ABSTRACT
Background: Although many case reports on neologistic jargon have been documented, reports on semantic jargon are extremely rare, suggesting that semantic jargon may occur more rarely than neologistic jargon.
Aims: To investigate potential mechanisms underlying semantic jargon.
Methods & Procedures: We describe a patient who presented with semantic jargon after a left thalamic hemorrhage that mainly affected the pulvinar, lateral posterior nucleus, centromedian nucleus, and reticular nucleus. She was followed for 8 years, during which the temporal changes in her linguistic and neuropsychological functions were investigated.
Outcomes & Results: The patient’s semantic jargon disappeared and selective attention improved in parallel. Word-finding deficits remained at the end of the observation period.
Conclusions: Our observations of this patient suggest that a thalamic lesion can cause attentional and linguistic dysfunction that does not activate an intended word and its images and, conversely, fails to inactivate non-relevant words and associated images, resulting in semantic jargon.
Introduction
Semantic jargon is a form of fluent and well-articulated speech that is mostly devoid of phonological errors but is full of semantic anomalies and frequent verbal paraphasias (Brown, Citation1981). Verbal paraphasias in semantic jargon are real words, in contrast to the non-existent neologistic words found in neologistic jargon. Although many cases of neologistic jargon have been documented, case reports of semantic jargon are extremely rare, suggesting that semantic jargon may occur more rarely than neologistic jargon. To our knowledge, only a small number of reports have documented cases of semantic jargon in detail (Brown, Citation1981; Marshall, Chiat, Robson, & Pring, Citation1996). Marshall et al. (Citation1996) suggested that semantic jargon arises from difficulties in lexical access, resulting in missing noun slots being filled with paraphasias. Brown (Citation1981) emphasized an association between semantic jargon and attentional dysfunction. He reported that semantic jargon can be observed during confusional states, and that semantic jargon, confusion, and Korsakoff syndrome (confabulatory amnesia) constitute interrelated deficits, suggesting a relationship between semantic jargon and attentional function. Regarding the impact of attentional dysfunction on linguistic function, Murray (Citation2000) reported a negative correlation between attentional function and the ability to retrieve words. Thus, difficulties in lexical retrieval and attentional dysfunction may cause verbal paraphasias, which in the worst case result in semantic jargon. To date, however, no report has addressed this issue or described temporal changes in patients with semantic jargon. As Simmons and Buckingham (Citation1992) suggested, describing temporal changes in patients with aphasia is useful when investigating the mechanisms underlying this disease state.
Herein, we describe a patient who developed semantic jargon after a left thalamic hemorrhage. We followed her for 8 years, during which her linguistic and neuropsychological functions were documented in detail. We discuss potential mechanisms that may have caused her semantic jargon – in particular, attentional function and word retrieval ability.
Methods and procedures
Case presentation
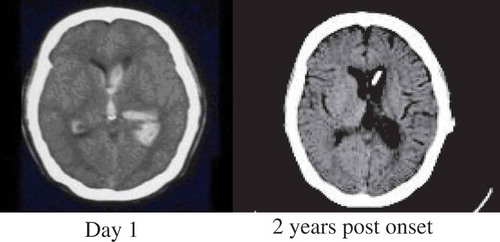
The patient and her family members granted informed consent in accordance with the Declaration of Helsinki. The ethical aspects of this study were reviewed and approved by the Human Research Ethics Committee of the Ashikaga Red Cross Hospital. The patient was a 39-year-old, right-handed native Japanese female with 16 years of education. She had no neurological or psychiatric disorders prior to her brain damage. She was intelligent and was working at a preschool education center when she suffered a left thalamic hemorrhage (, left panel) that affected the middle-to-posterior part of the left thalamus, covering the pulvinar, lateral posterior, centromedian, and reticular nuclei. Hydrocephalus owing to the hemorrhage to the left lateral ventricle was treated with ventriculoperitoneal shunting. For the first few months after onset, her condition was almost vegetative; she then gradually improved to a point where she was able to eat with assistance. She was transferred to a rehabilitation facility 3 months after the stroke and stayed there for 9 months. Since her discharge, her parents have cared for her at home. Although she had no right hemi-palsy, she could not perform daily living activities such as routine use of the toilet, owing largely to attentional dysfunction and right hemi-space neglect. Since year 1.5 post onset, she has participated in once-weekly linguistic rehabilitation sessions at the cognitive function clinic affiliated with the Ashikaga Red Cross Hospital. However, she continues to be easily fatigued and cannot concentrate on easy tasks even for a few minutes, suggesting that she has severe attentional dysfunction. Although she has episodic memory deficits, she does not show any confabulations associated with Korsakoff syndrome. Computed tomography of her brain taken 2 years after her stroke (, right panel) revealed a lesion in the middle-to-posterior part of her left thalamus.
