006; Grahek et al., Citation2019; Pryce et al., Citation2011; Rolls, Citation2016; Wichers, Citation2014; Willner et al., Citation2013). Unresolvable stress, which generates such an adverse discrepancy, has been identified as a basic depressogenic factor in individuals with no noticeable susceptibility to depression (Bianchi et al., Citation2021; Dohrenwend, Citation2000; Grahek et al., Citation2019; Pryce et al., Citation2011; Seligman, Citation1975; Willner et al., Citation2013). As emphasised by the World Health Organization (Citation2023), “[d]epression can happen to anyone”; although certain individuals have characteristics that make them more vulnerable to depressive decompensation (e.g. affective, cognitive, behavioural, social, economic, metabolic, [epi]genetic characteristics), even the strongest, most resilient and resourceful individuals have adaptive limits and can succumb to depression when their defenses and coping abilities are overwhelmed.
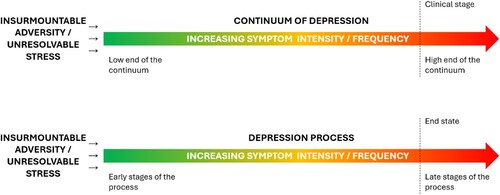
In keeping with contemporary trends in psychopathological science (Haslam et al., Citation2023; Kotov et al., Citation2017; Wichers, Citation2014), depression has been approached both categorically (i.e. diagnostically, as a taxon; “all-or-nothing” approach) and dimensionally (i.e. spectrally, as a continuum; “more-or-less” approach). Pickles and Angold (Citation2003) employed an analogy based on the “duality” of light, a phenomenon having both wave – and particle-like properties, to illustrate the fundamental complementarity of dimensional and categorical approaches to psychopathology. An integrative view of depression, assorting dimensional and categorical approaches, is provided in . A dimensional approach can be particularly useful in examining the dynamics of etiological processes and symptom development(Wichers, Citation2014). A categorical approach can serve screening and diagnostic purposes and help clinicians, organisations, or public health professionals in their decision-making (Pickles & Angold, Citation2003).
Figure 1. View of depression that integrates dimensional and categorical frameworks. The clinical stage of depression, at which a depressive disorder can potentially be diagnosed, is an integral part of the depression continuum – it reflects the high end of that continuum. The two representations, top and bottom, have the same meaning. The illustration at the bottom distinguishes itself by using the state/process terminology found in burnout research.
Theoretical arguments pertaining to the burnout-depression distinction have been dissected on several occasions (e.g. Bianchi et al., Citation2019; Shirom, Citation2005; Verkuilen et al., Citation2021). Perhaps the most frequently invoked justification for singling out burnout has been the “job-relatedness” ascribed to the syndrome (e.g. Maslach et al., Citation2001; Schaufeli et al., Citation2009). From this perspective, burnout is specific to work whereas depression is “context-free” and can originate in any domain of life. Though popular, this line of reasoning has raised objections. Bianchi et al. (Citation2021), for instance, pointed out that burnout could be job-related and depressive in nature without contradiction. The link between job stress and depression is well-established (Niedhammer et al., Citation2021; Schonfeld & Chang, Citation2017; Sen, Citation2022), and explicit in research on occupational depression (Bianchi & Schonfeld, Citation2020; Rydmark et al., Citation2006). A related idea is that job-relatedness is largely irrelevant to the fundamental nature of a condition – e.g. job-related depression is depression, job-related back pain is back pain, job-related cancer is cancer (Bianchi et al., Citation2019; Sen, Citation2022). Following a domain-based argument, burnout could be seen as nested within the realm of depression rather than separate from it. Taking the issue the other way around, several authors have considered that burnout can be construed in a context-free fashion (e.g. Kristensen et al., Citation2005). Such authors include pioneers of burnout research (Pines et al., Citation1981). Overall, the field has been quite divided about the rationale underlying the burnout-depression distinction. For some, burnout is rendered unique by its occupational prism. For others, the job-relatedness argument acts as a red herring in the debate on the fundamental nature of the burnout phenomenon.
Another issue that has piqued the attention of researchers concerns the coordination of dimensional and categorical approaches in burnout research. According to Verkuilen et al. (Citation2021), the debate on burnout and depression has been obscured by a tendency to reduce depression to its clinical stage. Because the clinical stage of depression reflects only a fraction of the continuum of depression – its high end (), such reduction has been regarded as a significant truncation of the depression phenomenon, likely to distort the burnout-depression comparison. The conjecture that burnout is a phase in the development of a depressive disorder (Maslach & Leiter, Citation2016), for example, implies a focus restricted to the clinical stage of depression. Such a conjecture becomes more difficult to navigate when the continua of burnout and depression are considered in their entirety.
The question has been raised of whether burnout-related concepts (e.g. exhaustion, cynicism, and inefficacy) partly reference depressive symptoms using nonmedical terminology (Bianchi et al., Citation2019). This concern, which is not new (Kasl, Citation1998; Schonfeld, Citation1991), aligns with the broader view that burnout may be “uncomfortably close to depressive symptomatology” (Taris, Citation2006, p. 101). Loss of energy and loss of motivation, which have been described as the two pillars of burnout (Schaufeli & Taris, Citation2005), are nodal symptoms of depression (American Psychiatric Association, Citation2022; Beck & Alford, Citation2009). Other descriptions of burnout are highly reminiscent of depression. For example, Maslach and Leiter (Citation1997) underlined that (a) burnout is not only about the “presence of negative emotions” but also about the “absence of positive ones” and (b) in burnout, “positive feelings erode to the point that they no longer have the power to offset the negatives” (p. 28). The authors wrote that “[b]urnout can have a deadly impact even beyond its erosion of the soul” (p. 18). Schaufeli and Enzmann (Citation1998) indicated that “[f]irst and foremost, the burned-out professional feels helpless, hopeless, and powerless” (p. 25). All these characteristics are hallmarks of depression (American Psychiatric Association, Citation2022: Beck & Alford, Citation2009; Peterson et al., Citation1993). In fact, one could replace the terms “burnout” and “burned-out” with the terms “depression” and “depressed” in the abovementioned descriptions without generating any counter-sense. Such interchangeability is not expected when dealing with distinct conditions. Fuelling theoretical reflections on burnout and depression with historical considerations, Schaffner (Citation2016) observed that entities such as nervous weakness (described in the eighteenth century), neurasthenia (described in the nineteenth century), and burnout (described in the twentieth century) could be regarded as successive avatars of melancholic weariness, a depressive condition already theorised by physicians of the Hellenic and Roman eras.