Figure 1. Computed tomography of the patient’s brain.
Left thalamic hemorrhage with ventricle rupture as seen immediately after the hemorrhage (day 1), and the same area at year 2 post onset. The lesion mainly involved middle-to-posterior parts of the thalamus, including the pulvinar, lateral posterior, centromedian, and reticular nuclei.
Regarding linguistic function, the patient’s speech is fluent, grammatically correct, articulate, and prosodic. Her maximum number of phrases in sentence repetition is six, which is normal. Her forward digit span has a maximum of six, and her non-word repetition is preserved. She has no phonological paraphasias. In daily conversation, however, her speech includes semantic jargon with frequent irrelevant verbal paraphasias, and her meaning is often unclear. For example, she once said, “Yuka tatsumi ni itoganakatta?” (“Was there some thread on the floor and southeast?”). The examiner replied, “What kind of thread do you mean?” She replied, “Saibou no ittchi.” (“It was the consistency of cells.”). The examiner asked, “What are you going to use it for?” She answered, “Kuchino naka 100do ni nattari 10do ni nattarisite amari takaioto niwa naranaikeredo, 100do toka 120do ni narukara.” (“It rises to 100 or decreases to 10 degree Celsius in my mouth. Although it would not become so high-pitch sound, it rose to 100 or 120 degrees Celsius.”). Her auditory word comprehension and reading are poor but are less impaired than her jargon-filled speech would indicate. These features are consistent with what is known about thalamic aphasia: fluent output and unimpaired repetition with frequent verbal paraphasias that can deteriorate into jargon (Crosson, Citation2013). Among verbal paraphasias, irrelevant verbal paraphasia rather than relevant verbal paraphasia is one of the prominent features of thalamic aphasia (Luria, Citation1977; Nakano & Shimomura, Citation2015) as well as semantic jargon (Brown, Citation1981). In summary, her aphasia induced by the thalamic lesion is categorized as transcortical sensory aphasia accompanied by semantic jargon, which is the focus of this report. According to the microgenetic model of Brown (Citation1977), language production involves three stages: semantic, nominal, and phonemic. For this patient, the phonemic stage should be intact because her repetition is preserved and her speech contains no phonological paraphasias. In contrast, the first two stages are disrupted because she frequently uses both irrelevant and relevant verbal paraphasias.
Methods
We followed the temporal changes in the patient’s linguistic and neuropsychological functions in relation to her semantic jargon at 2, 4, and 8 years post stroke and investigated how her semantic jargon improved in relation to her attentional function and word-retrieval ability.
Linguistic function
To assess the patient’s general linguistic function, we administered the Standard Language Test of Aphasia (SLTA) in Japanese (Hasegawa, Kishi, Shigeno, Tanemura, & Kusunoki, Citation1985). The SLTA is composed of 26 tests of several language modalities, including auditory comprehension, speech, reading comprehension, writing, and arithmetic. For an overall assessment, data from the 26 subtests were converted into a total score, which was then classified as a grade on a scale from 0 to 10, with 10 being the best performance (Hasegawa et al., Citation1985). To assess the patient’s auditory comprehension, the word comprehension subtest in the SLTA was used.
To investigate the semantic and nominal levels in the language production process (Brown, Citation1977), the word-retrieval test (using 200 words) in the Test of Lexical Processing in Aphasia (TLPA; Fujita et al., Citation2000) was employed. In semantic jargon, semantic errors are typically distant in meaning from their presumed targets (i.e., irrelevant verbal paraphasia), thus differing from verbal paraphasia errors in which the category of the target is a relevant verbal paraphasia (Brown, Citation1981). According to Brown’s microgenetic model (Brown, Citation1977), irrelevant verbal paraphasia reflects disruption of the semantic level, where a set of semantic associates is aroused. Semantic jargon is most likely related with this level. Meanwhile, relevant verbal paraphasias (or no response) is considered to be caused by disruption of the nominal level, where the target word is selected from among semantic associates. To investigate changes in the patient’s semantic jargon over time, we assessed the proportion of irrelevant verbal paraphasias – the hallmark of semantic jargon – using the TLPA word-retrieval test. We recorded all responses to this test and transcribed them afterward. For classification of paraphasias, we followed the methods of Kohn and Goodglass (Citation1985) as follows:
No response. The patient (a) said nothing, (b) responded only with a general comment or question, or (c) used circumlocutions.
Relevant verbal paraphasias. The patient used real words (i.e., a superordinate, an in-class coordinate, a contextual associate, or material from which the target was made) to replace target words (e.g., “dog” rather than “cat”).
Irrelevant verbal paraphasias. The patient used real words to replace target words, but the words had no semantical or phonological association with the target words (e.g., “airplane” rather than “cat”). This classification included anomalous combination of Japanese morphemes (e.g., “kanazuchi-nihon”, or “hammer-Japan”, for “cat”).
Formal paraphasia. The patient used real words that are phonologically related to the target words (e.g., “negi” [radish] for “neko” [cat]).
Phonological paraphasia. The patient replaced target words with non-words that preserve at least half of the phonemes of the target word. Fragmentary syllables (e.g., “tochi” for “tomodachi” [friend]) were included in this category.
Neologism. The patient’s words phonologically flowed to the point of not being clearly recognizable when she attempted to produce a Japanese word. To distinguish between phonological paraphasia and neologism, phonological paraphasia was assigned when >50% of the target word phonemes were included in her answer, whereas neologism was assigned when the similarity of phonemes was <50%.
Perseveration. The patient responded in the same manner as found earlier in all responses. Preservation superseded classification as irrelevant or relevant verbal paraphasia when the response was classified as preservation and as verbal paraphasia (e.g., “dog” for “bridge” when the previous answer was “dog”).
Cognitive function
Assessment of the patient’s cognitive function covered only the non-verbal domain (i.e., non-verbal intelligence and attentional function) because her aphasia made it difficult to assess her memory and executive functions. However, memory and executive functions normally are unrelated to aphasia. Non-verbal intelligence was assessed by the Raven’s Colored Progressive Matrices (RCPM) (Sugishita & Yamazaki, Citation1993) and Performance Intelligence Quotient (PIQ) in the Japanese version of the Wechsler Adult Intelligence Scale (WAIS) (Fujii, Citation2006). We defined attention in this study as a basic cognitive function that is often a precursor to all other neurological/cognitive functions, including arousal, alertness, sustained attention, and selective attention (Fan, McCandlis, Sommer, Raz, & Posner, Citation2002; Ponsford & Kinsella, Citation1991). In this respect, unilateral spatial neglect, awareness, and anosognosia, which are included in attentional function, were excluded. To assess arousal, alertness, sustained attention, and selective attention, two types of assessments were administered: an observation assessment scale, as determined by the examiner, and performance of tasks. The observation assessment scale used was the Japanese version of Ponsford and Kinsella’s Attentional Rating Scale (Ponsford & Kinsella, Citation1991; Senzaki, Edakubo, Hoshi, & Kato, Citation1997), which covers 14 clinical inattention symptoms, each rated from 0 (no deficit) to 4 (most severe), with a maximum total score of 56. This scale contrasts with that of the cancellation of triangles in the Clinical Attention Assessment Test (Kato, Citation2006), which measures mainly the patient’s selective attention performance by requiring the patient to selectively delete triangles found with other non-relevant figures, such as circles or crosses. The percentages of omission errors per correct answers and false positives per total responses were recorded.
Results
presents temporal changes in the patient’s linguistic and neuropsychological function at 2, 4, and 8 years after onset.
Table 1. Results of neuropsychological assessments.