On the empirical side, several studies have challenged the burnout-depression distinction over the last decade. For instance, in a three-wave, seven-year cluster analytic study of nearly 2,000 participants, Ahola et al. (Citation2014) found burnout and depressive symptoms to be interwoven. The authors concluded that “burnout could be used as an equivalent to depressive symptoms in work life” (p. 35). In a factor-analytic study involving 14 samples and over 12,000 participants, Bianchi et al. (Citation2021) observed that burnout problematically overlaps with depression and “does not present the unity expected of a distinct syndrome” (p. 589). Bianchi et al.’s (Citation2021) study is, to our knowledge, the largest and most sophisticated factor-analytic study of burnout-depression overlap available. Recent studies that assessed depressive symptoms with the Occupational Depression Inventory (ODI) cast further doubt on the distinctiveness and coherence of the burnout construct (e.g. Schonfeld & Bianchi, Citation2022; Sowden et al., Citation2022). The ODI focuses on depressive symptoms that individuals specifically attribute to their work (Bianchi et al., Citation2023; Bianchi & Schonfeld, Citation2020; Bianchi & Sowden, Citation2022).
One particularly intriguing finding, documented in dozens of studies, is that burnout’s core feature – exhaustion – correlates more strongly with depressive symptoms than it does with cynicism and inefficacy – the two other defining features of burnout. Such a pattern of results does not comport with the notion that burnout constitutes a stand-alone syndrome (Hodson, Citation2021). By definition, a syndrome refers to a set of symptoms and signs grouped based on their frequent co-occurrence (American Psychiatric Association, Citation2013; Shirom, Citation2005). If exhaustion co-occurs less frequently with cynicism and inefficacy than with depressive symptoms, then why are cynicism and inefficacy considered part of the burnout syndrome while depressive symptoms are not? This crucial issue has been a blind spot in the case made for burnout’s distinctiveness. Two comprehensive meta-analyses did not compare the correlations among burnout symptoms to the correlations between burnout symptoms and depressive symptoms (Koutsimani et al., Citation2019; Meier & Kim, Citation2022). Such a comparison should be high on our agenda given its potential for clarifying the issue of burnout-depression overlap.
When addressing the correlations between burnout and depression, it could be useful to more closely consider the measures utilized. A proper examination of burnout-depression overlap requires, for instance, that the depression scales employed cover depressive symptoms comprehensively. While scales such as the PHQ-9 tend to do so (Bianchi et al., Citation2022), with a focus on each of the nine diagnostic symptoms of major depression, other scales exhibit a narrow symptom scope, leading to truncated assessments. The Four-Dimensional Symptom Questionnaire (4DSQ), for example, focuses only on a small number of depressive symptoms, omitting key features of depression such as fatigue and loss of energy or cognitive impairment (Terluin et al., Citation2004). Relying on such scales is inadvisable if the goal is to clarify the issue of burnout-depression overlap further.
The difficulty identifying tangible differences between burnout and depression has manifested itself on an interventional level. Clinicians have often regarded the burnout-depression distinction as having little therapeutic significance (e.g. Durand-Moreau & Dewitte, Citation2015; Plys et al., Citation2022; Schwenk & Gold, Citation2018). It would be important for burnout researchers to clarify what exactly should be done to help burned-out workers that would be unhelpful to depressed workers, and vice versa. To date, attempts at burnout-specific interventions have not been fully conclusive (Dreison et al., 2018; Haslam et al., 2023; Lambreghts et al., 2023). Because untreated depression can lead to fatal outcomes, primarily suicide (Chesney et al., Citation2014), the risk of withholding life-saving treatments for depression from individuals labelled as “burned-out” needs to be carefully considered.
The debate on burnout-depression overlap has given rise to a questioning of the original research that led investigators to consider that (a) an entity such as “burnout” existed in its own right, i.e. as a stand-alone syndrome irreducible to already described stress-related conditions, and (b) such an entity was aptly defined as a syndrome of exhaustion, cynicism, and inefficacy symptoms. The MBI, which crystallised this three-component definition of burnout (Maslach & Jackson, Citation1981), was “neither grounded in firm clinical observation nor based on sound theorising” (Schaufeli, Citation2003, p. 3; see also Shirom, Citation2005). The MBI was developed based on anecdotal reports and rudimentary studies (e.g. Maslach, Citation1976, Citation1978; Maslach & Pines, Citation1977; see also Bianchi & Schonfeld, Citation2023). Moreover, Schaufeli and Enzmann (Citation1998) observed that the development of the MBI involved unclear operations and arbitrary decisions at the level of item creation and item selection. Enzmann (Citation2005, p. 497) underlined the implications of this modus operandi:
“It is quite conceivable that another pool of items could have resulted in different dimensions of burnout … It is likely that this would have led to a different definition of burnout and it could have changed the course of research on burnout considerably.”