Intelligence
For non-verbal intelligence, the patient’s RCPM scores were the same at years 2 and 4 post-onset, and then slightly improved at year 8 post onset. Her WAIS PIQ at year 2 post onset was difficult to measure, mainly owing to her attentional dysfunction. Her attention span was short, and she tired easily after performing several tasks. For persons with severe attentional dysfunction, the RCPM is considered an easier test than the WAIS because the RCPM involves fewer tasks and has no time limit.
Attentional function
The patient made many omission errors during the triangle cancellation task at year 2 post onset, although she received perfect scores at years 4 and 8 post onset. Similarly, her percentage of false positives per total responses gradually decreased with time. Her score on the Ponsford and Kinsella Attentional Rating Scale also gradually improved. In summary, her attentional function improved substantially between years 2 and 8 post onset.
Linguistic function
In daily conversation, the patient frequently used semantic jargon at year 2 post onset, but she did so rarely by year 4 and not at all by year 8. At year 2 post onset, the patient was unaware that she was using semantic jargon. At no time did the patient exhibit pressured speech, which is sometimes observed in patients with jargon aphasia. In the linguistic assessment, the patient’s general linguistic function improved slightly over time, as did her comprehension.
At year 2 post onset, the percentage of correct answers for the TLPA word-retrieval test was 21% and the no-response score was 27%. Responses were classified as 29% irrelevant paraphasias, 14% relevant paraphasias, 5% perseveration, 2% phonological paraphasias, 2% neologisms, and 0% formal paraphasias. At year 4 post onset, the percentage of correct answers dropped to 18%, and the no-response score rose to 63%. The percentage for irrelevant paraphasias decreased to 9%, and relevant paraphasias, perseveration, phonological paraphasias, and formal paraphasias were 6%, 3%, 1%, and 0%, respectively. At year 8 post onset, the percentage for correct naming increased to 32%, and the no-response score was 50%. The percentage of irrelevant paraphasias decreased to 5%, the percentage of relevant paraphasias was 10%, and those for neologisms, perseveration, phonological paraphasias, and formal paraphasias were 2%, 1%, 0%, and 0%, respectively.
The percentage of irrelevant verbal paraphasias decreased sequentially over time and paralleled the improvement in attentional function (). The remarkable word-finding difficulties remained at the end of the observation period.
Figure 2. Changes in linguistic and neuropsychological function over the course of the study. The decline in the patient’s irrelevant paraphasias correlated with improved attentional function but not with intelligence or word-retrieval ability. CAT = Clinical Attention Assessment Test; RCPM = Raven’s Colored Progressive Matrices; TLPA = Test of Lexical Processing in Aphasia.
Discussion
Attentional dysfunction and word-finding difficulties are related to semantic jargon
This study found that attentional dysfunction is related to irrelevant verbal paraphasia and that word-finding difficulties remained at the end of the study period, suggesting that both attentional dysfunction and word-finding difficulties are related to semantic jargon after a thalamic lesion. Regarding attentional dysfunction, we particularly found that the percentage of false positives in the selective attention task correlated with the percentage of irrelevant paraphasia. Although the former involves an attentional task and the latter reflects linguistic function, the characteristics of these types of mistakes were similar because the patient gave irrelevant responses for each task. Several hypotheses have posited mechanisms underlying jargon aphasia. Some researchers have stressed that perseveration is crucial for the development of jargon aphasia (Butterworth, Citation1979; Green, Citation1969; Moses, Nickels, & Sheard, Citation2004). This was not the case for our patient, however, because the proportion of perseveration at each stage was quite small, with a maximum of 5% at year 2 post onset. The conclusion derived from an earlier study on jargon aphasia was that pressured speech as a result of hyperactivation of the linguistic system might cause jargon aphasia (Kinsbourne & Warrington, Citation1963). However, our patient did not show pressured speech. A self-monitoring deficit or anosognosia (Marshall, Citation2006) might account for our patient’s semantic jargon, but such deficits generally do not explain the specific reasons for semantic jargon because most patients with jargon aphasia – and even some patients with aphasia who show no jargon aphasia – show self-monitoring deficits or anosognosia. Our study thus extends the literature support for a positive correlation between attentional dysfunction and semantic jargon (Brown, Citation1981).
In addition to attentional dysfunction, the remaining word-finding difficulties are also considered a contributing factor to semantic jargon. The close relationship between word-finding difficulties and semantic jargon correspond to the gap-filling hypothesis for semantic jargon (Marshall et al., Citation1996) and also for neologistic jargon (Buckingham, Citation1977; Buckingham & Kertesz, Citation1976), in which paraphasias fill in gaps caused by word-finding difficulties. Disruption of nominal processes in the microgenetic model might have contributed to semantic jargon in this patient although it might be less critical compared with disruption of semantic processes.
The thalamus and semantic jargon
The thalamus consists of many nuclei, each with a distinctive role. For our patient, the middle-to-posterior parts of the thalamus were affected, covering the centromedian, lateral posterior, pulvinar, and reticular nuclei. The lateral posterior nucleus is mainly involved in various sensory functions (Krause et al., Citation2012), whereas the other three nuclei play crucial roles in aphasia and attentional dysfunction. The centromedian nucleus plays an important role in arousal and attentional function and mediates cortical and basal ganglia activities through its afferents and efferents (Nanda, Galvan, Smith, & Wichmann, Citation2009; van der Werf, Witter, & Groenewegen, Citation2002). The reticular and pulvinar nuclei have linguistic function through attentional function (Crosson, Citation2013). For our patient, attentional dysfunction (in particular, an arousal deficit) was most likely caused by disruption of the centromedian nucleus.
The basic function of the thalamus is to regulate the transfer of information from the sensory systems to the cortex and to relay information between cortical areas (Connelly, Laing, Errington, & Crunelli, Citation2015; McAlonan, Cavanaugh, & Wurtz, Citation2008; Saalmann & Kastner, Citation2011). Thalamic activity has been likened to a filter or a gate, i.e., it only lets through information dictated by higher areas. However, recent studies found that it also plays a role in inactivating irrelevant information and enhancing necessary information (Connelly et al., Citation2015; McAlonan et al., Citation2008; Saalmann & Kastner, Citation2011) to simultaneously increase correct information and decrease error. A stroke in the thalamus can result in superimposition of temporally unrelated information (Schmahmann, Citation2003).
Regarding linguistic function, Sebastian et al. (Citation2014) found that aphasia can occur without cortical hypoperfusion after thalamic stroke, suggesting that the left thalamus has a direct role in language processing by activating corresponding cortical areas. According to Crosson (Citation2013), the thalamus selectively activates cortical areas necessary for recalling the construct of a word, e.g., the construct “hammer,” including the visual form of a hammer, the motor sequences necessary to use a hammer, and an image of a nail being pounded into a board, while maintaining areas not involved in the word in a state of relative disengagement. In particular, the pulvinar nuclei are engaged in activating and deactivating specific cortical areas, and the reticular nucleus plays a role in passing information within the thalamus (Crosson, Citation2013) to activate the pulvinar nuclei. The thalamus also enhances the signal-to-noise ratio of the lexical selection process, thereby decreasing the chances for error, e.g., by activating an image of hammering while inactivating those of pounding and nailing. The ventral anterior nucleus and the reticular nucleus are related to this process (Crosson, Citation2013). In short, the thalamus (in particular, the pulvinar, reticular, and ventral anterior nuclei) activates a word and its relevant images and also inactivates irrelevant words and their images. Therefore, our findings suggest that thalamic injury can produce irrelevant paraphasias because it is unable to inactivate irrelevant words and images or distinguish a target word from other words. This process might overlap between a selective attention function and a linguistic function. However, frequent irrelevant paraphasias might reflect a selective attention function more than a linguistic function. The attentional mechanism differs from common aphasias caused by disruption of the language area. Luria (Citation1977) termed a type of aphasia induced by a thalamic lesion as a quasi-aphasia speech disturbance, which he did not consider to be of normal nature of aphasia. He also suggested that a defect of vigilance (i.e., sustained attention; Oken, Salinsky, & Elsas, Citation2006) might perturb verbal processes, resulting in a quasi-aphasia speech disturbance.