While some investigators have embarked on a redefinition journey, others worry about the overall framework of burnout research and the possible side-effects of the construct’s extensive use. On the clinical and public health fronts, for example, the captation of the issue of job-related distress by the burnout construct has raised ethical alarms (Oquendo et al., Citation2019; Schonfeld, Citation2018; Sen, Citation2022). A concern is that burnout may divert us from the potentially tragic consequences of unresolvable job stress, including depressive disorders and suicide (Bianchi et al., Citation2023; Greiner & Arensman, Citation2022; Howard et al., Citation2022). This concern is well illustrated by Sen (Citation2022, p. 1630) in relation to physician distress:
“ … despite the conceptualization of burnout as being unique as a work-related phenomenon, work-related stress is the primary driver of depression among physicians … Crucially, identification and treatment of depression can help reduce the risk of suicide among physicians. Unfortunately, when we encourage clinicians to consider themselves burned out rather than depressed, they tend not to seek or receive the individual-level interventions that can improve well-being.”
Concluding remarks
Much has been written on burnout since the mid-1970s. The state of science suggests that some of the beliefs that have structured and justified burnout research remain ill-supported and need to be treated with greater caution.
Various paths to clarification can be envisaged by burnout researchers. Regarding the elucidation of burnout’s etiology, a fruitful strategy might be to design follow-up studies assessing multiple candidate predictors of burnout simultaneously. The inclusion of work-related, work-unrelated, and dispositional factors and the examination of the possible interactions among those factors could be informative. The use of more diversified and “objective” indicators of stress and health may help limit estimation biases linked to common method variance.
Regarding the issue of burnout prevalence, establishing a clear and clinically valid diagnosis for burnout constitutes an essential preliminary step. Importantly, being able to identify individuals with burnout is a prerequisite for prevalence estimation whether one prefers to designate burnout as a syndrome, an illness, or a disorder (Bianchi et al., Citation2023). In making these observations, our point is not to either encourage or discourage a “disease framework” in burnout research. Our point is to call for coherence in how the diagnosis and prevalence issues are coordinated. One cannot count burnout cases if one cannot diagnose burnout cases.
An intensified cross-disciplinary dialogue may help clarify the nature of the phenomenon that the burnout construct is supposed to represent. For instance, biological research tells us that, as biological systems, human beings cannot respond to intractable stress in an infinity of ways. Our biological structure and architecture define and constrain the range of our responses to insurmountable adversity (Lewontin, Citation2000; Sapolsky, Citation2004). While various constructs have been used across history and scholarly traditions for studying such responses, what these constructs capture has been commonly boiled down to two sets of manifestations, namely, anxiety and depressive symptoms (Frank, Citation1974; Kessler et al., Citation2003; Laborit, Citation1977; Lang & McTeague, Citation2009; Nesse, Citation2000; Sapolsky, Citation2021; Seligman, Citation1975; Wichers, Citation2014). Given this backdrop, the proposition that burnout is both a response to intractable stress and a sui generis phenomenon is difficult to articulate. A strengthened dialogue between occupational health psychology and neurobiology may help researchers evaluate the view that burnout stands apart from and outside the spectra of anxiety and depressive conditions.
As researchers, it is our responsibility to avoid propagating narratives that rest on insufficient evidence. This responsibility is critical when such narratives have health implications, as is the case with the narratives surrounding burnout. We believe renewed research efforts are needed before one can make confident claims about the etiology, the prevalence, or the nature of the burnout phenomenon. We hope this paper will stimulate debate on burnout and help strengthen research on job-related distress.
Cautionary note
The views expressed in Work & Stress position papers are those of the author(s) and do not necessarily represent those of the journal or of any other person or organisation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ahola, K., Hakanen, J., Perhoniemi, R., & Mutanen, P. (2014). Relationship between burnout and depressive symptoms: A study using the person-centred approach. Burnout Research, 1(1), 29–37. https://doi.org/10.1016/j.burn.2014.03.003
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). American Psychiatric Publishing.
- Aronsson, G., Theorell, T., Grape, T., Hammarström, A., Hogstedt, C., Marteinsdottir, I., Skoog, I., Träskman-Bendz, L., & Hall, C. (2017). A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health, 17(1), 264. https://doi.org/10.1186/s12889-017-4153-7
- Banerjee, S., Califano, R., Corral, J., de Azambuja, E., De Mattos-Arruda, L., Guarneri, V., Hutka, M., Jordan, K., Martinelli, E., Mountzios, G., Ozturk, M. A., Petrova, M., Postel-Vinay, S., Preusser, M., Qvortrup, C., Volkov, M. N. M., Tabernero, J., Olmos, D., & Strijbos, M. H. (2017). Professional burnout in European young oncologists: Results of the European Society for Medical Oncology (ESMO) Young Oncologists Committee Burnout Survey. Annals of Oncology, 28(7), 1590–1596. https://doi.org/10.1093/annonc/mdx196
- Beck, A. T., & Alford, B. A. (2009). Depression: Causes and treatment (2nd ed.). University of Pennsylvania Press.
- Bianchi, R. (2018). Burnout is more strongly linked to neuroticism than to work-contextualized factors. Psychiatry Research, 270, 901–905. https://doi.org/10.1016/j.psychres.2018.11.015
- Bianchi, R., & Brisson, R. (2019). Burnout and depression: Causal attributions and construct overlap. Journal of Health Psychology, 24(11), 1574–1580. https://doi.org/10.1177/1359105317740415
- Bianchi, R., & Laurent, E. (2018). Editorial commentary: Burnout in cardiology—Going to the heart of the misunderstanding. Trends in Cardiovascular Medicine, 28(1), 8–9. https://doi.org/10.1016/j.tcm.2017.07.008
- Bianchi, R., Lavaux, M., & Brisson, R. (2015). Using liberal criteria to identify burnout poses the risk of pathologizing normal adaptive states. Academic Medicine, 90(12), 1584. https://doi.org/10.1097/ACM.0000000000000962
- Bianchi, R., & Schonfeld, I. S. (2020). The Occupational Depression Inventory: A new tool for clinicians and epidemiologists. Journal of Psychosomatic Research, 138, 110249. https://doi.org/10.1016/j.jpsychores.2020.110249
- Bianchi, R., & Schonfeld, I. S. (2023). Examining the evidence base for burnout. Bulletin of the World Health Organization, 101(11), 743–745. https://doi.org/10.2471/BLT.23.289996
- Bianchi, R., Schonfeld, I. S., & Laurent, E. (2019). Burnout: Moving beyond the status quo. International Journal of Stress Management, 26(1), 36–45. https://doi.org/10.1037/str0000088
- Bianchi, R., & Sowden, J. F. (2022). A paradigm shift from burnout to occupational depression. Journal of Affective Disorders, 303, 230–232. https://doi.org/10.1016/j.jad.2022.02.049
- Bianchi, R., Verkuilen, J., Schonfeld, I. S., Hakanen, J. J., Jansson-Fröjmark, M., Manzano-García, G., Laurent, E., & Meier, L. L. (2021). Is burnout a depressive condition? A 14-sample meta-analytic and bifactor analytic study. Clinical Psychological Science, 9(4), 579–597. https://doi.org/10.1177/2167702620979597
- Bianchi, R., Verkuilen, J., Sowden, J. F., & Schonfeld, I. S. (2023). Towards a new approach to job-related distress: A three-sample study of the Occupational Depression Inventory. Stress and Health, 39(1), 137–153. https://doi.org/10.1002/smi.3177
- Bianchi, R., Verkuilen, J., Toker, S., Schonfeld, I. S., Gerber, M., Brähler, E., & Kroenke, K. (2022). Is the PHQ-9 a unidimensional measure of depression? A 58,272-participant study. Psychological Assessment, 34(6), 595–603. https://doi.org/10.1037/pas0001124
- Brisson, R., & Bianchi, R. (2017). Stranger things: On the upside down world of burnout research. Academic Psychiatry, 41(2), 200–201. https://doi.org/10.1007/s40596-016-0619-7
- Chesney, E., Goodwin, G. M., & Fazel, S. (2014). Risks of all-cause and suicide mortality in mental disorders: A meta-review. World Psychiatry, 13(2), 153–160. https://doi.org/10.1002/wps.20128
- Dakin, B. C., McGrath, M. J., Rhee, J. J., & Haslam, N. (2023). Broadened concepts of harm appear less serious. Social Psychological and Personality Science, 14(1), 72–83. https://doi.org/10.1177/19485506221076692
- Demerouti, E., Bakker, A. B., Peeters, M. C. W., & Breevaart, K. (2021). New directions in burnout research. European Journal of Work and Organizational Psychology, 30(5), 686–691. https://doi.org/10.1080/1359432X.2021.1979962
- Dohrenwend, B. P. (2000). The role of adversity and stress in psychopathology: Some evidence and its implications for theory and research. Journal of Health and Social Behavior, 41(1), 1–19. https://doi.org/10.2307/2676357
- Dreison, K. C., Luther, L., Bonfils, K. A., Sliter, M. T., McGrew, J. H., & Salyers, M. P. (2018). Job burnout in mental health providers: A meta-analysis of 35 years of intervention research. Journal of Occupational Health Psychology, 23(1), 18–30. https://doi.org/10.1037/ocp0000047
- Durand-Moreau, Q., & Dewitte, J.-D. (2015). La création d’un tableau de maladie professionnelle pour le syndrome d’épuisement professionnel (burnout) n’est pas une bonne réponse pour sa prévention [Creating a new table of occupational diseases for burnout is not a good answer to prevent it]. La Presse Médicale, 44(12, Part 1), 1215–1218. https://doi.org/10.1016/j.lpm.2015.11.003
- Enzmann, D. (2005). Burnout and emotions: An underresearched issue in search of a theory. In A.-S. G. Antoniou & C. L. Cooper (Eds.), New horizons in management: Research companion to organizational health psychology (pp. 495–592). Elgar.
- Faragher, E. B., Cass, M., & Cooper, C. L. (2005). The relationship between job satisfaction and health: A meta-analysis. Occupational and Environmental Medicine, 62(2), 105–112. https://doi.org/10.1136/oem.2002.006734
- Farber, B. A. (1983). Stress and burnout in the human service professions. Pergamon Press.