Although this study involved only one case, our findings suggest that semantic jargon induced by a thalamic lesion may be heavily dependent on attentional dysfunction and word-finding difficulties. Our view is compatible with Brown’s remark that semantic jargon may be observed during a confusional state (Brown, Citation1981) and also with Marshall’s gap-filling theory (Marshall et al., Citation1996). To our knowledge, this is the first demonstration of a relationship between attentional function and semantic jargon. Studies of the neural basis for semantic jargon are relatively rare, and Brown (Citation1981) mainly addresses the left temporal lobe. Semantic jargon in Brown’s case may be more dependent on word-finding difficulties due to disruption in the language area. In contrast, our study suggests that semantic jargon following a thalamic lesion may be more dependent on thalamic attentional dysfunction.
Conclusions
We describe the temporal monitoring of a patient who displayed semantic jargon after thalamic hemorrhage. Our observations suggest that attentional dysfunction and word-finding difficulties might cause semantic jargon. In this patient, the observed semantic jargon might be related to failure to prioritizing the intended word and its images and inactivating irrelevant words and their images
Consent for publication
Written informed consent to publish in this journal was obtained from the patient.
Availability of data and materials
All data are presented in the manuscript.
Acknowledgments
We thank the patient and members of her family for allowing us to perform this study.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
Notes on contributors
Asuka Nakajima
Both authors acquired the case data, designed the study, and drafted the manuscript.
Michitaka Funayama
Both authors acquired the case data, designed the study, and drafted the manuscript.
References
- Brown, J. W. (1977). Mind, brain, and consciousness: The neuropsychology of cognition. New York, NY: Academic Press.
- Brown, J. W. (1981). Case reports of semantic jargon. In J. W. Brown (Ed.), Jargonaphasia (pp. 169–176). New York, NY: Academic Press.
- Buckingham, H. M., & Kertesz, A. (1976). Neologistic jargon aphasia: Neurolinguistics III. Amsterdam: Swets & Zeitlinger.
- Buckingham, H. W. (1977). The conduction theory and neologistic jargon. Language and Speech, 20, 174–184. doi:10.1177/002383097702000209
- Butterworth, B. (1979). Hesitation and the production of verbal paraphasias and neologisms in jargon aphasia. Brain and Language, 8, 133–161. PubMed: 487066 10.1016/0093-934X(79)90046-4
- Connelly, W. M., Laing, M., Errington, A. C., & Crunelli, V. (2015). The thalamus as a low pass filter: Filtering at the cellular level does not equate with filtering at the network level. Front Neural Circuits, 9, 89. doi:10.3389/fncir.2015.00089
- Crosson, B. (2013). Thalamic mechanisms in language: A reconsideration based on recent findings and concepts. Brain and Language, 126, 73–88. doi:10.1016/j.bandl.2012.06.011
- Fan, J., McCandlis, B. D., Sommer, T., Raz, A., & Posner, M. I. (2002). Testing the efficiency and independence of attentional networks. Journal of Cognitive Neuroscience, 14, 340–347. doi:10.1162/089892902317361886
- Fujii, K. (2006). Wechsler adult intelligence scale. Tokyo: Nihon Bunka Kagakusha.
- Fujita, I., Monoi, H., Okudaira, N., Uedai, M., Ono, K., Shimogaki, Y., … Sasanuma, S. (2000). Developing a Test of Lexical Processing in Aphasia (TLPA). The Japan Journal of Logopedics and Phoniatrics, 41, 179–202. doi:10.5112/jjlp.41.179
- Green, E. (1969). Phonological and grammatical aspects of Jargon in an Aphasic patient: A case study. Language and Speech, 12, 103–118. doi:10.1177/002383096901200203
- Hasegawa, T., Kishi, H., Shigeno, K., Tanemura, J., & Kusunoki, T. (1985). Three-dimensional structure in language tests of aphasia. Folia Phoniatrica et Logopaedica, 37, 246–258. [PubMed: 2419231] 10.1159/000265805
- Kato, M. (2006). Clinical assessment of attention. Tokyo: Shinkoigakushuppankai.
- Kinsbourne, M., & Warrington, E. (1963). Jargon aphasia. Neuropsychologia, 1, 27–37. doi:10.1016/0028-3932(63)90010-1
- Kohn, S. E., & Goodglass, H. (1985). Picture-naming in aphasia. Brain and Language, 24, 266–283. [PubMed: 3978406] 10.1016/0093-934X(85)90135-X
- Krause, T., Brunecker, P., Pittl, S., Taskin, B., Laubisch, D., Winter, B., … Jungehulsing, G. J. (2012). Thalamic sensory strokes with and without pain: Differences in lesion patterns in the ventral posterior thalamus. Journal of Neurology, Neurosurgery, and Psychiatry, 83, 776–784. doi:10.1136/jnnp-2011-301936
- Luria, A. R. (1977). On quasi-aphasic speech disturbances in lesions of the deep structures of the brain. Brain and Language, 4, 432–459. [PubMed: 907879] 10.1016/0093-934X(77)90036-0
- Marshall, J. (2006). Jargon aphasia: What have we learned? Aphasiology, 20, 387–410. doi:10.1080/02687030500489946
- Marshall, J., Chiat, S., Robson, J., & Pring, T. (1996). Calling a salad a federation: An investigation of semantic jargon. Part 2- verbs. Journal of Neurolinguistics, 9, 251–260. doi:10.1016/S0911-6044(97)82797-2
- McAlonan, K., Cavanaugh, J., & Wurtz, R. H. (2008). Guarding the gateway to cortex with attention in visual thalamus. Nature, 456, 943–956. doi:10.1038/nature07382
- Moses, M., Nickels, L., & Sheard, C. (2004). Disentangling the web: Neologistic perseverative errors in jargon aphasia. Neurocase, 10, 452–461. doi:10.1080/13554790490894057
- Murray, L. L. (2000). The effects of varying attentional demands on the word retrieval skills of adults with aphasia, right hemisphere brain damage, or no brain damage. Brain and Language, 72, 40–72. doi:10.1006/brln.1999.2281
- Nakano, A., & Shimomura, T. (2015). Dominant thalamus and aphasia. Brain Nerve, 67, 1495–1498. doi:10.11477/mf.1416200327
- Nanda, B., Galvan, A., Smith, Y., & Wichmann, T. (2009). Effects of stimulation of the centromedian nucleus of the thalamus on the activity of striatal cells in awake rhesus monkeys. European Journal of Neuroscience, 29, 588–598. doi:10.1111/j.1460-9568.2008.06598.x
- Oken, B. S., Salinsky, M. C., & Elsas, S. M. (2006). Vigilance, alertness, or sustained attention: Physiological basis and measurement. Clinical Neurophysiology, 117, 1885–1901. doi:10.1016/j.clinph.2006.01.017
- Ponsford, J., & Kinsella, G. (1991). The use of a rating scale of attentional behaviour. Neuropsychological Rehabilitation, 1, 241–257. doi:10.1080/09602019108402257
- Saalmann, Y. B., & Kastner, S. (2011). Cognitive and perceptual functions of the visual thalamus. Neuron, 71, 209–223. doi:10.1016/j.neuron.2011.06.027
- Schmahmann, J. D. (2003). Vascular syndromes of the thalamus. Stroke, 34, 2264–2278. doi:10.1161/01.STR.0000087786.38997.9E
- Sebastian, R., Schein, M. G., David, C., Gomez, Y., Newwart, M., Oishi, K., & Hillis, A. E. (2014). Aphasia or neglect after thalamic stroke: The various ways they may be related to cortical hypoperfusion. Frontier in Neurology, 5, 1–7. doi:10.3389/fneur.2014.00231
- Senzaki, A., Edakubo, T., Hoshi, K., & Kato, M. (1997). The reliability and validity of a clinical attentional scale. Sogo Rehabilitation, 25, 567–573. doi:10.11477/mf.1552108403
- Simmons, N. N., & Buckingham, H. W. (1992). Recovery in jargonaphasia. Aphasiology, 6, 403–414. doi:10.1080/02687039208248611
- Sugishita, M., & Yamazaki, K. (1993). Japanese Raven’s coloured progressive matrices. Tokyo, Japan: Nihonbunkasha.
- van der Werf, Y. D., Witter, M. P., & Groenewegen, H. J. (2002). The intralaminar and midline nuclei of the thalamus. Anatomical and functional evidence for participation in processes of arousal and awareness. Brain Research Reviews, 39, 107–140. [PubMed: 12423763] 10.1016/S0165-0173(02)00181-9