- Fargen, K. M. (2022). The physician burnout conundrum: Where do we go from here? Journal of NeuroInterventional Surgery, 14(2), 105–106. https://doi.org/10.1136/neurintsurg-2022-018651
- Firth, H., McIntee, J., McKeown, P., & Britton, P. (1986). Burnout and professional depression: Related concepts? Journal of Advanced Nursing, 11(6), 633–641. https://doi.org/10.1111/j.1365-2648.1986.tb03380.x
- Frank, J. D. (1974). Psychotherapy: The restoration of morale. The American Journal of Psychiatry, 131(3), 271–274. https://doi.org/10.1176/ajp.131.3.271
- Friedman, R. A. (2019, June 3). Is burnout real? https://www.nytimes.com/2019/06/03/opinion/burnout-stress.html
- Gallup. (2020). Employee burnout: Causes and cures. https://www.gallup.com/workplace/282659/employee-burnout-perspective-paper.aspx
- GGZ Standaarden. (2018). Zorgstandaard Aanpassingsstoornis (incl. overspanning en burn-out). https://www.ggzstandaarden.nl/zorgstandaarden/aanpassingsstoornis-incl-overspanning-en-burn-out/over-de-aanpassingsstoornis/inleiding/burn-out
- Gilbert, P. (2006). Evolution and depression: Issues and implications. Psychological Medicine, 36(3), 287–297. https://doi.org/10.1017/S0033291705006112
- Grahek, I., Shenhav, A., Musslick, S., Krebs, R. M., & Koster, E. H. W. (2019). Motivation and cognitive control in depression. Neuroscience & Biobehavioral Reviews, 102, 371–381. https://doi.org/10.1016/j.neubiorev.2019.04.011
- Greiner, B. A., & Arensman, E. (2022). The role of work in suicidal behavior – uncovering priorities for research and prevention. Scandinavian Journal of Work, Environment & Health, 48(6), 419–424. https://doi.org/10.5271/sjweh.4051
- Guthier, C., Dormann, C., & Voelkle, M. C. (2020). Reciprocal effects between job stressors and burnout: A continuous time meta-analysis of longitudinal studies. Psychological Bulletin, 146(12), 1146–1173. https://doi.org/10.1037/bul0000304
- Hakanen, J. J., & Bakker, A. B. (2017). Born and bred to burn out: A life-course view and reflections on job burnout. Journal of Occupational Health Psychology, 22(3), 354–364. https://doi.org/10.1037/ocp0000053
- Halbesleben, J. R. B. (2006). Sources of social support and burnout: A meta-analytic test of the conservation of resources model. Journal of Applied Psychology, 91(5), 1134–1145. https://doi.org/10.1037/0021-9010.91.5.1134
- Halbesleben, J. R. B., & Demerouti, E. (2005). The construct validity of an alternative measure of burnout: Investigating the English translation of the Oldenburg Burnout Inventory. Work & Stress, 19(3), 208–220. https://doi.org/10.1080/02678370500340728
- Haslam, N. (2016). Concept creep: Psychology’s expanding concepts of harm and pathology. Psychological Inquiry, 27(1), 1–17. https://doi.org/10.1080/1047840X.2016.1082418
- Haslam, A., Tuia, J., Miller, S. L., & Prasad, V. (2023). Systematic review and meta-analysis of randomized trials testing interventions to reduce physician burnout. The American Journal of Medicine, 137, 249–257.e1. https://doi.org/10.1016/j.amjmed.2023.10.003
- Hewitt, D. B., Ellis, R. J., Hu, Y.-Y., Cheung, E. O., Moskowitz, J. T., Agarwal, G., & Bilimoria, K. Y. (2020). Evaluating the association of multiple burnout definitions and thresholds with prevalence and outcomes. JAMA Surgery, 155(11), 1043–1049. https://doi.org/10.1001/jamasurg.2020.3351
- Hjörleifsson, S., & Getz, L. O. (2023). Editorial: The sustainability of universal health care. Journal of the Norwegian Medical Association, 2, 1–3. https://doi.org/10.4045/tidsskr.23.0025
- Hodson, G. (2021). Construct jangle or construct mangle? Thinking straight about (nonredundant) psychological constructs. Journal of Theoretical Social Psychology, 5, 576–590. https://doi.org/10.1002/jts5.120
- Hofmann, B. (2022). Too much, too mild, too early: Diagnosing the excessive expansion of diagnoses. International Journal of General Medicine, 15, 6441–6450. https://doi.org/10.2147/IJGM.S368541
- Howard, M. C., Follmer, K. B., Smith, M. B., Tucker, R. P., & Van Zandt, E. C. (2022). Work and suicide: An interdisciplinary systematic literature review. Journal of Organizational Behavior, 43(2), 260–285. https://doi.org/10.1002/job.2519
- Johansson, M., Bero, L., Bonfill, X., Bruschettini, M., Garner, S., Glenton, C., Harris, R., Jørgensen, K. J., Levinson, W., Lotfi, T., Montori, V., Meng, D. M., Schünemann, H., Vaz Carneiro, A., Woloshin, S., & Moynihan, R. (2019). Cochrane Sustainable Healthcare: Evidence for action on too much medicine. The Cochrane Database of Systematic Reviews, 12, ED000143. https://doi.org/10.1002/14651858.ED000143
- Kasl, S. V. (1998). Measuring job stressors and studying the health impact of the work environment: An epidemiologic commentary. Journal of Occupational Health Psychology, 3(4), 390–401. https://doi.org/10.1037/1076-8998.3.4.390
- Kessler, R. C., Barker, P. R., Colpe, L. J., Epstein, J. F., Gfroerer, J. C., Hiripi, E., Howes, M. J., Normand, S.-L. T., Manderscheid, R. W., Walters, E. E., & Zaslavsky, A. M. (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184–189. https://doi.org/10.1001/archpsyc.60.2.184
- Kleijweg, J. H. M., Verbraak, M. J. P. M., & Van Dijk, M. K. (2013). The clinical utility of the Maslach Burnout Inventory in a clinical population. Psychological Assessment, 25(2), 435–441. https://doi.org/10.1037/a0031334
- Kotov, R., Krueger, R. F., Watson, D., Achenbach, T. M., Althoff, R. R., Bagby, R. M., Brown, T. A., Carpenter, W. T., Caspi, A., Clark, L. A., Eaton, N. R., Forbes, M. K., Forbush, K. T., Goldberg, D., Hasin, D., Hyman, S. E., Ivanova, M. Y., Lynam, D. R., Markon, K., … Zimmerman, M. (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. https://doi.org/10.1037/abn0000258
- Koutsimani, P., Montgomery, A., & Georganta, K. (2019). The relationship between burnout, depression, and anxiety: A systematic review and meta-analysis. Frontiers in Psychology, 10, 284. https://doi.org/10.3389/fpsyg.2019.00284
- Kristensen, T. S., Borritz, M., Villadsen, E., & Christensen, K. B. (2005). The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress, 19(3), 192–207. https://doi.org/10.1080/02678370500297720
- Kupferberg, A., Bicks, L., & Hasler, G. (2016). Social functioning in major depressive disorder. Neuroscience & Biobehavioral Reviews, 69, 313–332. https://doi.org/10.1016/j.neubiorev.2016.07.002
- Laborit, H. (1977). Decoding the human message. Allison & Busby.
- Lambreghts, C., Vandenbroeck, S., Goorts, K., & Godderis, L. (2023). Return-to-work interventions for sick-listed employees with burnout: A systematic review. Occupational and Environmental Medicine, 80(9), 538–544. https://doi.org/10.1136/oemed-2023-108867
- The Lancet. (2019). Physician burnout: A global crisis. The Lancet, 394(10193), 93. https://doi.org/10.1016/S0140-6736(19)31573-9
- Lang, P. J., & McTeague, L. M. (2009). The anxiety disorder spectrum: Fear imagery, physiological reactivity, and differential diagnosis. Anxiety, Stress, and Coping, 22(1), 5–25. https://doi.org/10.1080/10615800802478247
- Lemaire, J. B., & Wallace, J. E. (2017). Burnout among doctors. BMJ, 358, j3360. https://doi.org/10.1136/bmj.j3360
- Lesener, T., Gusy, B., & Wolter, C. (2019). The job demands-resources model: A meta-analytic review of longitudinal studies. Work and Stress, 33(1), 76–103. https://doi.org/10.1080/02678373.2018.1529065
- Lewontin, R. (2000). The triple helix: Gene, organism, and environment. Harvard University Press.
- Lievens, D. (2021). How the pandemic exacerbated burnout. Harvard Business Review. https://hbr.org/2021/02/how-the-pandemic-exacerbated-burnout
- Lindsäter, E., Svärdman, F., Wallert, J., Ivanova, E., Söderholm, A., Fondberg, R., Nilsonne, G., Cervenka, S., Lekander, M., & Rück, C. (2022). Exhaustion disorder: Scoping review of research on a recently introduced stress-related diagnosis. BJPsych Open, 8(5), e159. https://doi.org/10.1192/bjo.2022.559
- Lundgren-Nilsson, Å., Jonsdottir, I. H., Pallant, J., & Ahlborg, G., Jr. (2012). Internal construct validity of the Shirom-Melamed Burnout Questionnaire (SMBQ). BMC Public Health, 12(1), 1. https://doi.org/10.1186/1471-2458-12-1
- Maslach, C. (1976). Burned-out. Human Behavior: The Newsmagazine of the Social Sciences, 5, 16–22.
- Maslach, C. (1978). The client role in staff burn-out. Journal of Social Issues, 34(4), 111–124. https://doi.org/10.1111/j.1540-4560.1978.tb00778.x
- Maslach, C., & Jackson, S. E. (1981). The measurement of experienced burnout. Journal of Organizational Behavior, 2(2), 99–113. https://doi.org/10.1002/job.4030020205
- Maslach, C., Jackson, S. E., & Leiter, M. P. (1996). Maslach Burnout Inventory manual (3rd ed). Mind Garden.
- Maslach, C., Jackson, S. E., & Leiter, M. P. (2016). Maslach Burnout Inventory manual (4th ed). Mind Garden.
- Maslach, C., Jackson, S. E., Leiter, M. P., Schaufeli, W. B., & Schwab, R. L. (2022, December 15). Maslach Burnout Inventory™ (MBI). Mind Garden. https://www.mindgarden.com/117-maslach-burnout-inventory-mbi#horizontalTab4.
- Maslach, C., & Leiter, M. P. (1997). The truth about burnout: How organizations cause personal stress and what to do about it. Jossey-Bass.
- Maslach, C., & Leiter, M. P. (2016). Chapter 43 - Burnout. In G. Fink (Ed.), Stress: Concepts, cognition, emotion, and behavior (pp. 351–357). Academic Press. https://doi.org/10.1016/B978-0-12-800951-2.00044-3
- Maslach, C., & Leiter, M. P. (2022). The burnout challenge managing people’s relationships with their jobs. Harvard University Press.
- Maslach, C., & Pines, A. (1977). The burn-out syndrome in the day care setting. Child Care Quarterly, 6(2), 100–113. https://doi.org/10.1007/BF01554696
- Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52(1), 397–422. https://doi.org/10.1146/annurev.psych.52.1.397
- McCammon, L. C., Patricia, G., & Kernohan, W. G. (2023). Explaining and addressing the limitations in usefulness of available estimated prevalence figures relating to burnout in family doctors: Evidence from a systematic scoping literature review. Journal of Psychiatric Research, 158, 261–272. https://doi.org/10.1016/j.jpsychires.2022.12.013
- Meier, S. T. (1984). The construct validity of burnout. Journal of Occupational Psychology, 57(3), 211–219. https://doi.org/10.1111/j.2044-8325.1984.tb00163.x
- Meier, S. T., & Kim, S. (2022). Meta-regression analyses of relationships between burnout and depression with sampling and measurement methodological moderators. Journal of Occupational Health Psychology, 27(2), 195–206. https://doi.org/10.1037/ocp0000273
- Melnick, E. R., Powsner, S. M., & Shanafelt, T. D. (2017). In reply—Defining physician burnout, and differentiating between burnout and depression. Mayo Clinic Proceedings, 92(9), 1456–1458. https://doi.org/10.1016/j.mayocp.2017.07.005
- Milner, A., Page, K., Spencer-Thomas, S., & LaMontagne, A. D. (2014). Workplace suicide prevention: A systematic review of published and unpublished activities. Health Promotion International, 30(1), 29–37. https://doi.org/10.1093/heapro/dau085
- Nesse, R. M. (2000). Is depression an adaptation? Archives of General Psychiatry, 57(1), 14–20. https://doi.org/10.1001/archpsyc.57.1.14
- Niedhammer, I., Bertrais, S., & Witt, K. (2021). Psychosocial work exposures and health outcomes: A meta-review of 72 literature reviews with meta-analysis. Scandinavian Journal of Work, Environment & Health, 47(7), 489–508. https://doi.org/10.5271/sjweh.3968
- Oquendo, M. A., Bernstein, C. A., & Mayer, L. E. S. (2019). A key differential diagnosis for physicians-major depression or burnout? JAMA Psychiatry, 76(11), 1111–1112. https://doi.org/10.1001/jamapsychiatry.2019.1332
- Paykel, E. S., Brugha, T., & Fryers, T. (2005). Size and burden of depressive disorders in Europe. European Neuropsychopharmacology, 15(4), 411–423. https://doi.org/10.1016/j.euroneuro.2005.04.008
- Peterson, C., Maier, S. F., & Seligman, M. E. P. (1993). Learned helplessness: A theory for the age of personal control. Oxford University Press.
- Pickles, A., & Angold, A. (2003). Natural categories or fundamental dimensions: On carving nature at the joints and the rearticulation of psychopathology. Development and Psychopathology, 15(3), 529–551. https://doi.org/10.1017/S0954579403000282
- Pines, A. M., Aronson, E., & Kafry, D. (1981). Burnout: From tedium to personal growth. The Free Press.
- Plys, E., Al-Gobari, M., Farine, A., Rochat, L., Talpain, O., Blanc, S., Weissbrodt, R., Saillant, S., Rota, F., Droz, N., Wahlen, A., & Guseva Canu, I. (2022). Prise en charge des personnes en burnout en Suisse : Résultats de l’étude épidémiologique auprès des professionnels de la santé [Management of individuals with burnout in Switzerland: Results from an epidemiological study among healthcare professionals.]. Unisanté – Centre universitaire de médecine générale et santé Publique. Raisons de Santé, 337, 1–112.
- Podsakoff, P. M., Podsakoff, N. P., Williams, L. J., Huang, C. (2024). Common method bias: It's bad, it's complex, it's widespread, and it's not easy to fix. Annual Review of Organizational Psychology and Organizational Behavior, 11, 17–61. https://doi.org/10.1146/annurev-orgpsych-110721-040030
- Pryce, C. R., Azzinnari, D., Spinelli, S., Seifritz, E., Tegethoff, M., & Meinlschmidt, G. (2011). Helplessness: A systematic translational review of theory and evidence for its relevance to understanding and treating depression. Pharmacology & Therapeutics, 132(3), 242–267. https://doi.org/10.1016/j.pharmthera.2011.06.006
- Robins, E., & Guze, S. B. (1970). Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. The American Journal of Psychiatry, 126(7), 983–987. https://doi.org/10.1176/ajp.126.7.983
- Rolls, E. T. (2016). A non-reward attractor theory of depression. Neuroscience and Biobehavioral Reviews, 68, 47–58. https://doi.org/10.1016/j.neubiorev.2016.05.007
- Rotenstein, L. S., Torre, M., Ramos, M. A., Rosales, R. C., Guille, C., Sen, S., & Mata, D. A. (2018). Prevalence of burnout among physicians: A systematic review. JAMA, 320(11), 1131–1150. https://doi.org/10.1001/jama.2018.12777
- Rydmark, I., Wahlberg, K., Ghatan, P. H., Modell, S., Nygren, Å, Ingvar, M., Åsberg, M., & Heilig, M. (2006). Neuroendocrine, cognitive and structural imaging characteristics of women on longterm sickleave with job stress–induced depression. Biological Psychiatry, 60(8), 867–873. https://doi.org/10.1016/j.biopsych.2006.04.029
- Sapolsky, R. M. (2004). Why zebras don't get ulcers (3rd ed.). Holt Paperbacks.
- Sapolsky, R. M. (2021). Glucocorticoids, the evolution of the stress-response, and the primate predicament. Neurobiology of Stress, 14, 100320. https://doi.org/10.1016/j.ynstr.2021.100320
- Schaffner, A. K. (2016). Exhaustion and the pathologization of modernity. The Journal of Medical Humanities, 37(3), 327–341. https://doi.org/10.1007/s10912-014-9299-z
- Schaufeli, W. B. (2003). Past performance and future perspectives of burnout research. SA Journal of Industrial Psychology, 29(4), 1–15. https://doi.org/10.4102/sajip.v29i4.127
- Schaufeli, W. B., Bakker, A. B., Hoogduin, K., Schaap, C., & Kladler, A. (2001). On the clinical validity of the Maslach Burnout Inventory and the Burnout Measure. Psychology & Health, 16(5), 565–582. https://doi.org/10.1080/08870440108405527
- Schaufeli, W., Desart, S., & De Witte, H. (2020). The Burnout Assessment Tool (BAT) – development, validity and reliability. International Journal of Environmental Research and Public Health, 17(24), 9495. https://doi.org/10.3390/ijerph17249495
- Schaufeli, W. B., De Witte, H., Hakanen, J. J., Kaltiainen, J., & Kok, R. (2023). How to assess severe burnout? Cutoff points for the Burnout Assessment Tool (BAT) based on three European samples. Scandinavian Journal of Work, Environment & Health, 49(4), 293–302. https://doi.org/10.5271/sjweh.4093
- Schaufeli, W. B., & Enzmann, D. (1998). The burnout companion to study and practice: A critical analysis. Taylor & Francis.
- Schaufeli, W. B., Leiter, M. P., & Maslach, C. (2009). Burnout: 35 years of research and practice. The Career Development International, 14(3), 204–220. https://doi.org/10.1108/13620430910966406
- Schaufeli, W. B., & Taris, T. W. (2005). The conceptualization and measurement of burnout: Common ground and worlds apart. Work and Stress, 19(3), 256–262. https://doi.org/10.1080/02678370500385913
- Schonfeld, I. S. (1991). Burnout in teachers: Is it burnout or is it depression? ERIC Document No. 335329. http://www.eric.ed.gov/PDFS/ED335329.pdf.
- Schonfeld, I. S. (2018, July 3). When we say ‘physician burnout,’ we really mean depression. Medscape Psychiatry. https://www.medscape.com/viewarticle/898662.
- Schonfeld, I. S., & Bianchi, R. (2022). Distress in the workplace: Characterizing the relationship of burnout measures to the Occupational Depression Inventory. International Journal of Stress Management, 29(3), 253–259. https://doi.org/10.1037/str0000261
- Schonfeld, I. S., & Chang, C.-H. (2017). Occupational health psychology: Work, stress, and health. Springer Publishing Company.
- Schwenk, T. L., & Gold, K. J. (2018). Physician burnout—A serious symptom, but of what? JAMA, 320(11), 1109–1110. https://doi.org/10.1001/jama.2018.11703
- Seidler, A., Thinschmidt, M., Deckert, S., Then, F., Hegewald, J., Nieuwenhuijsen, K., & Riedel-Heller, S. G. (2014). The role of psychosocial working conditions on burnout and its core component emotional exhaustion – A systematic review. Journal of Occupational Medicine and Toxicology, 9(1), 10. https://doi.org/10.1186/1745-6673-9-10
- Seligman, M. E. P. (1975). Helplessness: On depression, development, and death. W. H. Freeman.
- Sen, S. (2022). Is it burnout or depression? Expanding efforts to improve physician well-being. New England Journal of Medicine, 387(18), 1629–1630. https://doi.org/10.1056/NEJMp2209540
- Sethi, N. K., Bianchi, R., Sigsbee, B., & Bernat, J. L. (2015). Physician burnout: A neurologic crisis. Neurology, 84(20), 2098–2099. https://doi.org/10.1212/WNL.0000000000001630
- Shanafelt, T., Goh, J., & Sinsky, C. (2017). The business case for investing in physician well-being. JAMA Internal Medicine, 177(12), 1826–1832. https://doi.org/10.1001/jamainternmed.2017.4340
- Shirom, A. (2003). Job-related burnout: A review. In J. C. Quick, & L. E. Tetrick (Eds.), Handbook of occupational health psychology (pp. 245–265). American Psychological Association.
- Shirom, A. (2005). Reflections on the study of burnout. Work & Stress, 19(3), 263–270. https://doi.org/10.1080/02678370500376649
- Sowden, J. F., Schonfeld, I. S., & Bianchi, R. (2022). Are Australian teachers burned-out or depressed? A confirmatory factor analytic study involving the Occupational Depression Inventory. Journal of Psychosomatic Research, 157, 110783. https://doi.org/10.1016/j.jpsychores.2022.110783
- Swider, B. W., & Zimmerman, R. D. (2010). Born to burnout: A meta-analytic path model of personality, job burnout, and work outcomes. Journal of Vocational Behavior, 76(3), 487–506. https://doi.org/10.1016/j.jvb.2010.01.003
- Taris, T. W. (2006). Bricks without clay: On urban myths in occupational health psychology. Work & Stress, 20(2), 99–104. https://doi.org/10.1080/02678370600893410
- Tavella, G., Hadzi-Pavlovic, D., & Parker, G. (2021). Burnout: Redefining its key symptoms. Psychiatry Research, 302, 114023. https://doi.org/10.1016/j.psychres.2021.114023
- Terluin, B., Van Rhenen, W., Schaufeli, W. B., & De Haan, M. (2004). The Four-Dimensional Symptom Questionnaire (4DSQ): Measuring distress and other mental health problems in a working population. Work & Stress, 18(3), 187–207. https://doi.org/10.1080/0267837042000297535
- Tyssen, R. (2018). What is the level of burnout that impairs functioning. Journal of Internal Medicine, 283(6), 594–596. https://doi.org/10.1111/joim.12769
- Verkuilen, J., Bianchi, R., Schonfeld, I. S., & Laurent, E. (2021). Burnout–depression overlap: Exploratory structural equation modeling bifactor analysis and network analysis. Assessment, 28(6), 1583–1600. https://doi.org/10.1177/1073191120911095
- Weber, A., & Jaekel-Reinhard, A. (2000). Burnout syndrome: A disease of modern societies? Occupational Medicine, 50(7), 512–517. https://doi.org/10.1093/occmed/50.7.512
- Weinberger, A. H., Gbedemah, M., Martinez, A. M., Nash, D., Galea, S., & Goodwin, R. D. (2018). Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychological Medicine, 48(8), 1308–1315. https://doi.org/10.1017/S0033291717002781
- Wichers, M. (2014). The dynamic nature of depression: A new micro-level perspective of mental disorder that meets current challenges. Psychological Medicine, 44(7), 1349–1360. https://doi.org/10.1017/S0033291713001979
- Willner, P., Scheel-Krüger, J., & Belzung, C. (2013). The neurobiology of depression and antidepressant action. Neuroscience & Biobehavioral Reviews, 37(10), 2331–2371. https://doi.org/10.1016/j.neubiorev.2012.12.007
- World Health Organization. (2019, May 28). Burn-out an “occupational phenomenon”: International Classification of Diseases. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
- World Health Organization. (2022, December 15). International Classification of Diseases (11th ed.): QD85 Burnout. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281
- World Health Organization. (2023, March 31). Depressive disorder (depression). https://www.who.int/news-room/fact-sheets/detail/depression
